In 2013, physical therapy students demonstrated low guideline-adherent recommendations regarding chronic low back pain (CLBP) for spinal pathology, activity, and work.
ObjectivesTo assess the differences in physical therapy students’ attitudes, beliefs, and adherence to guideline recommendations regarding CLBP and knee osteoarthritis between 2013 and 2020.
MethodsIn 2013 and 2020, second and fourth-year physical therapy students were recruited from 6 Belgian and 2 Dutch institutions. Attitudes and beliefs regarding CLBP and knee OA were evaluated using the Pain Attitudes and Beliefs Scale for Physiotherapists (PABS-PT), the Health Care Providers’ Pain and Impairment Relationship Scale (HC-PAIRS), and a questionnaire regarding therapeutic exercise and knee osteoarthritis. A clinical vignette was used to measure guideline-adherent recommendations regarding spinal pathology, activity, and work.
ResultsIn 2013, 927 second-year and 695 fourth-year students; in 2020, 695 second-year and 489 fourth-year students; were recruited to participate in the study. Compared to 2013, students had less biomedical and stronger biopsychosocial attitudes and beliefs regarding CLBP, more guideline-adherent recommendations for activity, and more biopsychosocial beliefs regarding the benefits of exercise for patients with knee osteoarthritis in both the second and fourth year. Only fourth-year students in 2020 scored significantly better on HC-PAIRS and guideline-adherent recommendation relating to spinal pathology. No differences were found regarding work recommendations.
ConclusionsBetween 2013 and 2020, physical therapy students made a positive shift towards a more biopsychosocial approach to CLBP and knee osteoarthritis management. Guideline-adherent recommendations for CLBP concerning activity improved, however, concerning work and spinal pathology, it remained low.
Although scientific research regarding chronic pain is exponentially rising, the management of chronic pain remains challenging for patients, physical therapists, and society.1-8 There has been substantial progress in the neuroscientific knowledge of pain, taking into account that biomedical, psychological, and social factors significantly influence chronic pain and pain-related disability.9-13 Yet, many physical therapists think pain and disability result from a specific structural impairment, and pain management remains mainly biomedically oriented.14-19 Physical therapists with higher biomedical attitudes and beliefs generally adhere less to the clinical guidelines, are more likely to advise patients to restrict physical activities and work, and are associated with worsening pain and poor disability outcomes.19-23
Education could play a key role in shifting these misbeliefs towards a biopsychosocial approach.24-27 However, previous studies found inadequate hours of pain education in pain curricula within educational programs and that pain was not a core part of curricula.28-30 These findings imply that there was strong potential for improving biopsychosocial beliefs among physical therapy students towards chronic pain management. Our previous study showed that Dutch and Belgian physical therapy students’ orientation shifted towards a more biopsychosocial approach from their second to fourth-year during education in 2013.31 Yet, most fourth-year physical therapy students retained a biomedical orientation towards chronic low back pain (CLBP) treatment.31
Within the last decade, multiple calls for action were made by researchers and policymakers to improve pain care through changes in pain-related health systems, societal initiatives, and by implementing biopsychosocial pain management within educational curricula to improve the biopsychosocial knowledge and beliefs of future healthcare professionals, including physical therapists.29,32-34 However, it is unknown whether these calls for action have resulted in a change in biopsychosocial knowledge and beliefs of future healthcare professionals in line with modern pain science. Interestingly, no studies have investigated if physical therapy students’ pain attitudes and beliefs have become more biopsychosocially oriented over the past few years, reflecting a biopsychosocial shift within physical therapy education.
The primary objective of this study was to (1) evaluate the differences in biomedical and biopsychosocial attitudes and beliefs regarding the management of CLBP and knee osteoarthritis (OA) and guideline-adherent recommendations regarding the management of CLBP in Dutch and Belgian between second- and fourth-year physical therapy students educated in 2013 versus those educated in 2020. Secondary objectives were to examine (2) whether CLBP-related attitudes, beliefs, and guideline-adherent recommendations regarding spinal pathology, activity, and work changed from the second to the fourth-year of physical therapy education in 2020 (3) and if age, sex, institutions, history of low back pain (LBP), and current LBP were predictors of attitudes, beliefs, and guideline-adherent recommendations regarding CLBP.
