Children with motor delays are at increased risk for delayed means-end problem-solving (MEPS) performance.
ObjectivesTo evaluate children with motor delays: 1) the impact of motor delay severity and MEPS mastery timing on developmental trajectories of MEPS; and 2) the effectiveness of Sitting Together And Reaching To Play (START-Play) intervention for improving MEPS.
MethodsThis represents a secondary analysis from a multi-site randomized controlled trial, with blinded assessors and prospective registration. Children with mild or significant motor delays (n = 112, mean age=10.80, SD=2.59 months at baseline) were randomly assigned to START-Play or usual care early intervention (UC-EI) and assessed at five visits across one year using the Means-End Problem-Solving Assessment Tool that included three 30-second MEPS trials per visit. Task mastery occurred at the first visit the child achieved the highest level of performance in at least two of the three trials. Multilevel analyses evaluated trajectories of MEPS outcomes dependent upon the timing of MEPS mastery, motor delay severity, and intervention group.
ResultsAt baseline, children with mild motor delays demonstrated better MEPS than children with significant delays, but this difference was only observed for children who achieved mastery late. Children with significant delays demonstrated greater improvements in MEPS in the post-intervention phase compared to children with mild delays. No MEPS differences were found between START-Play and UC-EI.
ConclusionMotor delay severity and timing of task mastery impacted MEPS trajectories, whereas START-Play intervention did not impact MEPS for children with motor delays.
Clinical Trials Registry identifierNCT02593825 (https://clinicaltrials.gov/ct2/show/NCT02593825)
Children with motor delays are at increased risk for delayed or impaired means-end problem-solving (MEPS) performance,1,2 which signifies intentional actions to achieve a goal.3,4 Young children at risk for autism spectrum disorder (ASD) used fewer problem-solving strategies and greater assistance in MEPS tasks compared to typically developing children within the first 15 months of life.5 At 6–12 months of age, infants with low socioeconomic status showed delayed performance and less success in the means-end towel task compared to children with moderate to high socioeconomic status.6 Infants born preterm had lower MEPS success rates and delayed emergence of intentionality than their full-term peers.1 Furthermore, at the age of 7 months, preterm infants at risk for motor delays had lower scores than full-term infants on one- to three-step planning tasks (i.e., one-step: pulling a towel to retrieve a distant, supported toy; two-step: added transparent barrier; three-step: goal object placed off the cloth with a string attached resting out of the infant's reach).7
It is important to have tools that enable screening for early problem-solving delays and tracking of changes across time.2,8 The Means-End Problem-Solving Assessment Tool (MEPSAT) was designed to measure children's learning and performance in the one-step towel-pull task described above.2 The MEPSAT is supported by validity and reliability evidence; it is sensitive to detect MEPS differences in young children and to capture changes across time.2 Previous research validated the MEPSAT2 while incorporating a subset of the data from the Sitting Together And Reaching To Play (START-Play) multi-site randomized controlled trial9 reported in the current manuscript, along with data collected from typically developing children. While this prior work2 focused on psychometric analysis of the MEPSAT, the current manuscript used the MEPSAT to longitudinally evaluate MEPS in relation to severity of motor delay, timing of mastery achievement in the MEPS task, and type of early intervention received by children, across the complete dataset from the START-Play study.
Children with motor delays may benefit from early interventions aimed at advancing MEPS skills; however, few studies evaluated this effect. Full-term infants with low birth weight showed higher scores on a MEPS task (i.e., towel removal to retrieve a hidden toy) than control peers after a psychosocial intervention program provided during the first eight weeks of life.10 Young children (8–34 months of age) with motor delays who received a motor-based problem-solving intervention improved problem-solving skills compared to children who received body-weight-support intervention.11 The START-Play intervention showed to advance motor and cognitive skills and improve visual-manual problem-solving skills in children with significant motor delays based on performance in the Assessment of Problem-Solving in Play,9 which measures looking, object exploration, and problem-solving behavior during play with a standardized set of toys.12 However, the effect of START-Play intervention and related motor-based problem-solving interventions, specifically on children's MEPS skills, has not been evaluated.
Here, we aimed to document the developmental trajectories of MEPS for young children with mild versus significant motor delays and evaluate the effectiveness of START-Play intervention for improving MEPS in these children. We hypothesized that children with mild delays would outperform children with significant delays and that START-Play intervention would improve MEPS. We also aimed to determine whether MEPS mastery timing affected MEPS trajectories, expecting decreased task interest after MEPS mastery achievement. To our knowledge, this is the first study to evaluate whether MEPS mastery level impacts MEPS development across time.
