The Tampa Scale for Kinesiophobia (TSK) is one of the most frequently employed instruments for assessing maladaptive beliefs about pain, injury, and movement in patients with chronic musculoskeletal pain. However, the measurement properties of this tool have so far not been tested for individuals with migraine.
ObjectiveTo evaluate the structural, construct, and criterion validity, and the internal consistency for three versions (TSK-11, TSK-13, and TSK-17) of the TSK for patients with migraine.
MethodsA total of 113 individuals aged between 18 and 55 years old with migraine diagnosis were included. All participants completed the TSK with 17 items, the Fear-Avoidance Beliefs Questionnaire, the Headache Impact Test, and the Pain Catastrophizing Scale questionnaires. Confirmatory factor analysis was used to assess the structural validity of the TSK, and Cronbach's α was used to assess internal consistency. For construct and criterion validity, the Spearman's correlation was calculated.
ResultsThe TSK structure with one factor and the 17, 13, or 11 items versions were suitable, with suitable values in all fit indices related to structural validity. The three versions showed acceptable internal consistency (α = 0.75). All TSK versions showed moderate positive correlation with the other questionnaires (rho range= 0.31–0.63), confirming most of the predefined hypothesis for the construct validity. Also, the criterion validity of the 13-item and 11-item versions was confirmed (rho=0.95 and rho=0.94, respectively).
ConclusionAll versions of the TSK demonstrated good measurement properties in the assessment of maladaptive beliefs about pain, injury, and movement in individuals with migraine.
Migraine is a primary headache that affects one billion people worldwide.1 It is a neurological disease characterized by moderate-to-severe headache attacks, accompanied by nausea/vomiting, light and/or sound sensitivity, and avoidance of physical activity.2,3 Migraine is a subtype of chronic primary headache, but not a chronic primary musculoskeletal pain.4,5 Nevertheless, individuals with migraine show many musculoskeletal repercussions and characteristics, especially at the cervical region.6-9 Also, more than half of these individuals present maladaptive beliefs about pain, injury, and movement.4,10
In previous studies, the term maladaptive beliefs has been equated with kinesiophobia.4,10 However, it should be noted that these two definitions are not interchangeable.11 Kinesiophobia is defined as an excessive, irrational, and debilitating fear of carrying out physical movement due to a feeling of vulnerability to a painful injury or reinjury.12 Conversely, maladaptive beliefs encompass beliefs about pain, injury, and movement, and not just fear of movement. Considering these definitions and the content of the tools applied, previous studies investigated maladaptive beliefs, not kinesiophobia, in individuals with migraine using customized questions or the Tampa Scale for Kinesiophobia (TSK).4,10,13 Due to the inconsistency surrounding the definition of kinesiophobia, the term maladaptive beliefs will be used throughout this document.
Maladaptive beliefs, especially fear of movement, alter movement because they generate avoidance and escape behaviors. As a result of avoidance, individuals present increased pain and pain disability.14 Pain processing is related to how maladaptive beliefs are perceived, and a vicious cycle begins.14,15 Maladaptive beliefs are associated with disability, pain, and lower quality of life in individuals with chronic musculoskeletal pain.16,17 However, maladaptive beliefs in patients with migraine have not yet been extensively explored. Although migraine is not a primary musculoskeletal pain, individuals with migraine and maladaptive beliefs experience greater migraine-related disability than those without, and higher TSK scores are associated with greater risk of more severe migraine disability.10
Movement avoidance is reported by 96% of patients with migraine during a headache attack.13 Maybe because the migraine headache worsens due to daily physical activity (i.e., climbing stairs).3 However, maladaptive beliefs have been observed in 51% of individuals with migraine during headache-free periods.10 Overall, individuals with migraine avoided performing general body movements because of pain,4 and they presented a high prevalence of fear of falling,10,18 which is associated with maladaptive beliefs.10 Despite this, 82.2% and 79.1% of individuals with migraine and migraine with aura, respectively, reported physical activity in their leisure time and commuting time.19 It is known that aerobic exercise is of great importance for these patients and has shown moderate quality evidence for reducing pain intensity, frequency, and duration of migraine, and can also increase the quality of life.20,21
