Physical health is an important factor for what is considered successful aging. Using valid and reproducible tools to classify PH of older adults may help to develop appropriate rehabilitation protocols for this population.
ObjectiveTo evaluate the convergent validity and reproducibility of the International Classification of Functioning, Disability and Health (ICF) core set to classify the physical health of older adults.
MethodsA total of 101 older adults were evaluated for handgrip strength, physical performance (Short Physical Performance Battery), and physical activity level (International Physical Activity Questionnaire). Physical health was classified with the ICF core set (14 categories of body functions, 4 of body structures, 9 of activity and participation, and 3 environmental factors) and an impairment index was calculated for each component.
ResultsHigher levels of physical activity were associated to lower impairment index in the body function and activity and participation components, but was not associated to environmental factors. Better physical performance and handgrip strength were also related to lower impairment index in all components. The Intraclass Correlation Coefficient analysis indicated good reproducibility for body function, body structure, the capacity component of the activity and participation, and for two environmental factors (use of medications and assistive devices), but moderate reproducibility for the performance component of activity and participation, and poor reproducibility for the environmental factor related to access to health services.
ConclusionThe ICF core set for the physical health of older adults is a valid and reproducible tool and can be used in clinical practice and research.
The aging process is characterized by being multifactorial which is associated with increased vulnerability of the body to stressors and with an overload of homeostatic control mechanisms. Hence, older adults may develop functional disability and chronic conditions.1 The maintenance of physical health (PH) is an important factor for what is considered successful aging.2 In particular, PH has been associated with functional independence, and is commonly assessed by functional measures such as the ability to generate muscle strength, to move around, and to stay active, which are not only closely related to the individual’s own factors, but also to the contextual factors in which they live and function.3 When PH is altered, there is increased vulnerability of older adults to adverse events such as higher morbidity, falls, and death.4
Considering the importance of PH as a predictor of adverse outcomes among older adults, it is recommended to use tools which help identify physical impairments and functional disabilities with the intent to develop appropriate rehabilitation protocols for this population.5 From this perspective, the International Classification of Functioning, Disability and Health (ICF) appears as a comprehensive classification resource which considers the health situation of people in a multidimensional manner based on a biopsychosocial and holistic model.6 It has the advantage of providing a common language for describing health-related states, which therefore enables a comparison of different populations and assists in communication and exchange of information about individuals all around the world.6
The World Health Organization encourages the development of core sets to increase the usefulness of the ICF.7 Core sets are composed of lists of ICF categories which are relevant for specific conditions and make it practical to be used in clinical practice and research.5 Although several instruments in gerontology provide important information about different domains of PH, there is a lack of unified instruments which are able to provide crucial information and can be applied in diverse sociocultural contexts. With this in mind, Ruaro et al8 developed a core set designed to gather the important components for PH of community-dwelling older adults into a single instrument. This core set qualifies the PH of older adults using an overall approach which includes biological factors, activities, social participation, and environmental factors in an instrument with high internal consistency.9 However, other measurement properties, such as its validity and reproducibility, still need to be determined before it can be implemented in clinical practice and research.
Thus, the aim of the present study was to evaluate the convergent validity and test-retest reproducibility of the ICF core set for the PH of older adults. The measures used to determine convergent validity included muscle strength, functional performance, and physical activity. These measures can predict important adverse outcomes for other adults such as institutionalization, mortality, and disability, and are associated with physiological functions that frequently decline as people age.10
MethodsStudy design and locationThis study on measurement properties was conducted in the city of Santa Cruz in the state of Rio Grande do Norte (RN), Brazil. This study was approved by the Ethics Committee of the Faculty of Health Sciences of Trairi, Universidade Federal do Rio Grande do Norte (FACISA/UFRN), Santa Cruz, RN, Brazil (approval number 2.569.124).
ParticipantsThe study sample was recruited by convenience sampling and was stratified by neighborhoods to allow the inclusion of older adults from different living environments. Recruiters performed home visits to contact older adults from all neighborhoods based on a list of people aged 60 years or over who had participated in previous research projects at the FACISA/UFRN campus. Primary healthcare units from each neighborhood were also contacted for potential participants. A sample size of 100 older adults was considered sufficient to evaluate the measurement properties of an instrument.11,12 Because the urban area of Santa Cruz has five neighborhoods, we aimed to recruit a sample of at least 20 participants from each of them.