MethodsStudy design and settingThis multi-site randomized controlled clinical trial, single-blind, parallel group design was prospectively registered in the Clinical Trials Registry (NCT02593825). This study presents a pre-planned secondary analysis from the START-Play clinical trial.9 Intervention and assessments were performed across five sites in the United States [Duquesne University, Pittsburgh, PA; University of Delaware (UD), Newark, DE; University of Nebraska Medical Center (UNMC), Omaha, NE; University of Washington (UW), Seattle, WA; Virginia Commonwealth University (VCU), Richmond, VA]. The study was completed in accordance with regulations set by the Duquesne University (protocol #2015/06/5) and VCU (protocol # HM20005431) Institutional Review Boards. Parents provided informed consent. Data were analyzed at the University of Nebraska-Lincoln (UNL), Lincoln, NE.
ParticipantsChildren with motor delays were recruited during 2016–2019 across five sites. Eligibility criteria were: 1) 7–16 months of corrected age at baseline; 2) ability to sit with or without arm support for at least 3 seconds; 3) inability to transition in or out of sitting; 4) presence of spontaneous arm movements; and 5) gross motor delays evidenced by a scaled score of more than 1SD below the mean for the gross motor subscale of Bayley Scales of Infant and Toddler Development, 3rd Edition (Bayley-III).13 Exclusion criteria were significant visual disorder, ASD, Down syndrome, spinal cord injury, uncontrolled seizure disorder, or neurodegenerative disorders.
An a priori power analysis was performed for the primary outcomes (e.g., reaching, sitting, problem-solving, and global development)9 and a sample size of 152 children was suggested to detect intervention effects (two-tailed, α=0.05, power≥.80, attrition rate 8%).13,14 Initially, 155 potential participants were assessed for eligibility; 134 children were tested at baseline; 22 children were excluded from analysis (Supplementary material – Fig. 1S). The remaining 112 participants were classified as having mild (n = 62) or significant (n = 50) motor delays based on the Bayley-III motor composite score.9 Group comparisons are underpowered, and implications are discussed in the limitations section.
RandomizationAfter the baseline assessment, concealed random assignment was performed as predetermined by an investigator not involved in data collection. Sequentially numbered, sealed, and opaque envelopes were used. All participants were randomly assigned in blocks, with stratification into groups of movement ability9 to either usual care early intervention (UC-EI, n = 55) or START-Play (START-Play, n = 57) group to achieve equivalent groups.
InterventionThe START-Play intervention was provided twice weekly (40–60 minutes/session) throughout the first 12 weeks of the study by trained physical therapists at each site in collaboration with parents/caregivers, using key ingredients of START-Play.9,13,15 Children assigned to START-Play continued receiving their usual care (i.e., early intervention and/or outpatient therapy services). Those in UC-EI received only their usualcare services.
ProcedureChildren were assessed in their homes by trained examiners blind to children's intervention group at baseline and 1.5, 3-, 6-, and 12-months post-baseline (mean=4.5, SD=1.1 visits per child; 11.3% missing visits). At each visit, children were seated in a portable highchair (Fig. 1) and engaged in a MEPS task assessing their ability to pull a towel (means object) to obtain a toy (end object).3,4 Children were provided three 30-second trials with a small, interesting toy placed out of reach on the far end of the towel. Trials ended when the child touched the toy, moved any of the task objects out of reach, or 30 seconds elapsed.1,16
Outcome measuresTesting procedures were video-recorded, and behaviors were scored from videos by trained experimenters blind to intervention group allocation using the MEPSAT. Videos were recoded for intra- and inter-rater reliability. Strong intra-rater [ICC= 0.996 (0.992, 0.999)] and inter-rater [ICC=0.997 (0.995, 0.999)] reliability evidence of means-end performance scores was found.2
The MEPSAT outcomes were: 1) MEPS learning: the determination of successful MEPS was based on a rubric incorporating three outcomes measures: a) Toy contact: contacting the toy by pulling the towel (yes vs no); b) Looking at the toy: looking at the toy in the five seconds prior to contacting it (yes vs no), c) Intentionality: attempting to retrieve the toy with clear intention, meaning focus on the toy, interacting with the towel to retrieve the toy, and looking at and grasping the toy (yes: clear intention vs no: no evidence of intention or unclear/ambiguous intention). MEPS learning occurred when contact was made with the toy, visual attention to the toy occurred within the five seconds before contact, and intention to retrieve the toy was rated as “clear” for a trial; and 2) MEPS level of performance: rated on a scale of 0–9 using a decision tree with 9 marking the highest level of performance (e.g., 0: no towel contact, 9: toy contact, looking at the toy).2 All variables were averaged across the three 30-second trials for statistical analyses.