MethodsThe study was approved by an independent Medical Ethical Committee (#2020/321) linked to the University Hospital of Brussels, and was conducted in accordance with the Helsinki Declaration of 1975. The study is reported following the STROBE recommendations.35
Study designThis study conducted a cross-sectional assessment of physical therapy students in Dutch and Belgian institutions in 2020 compared to students in 2013.31 A more detailed description regarding the methods and reliability and validation of the questionnaires can be found in the study reporting the cross-sectional results of 2013.31
Recruitment and participantsFour Flemish (Vrije Universiteit Brussel, University of Antwerp, University of Ghent, and the Catholic University of Leuven), two Walloon (University of Liège and Université Catholique de Louvain), and two Dutch (Hanze University of Applied Sciences Groningen and University of Applied Sciences Rotterdam) institutions participated in 2013 and 2020. All participating institutions' second and fourth-year students were eligible for inclusion. In 2013, students were recruited by phone, through practice visits (convenience sampling), or at lectures. In 2020, due to COVID-19, students were recruited through notifications on digital platforms at their institution, emails, and information during lectures. All participants signed informed consent before participating in the study.
Data collectionData were collected within the first semester of the academic year in 2013–2014 and 2020–2021. In 2020, students received a link to the online survey at Qualtrics or the questionnaire on paper. In 2013, all students filled in the questionnaire on paper. The questionnaire was provided in French or Dutch, based on the languages in which the students were being taught. To avoid social desirability response bias, all students were told that they were free to express their actual thoughts and beliefs when filling in the questionnaire, that there were no ‘correct’ responses and that the procedure was not an examination.36 No further information was given.
Outcome measuresThe outcome measures in 2020 were identical to those in 2013. A general questionnaire was used to collect characteristics of the students, i.e. age, sex, personal history, and presence of LBP. Attitudes and beliefs regarding CLBP and knee OA were quantified with three questionnaires, and a clinical vignette was used to assess their clinical recommendations regarding CLBP. These tools are described below.
The Pain Attitudes and Beliefs Scale for Physiotherapists (PABS-PT) was used to assess the biomedical and biopsychosocial approach towards the management of patients with CLBP.37,38 The biomedical subscale (PABS-BM) contains 10 items and score ranges between 10 and 60, and the biopsychosocial subscale (PABS-BPS) contains 9 items and total scores range between 9 and 54. Higher PABS-BM scores indicate a stronger biomedical orientation, and higher PABS-BPS scores indicate a stronger biopsychosocial orientation. The PABS-PT had adequate internal consistency, construct validity, reliability, and responsiveness.39 However, the discriminative ability of the psychosocial subscale was low and the content validity is unknown.39,40
The Health Care Providers’ Pain and Impairment Relationship Scale (HC-PAIRS) evaluates the attitudes and beliefs of healthcare practitioners regarding the functional expectations of patients with CLBP.41,42 The questionnaire contains 13 items, total scores range from 13 to 91, and higher scores reflect stronger beliefs about the relationship between pain and impairment. The HC-PAIRS internal consistency, construct validity, and discriminant validity was adequate.41-43
The Physical Therapists’ Attitudes and Beliefs About Exercise and Knee OA contains 23 attitude statements, 12 statements regarding the benefits of exercise for knee OA and 11 statements regarding the delivery of exercise and exercise adherence.23 Each attitude statement is scored on a 6-point Likert scale ranging from ‘totally disagree’ to 6 ‘totally agree’. Scores of each item are evaluated individually. The psychometric properties of this questionnaire are unknown.
The clinical vignette (Supplemental material online 1) contains a clinical case scenario of a patient with CLBP purposed to evaluate if symptoms result from spinal pathology and their treatment recommendations concerning activity and work on a 5-point Likert scale.44 The following recommendations were defined as consistent with clinical guidelines for spinal pathology: (1) spinal pathology: ‘no spinal pathology’ and ‘mild spinal pathology’, (2) activity: ‘no activity limitations’, ‘avoid only painful activities’, (3) and work: ‘full time, full duty’ and ‘full time, moderate duty’. The validity of clinical vignettes is unclear and ranges from little differences to poor concordance with actual behaviour and standardized patients.45-49
Statistical analysisDifferences in attitudes and beliefs and clinical recommendations between 2013 and 2020 were examined with general(ized) mixed models (GLMM), and students were clustered by institutions. The estimated marginal mean of 2013 and 2020 was calculated through GLMM to account for differences in observations within and between institutions. Age, sex, institution, history of LBP, and current LBP were evaluated to determine whether these factors help to predict the outcomes. Intraclass correlation coefficients of the GLMM were reported to represent the average correlation of students within the clustering of institutions.50 Institutions pre-arranged to report results anonymously. Subgroups were created for second- and fourth-year students. A p-value of 0.05 was considered significant. Single linear regression imputation was used to impute missing values (<5%) for the PABS-PT and HC-PAIR.51 Cases were excluded for imputation per questionnaire when >50% of the items within that questionnaire had missing data.51 Due to the limited number of missing values (<5%), it did not suggest any systematic bias. Q/Q’-plots were used to evaluate normality assumptions. IBM SPSS Statistics 27 was used for statistical analysis.
