A mixed methods study which aimed to evaluate the influence of Good Life with osteoArthritis Denmark (GLA:D®) on physical activity participation, including perceived capability, barriers, and facilitators in people with knee osteoarthritis.
ObjectiveQuantify changes in physical activity participation at 3- and 12-months for people with knee osteoarthritis who participated in an education and exercise-therapy program (GLA:D®).
MethodsA mixed-methods study involving 44 participants with knee osteoarthritis who completed GLA:D®. Guided by the Theoretical Domains Framework, 19 were interviewed, with transcripts analysed using reflexive thematic analysis. University of California Los Angeles physical activity scores were dichotomised as ‘more’ (≥7) or ‘less’ active (≤6), and compared between baseline and 3- and 12-months using McNemar's test. Motivation and confidence to exercise (0–10 scale); fear of knee joint damage with exercise (yes/no); and Knee Osteoarthritis Outcome Scores (KOOS) were evaluated.
ResultsFour overarching themes were identified: prior to GLA:D® 1) fear of knee joint damage, and scarcity of exercise and physical activity information prior to GLA:D®; and following GLA:D® 2) varied exercise-therapy and physical activity participation; 3) facilitators including reduced fear of knee damage, increased confidence, routine, strategies, and support; and 4) ongoing barriers including persistent knee pain, comorbidities, cost, and lack of opportunity and motivation. There was no difference in the proportion of ‘more’ active participants between baseline (41%) and at 3-months (37%, p = 0.774) or 12-months (35%, p = 0.375). The proportion with fear of damage reduced from baseline (50%) to 3-months (5%) and 12-months (21%). Self-reported motivation (9.1/10) and confidence (9.1/10) to exercise at 3-months were high, and all KOOS subscales improved from baseline to 3-months (effect sizes = 0.41–0.58) and 12-months (effect sizes = 0.29–0.66).
ConclusionVaried and often inadequate physical activity participation following GLA:D® indicates more targeted interventions to address ongoing barriers may be required.
Knee osteoarthritis negatively impacts quality of life (QoL),1 community and social participation,2 and occupational capacity.3 Just 13%4 of people with knee osteoarthritis are estimated to meet the physical activity guidelines,5 increasing their risk of comorbidities.6,7 Therefore, increasing physical activity is important for people with knee osteoarthritis due to their increased risk of comorbidities and low levels of physical activity.8 Major international guidelines consistently recommend exercise-therapy, education, and weight management when needed as first-line treatment for knee osteoarthritis.9-11 Exercise-therapy and education are safe and effectively improve knee pain, physical function, and QoL.12-14 However, findings related to changes in physical activity following exercise-therapy in controlled clinical trials are mixed.8 While exercise-therapy programs focused on walking or other aerobic exercise4,15-17 may increase physical activity compared to control interventions, resistance-training alone does not seem to have the same effect.18-20 Additionally, exercise-therapy may not alter physical activity participation in the medium- (6–12 months) or long-term (>12-months) compared to control interventions.18,19,21-23 When education focused on pain coping skills is combined with resistance-training, it provides moderate increases to physical activity in the medium-term compared to exercise-therapy alone.8,18,19
The Good Life with osteoArthritis from Denmark (GLA:D®) is an education and exercise-therapy program developed for people with knee or hip osteoarthritis.24,25 It includes education about the importance of physical activity to osteoarthritis management and general health, and is now implemented in at least seven countries, including Australia.26 Outcomes reported at 3- and 12-months include improved pain, joint- and health-related QoL, and functional capacity in people with knee osteoarthritis.25,27-29 Evaluation of GLA:D® in Denmark indicates that the program may slightly increase the proportion of people who regularly report being more physically active at 3-months, but may have limited influence at 12-months (odds ratio 1.18 and 1.10 respectively, compared to baseline).27
Barriers to physical activity participation for people with knee osteoarthritis include lack of knowledge about benefits, fear of pain and damage with exercise, beliefs and attitudes towards physical activity, environmental constraints, and social influences.30,31 Some barriers may be addressed through education and exercise-therapy provided in programs such as GLA:D®. However, beyond initial quantitative data provided by an initial program evaluation in Denmark, the influence of GLA:D® on physical activity participation has not been explored with qualitative methods. Also, it is not known how capable and motivated participants are to increase their physical activity following GLA:D®. We believe this study will identify important participant perspectives about why their physical activity did or didn't change following a structured education and exercise-therapy program like GLA:D®.
