To compare the effects of conventional (constant load) eccentric training and isokinetic eccentric training on quadriceps muscle mass, strength and functional performance in recreational athletes following anterior cruciate ligament (ACL) reconstruction.
MethodsThirty recreational male athletes (25 years old) undergoing ACL reconstruction received a standard rehabilitation program. Volunteers were randomized to conventional group (CG; n = 15) or isokinetic group (IG; n = 15) to be engaged in a 6-week (2 sessions/week) quadriceps eccentric training program at the extensor chair or at the isokinetic dynamometer, respectively. Assessments of quadriceps muscle mass (through magnetic resonance imaging), strength (through isokinetic dynamometry) and self-aware functionality (through questionnaire) were performed before and after the training programs. Single leg hop test performance was assessed only at post-training evaluation.
ResultsIG had significantly higher improvements than CG (p < 0.05) for all muscle mass outcomes (+17–23% vs. +5–9%), as well as for isometric (+34% vs. +20%) and eccentric (+85% vs. +23%) peak torques. There was no between-group difference (p > 0.05) for concentric peak torque, Lysholm score, and single leg hop test.
ConclusionIsokinetic eccentric training promotes greater responses than conventional eccentric training on quadriceps muscle mass and strength of recreational athletes following ACL reconstruction.
The anterior cruciate ligament (ACL) plays a fundamental role in the passive stability of the knee joint.1 The ACL rupture occurs more frequently in physically active young adults,2 mainly professional, amateur and recreational athletes.3 Despite the growing knowledge over the risk factors and strategies for prevention of ACL rupture,4 the incidence within professional athletes has not decreased in the past two decades.5 The average time to return to sport is 244 days,6 so ACL injuries compromise team performance and finances.7
The current standard procedure to treat physically active patients with ACL rupture is ligament reconstruction surgery.2 Although this surgery restores the knee mechanical stability,8 patients are often affected by considerable loss of muscle mass and by inhibition of the voluntary activation of the quadriceps muscle during post-operative period.9 Consequently, a marked quadriceps muscle weakness is expected in the initial rehabilitation phase.10 Since strength deficits can persist for up to three years after reconstruction,9 some athletes may return to sport with strength imbalances between the operated and the unaffected limb, and/or between the knee extensor and flexor muscle groups.11 These strength deficits have been associated to alterations in knee mechanics,12 reduction in functional performance,13 delayed return to preinjury competitive level,14 increased risk of ligament re-injury15 and development of knee osteoarthritis.16
Strength training is a fundamental stage within the rehabilitation programs following ACL reconstruction.17 Although traditional strength training is performed with the same external load during the exercises’ concentric and eccentric phases, evidence suggests that eccentric overload exercises optimize muscle hypertrophy and strengthening.18 Studies with healthy elderly,19 young adults20 and athletes21 have demonstrated higher increments in muscle mass, strength and functional performance through eccentric training compared to traditional strength training. Similarly, eccentric training appears to be more effective to restore quadriceps muscle mass,22–24 strength23,25 and functional performance23,25 in individuals undergoing ACL reconstruction. This body of evidence supports the safety and effectiveness of eccentric training in rehabilitation programs of these patients.22–29
Eccentric loading during ACL rehabilitation has been performed through exercises on specific cycle ergometers,22–26 conventional (constant load) gym machines (e.g. leg press)28,29 and isokinetic dynamometers (either in open27 or closed24 kinetic chain). The isokinetic dynamometer enables the performance of exercises with maximal intensity and constant angular velocity along the full range of motion.30 It means the equipment allows the exercise to be performed at the individual strength maximal level at each joint angle, and minimizes the risk of loading above the patient’s tolerance.31 Therefore, isokinetic exercise has been included in rehabilitation programs to optimize muscle strengthening, especially when treating elite athletes.32 Nevertheless, a question remains to be answered in sports physical therapy: does isokinetic exercise produce greater muscle strength gains than conventional exercise (i.e. constant load) in patients following ACL reconstruction?