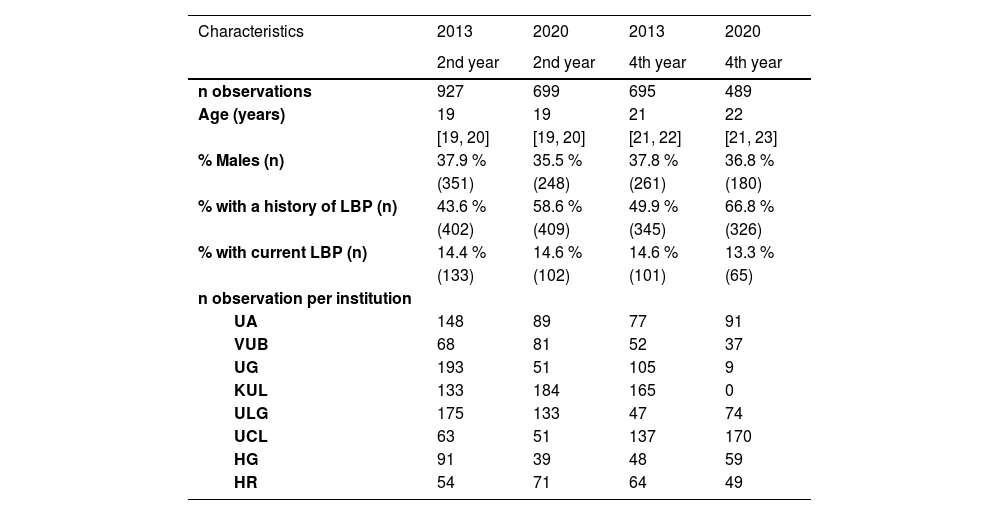
ResultsA total of 2810 physical therapy students participated. In 2013, 927 second-year and 695 fourth-year students participated, and in 2020, 695 second-year and 489 fourth-year students were included. Characteristics of all students are presented in Table 1. The characteristics of the 2013 and 2020 samples are similar regarding sex and the percentage of participants experiencing LBP at the time of data collection (Table 1). Fourth-year students’ median age was one year higher in 2020 compared to 2013, and 15.0% more second-year students and 16.9% more fourth-year students had a history of LBP in 2020. The number of observations within institutions also differed between 2013 and 2020, and between institutions. One institution did not recruit fourth-year students in 2020.
Characteristics of second and fourth-year physical therapy students in 2013 and 2020 (n = 2810).
Data are presented as proportions or median (interquartile range [Q1, Q3]).
