Migraine may be accompanied by several cervical musculoskeletal dysfunctions, for example an altered performance on the Craniocervical Flexion Test (CCFT). However, CCFT measurement properties are still unclear in patients with migraine.
ObjectivesTo determine intra- and inter-examiner reliability, construct validity, standard measurement error (SEM), and minimal detectable change (MDC) of the CCFT in patients with migraine.
MethodsWomen diagnosed with migraine were considered eligible for this study. Participants were assessed by two examiners for the inter-examiner reliability, and with 7–10 days interval for the intra-examiner reliability. Construct validity was assessed considering headache and neck pain frequency and intensity, and self-reported questionnaires, including the Headache Impact Test – 6 items (HIT-6), the 12-item Allodynia Symptom Checklist/Brazil (ASC-12), and the Neck Disability Index (NDI). In addition, participants performed cervical endurance and maximal voluntary isometric contraction of the cervical flexors.
ResultsA total of 103 women with migraine were recruited. The intra-examiner reliability was rated as good (ICC= 0.81, 95% CI: 0.73, 0.87), while the inter-examiner reliability was rated as moderate (ICC= 0.55, 95% CI: 0.40, 0.67). The intra and inter-examiner SEM were 1.31 and 1.36 mmHg respectively, and MDC were 3.63 and 3.77 mmHg. The HIT-6 and the cervical endurance flexion test were associated with the CCFT in a multiple linear regression model (p = 0.004, R = 0.35).
ConclusionThe CCFT presents adequate intra- and inter-examiner reliability. Better performance on the CCFT test was associated with better HIT-6 scores and greater cervical endurance time, which was not influenced by the presence of neck pain.
Migraine is a primary headache that ranks second among the most prevalent neurological diseases, leading to healthcare costs and lost working days.1 It is a chronic disease affecting more than 1 billion people in all regions, cultures, and socioeconomic levels worldwide.2,3 The clinical presentation consists of a headache, typically unilateral, pulsatile, of moderate to severe intensity lasting between 4 and 72 h, accompanied by nausea and/or vomiting, photophobia, and phonophobia.4
Neck pain is also a frequent symptom among patients with migraine,5,6 associated with the chronicity process of the disease, delay in drug treatment effect, and increased disability related to headache.7,8 Besides neck pain, patients with migraine also exhibit cervical dysfunctions, including altered cervical mobility, increased sensitivity, postural changes, and changes in muscle parameters characterized by reduced strength, endurance, and performance of the cervical flexor muscles.9,10
The Craniocervical Flexion Test (CCFT) is used to evaluate the function of the deep neck flexors (longus capitis and longus colli muscles) when performing a craniocervical flexion movement.11 Although there is evidence showing that patients with migraine present musculoskeletal dysfunctions of the cervical spine, some studies suggest that not all patients with migraine will develop such dysfunctions.12,13 Thus, the clinical assessment of patients with migraine is essential for identifying potential associated cervical dysfunctions and planning tailored management strategies. The assessment should be based on appropriate instruments with established measurement properties.14,15
The CCFT is a reliable and valid, but poorly responsive, test for healthy individuals and those with primary neck pain disorders.16-20 The CCFT correlates with disability measures, pain intensity,14 cervical flexor endurance, and maximal isometric voluntary contraction (MVIC) in patients with neck pain.20 Although most patients (about 70%) with migraine may present with neck pain; there is no agreement in the literature on the presence of an altered muscle function similar to that observed in primary neck-related conditions.21-23
In the population of patients with migraine, the CCFT has been considered one of the most clinically useful assessment tests.24 Despite this recommendation, only one study has investigated measurement properties of the CCFT, that is the discriminant validity, in people with migraine. The results showed that the CCFT could discriminate people with and without migraine but could not discriminate between people with migraine with and without associated neck pain.24 Therefore, the basic measurement properties of the CCFT, such as reliability and construct validity, have not been evaluated in people with migraine.
The aim of this study was to determine the measurement properties of the CCFT, including intra- and inter-examiner reliability, construct validity, standard measurement error (SEM), and minimal detectable change (MDC) in patients with migraine.