Several clinical tools are available to assess the signs and symptoms associated with migraine.22 However, there is a lack of literature on the validity and reliability of these tools, especially those that assess maladaptive beliefs and biopsychosocial factors. One of the questionnaires currently available to assess maladaptive beliefs is the TSK.23 Although the name of the questionnaire suggests that it assesses the construct of kinesiophobia,23 it assesses beliefs about pain, injury, and movement. The TSK has been translated into Brazilian Portuguese and has good internal consistency,24 and its measurement properties were tested in patients with fibromyalgia.25 The measurement properties of the TSK were investigated in different versions: the original 17-item version and 13-item and 11-item versions.26,27
Even though it is a widely used tool in individuals with chronic pain, to the authors’ knowledge, its measurement properties in patients with migraine have not been tested. For its use, evidence on measurement properties must be available in the target population.28 If adequate measurement properties are obtained, it would provide researchers and clinicians a viable tool to assess maladaptive beliefs in the migraine population. Therefore, this study aimed to investigate the measurement properties (structural validity, hypotheses testing for construct validity and criterion validity, and internal consistency) of the TSK for individuals with migraine.
MethodsThe study followed the Consensus-based Standards for the Selection of Health Measurement Instruments (COSMIN) reporting guideline.29 The study was approved by the local ethics committee at the Clinical Hospital of the School of Medicine of Ribeirão Preto, Universidade de São Paulo (HCFMRP/USP–protocol number 5.276.812/2022) and a written informed consent form was obtained from all participants before data collection.
ParticipantsThe sample consisted of volunteers recruited among patients in tertiary headache outpatient clinics and the general community between February and September 2022. According to COSMIN guidelines, sample sizes greater than 100 are needed and considered excellent to test the measurement properties of a questionnaire.29 The inclusion criteria were age between 18 and 55 years old and having at least one migraine attack a month in the previous three months. The subjects were diagnosed with migraine by a neurologist specializing in headaches.3 The exclusion criterion was a diagnosis of other concomitant headaches, primary or secondary, to avoid an overlap of diagnosis as well as being illiterate or cognitively impaired.
QuestionnairesAll participants responded to a single-day demographic and migraine clinical data questionnaire and completed the TSK, the Fear-Avoidance Beliefs Questionnaire (FABQ), the Headache Impact Test (HIT-6), and the Pain Catastrophizing Scale (PCS) questionnaires. The data were entered into an electronic research database (REDCap).30
The TSK is a 17-item tool used to assess fear of movement, with items 4, 8, 12, and 16 being reverse scored. Scoring options range from strongly disagree to strongly agree, with a total score of between 17 and 68.23 The higher the final score, the higher the level of maladaptive beliefs.31 This questionnaire has been translated into Brazilian Portuguese and it showed good reliability (ICC 0.93)24 and correlates with disability.32 Two short versions (13 items and 11 items) have good psychometric properties for chronic pain.25-27
The FABQ33 has 16 items with two subscales: the work subscale (FABQ-W) with seven items, and the physical activity (FABQ-PA) subscale with four items. This tool focuses on patients’ beliefs about how physical activity and work affect their current pain.33 Each item ranges from 0 (completely disagree) to 6 (completely agree). It is scored separately for each subcategory, ranging from 0 to 24 points for the FABQ-PA and 0 to 42 points for the FABQ-W.34 The FABQ is a valid tool with a high value for internal consistency (Cronbach's α 0.93) and reproducibility (ICC 0.96).35
HIT-6 is a tool assessing headache impact among patients with headache36; the Brazilian Portuguese version showed suitable measurement properties.37 According to the items, the final score varies between 36 and 78 and is classified as little or no impact (≤ 49 points), some impact (50–55 points), considerable impact (56–59 points), and severe impact (≥ 60 points).36 The Brazilian Portuguese version showed suitable reliability (ICC 0.95) and internal consistency (Cronbach's α 0.97).37
The PCS38 consists of 13 items describing different pain-related thoughts and feelings. Patients answer on a 5-point scale with the endpoints 0 (“not at all”) and 4 (“all the time”) in which information about the frequency and intensity of pain is fairly represented. The PCS total score ranges from 0 to 52 points, computed by the summation of all the items. This tool has three domains (magnification, rumination, and helplessness), which scores are given by the sum of the corresponding items. The PCS is a valid and reliable tool with suitable reliability (ICC 0.92) and internal consistency (Cronbach's α: helplessness 0.93, magnification 0.88, and rumination 0.86).39