Legend: UA, University of Antwerp; VUB, Vrije Universiteit Brussel; UG, University of Ghent; KUL, Catholic University of Leuven; ULG, University of Liège; UCL, Université Catholique de Louvain; HG, Hanze University of Applied Sciences Groningen; HR, University of Applied Sciences Rotterdam; LBP, low back pain.
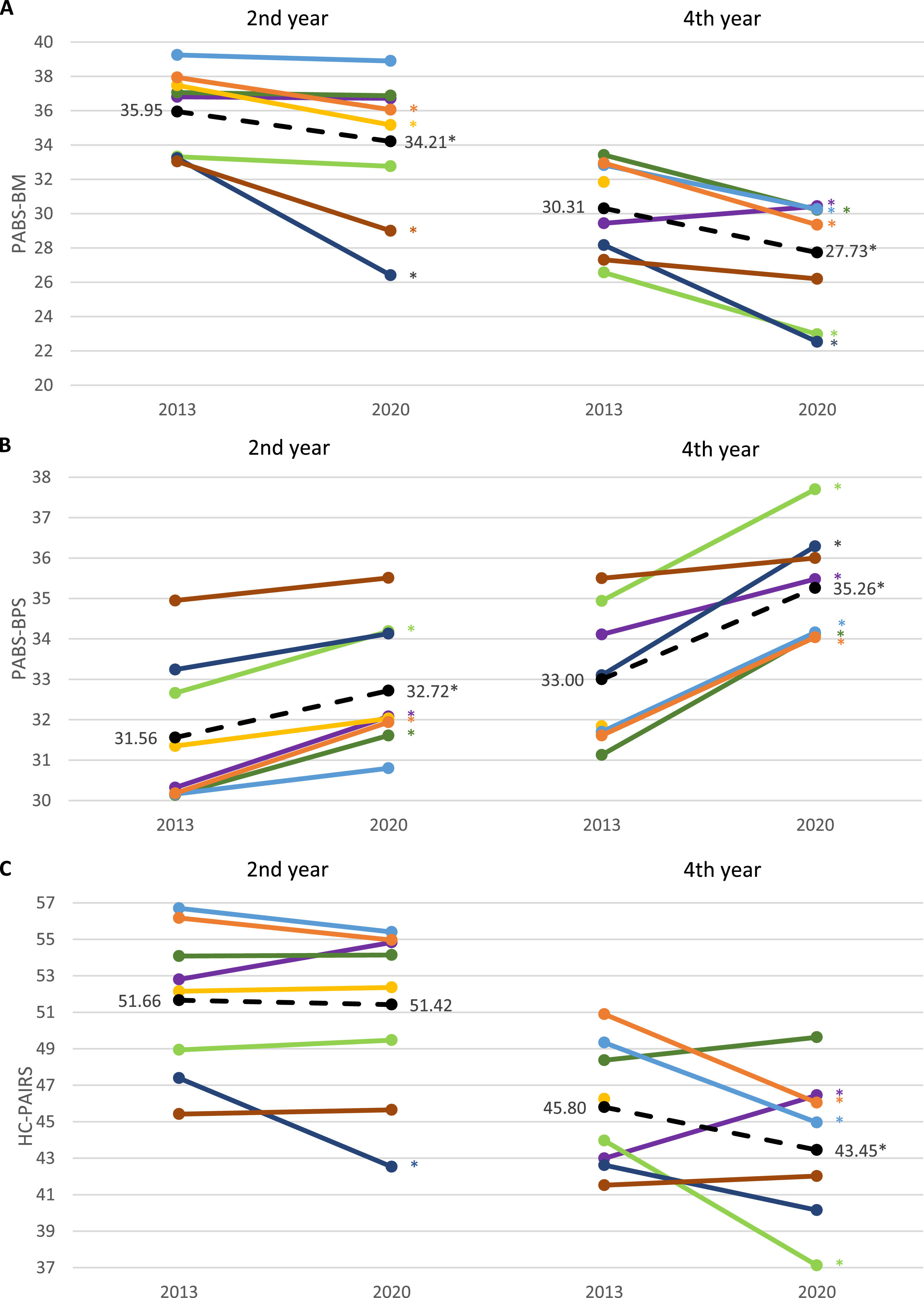
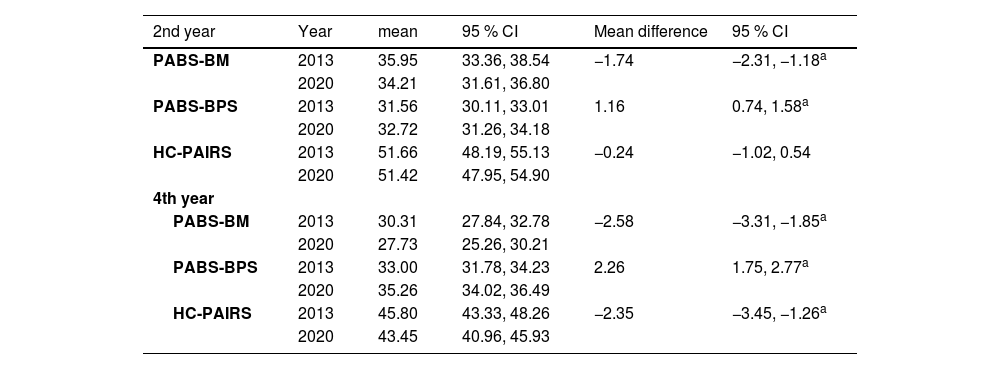
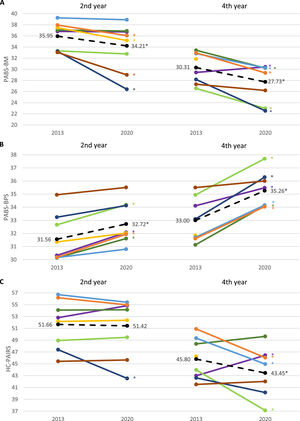
Compared to 2013, the 2020 students had less biomedical beliefs, higher biopsychosocial beliefs, and less beliefs in the relationship between pain and impairment (Table 2). Differences in beliefs were larger in fourth-year students (PABS-BM: MD = −2.58, 95% CI: −3.31, −1.85; PABS-BPS: MD = 2.26, 95% CI: 1.75, 2.77; HC-PAIRS: MD = −2.35, 95% CI: −3.45, −1.26) than for second-year students (PABS-BM: MD = −1.74, 95% CI: −2.31, −1.18; PABS-BPS: MD = 1.16, 95% CI: 0.74, 1.58). There was no significant difference in beliefs between second-year students in the relationship between pain and impairments (HC-PAIRS: MD = −0.24, 95% CI: −1.02, 0.54).