For people with knee osteoarthritis who participated in an education and exercise-therapy program, (GLA:D®), our aim was to use mixed methods to quantify changes in physical activity participation at 3- and 12-months. Additionally, we aimed to explore their perceived capability (motivation, confidence, fear of damage), barriers, and facilitators to increasing their physical activity at 3-months. We aimed to use knee-related patient reported outcome measures (PROMs) for our cohort to compare our findings with the overall GLA:D® population.
MethodsDesignWe used a concurrent triangulation design, whereby, separate but complementary qualitative and quantitative methods were used concurrently to collect data, and both contributed to the interpretation of findings. Reporting was guided by Good Reporting of A Mixed Methods Study checklist (GRAMMS)32 and the consolidated criterion for reporting qualitative research checklist (COREQ).33 GLA:D® provides two group education sessions, and 12 supervised group exercise-therapy sessions involving neuromuscular, functional, and resistance-training exercises.28 Education delivered over two sessions, focuses on osteoarthritis, its treatment options, self-management, and exercise and physical activity.28 Further details about the program can be found in the original Danish,27 and subsequent Australian,28 evaluations. Ethics approval for this study was provided by La Trobe University's Human Ethics Research Committee (#HEC18500). All participants provided written informed consent.
SettingWe recruited participants from an existing prospective non-inferiority randomised controlled trial comparing GLA:D® delivered in person or via telehealth (ACTRN12619000235101), as a supplementary study. For our quantitative analysis, data were pooled from both groups to create a prospective cohort study design. We invited 19 participants to interview sequentially from both arms, via email before attending their 3-month follow-up assessment for the existing trial (Supplementary material 1). Following qualitative interviews, quantitative data were included for the full set of recruited participants from the main trial (n = 44).
ParticipantsKnee osteoarthritis clinical diagnosis was guided by NICE guidelines.10 We included participants if they: i) were aged >40 years, ii) had activity-related knee pain, and iii) had morning stiffness of the knee which lasts less than 30-minutes or no knee stiffness. We selected participants for this secondary analysis consecutively via convenience sampling at the conclusion of the education and exercise-therapy intervention.
QualitativeA descriptive phenomenology approach was used, whereby semi-structured interviews explored perspectives of people with knee osteoarthritis completing GLA:D® in Australia regarding physical activity participation including perceived capability, barriers, and facilitators. Interviews and qualitative data analysis were led by a female physical therapist (ECB), who was a PhD candidate with previous qualitative research experience34 and three years clinical experience at the time. ECB was supported by three experienced qualitative researchers (CJB, PO, JAW).
Data collectionSemi-structured interviews were guided by a topic guide (Supplementary material 2), developed based on the theoretical domains framework,35 and informed by the clinical and research experience of physical therapists (ECB, CJB, JAW) and a psychologist (PO). Examples were placed as a semi-structured prompt for the interviewer and were offered when participants could not come up with their own examples. This was done so that if participants couldn't think of an example, they may be prompted and able to expand or report that something was not relevant for them. Questions were not pilot tested prior to the first interview. Questions explored participant physical activity participation before and after GLA:D®; perceived capability, confidence, and motivation to participate in physical activity; and barriers and facilitators to physical activity participation. All interviews were conducted individually, in person at a university or via Zoom, audio recorded with verbal consent, and conducted within one-week after the 3-month follow-up from commencement of GLA:D®. Interviews were intended to be conducted on the day of quantitative data collection, and thus designed to be 20- to 30-minutes in duration so they did not overburden participants. Seven of the participants were known to the interviewer (ECB) through her involvement as a treating clinician in the GLA:D® trial, and were instructed to answer all questions, regardless of the nature of responses being positive or negative. One repeat interview was conducted due to a recording failure. Interview field notes were not collected. Participants were recruited until authors (ECB and CJB) felt they were no longer identifying new information. Analysis took place in batches in line with 3-month assessments. Whether new information was identified was carefully considered after each interview. Interviews were transcribed verbatim by a third-party transcription service (Transcription Australia). Participants were provided with a copy of their transcripts and the opportunity to correct any inaccuracies and provide further comments within a four-week period. Feedback was planned to be included in the analysis phase. No participants responded with specific feedback.