We included community-dwelling older adults aged 60 years or over, irrespective of physical complaints or comorbidities. Participants presenting with cognitive decline or who did not complete all assessment procedures were excluded from the study. A score of less than 22 points on the Leganés Cognitive Test (LCT) was considered an indicative of cognitive decline.13,14
ProceduresEligible older adults were initially informed about the research, then invited to participate in the study. Those who agreed to participate and signed the consent form were evaluated on the day and time scheduled at the initial contact by physical therapists and physical therapy students previously trained for this evaluation. The older adults were evaluated at their homes using an electronic questionnaire specifically developed to collect data for this study. The electronic questionnaire were completed on a laptop.
An evaluation form containing questions related to: age; sex; years of study (i.e. categorized as “up to 4 years” or “more than 4 years”); and monthly family income (i.e. recorded as number of minimum wage [R$954.00/month] in the year of the study and categorized as “less than 3 minimum wages” or “3 or more minimum wages”) was initially completed.15–17 Then, the anthropometric measures of weight and height were taken to calculate the body mass index (BMI), which was categorized as: BMI < 23 kg/m² = underweight; 23 kg/m² ≤ BMI < 28 kg/m² = normal; 28 kg/m² ≤ BMI < 30 kg/m² = overweight; BMI ≥ 30 kg/m² = obese.18
The long version of the International Physical Activity Questionnaire (IPAQ) was used to assess the level of physical activity at work, means of transportation, in domestic tasks, and in exercise and leisure.19 The weekly frequency and duration of each activity in a usual week were used to determine the metabolic expenditure in METs/min/week.19 Subsequently, the physical activity level was classified from the total energy expenditure as: low, moderate, or high, according to the guidelines described in the IPAQ guidelines.20
The older adults were assessed for lower limbs physical performance using the Short Physical Performance Battery (SPPB). The SPPB consists of three tests which assess static balance in three situations (joined feet, semi-tandem, and tandem), usual walking speed (for a distance of 3 m), and lower limbs muscle strength (the time taken to get up and sit down five times in a row at the fastest possible speed without using the hands).21,22 Each of these tests is scored on a scale from 0 to 4 points. The final score is obtained from the sum of the three tests, ranging from 0 to 12, with higher values indicating better performance.21 A score of 8 points or greater was used to identify those with good physical performance.23
A Saehan® SH5001 handgrip hydraulic dynamometer was used to assess handgrip strength. The participant was asked to perform a maximum isometric force with their dominant limb for 5 s.24 Three measurements were performed with a 1-minute rest interval between them.25 The participant remained seated during the test with their feet flat on the floor, shoulder adducted and in neutral rotation, elbow at 90° of flexion, forearm and wrist in neutral position.25 The handgrip dynamometer was used in position 3 for men, and in position 2 for women.25 We considered the average of the 3 measurements for the analysis.25
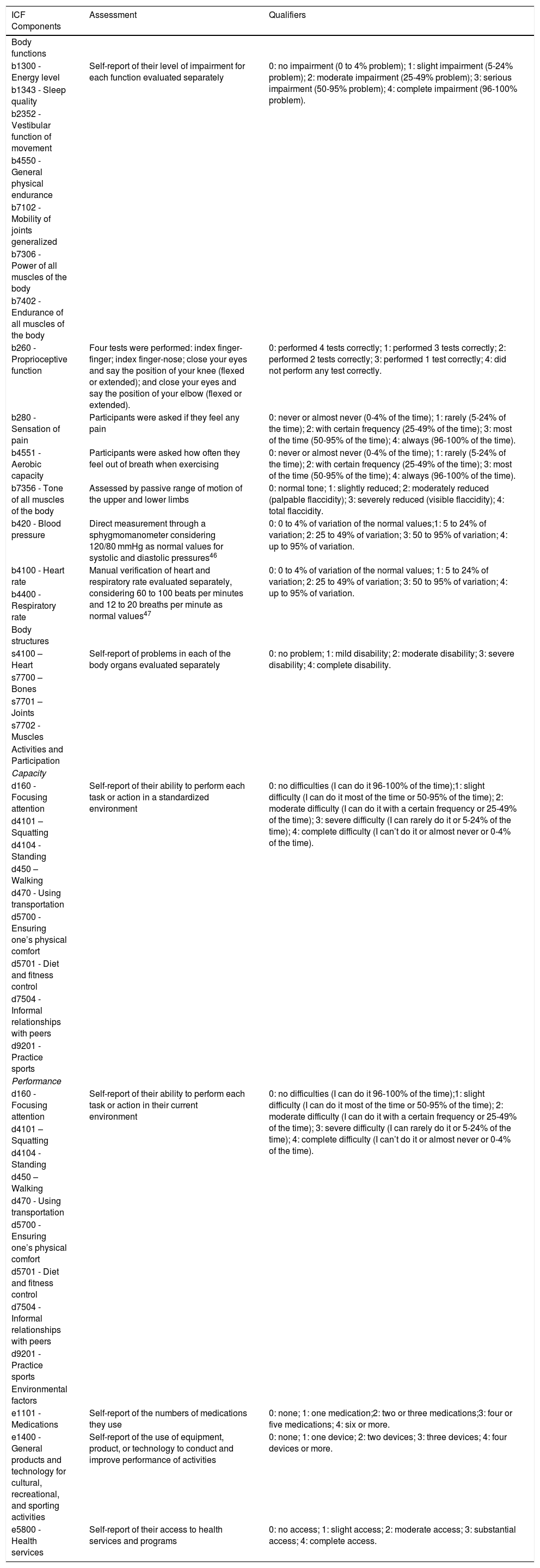
Finally, we applied the ICF core set for PH of older adults, with 30 categories divided into different components as follows: 14 for body functions, four for body structures, nine for activities and participation, and three related to environmental factors.9Table 1 describes each category as well as how they were assessed and qualifiers defined in this study.