Estimated marginal mean differences between second and fourth-year students’ attitudes and beliefs regarding chronic low back pain in 2013 versus 2020.
| 2nd year | Year | mean | 95 % CI | Mean difference | 95 % CI |
|---|---|---|---|---|---|
| PABS-BM | 2013 | 35.95 | 33.36, 38.54 | −1.74 | −2.31, −1.18a |
| 2020 | 34.21 | 31.61, 36.80 | |||
| PABS-BPS | 2013 | 31.56 | 30.11, 33.01 | 1.16 | 0.74, 1.58a |
| 2020 | 32.72 | 31.26, 34.18 | |||
| HC-PAIRS | 2013 | 51.66 | 48.19, 55.13 | −0.24 | −1.02, 0.54 |
| 2020 | 51.42 | 47.95, 54.90 | |||
| 4th year | |||||
| PABS-BM | 2013 | 30.31 | 27.84, 32.78 | −2.58 | −3.31, −1.85a |
| 2020 | 27.73 | 25.26, 30.21 | |||
| PABS-BPS | 2013 | 33.00 | 31.78, 34.23 | 2.26 | 1.75, 2.77a |
| 2020 | 35.26 | 34.02, 36.49 | |||
| HC-PAIRS | 2013 | 45.80 | 43.33, 48.26 | −2.35 | −3.45, −1.26a |
| 2020 | 43.45 | 40.96, 45.93 | |||
CI, Confidence interval; PABS-BM, Pain Attitudes and Beliefs Scale for Physiotherapists biomedical subscale; PABS-BPS, Pain Attitudes and Beliefs Scale for Physiotherapists biopsychosocial subscale; HC-PAIRS, Health Care Providers’ Pain and Impairment Relationship Scale.
Differences in attitudes and beliefs were found when data from all participating institutions were pooled. However, this shift was not found in all institutions. Estimated mean score and mean differences on the PABS-BM, PABS-BPS, and HC-PAIRS were significantly different (p < .001) between institutions (Fig. 1). In one institution, fourth-year students had significantly higher beliefs in the relationship between pain and impairment in 2020 than in 2013.
The biopsychosocial shift is seen in many but not all institutions in 2020 compared to 2013 (1A and 1B, n = 2808; 1C, n = 2720). 1A. Biomedical orientation; Lower scores represent less biomedical beliefs. 1B Biopsychosocial orientation; Higher scores represent stronger biopsychosocial beliefs. 1C. Beliefs in relationship between pain and impairment; Lower scores represent less belief in the relationship between pain and impairment.
Legend: Coloured lines represent mean scores per institution, dashed black line shows the mean scores of all institutions combined. *Group difference p < .05.
Table 3 presents an overview of the difference between students’ guideline-adherent recommendations based on the clinical vignette in 2013 versus 2020. Significantly more fourth-year students expected ‘no spinal pathology’ or ‘mild spinal pathology’ as the cause for the CLBP symptoms in 2020 than in 2013 (19.5% vs 9.3%; OR = 2.31). No differences were found in second-year students in 2020 compared to 2013 (6.8% vs. 7.1%; OR = 0.96). Regarding activity, “Not limit any activity” or “Avoid only painful activities” was significantly more recommended in 2020 compared to 2013 by second-year students (35.5% vs 42.4%, OR = 1.34) and fourth-year students (61.8% vs 69.5%, OR = 1.41). Regarding work recommendations in 2020, 11.4% of the second-year students and 27.7% of the fourth-year students recommended “Work full time, full duty” or “Work moderate duty, full time”, which was considered guideline-adherent. Both groups did not significantly differ compared to students in 2013 on guideline adherence (yes/no) nor on mean scores (means of the Likert scale scores). No results per institution were given for guideline-adherent recommendations due to the small proportion of guideline-adherent recommendations in physical therapy students regarding spinal pathology and work in combination with the very low response rate in two institutions. This resulted in groups with zero guideline-adherent recommendations, which provided potentially biased results and difficulty in drawing reliable conclusions on differences between institutions.
Guideline-adherent recommendations, 2013 versus 2020 (n = 2760).
| 2nd year | Year | Proportion/Percentage | 95 % CI | Df | t | Odds | 95 % CI |
|---|---|---|---|---|---|---|---|
| Spinal pathology | 2013 | 7.1 | 5.6, 9.0 | 1, 1591 | −0.21 | 0.96 | 0.65, 1.42 |
| 2020 | 6.8 | 5.2, 9.0 | |||||
| Activity | 2013 | 35.5 | 32.5, 38.6 | 1, 1596 | 2.81 | 1.34 | 1.09, 1.64a |
| 2020 | 42.4 | 38.7, 46.2 | |||||
| Work | 2013 | 9.8 | 8.0, 11.9 | 1, 1595 | 1.04 | 1.19 | 0.86, 1.64 |
| 2020 | 11.4 | 9.2, 14.0 | |||||
| 4th year | |||||||
| Spinal pathology | 2013 | 11.5 | 9.3, 14.1 | 1, 1160 | 5.17 | 2.31 | 1.68, 3.17a |
| 2020 | 23.1 | 19.5, 27.1 | |||||
| Activity | 2013 | 61.8 | 58.1, 65.4 | 1, 1158 | 2.70 | 1.41 | 1.10, 1.81a |
| 2020 | 69.5 | 65.2, 73.5 | |||||
| Work | 2013 | 23.7 | 20.7, 27.1 | 1, 1158 | 1.53 | 1.23 | 0.94, 1.61 |
| 2020 | 27.7 | 23.8, 32.0 | |||||
Legend: SE, standard error; CI, conference interval; df, degree of freedom; Odds, Odds ratio.