MethodsThe study was approved by the Research Ethics Committee of the Ribeirão Preto Medical School of the University of São Paulo (CAEE: 54774022.5.0000.5440). All participants received and signed the Informed Consent Form before data collection. This study followed the recommendations of the COnsensus-based Standards for selecting health Measurement INstruments (COSMIN), which classifies as excellent a sample size of at least 100 participants for reliability and validity studies.25
Women with migraine between 18 and 55 years old and who reported at least three days of headache in the last month were included. Patients were screened in the Headache Ambulatory Clinic of the Hospital das Clínicas de Ribeirão Preto (HCRP) and were also recruited from the population of Ribeirão Preto and the region, and were invited to participate through social media. Experienced neurologists diagnosed migraine for all the women included, based on the criteria listed in the 3rd Edition of the International Classification of Headache Disorders, characterised by a moderate to severe headache lasting 4–72 h, unilateral and pulsatile, accompanied by nausea and/or photophobia, phonophobia, and exarcebated by physical activity.4 The exclusion criteria were pregnancy, uncontrolled systemic diseases, history of trauma to the face and/or neck region, and having received an anesthetic block in the craniocervical region in the last three months.
EvaluationThe evaluation was performed between migraine attacks (the interictal period), and all assessment conditions, instructions, and the environment were standardized and similar between assessments. Patients attended two evaluation appointments with an interval of 7–10 days. On the first visit, information was collected regarding clinical and anthropometric characteristics, such as age, body mass index (BMI), headache, and neck pain frequency (pain days/month) and intensity. The CCFT was administered to the participants by examiners A and B in a simple randomized order, with an interval of approximately 15 min between evaluations. While the participants waited for the second evaluation round with the CCFT, they completed the Headache Impact Test (HIT-6), the 12-item Allodynia Symptom Checklist/Brazil (ASC-12/Brazil), and the Neck Disability Index (NDI) questionnaires. On the second visit, the CCFT was adminnistered again to the participants by examiner A, along with the cervical flexor endurance test and the MVIC of the neck flexor muscles. After all physical tests, participants were asked whether they had headache or neck pain and the pain intensity was recorded using the Numerical Pain Rating Scale (NPRS, 0–10 points).
The HIT-6 consists of six questions that assess the impact of headache on the individual's life. The participant answers the questions using a 5-choice scale (6= never, 8= rarely, 10= sometimes, 11= often, 13= always), and the final score ranges between 36 and 78.26,27 The ASC-12/Brazil questionnaire evaluates the presence and severity of cutaneous allodynia, and the total score ranges from 0 to 24 points.28,29 The NDI questionnaire consists of 10 questions assessing the influence of neck pain on activities of daily living, such as personal care, sleep, and reading. The maximum score of the items is 5 points, and the total score ranges from 0 to 50 points.30,31 In all the questionnaires, the higher the score, the worse the disability or allodynia. Our hypotheses were that the CCFT would have a strong to moderate negative correlation with these questionnaires, based on previous literature that shows that these patients have these dysfunctions,9,10 which were also correlated with the test in other patient populations.18,20
The CCFT evaluates the performance of the deep cervical flexors by their activation and resistance during five progressive stages of craniocervical flexion movement.11 Participants were positioned supine with relaxed lower limbs, and a pressure biofeedback unit (Stabilizer Pressure Biofeedback®; Chatanooga, Hixson, TN, USA) was placed behind the individual's neck near the occipital region. The unit was inflated to a baseline pressure of 20 mmHg and the participants were asked to perform a head flexion movement. To familiarize them with the test, the participants were instructed to perform a progressively stronger effort in 2 mmHg increments until reaching the maximum pressure of the test, which is 30 mmHg. In this familiarization trial, participants were instructed to avoid compensations, such as head retraction or elevation, mouth opening, and simultaneous contraction of the sternocleidomastoid and anterior scalene muscles, verified by the examiner's manual palpation. To perform the test, the participant had to sustain the craniocervical flexion movement for 10 s in each stage, with an interval of 30 s between stages, until completing the five stages. No instructions regarding compensations were given after familiarization. The last stage in which the participants could sustain the muscle contraction without performing the above mentioned compensations was recorded by the assessor.
Examiners A and B were both female, 25 years old, and had a bachelor's degree in physical therapy. They both underwent a 20-hour training program conducted by a highly experienced physical therapist with over five years of clinical expertise in utilizing the CCFT. During the training, the examiners practiced administering the test, focusing on the correct technique and verbal instructions.