Measurement propertiesStructural validity is the measurement property that estimates the degree to which the scores on a patient-reported outcome measure (PROM) are an adequate reflection of the dimensionality of the construct to be measured by exploratory factor analysis or confirmatory factor analysis.28 Confirmatory factor analysis is the most accurate approach to try to confirm the factor structure described previously.40 This measurement property is essential to demonstrate the adequacy of the instrument regarding the number of dimensions and to refine the instrument's fit according to the confirmatory factor analysis. Factor loadings represent the correlations between the original variables and the factors. The higher the factor loading, the greater the correlation with a given factor.40,41
Internal consistency refers to the degree of interrelatedness among the items and is often assessed by Cronbach's alpha28Hypotheses testing for construct validity is the measurement that estimates the degree to which an instrument is consistent with hypotheses, based on the assumption that the PROM validly measures the construct to be measured.28
Criterion validity is the measurement that estimates the degree to which the scores of an instrument are an adequate reflection of a “gold standard”.28 Considering that there is no PROM for the assessment of kinesiophobia recognized in the literature as the gold standard, we adopted the COSMIN recommendation in which the only exception is when a short version of an instrument is compared to the original long version. In that case, the original long version can be considered the gold standard.40 In this way, the long version of TSK (17 items) was considered the gold standard in the current study for the assessment of criterion validity.
Statistical analysisData regarding age, body mass index, and migraine characteristics related to the duration of the disease, frequency of crises, and pain intensity were described through descriptive analyses. A descriptive analysis of the positive responses in the TSK was performed to understand the maladaptive beliefs profile of the sample. Positive responses were those in which the patient answered, “partially agree” or “totally agree”, except questions 4, 8, 12, and 16, in which they were considered “totally disagree” or “partially disagree”.
The structural validity of the TSK was assessed by confirmatory factor analysis (IBM SPSS AMOS, version 22). We analyzed the goodness of fit of three models: i) the TSK with a one-factor model with 17 items23; ii) the TSK with a one-factor model with 13 items26; and the TSK with a one-factor model with 11 items.27 Acceptability of fit was evaluated based on several indexes: root mean square error of approximation (RMSEA, recommended value below 0.06),28 comparative fit and goodness of fit indexes (CFI and GFI, recommended value > 0.95),28 expected cross-validation index and consistent Akaike information criterion (ECVI and CAIC–lower values, best fit),42 and CMIN/df (chi-square / degrees of freedom - should be less than 3).42 Magnitudes of factor loadings of 0.3 or greater were considered suitable.43
We assumed hypothesis raised a priori to investigate construct validity.44 We ran correlations between the TSK and the FABQ, the HIT-6, and the PCS. Spearman's correlation was used to assess validity, considering r < 0.30 as weak correlation, 0.30<r < 0.70, moderate correlation, and r > 0.70, as strong correlation.45 Acceptable levels of construct validity are considered if at least 75% of the hypotheses are confirmed.46 A-priori hypotheses were formulated based on previous publications, as follows:
H1: Moderate to strong and positive correlations between the TSK scores vs. FABQ-W scores;
H2: Moderate to strong and positive correlations between the TSK scores vs. FABQ-PA scores;
H3: Moderate to strong and positive correlations between the TSK scores vs. PCS magnification scores;
H4: Moderate to strong and positive correlations between the TSK scores vs. and PCS rumination scores;
H5: Moderate to strong and positive correlations between the TSK scores vs. PCS helplessness scores;
H1 to H5: were raised considering that the TSK and the FABQ measure similar constructs and that the fear of pain can generate catastrophizing, as shown by the fear-avoidance model.47
H6: Mild and positive correlations between the TSK scores vs. HIT-6 score, because less than 20% of the variance in kinesiophobia is explained by the headache-related disability,10 showing that they are different but weakly related constructs.