Categories and definition of qualifiers of the ICF Core Set for the physical health of older adults.
| ICF Components | Assessment | Qualifiers |
|---|---|---|
| Body functions | ||
| b1300 - Energy level | Self-report of their level of impairment for each function evaluated separately | 0: no impairment (0 to 4% problem); 1: slight impairment (5-24% problem); 2: moderate impairment (25-49% problem); 3: serious impairment (50-95% problem); 4: complete impairment (96-100% problem). |
| b1343 - Sleep quality | ||
| b2352 - Vestibular function of movement | ||
| b4550 - General physical endurance | ||
| b7102 - Mobility of joints generalized | ||
| b7306 - Power of all muscles of the body | ||
| b7402 - Endurance of all muscles of the body | ||
| b260 - Proprioceptive function | Four tests were performed: index finger-finger; index finger-nose; close your eyes and say the position of your knee (flexed or extended); and close your eyes and say the position of your elbow (flexed or extended). | 0: performed 4 tests correctly; 1: performed 3 tests correctly; 2: performed 2 tests correctly; 3: performed 1 test correctly; 4: did not perform any test correctly. |
| b280 - Sensation of pain | Participants were asked if they feel any pain | 0: never or almost never (0-4% of the time); 1: rarely (5-24% of the time); 2: with certain frequency (25-49% of the time); 3: most of the time (50-95% of the time); 4: always (96-100% of the time). |
| b4551 - Aerobic capacity | Participants were asked how often they feel out of breath when exercising | 0: never or almost never (0-4% of the time); 1: rarely (5-24% of the time); 2: with certain frequency (25-49% of the time); 3: most of the time (50-95% of the time); 4: always (96-100% of the time). |
| b7356 - Tone of all muscles of the body | Assessed by passive range of motion of the upper and lower limbs | 0: normal tone; 1: slightly reduced; 2: moderately reduced (palpable flaccidity); 3: severely reduced (visible flaccidity); 4: total flaccidity. |
| b420 - Blood pressure | Direct measurement through a sphygmomanometer considering 120/80 mmHg as normal values for systolic and diastolic pressures46 | 0: 0 to 4% of variation of the normal values;1: 5 to 24% of variation; 2: 25 to 49% of variation; 3: 50 to 95% of variation; 4: up to 95% of variation. |
| b4100 - Heart rate | Manual verification of heart and respiratory rate evaluated separately, considering 60 to 100 beats per minutes and 12 to 20 breaths per minute as normal values47 | 0: 0 to 4% of variation of the normal values; 1: 5 to 24% of variation; 2: 25 to 49% of variation; 3: 50 to 95% of variation; 4: up to 95% of variation. |
| b4400 - Respiratory rate | ||
| Body structures | ||
| s4100 – Heart | Self-report of problems in each of the body organs evaluated separately | 0: no problem; 1: mild disability; 2: moderate disability; 3: severe disability; 4: complete disability. |
| s7700 – Bones | ||
| s7701 – Joints | ||
| s7702 - Muscles | ||
| Activities and Participation | ||
| Capacity | ||
| d160 - Focusing attention | Self-report of their ability to perform each task or action in a standardized environment | 0: no difficulties (I can do it 96-100% of the time);1: slight difficulty (I can do it most of the time or 50-95% of the time); 2: moderate difficulty (I can do it with a certain frequency or 25-49% of the time); 3: severe difficulty (I can rarely do it or 5-24% of the time); 4: complete difficulty (I can’t do it or almost never or 0-4% of the time). |
| d4101 – Squatting | ||
| d4104 - Standing | ||
| d450 – Walking | ||
| d470 - Using transportation | ||
| d5700 - Ensuring one’s physical comfort | ||
| d5701 - Diet and fitness control | ||
| d7504 - Informal relationships with peers | ||
| d9201 - Practice sports | ||
| Performance | ||