The cervical flexor endurance test asesses the capacity of the superficial and deep muscles along the head and along the neck to maintain the craniocervical flexion movement associated with neck flexion.32 Participants were placed in a supine position. Then, they were asked to perform the craniocervical flexion movement, such as nodding, followed by neck flexion until raising the head off about 2 cm the supporting surface. Time was recorded in seconds, and the test was stopped when the participant could not sustain craniocervical flexion, i.e., only neck flexion was maintained,33 or they reported pain.
The MVIC of the neck flexor muscle group was assessed using a hand-held isometric dynamometer (Lafayette InstrumentCompany®, model 2201163, Lafayette, IN, USA). The participants remained seated on a backless bench to avoid exerting force with the torso, with their feet resting on the floor, and the device was positioned in contact with the forehead region. Patients were instructed to perform maximum contraction of the cervical flexor muscles for 3 s, maintaining a static neck position.34 The peak force in kilogram-force (kgf) produced by the participants was recorded for 3 repetitions with an interval of 20 s between each repetition. Verbal commands were used to stimulate maximal effort.35 Based on the literature,9,10,18,20 for both endurance and cervical strength, our hypothesis was that these measurements would have a moderate to strong positive correlation with performance on the CCFT.
Statistical analysisDescriptive analysis was based on means and standard deviations for continuous variables, medians and interquartile ranges for categorical variables. Inter- and intra-examiner reliability was estimated using the intraclass correlation coefficient (ICC)(2,1) and considered the following classification: ICC < 0.50 poor reliability, ICC 0.50–0.75 moderate reliability, ICC 0.76–0.90 good reliability, and ICC > 0.90, excellent reliability.36 The standard error measurement (SEM) was calculated as:
Therefore, SD1 is the standard deviation of the observation of evaluator 1 while SD2 is the standard deviation of evaluator 2 and the ICC agreement is the result of calculating the ICC for these two evaluators. For the intra-rater calculation, SD1 is replaced by the SD of the first assessment and SD2 by the SD of the second recording session.37 The minimum detectable change (MDC) was calculated by 1.96 * √2 * SEM.38
We hypothesized that the frequency and intensity of migraine and neck pain, headache disability, allodynia, neck disability, reduced cervical flexion endurance, and MVIC would be correlated with performance on the CCFT, because these variables are frequently related in patients with migraine and are correlated with the CCFT in patients with neck pain.9,10,14,20 Due to the complexity of the migraine condition, the construct validity was determined by backward multiple linear regression considering the above-mentioned clinical variables to assess the relationship with variability in CCFT performance. The strength of association was determined using coefficient (B), R², adjusted R², R, and p values. Furthermore, standardized beta coefficients (β) were included for all variables in the final model to allow direct comparisons regarding the correlation between variables. Correlation values lower than 0.40 indicate weak correlation; 0.40 to 0.69 moderate correlation; and greater than 0.70 strong correlation.39 The sample was stratified into subgroups to perform an exploratory analysis according to the presence or absence of neck pain. We performed this additional analysis solely for data exploration purposes. The Mann-Whitney test was performed according to the absence of normal distribution.
The significance level adopted was α = 0.05. All statistical analyses were performed using the Statistical Package for the Sciences (SPSS, version 20.0).
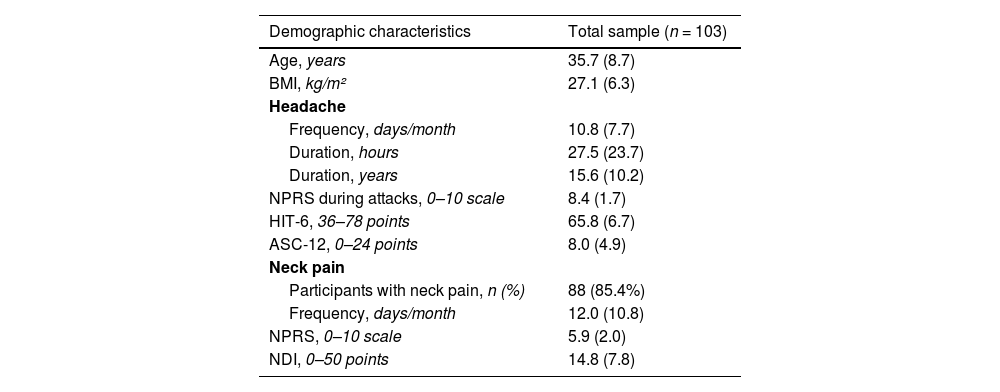
ResultsThe mean (SD) age of the participants was 35.7 (8.7) years old, with an average of 10.8 (7.7) headache days per month, and of high pain intensity (8.4 [1.7]). The participants were classified as having severe headache impact (65.8 [6.7]) and moderate allodynia (8.0 [4.9]). About 85.4% of the participants reported neck pain. There was a frequency of 12 (10.8) days of neck pain per month of an intensity of 5.2 (2.0) on the NPRS. They were classified as having moderate neck pain-related disability (14.8 [7.8]) (Table 1).