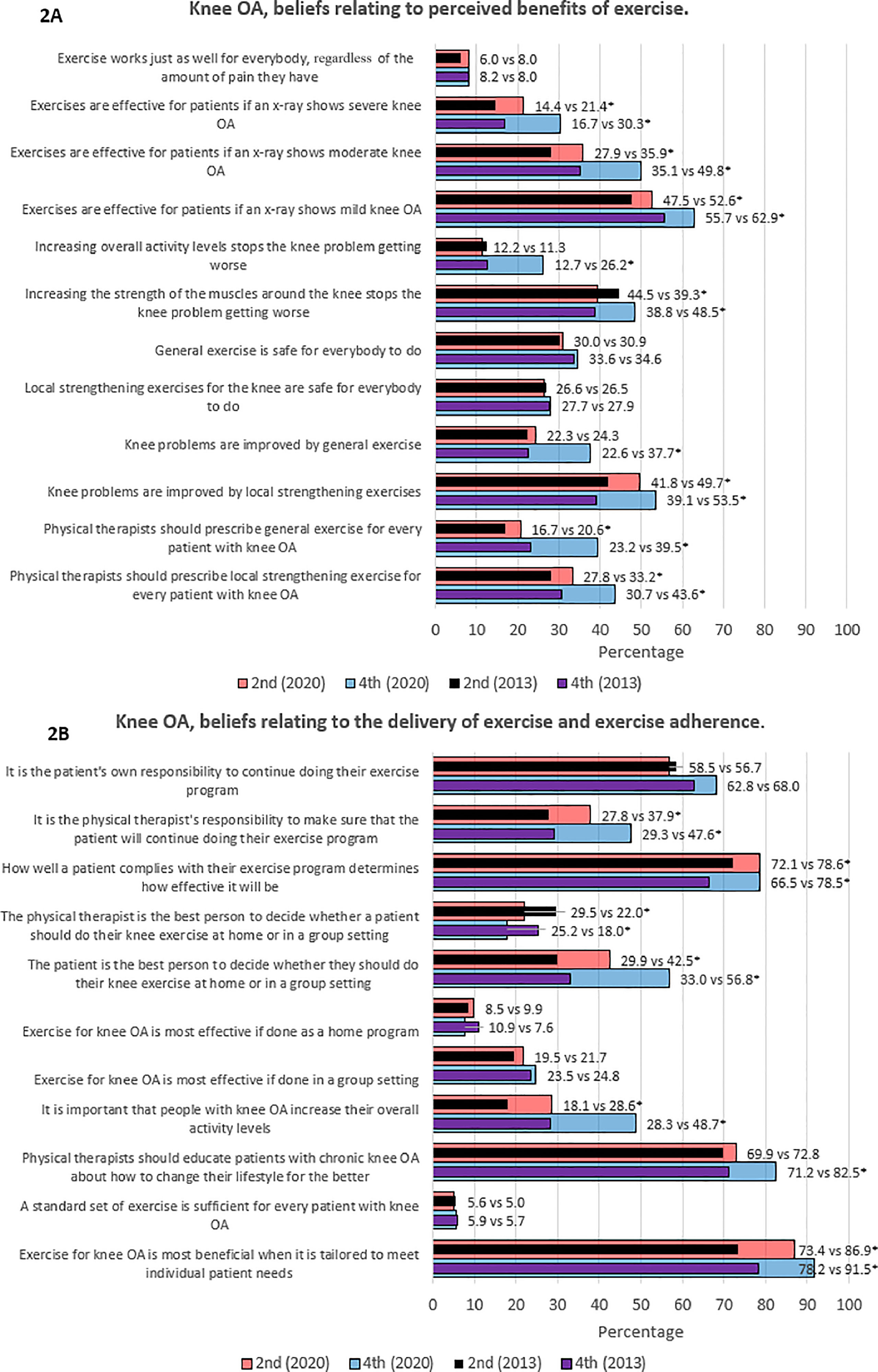
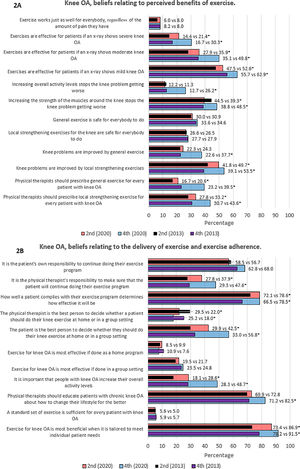
In general, a significantly higher percentage of second- and fourth-year students in 2020 in comparison to 2013 ‘largely agreed’ or ‘totally agreed’ with statements supporting the benefits of exercise and the biopsychosocial model (Fig. 2).