The internal consistency was analyzed in the three versions of the TSK using Cronbach's α, with acceptable results between 0.70 and 0.95.28 Spearman correlation was used to assess criterion validity. We ran a correlation between TSK-17, as the gold standard, and other versions (TSK-13 and TSK-11), considering rho ≥ 0.70.28 The significance level adopted was 0.05 for all the correlation analysis performed to evaluate construct and criterion validity.
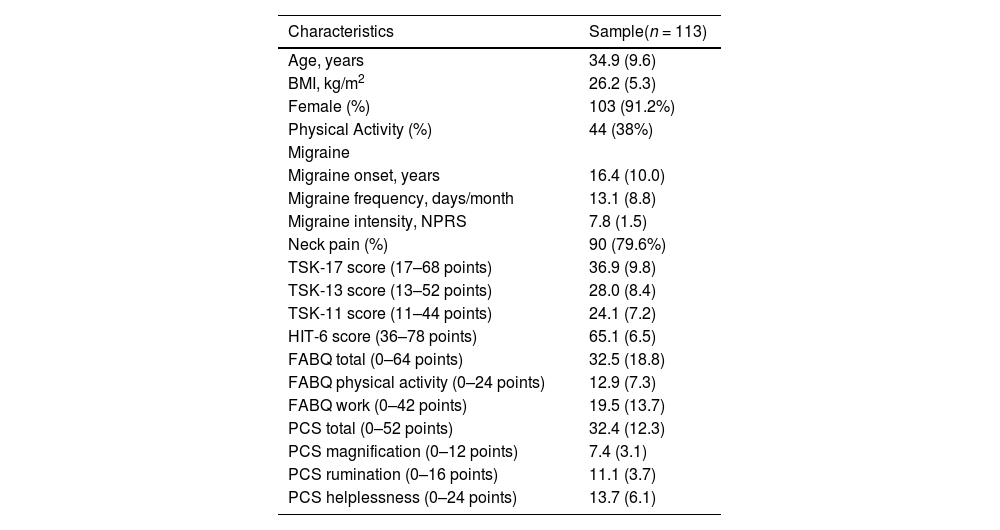
ResultsThe subjects were 113 individuals with a diagnosis of migraine. The mean age of the participants was 35 years (SD 9.6). Table 1 shows all the clinical and demographic characteristics of the participants. More than 50% of patients responded positively (agreement) to items 3, 10, and 13; while more than 70% of the participants disagree with the items 2, 6, 14, and 15.
Clinical and demographic sample data.
Data are mean (standard deviation) and frequency (percentage).
Abbreviations: BMI, body mass index; FABQ, Fear Avoidance Beliefs Questionnaire; HIT-6, Headache Impact Test; NPRS, Numeric Pain Rating Scale; PCS, Pain Catastrophizing Scale; TSK, Tampa Scale for Kinesiophobia.