Data analysisReflexive thematic analysis36 was supported by NVivo software (QSR International Pty Ltd, Melbourne, Australia). Analysis commenced with a close review of each transcript by two researchers (ECB, CJB) to gain an overall picture of the data and a meeting to discuss potential codes. To establish a thematic framework, one researcher assigned codes to each key issue identified, with similar codes being grouped to form subthemes, and subthemes being grouped to form overarching themes. All transcripts contributed to the thematic framework, and themes identified were not predetermined. A random sample of 50% of interviews were coded independently by a third researcher (PO) and compared with the initial analysis. Identified themes were discussed and refined between researchers (ECB, PO, JAW, CJB) at four meetings, until consensus was reached.
QuantitativeData collectionExcept for motivation and confidence ratings collected during interviews, quantitative data were collected via the secure online Research Electronic Data Capture (REDCap) system hosted by La Trobe University. Data were collected at baseline and 3-months on site at La Trobe University by a blinded assessor. An automatic survey was emailed to participants at 12-months, with email reminders every three days for two-weeks then up to three phone calls made to non-respondents.
Physical activity was assessed using the University of California, Los Angeles (UCLA) physical activity scale (1–10), which is recommended for observing physical activity participation of osteoarthritis populations (Supplementary material 3).37 The UCLA has established construct validity and reliability.37 Fear of physical activity and exercise was measured by participants answering ‘yes’ or ‘no’ to the question “Are you afraid that your joints will be damaged from physical activity and exercise”. Adherence to GLA:D® exercise-therapy classes, GLA:D® education sessions and home exercise-therapy sessions were also reported by participants at 3-months.
The Knee injury and Osteoarthritis Outcome Score (KOOS) was used to measure sport and recreation participation, pain, symptoms, function, and knee-related QoL (0–100). Higher scores indicate a more positive outcome.38 Each subscale of KOOS has high test-retest reliability.39
During interviews, participants were also asked to provide a numerical value from 0 to 10 (0 being not at all and 10 being maximal) to rate their motivation and confidence (Supplementary material 2).
Data analysisStatistical analysis was performed using SPSS version 28 (SPSS, Inc, Chicago, IL, USA). Minimal important change has not been defined for the UCLA physical activity scale. Median (interquartile range [IQR]) were calculated for the UCLA physical activity scale. We also dichotomised UCLA data as participants being (i) ‘more’ (≥7= “Regularly participates in active events, such as bicycling” or higher) or (ii) ‘less’ active (≤6= “Regularly participates in moderate activities, such as swimming and unlimited housework or shopping” or lower) (Supplementary material 3). Changes in the number of participants who were physically more active from baseline to 3-months and baseline to 12-months were determined using McNemar's test. The proportion of participants who answered “yes” to fear of damage with physical activity and exercise were presented at baseline and 3- and 12-months. Changes in the number of participants who reported fear from baseline to 3-months and baseline to 12-months were determined using McNemar's test. Mean (standard deviation (SD), range) were calculated for confidence and motivation at 3-months.
Independent one-way ANOVAs were performed to evaluate the changes following GLA:D® on all KOOS subscales. Significance level set at p < 0.05, and Bonferroni's post-hoc test was applied for multiple pairwise comparisons when appropriate. Effect sizes were calculated using Cohen's d, and classified as negligible (<0.10), small (≥0.10), moderate (≥0.30), or large (≥0.50).40 The minimally important change values set for KOOS subscales were 20 for sport and recreation,41 13 for pain,41 16 for symptoms,41 15 for function,41 and 15 for QoL.42 Comparisons of 3- and 12-month outcomes for each KOOS subscale were made with normative values from people without knee injury of similar age (55–74 years).43
To aid clinical interpretation, we compared our KOOS findings at 3- and 12-months to normative values43 to determine whether our participants outcomes were within normal limits, defined as within one standard deviation (SD) from the mean of normative values. Normative means (SDs) used were 67 (33) for sport & recreation, 83 (21) for pain, 83 (21) for symptoms, 82 (22) for function, and 78 (28) for QoL.43
Data synthesisTriangulation and synthesis of the qualitative and quantitative findings was facilitated by presenting a side-by-side table with an additional column added covering implications for practice generated by the research team and informed by current literature and practice. Findings were considered convergent where qualitative findings aligned with relevant quantitative data. Findings were considered divergent if qualitative findings conflicted with relevant quantitative data.
ResultsNineteen participants were interviewed (in-person=16, Zoom=3) at 3-months following commencement of GLA:D® between September 2019 and January 2020. No invited participants refused participation. Demographics of included participants are provided in Table 1.