| d160 - Focusing attention | Self-report of their ability to perform each task or action in their current environment | 0: no difficulties (I can do it 96-100% of the time);1: slight difficulty (I can do it most of the time or 50-95% of the time); 2: moderate difficulty (I can do it with a certain frequency or 25-49% of the time); 3: severe difficulty (I can rarely do it or 5-24% of the time); 4: complete difficulty (I can’t do it or almost never or 0-4% of the time). |
| d4101 – Squatting | ||
| d4104 - Standing | ||
| d450 – Walking | ||
| d470 - Using transportation | ||
| d5700 - Ensuring one’s physical comfort | ||
| d5701 - Diet and fitness control | ||
| d7504 - Informal relationships with peers | ||
| d9201 - Practice sports | ||
| Environmental factors | ||
| e1101 - Medications | Self-report of the numbers of medications they use | 0: none; 1: one medication;2: two or three medications;3: four or five medications; 4: six or more. |
| e1400 - General products and technology for cultural, recreational, and sporting activities | Self-report of the use of equipment, product, or technology to conduct and improve performance of activities | 0: none; 1: one device; 2: two devices; 3: three devices; 4: four devices or more. |
| e5800 - Health services | Self-report of their access to health services and programs | 0: no access; 1: slight access; 2: moderate access; 3: substantial access; 4: complete access. |
ICF: International Classification of Functioning, Disability and Health.
Most categories were assessed by self-report of the older adult’s function and perception, with exception of category b260 (proprioceptive function), which was assessed with proprioceptive tests; category b7356 (tone of all muscles of the body) which was assessed by performing passive range of motion of the upper and lower limbs; category b420 (blood pressure) which was assessed using a sphygmomanometer; and categories b4100 (heart rate) and b4400(respiratory rate) which were assessed by palpation and visual inspection, respectively.
Moreover, we assessed two constructs for activity and participation; one related to performance, which describes what an individual does in their current environment; and one related to capacity, which describes an individual’s ability to execute a task or an action in a standardized environment.6
For the test-retest reproducibility, the core set was reassessed for all participants five to eight days after the first evaluation. This interval was established with the objective of minimizing the probability of relevant changes in the participants’ health condition, and considering that it would be unlikely that they would remember the answers given in the first assessment due to the number of questions contained in the core set.26
Impairment indexThe impairment index was initially calculated for each core set component to summarize the data and facilitate statistical analysis. The index was calculated individually considering the sum of the qualifiers for all categories of the component divided by the maximum possible score for that same component.27 The result was multiplied by 100 and then written as a percentage, where 0% represents no impairment of the component and 100% represents complete impairment.27 This index was not calculated for environmental factors because the categories can be classified as barriers or facilitators depending on the context. Thus, data on environmental factors were analyzed using the qualifier (0–4) assigned to each category, i.e. the qualifiers for the environmental factors e1101 and e1400 indicate the respective number of medications and assistive devices used by the participant. For the environmental factor e5800, the qualifier indicates the participant’s perception of access to health services, varying from no access (qualifier 0) to complete access (qualifier 4).