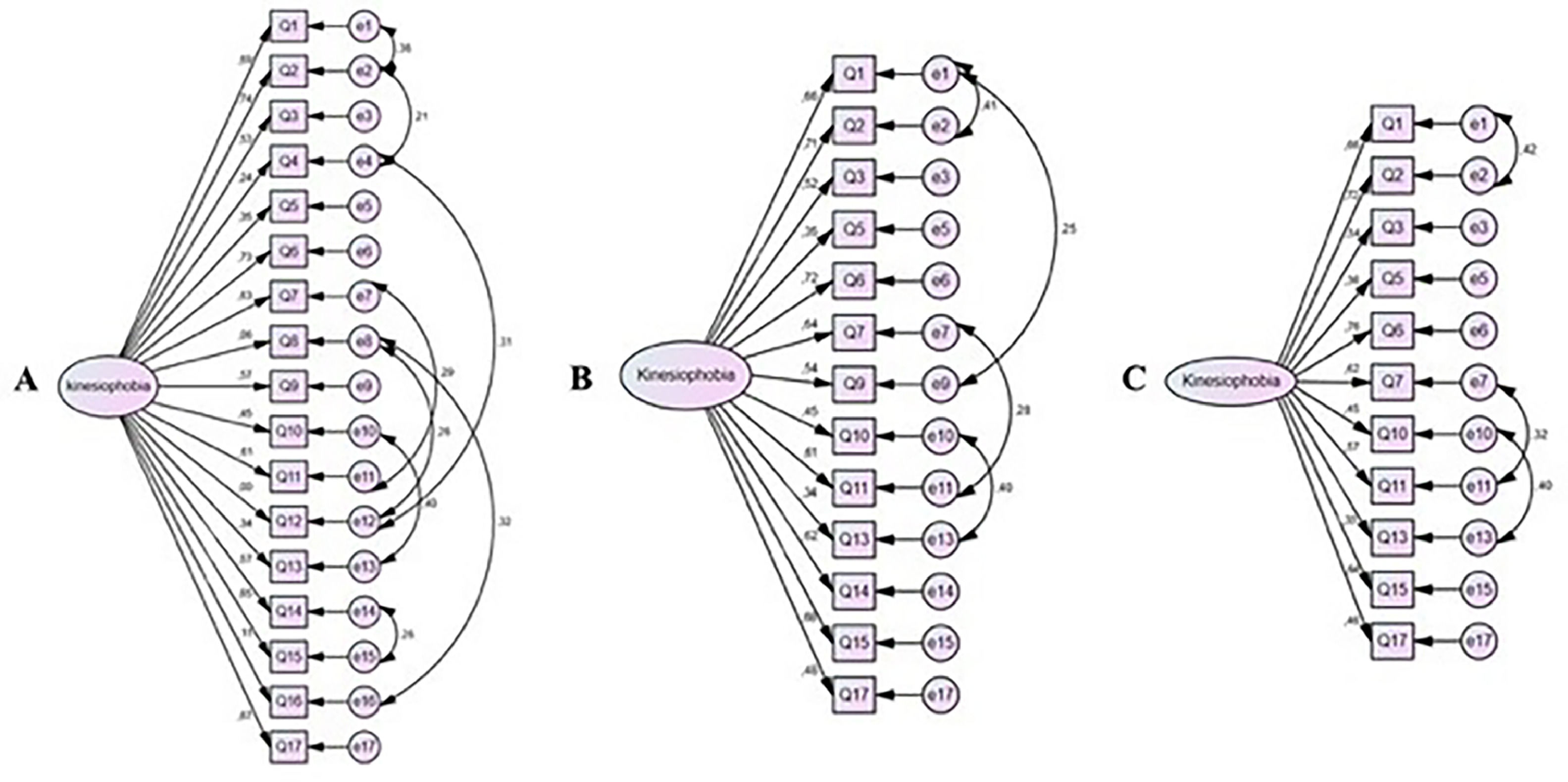
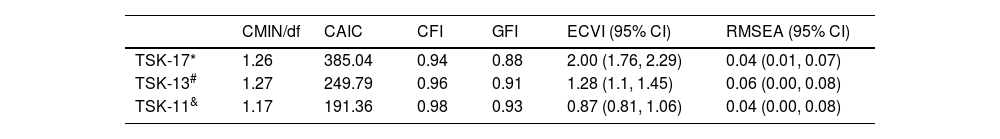
The confirmatory factor analysis showed acceptable values for three models, the TSK-17, the TSK-13, and the TSK-11. The factor loadings for the three models generated by the confirmatory factor analysis are depicted in Fig. 1. Items: 4, 8, 12, and 16 had a factor loading <0.3, showing that these questions are poorly related to the underlying factor. Therefore, these questions were initially withdrawn for the TSK-13 (Fig. 1, Table 2). In addition, we tested the TSK-11,25,27 which has been widely used in the literature, by removing items 9 and 14 from the scale (Fig. 1). An acceptable fit was observed for all versions of TSK. Therefore, all TSK models are considered adequate (Table 2).