Demographic and clinical characteristics of patients with migraine (n = 103).
Data are mean (standard deviation) unless otherwise stated.
ASC-12, 12-item Allodynia Symptom Checklist; BMI, body mass index; HIT-6, Headache Impact Test; NDI, Neck Disability Index; NPRS, numerical pain rating scale.
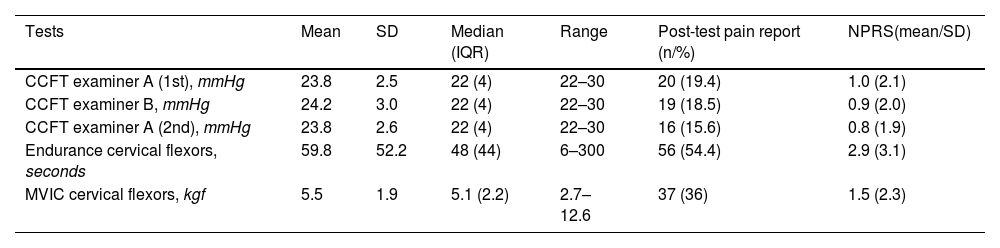
The mean (standard deviation) CCFT performance for examiner A in the first assessment, examiner B and examiner A in the second assessment was 23.8 (2.5), 24.2 (3.0), and 23.8 (2.6) mmHg, respectively. About 19.4%, 18.5%, and 15.6% had pain after the test, for each assessment occasion, respectively. The mean cervical flexor muscle endurance was 59.8 (52.2) seconds, and for this test, 54.4% reported pain after the test. The mean MVIC of the cervical flexor muscles was 5.5 (1.9) kgf, and 36% of the participants reported pain after the test (Table 2).
Clinical performance of participants with migraine (n = 103).
CCFT, Craniocervical Flexion Test; IQR, interquartile range; MVIC, maximal voluntary isometric contraction; NPRS, numeric pain rating scale; SD, standard deviation.
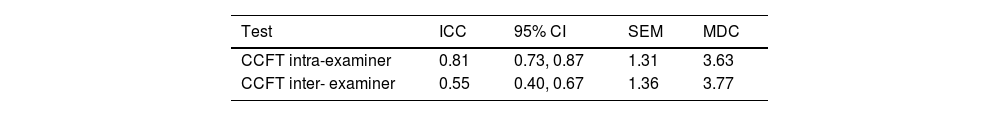
The results of intra- and inter-examiner reliability, SEM, and MDC are shown in Table 3.
Intra- and inter examiner reliability of Craniocervical Flexion Test (CCFT) (n = 103).
| Test | ICC | 95% CI | SEM | MDC |
|---|---|---|---|---|
| CCFT intra-examiner | 0.81 | 0.73, 0.87 | 1.31 | 3.63 |
| CCFT inter- examiner | 0.55 | 0.40, 0.67 | 1.36 | 3.77 |
95% CI, 95% confidence interval; CCFT, Craniocervical Flexion Test; ICC, intraclass correlation coefficient; MDC: minimal detectable change (mmHg); SEM, standard error measurement (mmHg).