The aim of the present study was to compare the effects of conventional eccentric training and isokinetic eccentric training on quadriceps muscle mass, strength and functional performance in recreational athletes following ACL reconstruction. Our hypothesis was that isokinetic eccentric training would lead to greater increments on quadriceps muscle mass, strength and functional performance compared to conventional eccentric training.
MethodsStudy designThis study was an assessor-blinded, randomized controlled trial. All participants underwent ACL reconstruction surgery. Next, they were randomized to conventional group (CG) or isokinetic group (IG). All participants were engaged in a standard rehabilitation program. Approximately 45 days post-surgery, they initiated either the 6-week conventional or isokinetic eccentric training program. Assessments of quadriceps muscle mass (through magnetic resonance imaging), strength (through isokinetic dynamometry) and self-aware functionality (through questionnaire) were performed one week prior to starting eccentric training and one week after conclusion. Single leg hop test performance was assessed only at post-training evaluation. This study was approved by the ethics committee of the Universidade Federal de Ciências da Saúde de Porto Alegre, Porto Alegre, RS, Brazil (protocol number 1.461.842) and prospectively registered at www.clinicaltrials.gov (NCT02961543).
ParticipantsMale subjects submitted to ACL reconstruction surgery were invited to the study. To be included, participants should be 18–40 years old recreational athletes (i.e., they practiced sports to be physically fit and/or to have fun),33 engaged in a systematic sports practice with minimum frequency of once a week, with body mass index between 18.5 and 24.9 kg/m², and unilateral ACL rupture diagnosed through clinical evaluation and magnetic resonance imaging. Participants were excluded in the following cases: re-injury; injury event longer than 90 days; associated ligament and/or meniscal injury; associated patellofemoral pain syndrome; muscle injury in the previous 6 months; respiratory or cardiovascular limiting condition; consumers of anabolic steroids or nutritional supplements designed to gain muscle mass. All eligible participants received instructions relative to the aims and procedures of the study and signed a consent form.
Sample sizeThe number of participants was estimated using the free-access software WinPepi (Copyright JH Abramson, 2012). The knee extension peak torque is considered a primary outcome in the current study, so results reported by Brasileiro et al.27 were used in the sample size estimation. Power was set as 80%, with an alpha level of 5%, resulting in a sample size of 15 subjects per group.
Randomization and blindingParticipants were randomly allocated to one of two groups by flipping a coin (heads—CG, tails—IG).34 This procedure was performed by an independent researcher not involved in the patients’ evaluation or rehabilitation. The surgeons and researchers responsible for evaluations were blinded to participants’ allocation until the end of the study. The physical therapists who applied the training programs did not participate in the evaluations.
ACL reconstruction surgeryThe technique performed was ACL anatomical reconstruction through simple band with autologous graft from ipsilateral knee flexor tendons (semitendinosus and gracilis muscles). All surgeries were performed at the Hospital Ortopédico de Passo Fundo (Passo Fundo, RS, Brazil) by the same two knee surgeons who had at least 15 years of technical experience with ACL reconstruction.35
Post-surgery rehabilitationUp to the 30th day after ACL reconstruction, participants received a standard physical therapy protocol with 60-min daily sessions. The main goals and procedures of this early stage of the rehabilitation were: (1) reducing pain and swelling (PRICE method); (2) increasing knee range of motion (stretching exercises for knee flexion and extension, and static stretching of muscle groups around hip and ankle); (3) avoiding muscle atrophy and improving neuromuscular activation (straight-leg raise exercise, unilateral closed kinetic chain isometric and dynamic exercises, proximal stability exercises); (4) improving balance and proprioception (neuromuscular exercises, from bipedal to unipedal and from the ground to unstable boards); and (5) restoring gait capacity (anterior, posterior and lateral displacement between parallel bars, followed by independent gait and exercises with steps). Participants adherence was of 100% and no adverse effects were reported.