Path diagram showing factor structure of the TSK-17 (Fig. A), TSK-13 (Fig. B), and TSK-11 (Fig. C) describing the factor loadings for each item. Q = questions. e = error.
Q1. I'm afraid that I might injure myself if I exercise; Q2. If I were to try to overcome it, my pain would increase; Q3. My body is telling me I have something dangerously wrong; Q4. My pain would probably be relieved if I were to exercise; Q5. People aren't taking my medical condition seriously enough; Q6. My accident has put my body at risk for the rest of my life; Q7. Pain always means I have injured my body; Q8. Just because something aggravates my pain does not mean it is dangerous; Q9. I am afraid that I might injure myself accidentally; Q10. Simply being careful that I do not make any unnecessary movements is the safest thing I can do to prevent my pain from worsening; Q11. I wouldn't have this much pain if there weren't something potentially dangerous going on in my body; Q12. Although my condition is painful, I would be better off if I were physically active; Q13. Pain lets me know when to stop exercising so that I don't injure myself; Q14. It's really not safe for a person with a condition like mine to be physically active; Q15. I can't do all the things normal people do because it's too easy for me to get injured; Q16. Even though something is causing me a lot of pain, I don't think it's actually dangerous; Q17. No one should have to exercise when he/she is in pain.
Confirmatory factor analysis indices obtained for the Tampa Scale for Kinesiophobia (n = 113).
| CMIN/df | CAIC | CFI | GFI | ECVI (95% CI) | RMSEA (95% CI) | |
|---|---|---|---|---|---|---|
| TSK-17* | 1.26 | 385.04 | 0.94 | 0.88 | 2.00 (1.76, 2.29) | 0.04 (0.01, 0.07) |
| TSK-13# | 1.27 | 249.79 | 0.96 | 0.91 | 1.28 (1.1, 1.45) | 0.06 (0.00, 0.08) |
| TSK-11& | 1.17 | 191.36 | 0.98 | 0.93 | 0.87 (0.81, 1.06) | 0.04 (0.00, 0.08) |
One factor structure with 13 items of original TSK (Goubert et al., 2004) with the exclusion of items 4, 8, 12, 16.
One factor structure with 11 items of original TSK (Woby et al., 2005) with the exclusion of items 4, 8, 9, 12, 14, 16.
Abbreviations: CAIC, consistent Akaike information criterion; CFI, comparative fit index; CI, confidence interval; CMIN/df, χ2/df; ECVI, expected cross-validation index; GFI, goodness of fit; RMSEA, root-mean-square error of approximation.
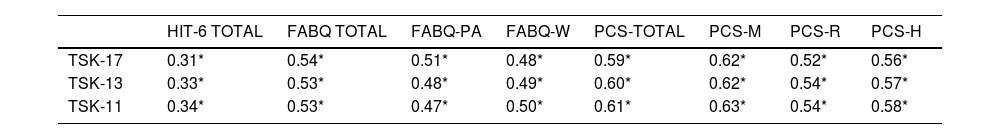
Significant correlations between the TSK and the HIT-6, the FABQ, and the PCS were observed, regardless of the number of TSK questions. The TSK-13 showed a moderate positive correlation in mean scores between the TSK and the HIT-6 (rho = 0.33; p < 0.01) and a moderate positive correlation in mean scores between the TSK and the FABQ (rho = 0.53; p < 0.01), and the TSK and the PCS (rho = 0.60; p < 0.01). The TSK-11 correlations were similar, moderately positive between the TSK and the HIT-6, and moderately positive between the TSK, the FABQ, and the PCS. Most predefined hypotheses (H1 to H5) were confirmed (Table 3), the only hypothesis not confirmed was the weak correlation between the TSK and the HIT-6, as a higher-than-expected correlation was found.