Beliefs relating to perceived benefits of exercise in patients with knee OA and beliefs relating to the delivery of exercise and exercise adherence in patients with knee OA (n = 2724).
Legend: Results show differences in percentages of students between students in 2013 and 2020 who largely agree or totally agree on the statements. OA, osteoarthritis; vs, versus. *Group difference p < .05.
Exercise therapy is believed to be effective for patients when radiographs show mild, moderate, or severe knee OA in more second-year and fourth-year students in 2020 than in students in 2013. However, radiographic findings influenced students’ beliefs regarding exercise effectiveness, the more severe the findings, the less likely the students were to agree that exercise therapy is effective for patients with knee OA. Further, more students in 2020 compared to students in 2013 agreed that general exercise (2nd year: 20.6% vs 16.7%; 4th year: 39.5% vs 23.2%) and local strengthening exercises (2nd year: 33.2% vs 27.8%; 4th year: 43.6% vs 30.7%) should be prescribed for patients with knee OA. Consistent with declining beliefs in exercise effectiveness when magnetic resonance imaging findings show more severe knee OA, the minority of students in 2013 and 2020 believed that both general and local strengthening exercises are safe for everybody to do.
Regarding beliefs relating to the delivery of exercise therapy and adherence, more students in 2020 compared to 2013 believed that patients compliance determined the effectiveness of exercise programs, (2nd year: 78.6% vs 72.1%; 4th year: 78.5% vs 66.5%), that exercise is most beneficial when it is tailored to meet individual patient needs (2nd year: 86.9% vs 73.4%; 4th year: 91.5% vs 78.2%), and that the patient is the best person instead of the physical therapist to decide whether they should do exercise at home or in a group setting (2nd year: 42.5% vs 29.9%; 4th year: 56.8% vs 33.0%). Furthermore, more fourth-year students in 2020 compared to students in 2013 (82.5% vs 71.2%) believed that physical therapists should educate patients with chronic knee OA about how to improve their lifestyle and more second and fourth-year students believed that it is important that patients with knee OA increase their overall activity levels (2nd year: 28.6% vs 18.1%; 4th year: 48.7% vs 28.3%).
Age, sex, current LBP, history of LBP, institution, and year of educationBased on the total sample, sex, current LBP, and history of LBP were no significant predictors for the level of attitudes and beliefs and guideline-adherent recommendations regarding CLBP. Higher age predicted lower biomedical orientation, less belief in the relationship between pain and impairment, and higher guideline-adherent recommendations regarding spinal pathology and activity (Supplemental material online 2). Being a fourth-year student predicted less biomedical and stronger biopsychosocial orientation, less belief in the relationship between pain and impairment, and more guideline-adherent recommendations in all outcome measurements. Studying in 2020 predicted better outcomes except for guideline-adherent recommendation regarding work. Institutions explained between 12.1% to 30.6% of the variance in attitudes and beliefs, and guideline-adherent recommendations regarding CLBP.
DiscussionThis study aimed to investigate if the 2020 physical therapy students’ attitudes and beliefs regarding CLBP and knee OA and their guideline-adherent recommendations are better than those of the students in 2013. In general, Dutch and Belgian physical therapy students had stronger biopsychosocial attitudes and beliefs regarding the management of both CLBP and knee OA and guideline-adherent recommendations were higher for spinal pathology and activity in 2020 compared to 2013.
Although physical therapy students had stronger biopsychosocial attitudes and beliefs towards CLBP and knee OA, their beliefs regarding the relationship between pain and impairment remained high. Previous studies with graduate and undergraduate healthcare professionals reported similar misbeliefs in the relationship between pain and impairment.52-55 These beliefs are associated with limiting patients’ activity and work participation and could explain the relatively small improvements in guideline-adherent recommendation regarding activity and the lack of difference in guideline-adherent recommendation regarding work participation between 2013 and 2020.56,57 In addition, it is also reflected by the large expectancy of moderate to extreme severe spinal pathology causing CLBP based on the clinical vignette, decreasing beliefs in the effectiveness of exercise therapy when the severity of knee OA increased, and a large percentage of students who believed that exercises are not safe for everybody with knee OA, which are common beliefs in healthcare professionals.23,58
The effect of adequate and comprehensive education in pain is reflected by the stronger biopsychosocial beliefs in fourth-year students compared to second-year students and the significant improvement within several institutions in 2020 compared to 2013.59 This positive learning curve in 2020 was also found in the cohort of 2013 and is consistent with previous studies observing the change in pain attitude and beliefs in physical therapy students from first to last year semesters and comparing physical therapy students between different semesters within an institution.26,27,60-64 However, these results were not found within every institution in our study, which can be due to differences between pain curricula in educational programs like pain content and hours taught but also the timing of measurements and pain lectures within the curricula.28-30,65 Although this study did not examine the curricula of physical therapy educational programs, the institution was a contributing factor in predicting the physical therapy students’ level of biopsychosocial beliefs and guideline-adherent recommendations regarding CLBP.