Eccentric training programsParticipants allocated to the IG were engaged in an isokinetic eccentric training program using a Biodex™ Multi Joint System 3 Pro computerized dynamometer (Biodex Medical System, United States of America). The isokinetic eccentric training program was applied for 6 weeks, twice a week, with a minimal interval of 72 h between sessions. In each training session, participants performed three (1st mesocycle: weeks 1–3) or four sets (2nd mesocycle: weeks 4–6) of 10 maximal intensity knee extensor eccentric contractions.36,37 A one-minute resting interval was given between sets. The isokinetic eccentric contractions were performed as described by Fallow36,37: after the researcher passively positioned the participant’s knee in 30° of flexion (0° = full knee extension), the participant was encouraged to perform a maximal eccentric contraction of the knee extensor muscles to resist against the movement of knee flexion exerted by the dynamometer until 90° of knee flexion, at a 60°/s constant angular velocity.
Participants allocated in the CG were engaged in a conventional eccentric training program using an extensor chair (Kenkorp, Brazil). Training duration, weekly frequency and volume (number of sets and repetitions) were the same adopted for IG. During the eccentric exercise on the extensor chair, the concentric phase (from 90° to 30° of knee flexion) was performed by a researcher. From this position, participants were instructed to perform a knee extensor eccentric contraction to return their legs to 90° of knee flexion in a controlled manner. An electronic metronome was used to maintain a standard cadence of 2 s for each movement phase. The load for the first training session was estimated at 80% of the knee extensor eccentric peak torque. The exercise load was increased progressively throughout the training program according to the individual patient feedback (i.e. self-perception of ability) and muscle strength response (i.e. once the patient could perform an 11th repetition into a set, the load was increased in the next set or training session).
Muscle mass evaluationThe anatomical cross-sectional area (ACSA) of the quadriceps femoris muscle was measured using images taken from participants’ thigh through T2-weighted magnetic resonance imaging (MRI) (3.0 T Magnetom, Siemens, Berlim, Germany; repetition time 4260 ms, echo time 95 ms, means: 3, vision field of 200 × 200, cutting thickness of 4 mm). Cross-sectional images were taken at 50% of the distance between the smaller trochanter and the lateral femoral condyle. All assessments were taken by the same radiologist with 12 years of experience in this evaluation. MR images were analyzed using the Image-J software (National Institute of Health, USA). The perimeter of each muscle (rectus femoris, vastus intermedius, vastus lateralis and vastus medialis) was assessed manually by a single researcher blinded to the groups allocation. The average of three measures was used for analysis. The quadriceps femoris’ ACSA was estimated by summing the perimeters of these muscles.
Muscle strength evaluationThe Biodex™ Multi Joint System 3 Pro computerized dynamometer (Biodex Medical System, United States of America) was calibrated prior to each assessment, and participants were positioned according to manufacturer’s recommendations. All participants performed a familiarization session two days before the pre-training evaluation in order to minimize learning effects. After a specific warm-up (10 submaximal concentric repetitions at 90°/s), isometric peak torque was assessed though three 5-s maximal isometric contractions of the knee extensor muscles at 60° of knee flexion (0° = full extension).37 Next, concentric and eccentric peak torques were measured through three maximal contractions at 60°/s with ranges of motion between 90° to 10° and 30° to 90°, respectively.36,37 Participants rested for 2 min between tests. A single researcher with experience in isokinetic evaluation and blinded to groups allocation was responsible for all assessmsents. He provided standard instructions, feedback and encouragement during testing.
Functional performance evaluationFunctional performance was assessed before and after the training programs using the Lysholm score version translated to Brazilian Portuguese and validated for patients with ligament injury.38 Additionally, the single leg hop test39 was performed only after the training programs (95–100 days after surgery).