Demographics of included participants.
Data are mean (standard deviation) and frequency (proportion). BMI, body mass index; kg, kilogram; m, metres; GLA:D®, Good Life with osteoarthritis.
Interviews lasted between 11 and 40 min (mean= 24 min), no participants made changes to their transcripts. Four overarching themes were identified (Tables 2 - 4): 1) fear of knee joint damage, and scarcity of exercise and physical activity information for osteoarthritis prior to GLA:D®; 2) varied exercise-therapy and physical activity participation following GLA:D®; 3) facilitators following GLA:D® included reduced fear of knee damage, increased confidence, routine, strategies, and support; and 4) barriers following GLA:D® included persistent knee pain, comorbidities, cost, and lack of opportunity and motivation. A qualitative matrix with all overarching themes, subthemes, and quotes related to each subtheme is provided in Supplementary material 4, with key illustrative quotes provided in Tables 2-4.
Theme extracted from qualitative interviews about participants’ views before GLA:D®.
Theme extracted about the influence of GLA:D® on physical activity.
Themes extracted relating to facilitators and barriers to physical activity participation following GLA:D®.
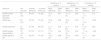
Quantitative data were collected for 44 participants at baseline, 43 at 3-months, and 40 at 12-months. There was no difference in the proportion of participants who were ‘more’ active (UCLA score of at least 7) between baseline (41%), 3-months (37%), and 12-months (35%) (McNemar's test 3-months p = 0.774; 12-months p = 0.375). Median [IQR] for UCLA at baseline and 3- and 12-months were 6 [5 to 7], 6 [5 to 6] and 5 [3 to 6], respectively. Detailed results from the UCLA scale are shown in Fig. 1. The proportion of participants reporting fear of knee damage from physical activity and exercise at baseline and 3- and 12-months was 50% (22), 5% (2), and 22.5% (9), respectively (McNemar's test 3-months p=<0.001; 12-months p = 0.013). Mean (SD, range) for confidence and motivation to participate in regular physical activities among interview participants (n = 19) at 3-months were 9.1 (1, 6 to 10) and 9.1 (1, 6 to 10), respectively. Table 5 contains one-way ANOVA results for all subscales of the KOOS.
Physical activity for baseline and 3- and 12-months. Figure legend: UCLA= University of Los Angeles Physical Activity Scale, 1=“Wholly inactive: dependent on others; cannot leave residence”, 2=”Mostly inactive: restricted to minimal activities of daily living”, 3="Sometimes participate in mild activities", 4="Regularly participate in mild activities, such as walking, limited housework, and limited shopping", 5="Sometimes participate in moderate activities", 6="Regularly participate in moderate activities, such as swimming and unlimited housework or shopping", 7="Regularly participate in active events, such as bicycling", 8="Regularly participate in very active events, such as bowling or golf", 9="Sometimes participate in impact sports" 10="Regularly participate in impact sports such as jogging, tennis, skiing, acrobatics, ballet, heavy labour, or back packing", solid black line between green and yellow indicates the distinction between ‘more’ and ‘less’ active.
ANOVA for KOOS.
| Baseline vs. 3-months | Baseline vs. 12-months | 3-months vs. 12-months | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Outcome | Pre-GLA:D® | 3-month follow-up | 12-month follow-up | Mean difference | Effect size | Mean difference | Effect size | Mean difference | Effect size |
| KOOS function sport and recreation | 42 (22) | 56 (24) | 53 (26) | 14 (1, 27) | 0.41 | 10 (−3, 23) | 0.29 | −4 (−17, 9) | 0.12 |
| KOOS pain | 63 (16) | 76 (15) | 75 (18) | 13 (4, 21) | 0.58 | 12 (3, 20) | 0.53 | −1 (−10, 8) | −0.04 |
| KOOS symptoms | 57 (20) | 67 (16) | 68 (18) | 11 (1, 19) | 0.44 | 11 (1, 20) | 0.43 | 0 (−9, 10) | 0.00 |
| KOOS function daily activities | 70 (18) | 81 (13) | 81 (17) | 11 (3, 20) | 0.49 | 11 (2, 19) | 0.48 | −1 (−9, 8) | −0.04 |
| KOOS quality of life | 43 (15) | 56 (15) | 57 (18) | 13 (5, 22) | 0.58 | 15* (6, 23) | 0.66 | 1 (−7, 10) | 0.04 |
Data are mean (standard deviation) and mean difference (95 % confidence interval). GLA:D®, Good Life with osteoArthritis from Denmark; KOOS, Knee injury and Osteoarthritis Outcome Score.