To our knowledge, no previous study used a similar design to compare the difference between academic years over a more extended period of time, preventing a comparison of our primary objective. However, the results illustrate that physical therapy students’ biomedical orientation is still too strong and biopsychosocial orientation and guideline-adherent recommendations are still too low, underscoring the need for additional efforts to implement the biopsychosocial model and evidence-based practice for the management of CLBP and knee OA within all physical therapy educations.
Strengths and limitationsThe strengths of this study include the substantial number of students (n = 2810) who participated in this international multi-institutional-based comparison of cross-sectional measurements in 2013 and 2020. Likewise, the number of participating institutions (n = 8) is a unique feature and has not been done before.
The missing data of this large sample size remained below 5%, limiting the risk of bias and enhancing the likelihood that the sample and the data represented the physical therapy students population in the Netherlands and Belgium.66 Moreover, having seven years between both measurements allowed sufficient time for physical therapy educational programs to adapt curricula in alignment with the biopsychosocial model. Another strength is the addition of attitudes and beliefs assessment regarding knee OA to evaluate whether potential differences in attitudes and beliefs were also found in another chronic musculoskeletal pain beyond CLBP.
This study also has several limitations. The PABS-PT and HC-PAIRS, respectively developed in 2003 and 1995, may not fully align with modern pain science, the PABS-PT's interpretability and content validity are lacking, and its biopsychosocial subscale demonstrated insufficient discriminative ability.39,67,68 Moreover, clinical vignettes’ validity ranges from little differences to poor concordance with actual behaviour and standardized patients, and a difference in attitudes and beliefs, and clinical recommendations based on vignettes do not perfectly reflect a difference in clinical behavior which has multifactorial causations.45-49 Further, classifying ‘avoiding painful activities’ as guideline-adherent might have led to overestimating guideline-adherent recommendations regarding activity as it did not distinguish between avoiding painful daily activities and those that exceed patient's physical capacity.69,70 Similarly, recommending “light duty, full time” could also be considered guideline-adherent as the clinical vignette lacks definition for “moderate duty” and “light duty” and Dutch and Belgian clinical guidelines recommend reducing work absenteeism without commenting on the intensity of work tasks.69,70
Clinical relevanceDespite the calls for action, after seven years, overall attitudes and beliefs were 5.1% to 8.5% more biopsychosocial; guideline-adherent recommendations regarding spinal pathology and activity was 11.6% and 7.7% higher; and there was even more variance in attitudes and beliefs of physical therapy students between institutions. On a large scale, it could indicate a clinically relevant improvement. However, average total scores of attitudes and beliefs differed by approximately 2 points, which makes the impact debatable. No cut-off points are known to decide whether attitudes and beliefs are considered ‘strong’ or ‘weak’ or if differences in scores are clinically relevant. There is much room for improvement to address physical therapy students’ misbeliefs regarding CLBP and knee OA management.
Educational programs have been proven effective in enhancing students' biopsychosocial attitudes and beliefs, underscoring the need to revise educational curricula by incorporating more essential pain-related items and increasing the hours taught using pedagogic approaches.59,71-73 Implementing these in all curricula could decrease the variance between universities, resulting in significant improvements in all institutions over time, and benefit students and physical therapists on the outcomes of this study. Future educational research should explore the role of content, dosage, timing, competence level, quality, years of education, bachelor or other physical therapy educational programs on physical therapy students’ attitudes, beliefs, and clinical recommendations. Additionally, a broader perspective of personal factors like cultural and social factors on students’ learning curves should be explored to determine which factors hinder or facilitate the development of biopsychosocial attitudes and beliefs of physical therapy students, because only age, year of education, academic year, and institution were significant predictors in our study.33,74-78 Further, outcome measures in future studies should also focus on more underlying beliefs and motives to provide a better understanding of physical therapy students’ clinical recommendations.
ConclusionThe comparison of the 2013 and 2020 cohorts of physical therapy students demonstrated a shift in attitudes and beliefs towards a more biopsychosocial approach and guideline-adherent recommendations for CLBP and knee OA management, but the improvements were limited and varied among institutions. However, no improvement was found in work recommendations, and guideline adherence of physical therapy students’ recommendations remained low, allowing ample room for improvement.
Conflicts of interestNone of the authors have any conflicts of interest related to the topic of this paper.
We would like to thank all institutions for their participation in this study.