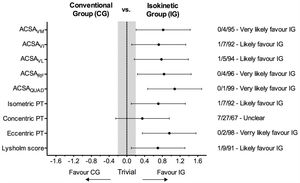
Statistical analysisIndividual deficits in muscle mass and strength found in operated compared to the non-operated leg before and after training for each group were calculated. Effect sizes (ES) found for muscle mass and strength outcomes were calculated through the Cohen’s d, and training effects were considered as “trivial” (ES < 0.2), “small” (ES > 0.2), “moderate” (ES > 0.5) or “large” (ES > 0.8).40 Longitudinal percent changes (pre- to post-training) were used for between-group comparison through independent t-tests, with a significance level set as 5% (α < 0.05). The same statistical procedure was used to compare the post-training single leg hop test found in IG and CG. In addition, data were analyzed for practical significance using magnitude-based inferences because null hypothesis tests do not indicate the magnitude of an effect.41 The chances of a possible substantial effect favorable to CG or IG were calculated [i.e., greater that the smallest worthwhile change (0.2 multiplied by the between-subject standard deviation)]. Quantitative chances of trivial effects and substantial effects for each group were assessed qualitatively as follows: <1%, almost certainly not; 1–5%, very unlikely; 5–25%, unlikely; 25–75% = possibly; 75–95% = likely; 95–99% = very likely; >99% = almost certain.42 When the CG and IG values were both >5%, the inference was classified as unclear.42
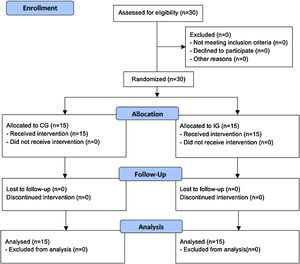
ResultsThe current study had no sample losses, as shown in Fig. 1. CG and IG were similar for age (24.3 ± 4.6 vs. 26.9 ± 5.8 years), body mass (78.7 ± 6.0 vs. 78.2 ± 8.7 kg), height (178.4 ± 8.9 vs. 178.5 ± 8.6 cm), and body mass index (23.7 ± 1.2 vs. 23.4 ± 1.0 kg/m2).
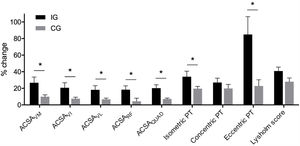
Fig. 2 shows the deficits on muscle mass and strength outcomes found in each group before and after the training programs. IG presented larger effect sizes (pre- to post-training) than CG for all outcomes (Table 1). IG had significantly higher improvements than CG (p < 0.05) for all muscle mass outcomes, as well as for isometric and eccentric peak torques (Fig. 3). There was no between-group difference (p > 0.05) for the concentric peak torque and for the Lysholm score (Fig. 3), as well as for the post-training single leg hop test (CG = 163.1 ± 31.8; IG = 168.0 ± 28.1). The magnitude-based inference supports that results ‘likely’ or ‘very likely’ favour IG compared to CG for all outcomes, with exception of the concentric peak torque (Fig. 4).
Muscle mass, strength and functionality (mean and standard deviation) at pre- and post-training for conventional group (CG) and isokinetic group (IG).
| CG (n = 15) | IG (n = 15) | |||||
|---|---|---|---|---|---|---|
| Pre | Post | ES | Pre | Post | ES | |
| Muscle mass (cm2) | ||||||
| ACSAVL | 27.6 ± 3.7 | 29.4 ± 3.6 | 0.51b | 23.3 ± 4.7 | 27.2 ± 5.2 | 0.81c |
| ACSAVI | 14.9 ± 2.5 | 16.0 ± 2.5 | 0.46a | 13.0 ± 2.5 | 15.5 ± 3.0 | 0.94c |
| ACSAVM | 16.9 ± 3.7 | 18.5 ± 3.8 | 0.44a | 14.1 ± 3.1 | 17.4 ± 3.0 | 1.12c |
| ACSARF | 8.4 ± 2.3 | 8.8 ± 2.4 | 0.18 | 7.4 ± 1.3 | 8.8 ± 1.9 | 0.89c |
| ACSAQUAD | 68.1 ± 10.0 | 72.8 ± 9.6 | 0.50b | 58.0 ± 8.1 | 69.0 ± 7.7 | 1.44c |
| Strength (Nm) | ||||||
| Isometric PT | 181.2 ± 30.3 | 215.5 ± 33.5 | 1.11c | 197.7 ± 45.2 | 256.0 ± 32.2 | 1.54c |
| Concentric PT | 176.6 ± 51.8 | 205.7 ± 44.1 | 0.63b | 165.1 ± 38.8 | 206.0 ± 41.6 | 1.05c |
| Eccentric PT | 109.1 ± 34.3 | 128.8 ± 30.7 | 0.63b | 97.7 ± 30.4 | 162.1 ± 38.3 | 1.93c |
| Functionality (a.u.) | ||||||
| Lysholm score | 72.7 ± 12.1 | 91.6 ± 9.8 | 1.78c | 71.5 ± 9.3 | 99.2 ± 1.7 | 4.29c |
ACSA, anatomical cros-sectional area; ES, effect size; PT, peak torque; QUAD, quadriceps; RF, rectus femoris; VI, vastus intermedius; VL, vastus lateralis; VM, vastus medialis.