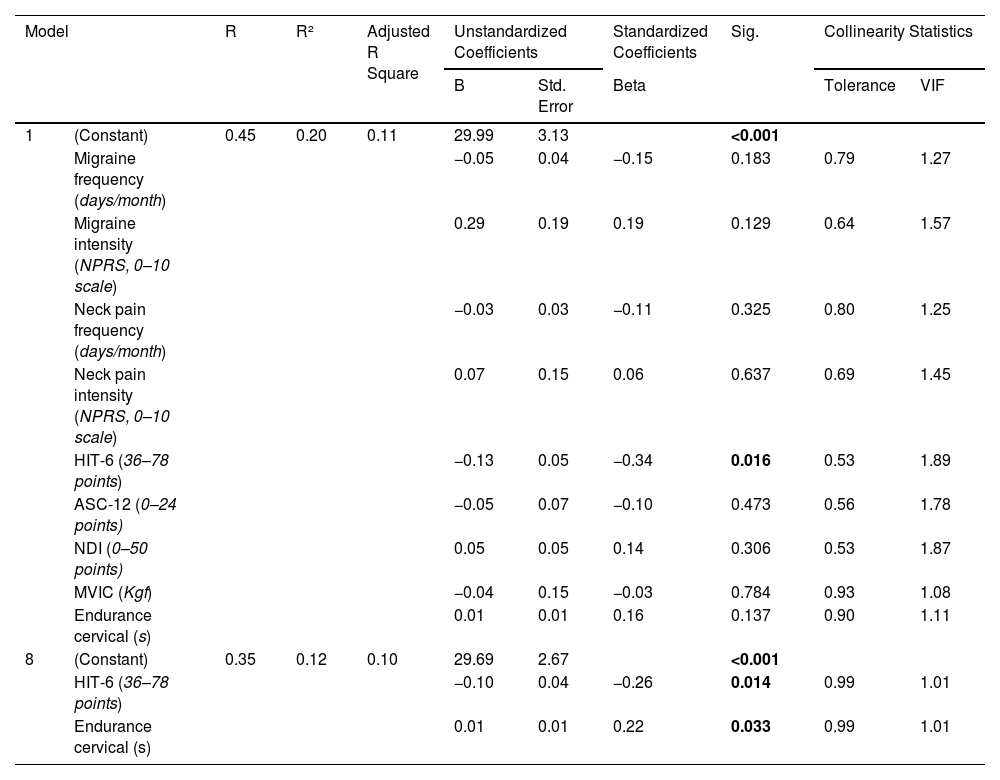
A statistically significant model was found by backward multiple linear regression (F(2.85)= 5.93; p = 0.004, R = 0.35 R²= 0.12). The total score on the HIT-6 questionnaire (β= −0.26; t= −2.50; p = 0.014) and cervical endurance time (β= 0.22; t = 2.17, p = 0.033) are considered significant predictors of performance in the CCFT (Table 4).
Craniocervical Flexion Test prediction variables (n = 103).
ASC-12, 12-item Allodynia Symptom Checklist; HIT-6, Headache Impact Test; kgf, kilogram force; MVIC, maximal voluntary isometric contraction; NDI, Neck Disability Index; NPRS, numeric pain rating scale; S, seconds; VIF, variance inflation factor. Bold font indicates significant p values.
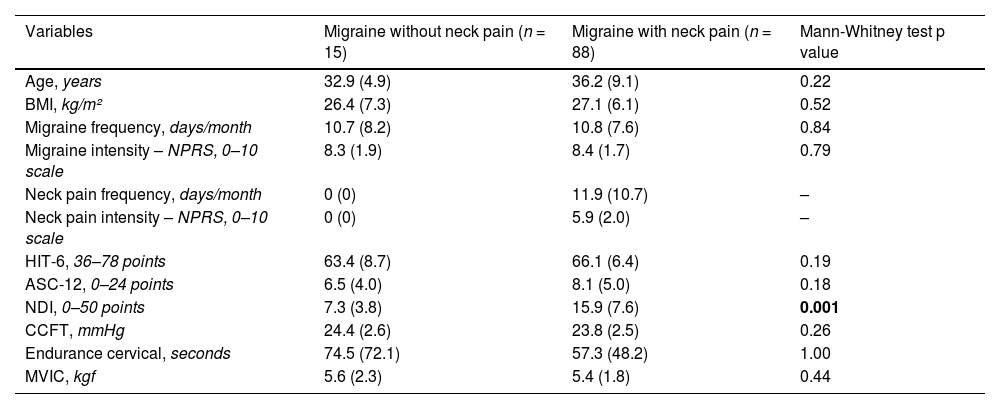
According to the subgroup analysis of patients with migraine stratified by the report of neck pain, a significant difference was observed for the NDI scores (p < 0.001), without further differences in the remaining outcomes (Table 5).
Mean and standard deviation for the difference between groups reporting neck pain (n = 103).
The CCFT demonstrated good intra-examiner reliability and moderate inter-examiner reliability. It was possible to determine the SEM (1.31 and 1.36 mmHg) and the MDC (3.77 and 3.65 mmHg). The construct validity hypothesis was partially confirmed through the association between the CCFT, headache disability, and cervical flexor endurance, in which there was a weak and negative correlation with HIT-6 and a weak and positive correlation with cervical endurance. Our exploratory analysis comparing subgroups of participants with and without neck pain showed no between-group differences for the clinical and physical characteristics, except for neck disability.