Statistical analysisData were analyzed using the Statistical Package for Social Sciences (SPSS) 20.0. Data normality was tested by the Kolmogorov-Smirnov test, which indicated a non-normal distribution of data. Therefore, median and interquartile range (i.e. 25th - 75th percentiles) were used as descriptive statistics to synthesize continuous data and frequency and proportion were used for categorical data. The association between the impairment rate and problems identified through the ICF core set and the other research instruments was assessed using the Kruskal-Wallis, Mann-Whitney, and Spearman correlation tests. We expected that participants with higher muscle strength, higher SPPB scores, and higher level of physical activity would have lower impairment index for body functions, body structures, and activity and participation, lower qualifier for medications and assistive devices, and higher qualifiers for the health services access category.
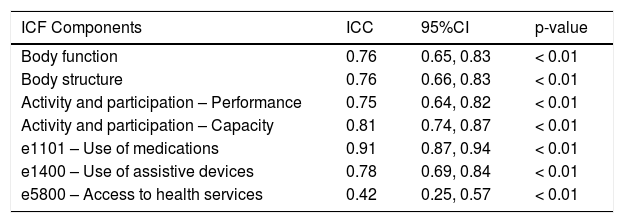
Reproducibility was assessed using the Intraclass Correlation Coefficient (ICC) (two-way mixed effects, absolute agreement, single measurement), which was interpreted as: poor reproducibility (ICC < 0.5); moderate reproducibility (ICC = 0.5−0.75); good reproducibility (ICC = 0.75−0.90); and excellent reproducibility (ICC = 0.90–1.00).28 A 5% alpha and 95% confidence interval (CI) were considered for statistical significance in all stages.
There was no missing data in this study, so data from all participants were included in the analyses.
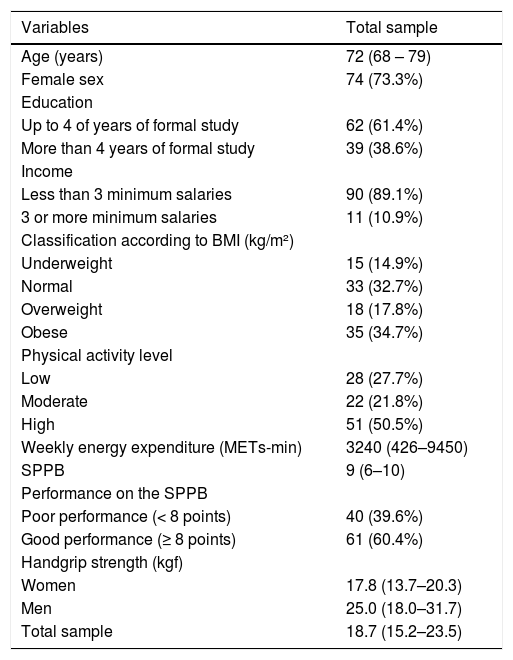
ResultsFrom March to August 2018, a total of 108 older adults were invited to participate in this study. Of these, 101 older adults were eligible and recruited for the study. We excluded six older adults due to cognitive decline and one older adult who failed to complete all assessment procedures. Table 2 presents the characteristics of the total sample. Most of the participants were women, had up to 4 years of education and income of less than 3 minimum monthly salaries. Most of them were overweight or obese, despite being classified as having a high level of physical activity (weekly median of 3240 METs-min). Satisfactory physical performance was also detected in the SPPB evaluation and median grip strength of 18.7 kgf for the total sample (17.8 kgf for women and 25.0 kgf for men).
Sample characterization (N = 101).
| Variables | Total sample |
|---|---|
| Age (years) | 72 (68 – 79) |
| Female sex | 74 (73.3%) |
| Education | |
| Up to 4 of years of formal study | 62 (61.4%) |
| More than 4 years of formal study | 39 (38.6%) |
| Income | |
| Less than 3 minimum salaries | 90 (89.1%) |
| 3 or more minimum salaries | 11 (10.9%) |
| Classification according to BMI (kg/m²) | |
| Underweight | 15 (14.9%) |
| Normal | 33 (32.7%) |
| Overweight | 18 (17.8%) |
| Obese | 35 (34.7%) |
| Physical activity level | |
| Low | 28 (27.7%) |
| Moderate | 22 (21.8%) |
| High | 51 (50.5%) |
| Weekly energy expenditure (METs-min) | 3240 (426–9450) |
| SPPB | 9 (6–10) |
| Performance on the SPPB | |
| Poor performance (< 8 points) | 40 (39.6%) |
| Good performance (≥ 8 points) | 61 (60.4%) |
| Handgrip strength (kgf) | |
| Women | 17.8 (13.7–20.3) |
| Men | 25.0 (18.0–31.7) |
| Total sample | 18.7 (15.2–23.5) |
Data are median (25th-75th percentiles) and frequency (proportion).