Correlations among the TSK and HIT-6, FABQ, and PCS using Spearman's correlation (n = 113).
| HIT-6 TOTAL | FABQ TOTAL | FABQ-PA | FABQ-W | PCS-TOTAL | PCS-M | PCS-R | PCS-H | |
|---|---|---|---|---|---|---|---|---|
| TSK-17 | 0.31* | 0.54* | 0.51* | 0.48* | 0.59* | 0.62* | 0.52* | 0.56* |
| TSK-13 | 0.33* | 0.53* | 0.48* | 0.49* | 0.60* | 0.62* | 0.54* | 0.57* |
| TSK-11 | 0.34* | 0.53* | 0.47* | 0.50* | 0.61* | 0.63* | 0.54* | 0.58* |
Abbreviations: FABQ, Fear Avoidance Beliefs Questionnaire; FABQ-PA, FABQ-physical activity subscale; FABQ-W, FABQ- work subscale; HIT-6, Headache Impact Test; PCS, Pain Catastrophizing Scale; PCS-H, PCS-helplessness domain; PCS-M, PCS-magnification domain; PCS-R, PCS-rumination domain; TSK, Tampa Scale for Kinesiophobia.
The Cronbach's α was acceptable: 0.73 for the TSK-17, 0.75 for the TSK-13, and 0.75 for the TSK-11.
Criterion validityWhen compared to our chosen gold standard (TSK-17), we observed good validity for the TSK-13 (rho = 0.95, p < 0.001) and TSK-11 (rho = 0.94, p < 0.001). We observed strong correlation between all TSK versions.
DiscussionTSK is the first PROM available in Brazilian Portuguese that evaluates maladaptive beliefs about pain, injury, and movement in patients with migraine. Our results support the structural validity, construct validity for hypothesis testing, criterion validity, and internal consistency of the TSK, with acceptable measurement properties for all versions. The criterion validity of the 13 and 11 items versions were confirmed and all three versions (TSK-17, TSK-13, and TSK-11) showed acceptable internal consistency. Also, all TSK versions showed a moderate positive correlation with the other questionnaires, confirming most of the predefined hypothesis for the construct validity.
Individuals with migraine avoid physical and daily activities, as well as moving their body, neck, or head to prevent a migraine attack or pain.4,10 Accordingly, the evaluation of maladaptive beliefs could help guide specific interventions. However, clinicians should be aware that, considering that the TSK has items unrelated to movement (e.g., “People aren't taking my medical condition seriously enough”), it is not appropriate to say that this scale measures fear of movement or kinesiophobia. It would be suitable to state that the TSK measures maladaptive beliefs in general. Furthermore, structured questionnaires about fear of the movement do not elicit the same responses as when the patient is asked to perform the feared movement.48
There is no single best structure (structural validity) among all versions of the TSK according to the confirmatory factor analysis. Moreover, findings confirmed the one-factor model reported for the original versions of the 17-item TSK23 (RMSEA = 0.04), 13-item TSK26 (RMSEA = 0.05), and 11-item TSK27 (RMSEA = 0.04), indicating that TSK scores in migraine participants adequately reflect the expected dimensionality of the construct being measured. Corroborating with the previous data,26,27 items 4, 8, 12, and 16 have reversed scores and are the same as those removed from the TSK-13 and TSK-11 with low factor loading. Therefore, these questions do not affect the underlying construct, as all TSK versions showed strong correlations with the full version, with 17 points, which is in agreement with previous reports.26,27
More than 75% of the hypotheses suggested between the TSK and the associated tools (FABQ, PCS, and HIT-6) were confirmed. The moderate correlation between FABQ and TSK confirms our construct similarity hypothesis. The presence of some questions considers fear beliefs within the TSK could justify the strength of its relationship with the FABQ total score and FABQ domains score. The relationship between PCS and TSK can also be confirmed. Higher TSK scores are associated with rumination, magnification, and hopelessness domains, which involve the inability to stop thinking about the pain, fear that something more serious could be happening, and the belief that nothing can be done to reduce the intensity of the pain.49 Although the FABQ and PCS have not been validated for individuals with migraine, they are tools that share the construct of maladaptive beliefs with the TSK and they would help to perform the hypothesis testing for construct validity. To date, to our knowledge, there was no validated tool available for this population that could be used to this aim.