Bold values denote p < 0.05.
All KOOS subscales improved from baseline to 3- and 12-months (Table 5). All KOOS subscales at 3- and 12-months were within normal limits (i.e. within one SD of normative means) (Supplementary material 5). All KOOS subscales except KOOS symptoms (3-months) and KOOS QoL (3- and 12-months) exceeded a value within one minimal important change below the normative mean (Supplementary material 5).
One participant (5%) underwent total knee replacement (TKR) 10-months following commencing GLA:D®. Their UCLA physical activity scale score (3: ‘sometimes participates in mild activities’) remained unchanged at 3- and 12-month follow-ups.
Table 6 contains a synthesis of qualitative and quantitative results, including implications for practice.
Synthesis of qualitative and quantitative data.
Legend: GLA:D®= Good Life with osteoArthritis from Denmark, KOOS = Knee injury and Osteoarthritis Outcome Score, QoL= quality of life, YMCA= Young Men's Christian Association, Theme 1= fear of knee joint damage, and scarcity exercise and physical activity information for osteoarthritis prior to GLA:D®, Theme 2= varied exercise-therapy and physical activity participation following GLA:D®, Theme 3= physical activity participation facilitators following GLA:D® included reduced fear of knee damage, increased confidence, routine, strategies and support, Theme 4= physical activity participation barriers following GLA:D® included persistent knee pain, comorbidities, cost, lack of opportunity, and lack of motivation, MIC= minimal important change.
Our mixed methods study provides unique insight into the influence of group education and exercise-therapy programs such as GLA:D® on physical activity participation in people with knee osteoarthritis. Convergent qualitative and quantitative findings indicate a lack of clear or consistent increases to physical activity participation among our cohort. This finding is consistent with previous evaluation of GLA:D® in Denmark over 12-months,27 and most other clinical trials evaluating the effects of exercise-therapy on physical activity, indicating a need for additional interventions beyond GLA:D® to increase physical activity participation in the longer term.8
Following GLA:D® in this study, participants reported greater confidence to engage in exercise and physical activity, alongside improved knowledge about how to manage their knee condition, along with the benefits and safety of exercise. Convergent findings also indicated that fear of knee pain and damage during physical activity participation, which is common in people with knee osteoarthritis,44 was also reduced following GLA:D®. The potential importance of addressing this psychological barrier to physical activity participation is highlighted by the association between lower fear of movement with more steps per day in people with knee osteoarthritis.45 However, lack of consistent increases to physical activity participation in this study despite apparent improvements in knee joint confidence suggests that additional barriers need to be considered and addressed.
Our qualitative findings provide key insights which may help explain the absence of clear or consistent increases to physical activity participation in the longer term following exercise-therapy.8 Firstly, some participants continued to describe lack of motivation as a barrier to physical activity participation following GLA:D®, despite quantitative findings indicating that participants’ motivation was typically high. The divergence between qualitative and quantitative findings may suggest social desirability bias,46 where participants feel that they should be motivated to be physically active following GLA:D®, due to the education they received, rather than actual motivation to be more physically active. Considering this, careful subjective assessment to identify true motivation to increase physical activity participation is encouraged. For those lacking motivation to increase physical activity participation, additional evidence-based behaviour change interventions such as motivational interviewing may help.47,48 Future research to explore this is encouraged.