MEPS mastery achievement occurred at the first visit when the child scored at the highest level of means-end performance (score 9) in at least two out of three trials. Note that mastery was not synonymous with perfection in the task. Mastery was defined based on one MEPS variable (level of performance: toy contact, while looking at the toy; successful trial) and allowed room for unsuccessful performance on one trial. Previous research showed that a score of nine in two of three trials likely represents intentional performance for young children.2 Therefore, it was possible for participants to show improvements in any MEPS variables even after achieving mastery.
Statistical analysesPiecewise linear mixed modeling was performed using Mplus version 8.5 (Muthén & Muthén, Los Angeles, CA). Linear mixed modeling accounted for repeated measures within each child. Piecewise modeling, using individually varying time points, allowed estimation of the intercept (baseline), slopes during the intervention (baseline to 3-month visits), and post-intervention phase (3–12-month visits) for the MEPS outcomes.
Independent variables included in the models were: 1) two-pieced individually varying time points to estimate two slopes (Time1: baseline to 3-months, and Time2: 3- to 12-months); 2) intervention effect (INT: 0=UC-EI; 1=START-Play); 3) child's motor delay severity (SEV: 0=mild; 1=significant); and 4) MEPS mastery timing (MST: Early mastery: mastery achieved at baseline or 1.5-month visit; Late mastery: mastery achieved after 1.5-month visit or not in this study). The 1.5-month visit was chosen as a cut-off point to dichotomize MEPS mastery timing based on our knowledge of typical and atypical developmental trajectories for MEPS.1,2,16
Two statistical models were performed. Model 1 evaluated severity and intervention effects across baseline, Time1, and Time2. To test whether the timing of MEPS mastery affected MEPS developmental trajectories, Model 2 evaluated the main effects of severity and intervention, as well as SEV*MST and INT*MST interactions across baseline, Time1, and Time2. Both models controlled for children's age at baseline and recruitment site.
Adhering to an intention-to-treat perspective, all cases were included in the analyses regardless of missing visits17 using full information maximum likelihood (FIML) estimation. Due to the complexity of the models, which included random effects and individually-varying times of assessment, a residual analysis could not be performed in Mplus. However, non-normality was suggested by univariate descriptive statistics and histograms, so robust FIML (denoted MLR in Mplus) was used to obtain standard errors and test statistics robust to non-normality. Statistical significance was based on α=0.05. Hedges g was calculated as a measure of effect size, with standardized differences of 0.20, 0.50, and 0.80 being interpreted as small, medium, and large effects, respectively.18 Positive g values signify the magnitude of the effect favoring children with significant motor delays and in the START-Play group, whereas negative g values denote the magnitude of the effect favoring children with mild motor delays and in the UC-EI group.
ResultsParticipants’ demographic and health-related information is presented in Table 1.
Demographic and health-related information for children with motor delays assigned to the START-Play or Usual Care-Early Intervention (UC-EI) group.
Note. Data are displayed as Mean ± SD or frequency (proportion).
Children with mild motor delays were more likely to achieve MEPS mastery earlier than those with significant delays (χ2(1) = 25.61, p<0.001). Among children with mild delays, 38.3% mastered the MEPS task early. In contrast, among children with significant delays, only 8.4% mastered the MEPS task early. The percentage of participants per each MEPS mastery level according to motor delay severity and intervention group is presented in Table 2.
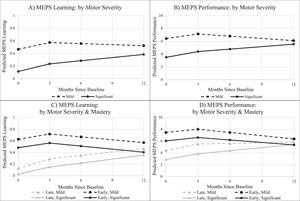
Estimated statistical parameters for Model 1 are summarized in Table 3, presented in Supplementary material - Table S1, and illustrated in Fig. 2A-B. No differences were found between the START-Play and UC-EI intervention groups for either MEPS outcome at baseline, during the intervention, or post-intervention.
Results from Model 1 evaluating differences between children with mild versus significant motor delays (severity effects) or between the START-Play and the UC-EI groups (intervention effects) at baseline, during the intervention phase, and during the post-intervention phase.
Mild = better performance for children with mild motor delays; Sig = better performance for children with significant motor delays; - = no statistically significant or clinically meaningful difference in performance between the groups, * statistically significant, ϕ medium effect size (g ≥ 0.5), ⊥ large effect size (g ≥ 0.8).