On the other hand, we expected a weak correlation between TSK and HIT-6. Because disability is related to the TSK score in primary musculoskeletal disease,47 and less than 20% of the TSK variance is explained by headache-related disability,10 we hypothesized that the correlation between both variables would be lower than the correlation expected in chronic primary musculoskeletal pain. However, the data do not confirm this hypothesis, showing only a moderate correlation between the two variables, and reinforcing that they are distinct and moderately related constructs.
Although the TSK's structural, construct, and criterion validity for individuals with migraine has been demonstrated, the response burden of using long questionnaires during the assessment must be considered. Given its conciseness and good measurement properties, the short version TSK measure also offers promise for reducing time to evaluation and response burden. Therefore, the short version of the TSK can be the most useful for the migraine population, and in the clinical context can help reduce administrative burden as 6 items were eliminated, particularly for the TSK-11. However, we did not control for the impact of time spent to completing the different versions of the TSK, although we believe it is intuitive that it is easier to answer a questionnaire with 11 items rather than 17 items.
It is widely recognized that daily physical activity (i.e., climbing stairs) can exacerbate migraine pain during an attack.3 While fewer than 50% of patients are not afraid of injuring themselves if they exercise, over 60% of patients responded positively to Item 13. Likewise, physical exertion during attacks can generate worsening pain, leading individuals to fear and avoiding movement. More than half of the sample also believe that their body is telling them that they have something dangerously wrong and agree that they should be careful with unnecessary movements to prevent their pain from worsening. The answers to individual TSK items, along with the total score, can help the physical therapist to identify major maladaptive beliefs to address during therapeutic education. Our results suggest that therapeutic education for patients with migraine may be composed of advice on the importance of physical activity in the interictal period, despite the avoidance of movement during the attacks. Moreover, therapeutic education could address the factors that can improve their pain and help them to manage migraine attacks.
The present study has several limitations. The TSK is a tool developed for and focused on chronic musculoskeletal pain. Because individuals with migraine have a complex disease with musculoskeletal symptoms, this questionnaire does not cover several components of avoidance beliefs in patients with migraine, e.g., fear of a new attack or worsening headache. Accordingly, future work may consider content validity for a better definition of content for patients with migraine. Future studies are needed to assess an adaptation of the TSK for individuals with migraine, as was done for temporomandibular disorders.50 Furthermore, other measurement properties such as reliability and responsiveness should also be considered.
To our knowledge, this is the first study to evaluate the measurement properties of the TSK in individuals with migraine. Validation of this tool will contribute to its use in research and clinical practice to measure the maladaptive beliefs in these patients. In addition, we followed all the COSMIN guidelines for assessing measurement properties,29 with a sample size of more than 100 individuals (which is considered excellent) and all analyses performed in accordance with the guidelines.
ConclusionThe results of this study support the structural, criterion, and construct validity (hypothesis testing) and internal consistency of all TSK versions for migraine individuals. The results suggest that all the TSK versions can be used in research and clinical settings to assess beliefs about pain, injury, and movement in patients with migraine. However, the TSK-11 offers the advantage of being shorter, which reduces the administrative burden related to completing the questionnaire.
This work was supported by the São Paulo Research Foundation(FAPESP) [grant numbers: 2020/10091–7; 2022/04179–4]. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.