Beyond motivation, we identified other key ongoing intrinsic barriers to physical activity participation following GLA:D®, including persistent knee pain and comorbidities. Despite all KOOS subscales improving to within normal limits at 3-months, only knee-related QoL was associated with a minimally important change. Medium to large effect increases were achieved by all KOOS subscales from baseline to both 3- and 12-months (except sport and recreation from baseline to 12-months). Additionally our participants remained more than one minimal important change score below aged matched norms for KOOS symptoms (67 vs 83) and KOOS QoL (56 vs 74).43 This suggests that although knee-related health improved following GLA:D®, ongoing difficulties with knee-related symptoms and QoL remained, meaning they were “better” but not necessarily “good”.49 Awareness and consideration of comorbidities such as other medical conditions, additional musculoskeletal conditions, or persistent knee pain are important for clinicians wanting to support people with knee osteoarthritis to increase physical activity participation.50,51
Key ongoing extrinsic barriers to physical activity participation identified following GLA:D® included out-of-pocket costs associated with physical activity programs, safety and physical environment, and inadequate social opportunity. Therefore, publicly funded physical activity programs, community supported activities (such as walking groups), and subsidised gymnasium memberships are encouraged to provide opportunity to participate in physical activity. Importantly, people with knee osteoarthritis may want health professionals to educate them about whether they can participate in more physical activity and where they can join others to participate in exercise following supervised exercise-therapy programs.52 This highlights an opportunity for physical therapists and other health professionals more broadly, to improve their knowledge of, and referral practices to, existing community programs such as walking or running groups (e.g. Parkrun),53 local exercise facilities or community exercise groups. Facilitators identified in this study also warrant consideration. Our participants reported that forming a routine for physical activity may help to keep them on track. Additionally, strategies including booster sessions54 and technology55 including telehealth or activity tracking devices, which can increase adherence to exercise-therapy in knee osteoarthritis were also considered by our participants as potential facilitators to increase physical activity participation.
Prior to GLA:D®, interactions with health professionals were reported to be inconsistent, and often lacked detailed exercise-therapy or physical activity prescription, with seemingly more emphasis on a potential need for surgery. This finding may reflect the common impairment discourse about osteoarthritis, leading people to believe their knee will eventually wear out and that surgery is inevitable.51 Some participants reported difficulty recalling specific physical activity or exercise-therapy information from online searching, while having better recall of surgical information, consistent with reports that only 31% of the commonly accessed knee osteoarthritis websites contain accurate and clear information about exercise-therapy and just 20% for physical activity.56 Collectively, these findings highlight an opportunity for health professionals to discuss and promote physical activity as part of regular practice,57 along with development and dissemination of more online resources promoting the safety and benefits of exercise for knee osteoarthritis.
Our study's findings should be considered in the context of its limitations. Participants were willing to participate in a clinical trial of education and exercise-therapy for their knee osteoarthritis, without any ‘out of pocket’ expenses. Therefore, qualitative findings may not reflect the attitudes of all people with knee osteoarthritis regarding willingness to participate in exercise-therapy and physical activity. Seven interview participants were known to the interviewer (ECB), which may have biased accounts of their experiences with GLA:D®. However, qualitative and quantitative findings mostly converged suggesting this is unlikely to have occurred. The average length of interviews was slightly shorter than some recommendations,58 which is a result of methodological design to not overburden participants. However, our qualitative data set was rich, identifying 4 themes and 14 subthemes to further strengthen our quantitative data. The interviewer did not record notes during interviews, which may mean that reactions were not recorded, however, audio files were able to be used for changes in tone, laughs, etc.
The UCLA physical activity scale has good construct validity and has been widely used in osteoarthritis.59,60 A limitation of this scale is that it combines one item to measure intensity, frequency, difficulty, and duration, potentially limiting sensitivity to change.61,62 Additionally, it is a self-reported measure, creating risk for recall and responder bias. However, our qualitative and quantitative findings related to physical activity participation generally converged, increasing the trustworthiness of quantitative findings. We used a cut-off to determine ‘more’ and ‘less’ active based on the UCLA deemed most likely to correlate with participants who meet physical activity guidelines. However, this cut off is arbitrary, and other cut points may change our findings. Future studies should look to measure physical activity changes following GLA:D® using activity monitoring devices. Some outcome measures used in this study are not well validated in this population, including fear, confidence, and motivation. However, they provide additional information related to barriers and facilitators of physical activity.
ConclusionEducation and exercise-therapy programs such as GLA:D® may address several intrinsic barriers to physical activity, including fear of damage, and knee-related symptoms and confidence. However, despite apparent improvements in knee joint confidence, physical activity participation does not appear to clearly, or consistently, increase at 3- or 12-months following GLA:D®. Further research should evaluate additional interventions beyond commonly implemented education and exercise-therapy programs to address ongoing barriers to increasing physical activity participation in people with knee osteoarthritis.
Author contributionsConceptualisation: ECB, PO, JAW, KMC, CJB
Participant recruitment: CJB, ZP, ECB, MFP
Project administration: All
Interviews: ECB
Qualitative analysis: ECB, PO, JAW, CJB
Quantitative analysis: ECB, MFP, CJB
First draft: ECB, MFP, PO, JAW, CJB
Final draft: All