Estimated modeled developmental trajectories for means-end learning and performance by baseline motor severity (mild vs significant motor delays); first averaged across MEPS mastery timing levels (Model 1; A: MEPS learning; B: MEPS performance), and then presented according to the timing of MEPS mastery (early vs late mastery) (Model 2; C: MEPS learning; D: MEPS performance).
Statistically significant substantial clinical effects were observed between children with mild vs significant motor delays. At baseline, children with mild delays outperformed those with significant delays in MEPS learning (g=−1.08, large effect; p< 0.001) and performance (g=−1.21, large effect; p< 0.001). During the intervention phase, both motor delay severity groups improved in MEPS learning and performance at the same rate of change. However, during the post-intervention phase, statistically significant substantial clinical effects were detected between the two severity groups in their rates of change for MEPS learning (g = 0.50, medium effect; p = 0.033) and performance (g = 0.81, large effect; p< 0.001): while children with mild motor delays had plateaus in these two outcomes, their peers with significant delays continued improving their MEPS learning and performance.
Model 2: severity and intervention effects while considering the timing of means-end problem-solving masteryEstimated statistical parameters for Model 2 are summarized in Table 4, presented in Supplementary materials - Tables S2 and S3, and illustrated in Fig. 2C-D. Model 2 showed no significant INT*MST interaction for either MEPS outcome at baseline, during intervention, or post-intervention. This indicates that the intervention effect did not significantly differ for infants who achieved MEPS mastery early vs. late. In addition, when stratifying by MEPS mastery (i.e., when looking at the intervention effect separately for infants who achieved MEPS mastery early vs. late), there were no significant intervention effects at baseline, during intervention, or post-intervention in either mastery group.
Results from Model 2 evaluating differences between children with mild versus significant motor delays (severity effects) or between the START-Play and the UC-EI groups (intervention effects) stratified by MEPS mastery timing (early = at the baseline or 1.5-mo visit; late = after the 1.5-month visit or not during the study) at baseline, during the intervention phase, and during the post-intervention phase.
Mild = better performance for children with mild motor delays; Sig = better performance for children with significant motor delays; early Mastery = better performance for children with early mastery; - = no statistically significant or clinically meaningful difference in performance between the groups, * statistically significant effect, ϕ small to medium effect size (g ≥ 0.35), ⊥ large effect size (g ≥ 0.8).
Model 2 also showed no significant SEV*MST interaction for either MEPS outcome at baseline, during intervention, or post-intervention, indicating that the severity effect did not significantly differ for infants who achieved MEPS mastery early vs. late. When stratifying by MEPS mastery, among children who achieved mastery late, there was a significant and clinically meaningful difference favoring children with mild motor delays at baseline in MEPS learning (g= −0.67, medium to large effect; p = 0.019) and performance (g= −0.82 – large effect, p = 0.003). Among children who achieved MEPS mastery early, the difference between children with mild vs. significant motor delays was not statistically significant and was smaller in magnitude but still clinically meaningful for MEPS learning (g= −0.40, small to medium effect; p = 0.299) and performance (g= −0.59, medium effect; p = 0.163).
During the intervention phase, no differences by severity were observed among children who achieved mastery early or among children who achieved mastery late. During the post-intervention phase, among children who achieved mastery late, children with significant delay demonstrated greater improvement in MEPS performance than children with mild delay; this difference was clinically meaningful but not statistically significant (g = 0.47, small to moderate effect; p = 0.090). No statistically or clinically meaningful severity effects during the post-intervention phase were observed for MEPS learning among children who achieved mastery late, or for either outcome among children who achieved mastery early.
DiscussionThe purpose of this study was to compare the developmental trajectories of MEPS in children with mild vs. significant motor delays and to evaluate the effectiveness of the START-Play intervention for improving MEPS in children with motor delays. We also aimed to test whether the timing of MEPS mastery (early vs late) affected MEPS trajectories. No effects of START-Play intervention were found for MEPS outcomes in the towel-pull task, despite the START-Play ingredients being different from UC-EI intervention15 and positive effects of START-Play being demonstrated for motor, cognitive, and even problem-solving outcomes across other tasks for children with significant motor delays.9 It may be that the towel-pull task, especially with the physical support provided by the chair, may have required gross and fine motor skills (e.g., gaze stabilization, reaching for objects on surfaces, and sitting) that were similarly advanced by both START-Play and UC-EI intervention.
Despite the lack of the hypothesized START-Play intervention effects on MEPS outcomes, our results demonstrated clinically important differences in the developmental trajectories of MEPS measures in children with different levels of motor delay that varied based on the timing of MEPS mastery achievement. Below, we expand on these identified differences.