aSmall effect size.
bModerate effect size.
cLarge effect size.
Percent change (mean and standard error) at pre- to post-training for conventional group (CG) and isokinetic group (IG).
ACSA, anatomical cros-sectional area; VL, vastus lateralis; VM, vastus medialis; VI, vastus intermedius; RF, rectus femoris; QUAD, quadriceps; PT, peak torque; * significant difference (baseline × pós-training; p < 0.05).
This randomized controlled trial used rehabilitation programs based on eccentric exercises, either in conventional (constant load) or in isokinetic conditions, to restore the quadriceps muscle mass, strength and functional performance of recreational athletes undergoing ACL reconstruction. The main finding of this study was that isokinetic training promoted greater muscle hypertrophy and strengthening than conventional training.
Evidence suggests that exclusively eccentric training programs or those containing eccentric overloading optimize the muscle responses to strength training.18 Although the underlying mechanics remain unclear, the maximal force production capacity of the skeletal muscle is higher during eccentric compared to concentric contraction.43 Therefore, using the same load during both the concentric and the eccentric phases leads the muscle to work in a lower relative intensity (percentage of maximal capacity) during the eccentric phase than during the concentric phase. Consequently, traditional strength training favours gains in concentric compared to eccentric strength.44 Moreover, the greater mechanical tension exerted on muscle tissue during eccentric exercise promotes a larger exercise-induced muscle damage, which is one of the key mechanisms to muscle hypertrophy.45 The superiority of eccentric training over traditional strength training has been endorsed by other studies involving patients submitted to ACL reconstruction.22,23,25
Studies that engaged patients that underwent ACL reconstruction in eccentric training programs found increases of 9–28% in quadriceps cross-sectional area,22,24,26,27 20–28% in maximal knee extension concentric strength,25,26 15–16% in maximal knee extension isometric strength,27,29 12–20% in maximal knee extension eccentric strength,27 and 25–40% in hopping tests.25,26 These previous studies employed eccentric training programs by 6–12 weeks.22–29 The trials by Gerber et al.22,23,25,26 started the strengthening programs with cycle ergometer exercise 3 weeks after the ACL reconstruction, while participants rehabilitated by Lepley et al.28,29 started the leg-press exercises at 6 weeks following surgery. In isokinetic conditions, the strengthening programs initiated exercises in closed and open kinetic chain at 3 and 9 months after surgery, respectively.24,26 Therefore, one must be cautious when comparing the effects promoted by the eccentric training programs of these previous studies with the effects of the current study, once our strengthening program started approximately 45 days after surgery and used open kinetic chain exercises in conventional or isokinetic devices. However, our findings agree with the body of evidence supporting the benefits of eccentric training in the rehabilitation of individuals that underwent ACL reconstruction, either using isokinetic or constant load exercises.