BMI: Body mass index.
SPPB: Short Physical Performance Battery.
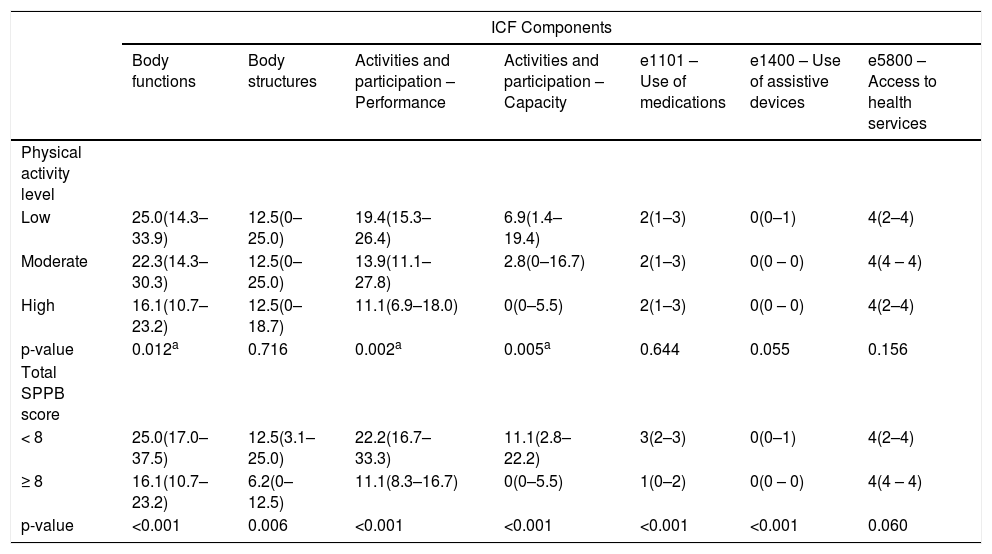
The relationship between the impairment index in the ICF core set components and the physical activity level and performance on the SPPB are presented in Table 3. More physically active participants presented lower levels of impairment in body functions and less difficulties to perform activities as evaluated by the ICF core set.
Comparisons between the impairment index of the ICF Core Set components across levels of physical activity and physical performance (N = 101).
| ICF Components | |||||||
|---|---|---|---|---|---|---|---|
| Body functions | Body structures | Activities and participation – Performance | Activities and participation – Capacity | e1101 – Use of medications | e1400 – Use of assistive devices | e5800 – Access to health services | |
| Physical activity level | |||||||
| Low | 25.0(14.3–33.9) | 12.5(0–25.0) | 19.4(15.3–26.4) | 6.9(1.4–19.4) | 2(1–3) | 0(0–1) | 4(2–4) |
| Moderate | 22.3(14.3–30.3) | 12.5(0–25.0) | 13.9(11.1–27.8) | 2.8(0–16.7) | 2(1–3) | 0(0 – 0) | 4(4 – 4) |
| High | 16.1(10.7–23.2) | 12.5(0–18.7) | 11.1(6.9–18.0) | 0(0–5.5) | 2(1–3) | 0(0 – 0) | 4(2–4) |
| p-value | 0.012a | 0.716 | 0.002a | 0.005a | 0.644 | 0.055 | 0.156 |
| Total SPPB score | |||||||
| < 8 | 25.0(17.0–37.5) | 12.5(3.1–25.0) | 22.2(16.7–33.3) | 11.1(2.8–22.2) | 3(2–3) | 0(0–1) | 4(2–4) |
| ≥ 8 | 16.1(10.7–23.2) | 6.2(0–12.5) | 11.1(8.3–16.7) | 0(0–5.5) | 1(0–2) | 0(0 – 0) | 4(4 – 4) |
| p-value | <0.001 | 0.006 | <0.001 | <0.001 | <0.001 | <0.001 | 0.060 |
Data are median (25th-75th percentiles).
SPPB: Short Physical Performance Battery; ICF: International Classification of Functioning, Disability and Health.
Note: Higher values for ICF components indicate higher impairment index.