At baseline, the START-Play and UC-EI groups showed similar MEPS performance, suggesting that the intervention groups were similar at the beginning of the study. By contrast, at baseline, children with mild delays outperformed children with significant motor delays in both MEPS outcomes. In addition, among children who achieved mastery later in the study (at 3-, 6-, or 12-month visits) or not during the study, the baseline difference in MEPS outcomes between severity groups was larger in magnitude for children with mild motor delays. Similar clinically meaningful effects were found for children who achieved mastery earlier. These results are consistent with previous research, reporting that young, typically developing children and children with mild motor delays consistently outperformed those with moderate or significant motor delays in both the MEPS learning and performance outcomes.2 Children with more significant motor delays present with more impaired postural control, reaching, and grasping abilities,19-21 which likely negatively impacts their learning and performance in the means-end towel task.2
During the intervention phase, children with mild or significant motor delays improved in all MEPS outcomes at similar rates, regardless of the timing of MEPS mastery. These results align with prior evidence showing that young children at risk for delays or those with varying levels of motor delay have poorer MEPS performance compared to their peers with typical development, but they can demonstrate similar rates of improvements in their MEPS performance and increase their MEPS success across time.1,2
During the post-intervention phase, differences were observed between children with mild vs. significant delays for MEPS learning and performance. While children with mild motor delays showed declines or plateaus in these two outcomes, children with significant delays continued improving. Declines or plateaus in children with mild delays likely reflect a shorter learning period and lack of engagement in the task after mastery. When stratifying by MEPS mastery timing, the late mastery group, clinically higher rates of change in MEPS performance were observed in children with significant motor delays compared to those with mild delays. In general, steeper rates of change during the post-intervention phase allowed children with significant delays to decrease the gap in MEPS performance between themselves and those with mild delays by the end of the study. Children with significant motor delays who achieved mastery later in the study or not during the study may continue finding the MEPS towel task interesting, thus, engaging in the task throughout the study.
LimitationsThere are potential limitations of this study. First, the number of participants included in the final analyses was less than the number suggested by an a priori power analysis, suggesting the study was underpowered. However, this study includes a secondary data analysis, whereas the power analysis was based on available data from preterm infants14 and estimated for the primary outcomes.9,13 Those data may not be representative of the children who ultimately participated in the study or for the MEPSAT outcomes. Regardless, the effects' clinical magnitude and statistical significance should be considered, and follow-up studies with larger sample sizes should be conducted to evaluate whether the findings replicate. Second, more than two-thirds of the children with mild delays achieved MEPS mastery early. Although it was possible for children to show improvements in MEPS outcomes even after achieving mastery, we cannot rule out the possibility of a ceiling effect for children with mild motor delays. Third, the intervention doses were not matched between the two groups. Future studies should investigate comparison with dose-matched intervention for this population and for other children with different motor and cognitive abilities. Lastly, our analyses controlled for children's age at baseline and recruitment site but did not control for socioeconomic status or dose of intervention. Future studies should evaluate the effect of these potential moderators.
ConclusionsThis study longitudinally evaluated MEPS developmental trajectories related to severity status, timing of mastery achievement in the MEPS task, and type of intervention. In summary, children with mild motor delays showed better MEPS outcomes than children with significant delays at baseline. However, children with mild delays showed declines or plateaus in their MEPS outcomes during the post-intervention phase, whereas those with significant delays sustained higher rates of change for MEPS learning and performance, which allowed them to catch up, at least to some degree, with their peers having mild delays. These severity differences were more pronounced among children who achieved mastery late, but the general pattern of findings, in which children with mild delays started off higher, but children with significant delays demonstrated higher rates of change and approached similar MEPS outcomes, was consistent. The START-Play intervention did not impact MEPS in the towel-pulling task for children with motor delays greater than UC-EI alone.
Evaluation of MEPS skills can be challenging in young children with motor delays, especially in natural settings.22 The MEPSAT might be a promising tool for screening early problem-solving delays in young children with motor delays. Our results suggest important clinical implications: 1) MEPS should be an important consideration for early intervention providers working with young children having motor delays; 2) children with significant motor delays may demonstrate greater impairments in MEPS; and 3) a longer period may be required to solidify learning of MEPS tasks for children with significant motor delays.
The authors would like to thank all the children and their parents for their participation in this longitudinal study, and the research assistants for coding the data. This research was supported by the Institute for Education Sciences (grant #R324A150103).
Funding information: This research was supported by the Institute for Education Sciences (grant #R324A150103).