Loss of quadriceps muscle strength following ACL reconstruction is related to the neuromuscular inhibition caused by both injury46 and post-surgery inflammatory process,47 and aggravated by subsequent immobilization.48 Hence, current recommendations support that rehabilitation after ACL reconstruction should be initiated as early as possible.17 Pain, swelling, joint stiffness, patient apprehension and the period necessary to graft healing are crucial factors that may limit the performance of dynamic exercises at the initial stages of rehabilitation; then, voluntary isometric exercises and neuromuscular electrical stimulation are frequently employed during this stage.49 Heretofore, there is no consensus about the appropriate time when dynamic exercises must be initiated within the ACL rehabilitation programs. Closed kinetic chain exercises are traditionally implemented prior to open kinetic chain exercises under the statement that the former reduces shear and acceleration forces within the joint, develops dynamic joint stability and stimulates proprioceptors.50 Open kinetic chain exercises have been started from two32 to 1251 weeks after surgery, always in a restricted range of motion (as performed in the current study) to reduce risk of increased anterior knee laxity because ACL peak loading occurs at lower knee flexion angles.52 The current knowledge on this issue supports no difference in knee laxity with early or late introduction of open kinetic chain exercises in the ACL reconstruction population.53 We did not have an arthrometer to quantify knee laxity in the current study, but all volunteers were followed by experience physicians from the ACL reconstruction until return to sport and no signs of knee instability was observed.
The resistant torque throughout the range of motion is a basic difference between the isokinetic exercise and the constant external load exercise.54 The isokinetic dynamometer enables the exercise to be performed at maximal strength levels exerted by the individual at each articular angle.31 Once individuals determine their own exercise intensity through the voluntary muscular torque exerted over the dynamometer, isokinetic exercise offers greater safety to patients when compared to exercise with constant external load that may sometimes exceed the patient’s tolerance. Moreover, while the progression of exercise intensity throughout the training program in the extension chair is dependent on load adjustment by the therapist, the adjustment of exercise intensity under isokinetic conditions occurs concomitantly with the increase in the patient's capacity to produce force. The abovementioned factors may explain, at least in part, the larger effects found for IG compared to CG in the current study.
Given the association between quadriceps muscle weakness and ACL re-rupture,15 as well as its detrimental effect on functional performance and return to sport,13,14 the optimization of muscle mass recovery and strengthening of athletes trained under isokinetic conditions has a pivotal clinical impact. A better muscular condition usually allows early introduction of proprioceptive exercises, running, plyometrics, and specific sport drills, which are necessary steps to transit towards sports practice. However, our findings did not support consistently a greater functional performance of patients rehabilitated with isokinetic exercise compared to those who used the extensor chair. In other words, the IG higher gains in muscle mass and strength were not transferred to the patients’ functional performance, which highlights the role of functional exercises after ACL reconstruction.
Following the post-eccentric training evaluations, participants in both groups continued their rehabilitation programs with the physical therapist in the clinical setting and without follow-up by researchers. This point might be cited as a limitation of our study, since the subsequent evaluations (e.g. 6 months after surgery) could show the impact of earlier strengthening caused by isokinetic eccentric training over the rehabilitation process. In addition, we encourage future studies with clinical bias to include ‘return to sport’ as an outcome measure, as well as to assess anterior knee laxity (specially at long-term) to further verify the safety of early introduction of open kinetic chain exercises after ACL reconstruction. Lastly, it is notable the occurrence of no adverse effects and that all participants were capable to perform the proposed interventions. This suggests the safety of such training regimes (when performed as reported here) and encourages researchers to develop new studies as well as physical therapists to adopt eccentric training (either with constant load or with isokinetic devices) in their rehabilitation programs for patients undergoing ACL reconstruction.
ConclusionOur results support the use of open kinetic chain eccentric training as a safe and effective strategy to the quadriceps muscle rehabilitation after ACL reconstruction. Isokinetic eccentric training promoted greater responses than conventional eccentric training on quadriceps muscle mass and strength of recreational athletes undergoing ACL reconstruction.
Conflicts of interestThe authors declare no conflicts of interest.
Registered at www.clinicaltrials.gov: NCT02961543 (https://clinicaltrials.gov/ct2/show/NCT029615430).