Regarding the association between the ICF core set and the SPPB, participants who were identified as having good physical performance (SPPB ≥ 8) were also classified as having less impairments in body functions and structures, and less difficulties in performing activities evaluated with the ICF core set. Good SPPB performance was also associated with lower use of medications and assistive devices.
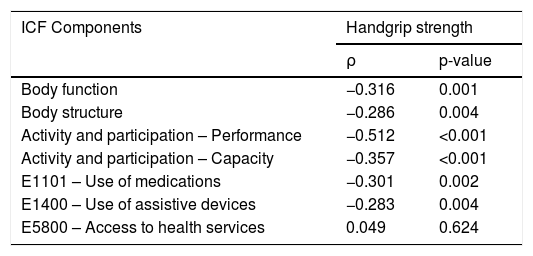
Table 4 shows that a higher grip strength was associated with lower levels of impairment in body structures and functions, less difficulties in performing activities, and lower use of medications and assistive devices.
Correlation between the impairment index of ICF core set components for physical health of older adults and handgrip strength (N = 101).
| ICF Components | Handgrip strength | |
|---|---|---|
| ρ | p-value | |
| Body function | −0.316 | 0.001 |
| Body structure | −0.286 | 0.004 |
| Activity and participation – Performance | −0.512 | <0.001 |
| Activity and participation – Capacity | −0.357 | <0.001 |
| E1101 – Use of medications | −0.301 | 0.002 |
| E1400 – Use of assistive devices | −0.283 | 0.004 |
| E5800 – Access to health services | 0.049 | 0.624 |
ICF: International Classification of Functioning, Disability and Health; ρ: Spearman rho correlation coefficient.
Note: Higher values for ICF components indicate higher impairment index.
The ICC analysis indicated good reproducibility for body function, activity, and participation components (capacity and performance), and for the category related to the use of core set assistive devices (Table 5). Reproducibility was considered excellent for the category of medications use. The body structure and body function components, and the category of use of assistive devices presented good reproducibility. The reproducibility for the activity and participation domain was better for the capacity component (good reproducibility) than for the performance component (moderate reproducibility). The category related to access to health services had poor reproducibility.
Test-retest reproducibility of ICF Core Set for Physical Health of the older adults (N = 101).
| ICF Components | ICC | 95%CI | p-value |
|---|---|---|---|
| Body function | 0.76 | 0.65, 0.83 | < 0.01 |
| Body structure | 0.76 | 0.66, 0.83 | < 0.01 |
| Activity and participation – Performance | 0.75 | 0.64, 0.82 | < 0.01 |
| Activity and participation – Capacity | 0.81 | 0.74, 0.87 | < 0.01 |
| e1101 – Use of medications | 0.91 | 0.87, 0.94 | < 0.01 |
| e1400 – Use of assistive devices | 0.78 | 0.69, 0.84 | < 0.01 |
| e5800 – Access to health services | 0.42 | 0.25, 0.57 | < 0.01 |
ICC: Intraclass correlation coefficient; ICF: International Classification of Functioning, Disability and Health; CI: Confidence Interval.
Our results show that the ICF core set for the PH of community-dwelling older adults was associated with handgrip strength, lower limbs physical performance, and physical activity level. These results support the convergent validity of ICF core set in relation to these measures. In addition, most of the ICF core set components showed good test-retest reproducibility. Our findings support the use of the ICF core set to assess the PH of community-dwelling older adults as a valid and reproducible tool which may be useful in clinical practice because it is easy, fast, and inexpensive to administer.
This ICF core set appears as an important classification instrument for its multidimensional aspect and for including relevant categories regarding the PH of older adults. From this perspective, it was necessary to evaluate whether the included categories were valid in relation to other already widely used and validated measures for evaluating PH in older adults to confidently indicate the use of the results obtained through the classification by the core set. We opted for validation with PH-related measures which are predictive of important outcomes in the health of older adults such as mortality, quality of life, disability, and self-perceived health.29–33 Thus, the results indicate that the ICF core set can be used as an instrument to classify the PH of older adults.
Physical activity is an important protective factor for the health of older adults, and its regular practice is associated with lower risk of developing cardiovascular and metabolic diseases, falls, cognitive disabilities, osteoporosis, and muscle weakness.34 Regarding the level of physical activity assessed through IPAQ, Eckert and Lange35 suggest that this instrument would be related to the ICF activity and participation component. The level of physical activity assessed through the IPAQ in the present study was not only statistically associated with the activity and participation component, but also with the body functions domain. This reinforces that the different components of the ICF are related to each other and must be considered together, because the performance of activities assessed by the IPAQ can both contribute to the integrity of body functions, the ability to perform such activities may be dependent on the integrity of these functions.
However, we highlight a peculiar feature of the present study sample regarding the IPAQ results, because most participants had a high level of physical activity. In assessing the physical activity level of older adult residents in a small city, Cifuentes and Silva36 observed that about 73% of them were active or very active, consistent with the findings presented here. It is speculated that this result may be associated with the characteristics of the city and population, considering that the sample has low education and resides in a small city, and thus performing domestic activities and using walking as a means of transportation are more common. Furthermore, although a systematic review37 of physical activity questionnaires concluded that the IPAQ long version presents moderate reliability, high measurement error, and moderate construct validity for different age groups, studies limited to older adults indicate that the IPAQ results are often underestimated or overestimated.38,39 They suggest that the questions of the IPAQ should be adapted to improve its validity and reliability for older adult populations.38,39
Regarding the SPPB, a relationship was observed with all evaluated ICF components. Considering that the SPPB evaluates the performance in important daily tasks, the association found reinforces that the items of this core set are useful for classifying the PH of older adults. Consistent with these findings, Ribeiro and Romão40 suggest that measures of physical functioning, including the SPPB, refer to the body functions addressed in ICF. Oliveira and collaborators41 reinforce that the SPPB is also related to the activity and participation component.
For handgrip strength, Pratama and Setiati42 reported a correlation between handgrip strength and mobility assessed by the Timed Up and Go test, noting that the higher the handgrip strength, the shorter the time in the test, which indicates a good outcome. In addition, Taekema et al.43 found that lower handgrip strength would be associated with greater decline in daily living activities and cognition. The results presented by these authors indicate a relationship between handgrip strength and measures related to body function and activities and participation components, thus corroborating the results found in the present study where grip strength appeared to be associated with body functions, body structures, and activity and participation in both constructs, and with the categories of medications and assistive devices.
The category of access to health services (e5800) did not appear associated with any of the evaluated instruments in this study. Moreover, it presented low reproducibility, which indicates that the question to evaluate access may not have been clearly understood by the study participants. Older people often need different health services because of the multiple demands they face, and the answers given may have been considering a particular service (access to the hospital, for example) or health services in general, reducing the confidence of the data for this category. Schneidert et al.44 suggest that it is still necessary to develop environmental indicators and appropriate environmental assessment tools in the context of the ICF to adequately explain the environment-functioning relationship.
Good results were observed regarding the reproducibility of the ICF core set, with most components showing good reproducibility. Okochi et al.45 found low test-retest reproducibility for most of the 237 ICF categories, with their qualifiers belonging to the body functions and activities and participation components in a sample of 742 institutionalized or home-care older adults. However, the authors found that reproducibility was influenced by the evaluator’s experience, and the greater the experience, the better the reproducibility.45 The evaluators in the present study were specifically trained for this evaluation in a standardized manner, which may have contributed to the good results.
The present study has some limitations which should be considered. Although the sample was stratified by neighborhoods to cover a great diversity of older adults in relation to sociodemographic characteristics, it was recruited by convenience, which may have led to a non-representative sample. Thus, the presented results may differ when considering other populations with different characteristics. Finally, the ICF core set for PH of older adults was applied using mostly subjective measures for each category, and further studies are needed to identify whether the use of other measures, such as clinical tests and examinations, would yield similar results. It is worth emphasizing that the ICF is a classification system which enables recording a person’s main health problems through categories and their respective domains. However, neither the ICF nor the core sets present the specific approach in which such categories must be measured. Although the methods used in this study to assess each category of the ICF have been based on previous studies and are valid methods, it is important to highlight that other forms of assessment for the same category are possible. Therefore, if there is a change in the approach of evaluating one or more categories of this core set, it may generate a different result in relation to its validity and reproducibility.
ConclusionThe results show that the ICF core set for PH of community-dwelling older adults is valid in relation to the handgrip strength, lower limbs physical performance, and physical activity level. It is also reproducible, indicating that the data obtained through this instrument can be used with confidence by clinicians and researchers. It is noteworthy that the referred core set presents a broad classification system with a low-cost biopsychosocial approach, along with easier and faster application when compared to other similar instruments.
Conflict of interestNone.
This work was supported by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) [Finance Code 001].