The intra-examiner and inter-examiner reliability of the CCFT has been tested previously in healthy subjects and those with neck pain.14,16-18,40,42 Our results differ from reliability among asymptomatic individuals, which resulted in high intra- and inter-examiner reliability (ICC 0.99 and ICC 0.91, respectively).16 In individuals with idiopathic neck pain, the intra-examiner reliability of the CCFT was also excellent for both intra- (ICC 0.85) and inter-examiner (ICC 0.86).18 The results of a previous study supported the use of the CCFT as an objective outcome measure in the assessment of the deep flexor muscles of the neck, but this cannot be generalized to patients with pathologies, thus suggesting the need to conduct further studies to assess the measurement properties of the test in other populations.16 Although our data indicate that the test did not achieve high reliability, it is necessary to emphasize that due to the characteristics of migraine, these patients have lower performance in the test, and this is associated with greater headache disability and also with reduced cervical endurance. Therefore, it is not possible to generalize the context of other pathologies for the performance of the test in patients with migraine. In fact, it is necessary to take into account that the condition has particularities that need to be investigated in a general context.
The SEMs are equivalent to less than 2 mmHg, which is one stage in the test. On the other hand, MDCs were above one stage in the CCFT. Therefore, any improvement in performance in patients with migraine that exceeds this threshold is indicative of a significant change in performance. In healthy subjects, the SEM was 0.73 and 0.29 mmHg, respectively for inter- and intra-examiners.16 Nevertheless, in patients with neck pain, the SEM was 1.55 mmHg and 1.64 mmHg, and therefore less than one stage (2 mmHg) is related to real change, exceeding the error. A previous study in patients with neck pain verified an MDC of 4.30 mmHg and 4.53 mmHg for intra- and inter-examiners, suggesting that two or more stages are needed to detect a real change.17 This would consequently negatively impact CCFT measurement capacity at different time points, considering that the test has only five stages.17 Although the MDC for intra- and inter-examiners in patients with migraine were numerically lower, they indicate that changes should also exceed two CCFT stages to be detected as observed for patients with neck pain.
Approximately 12% of the variability in CCFT performance is related to greater headache-related disability and lower cervical muscular endurance. There was a negative significant association between the CCFT and the HIT-6 questionnaire, which means that a lower level of disability is associated with better performance in the CCFT. Meanwhile, there was a positive association between the CCFT and cervical muscular endurance time, which suggests that higher cervical endurance is associated with better performance in the CCFT. In a sample with neck pain, the CCFT negatively correlated with neck disability, neck pain intensity, and quality of life.18 Similarly, better performance in the CCFT indicated better cervical muscular endurance and MVIC.20
Part of our hypothesis about the construct validity of the CCFT may be confirmed. Our initial hypotheses were that there would be a moderate to strong positive correlation between the CCFT and cervical muscular endurance and strength. Furthermore, we hypothesized moderate to strong negative correlations with the intensity and frequency of migraine and neck pain, as well as disability associated with headache and neck pain, and allodynia. Despite this, the CCFT demonstrated weak correlations with two factors: headache disability and cervical endurance. These results can be attributed to the complexity of the clinical presentation of migraine, a central nervous system disease in which there are particularities in the pathophysiology of the disease. The cervical manifestations in migraine are explained by the sensitization process of the trigeminocervical complex that occurs through inputs from nociceptive afferents from the meningeal vessels, the trigeminal nerve branches, and the cervical roots of C1-C3.42-44 Patients with migraine have altered performance compared to individuals without headache, but there are no differences compared to patients with neck pain and those without neck pain.23-45 Although clinical performance is altered in patients with migraine with and without neck pain and those with only neck pain, patients with migraine show hyperactivity of the superficial cervical antagonist musculature and not the flexor musculature.22,46,47 These results may indicate that these patients adopt a different compensation pattern characteristic of the migraine clinical presentation, a factor that needs to be better investigated. In addition to the differences related to the particularity of migraine and other diseases, we performed a multiple linear regression that considers the correlation between variables and the influence of all variables on the outcome, different from the simple correlation in other articles.14,18,21
In this study, there were no clinical differences between patients with migraine when stratified in subgroups with and without neck pain, except in neck disability. These results should be interpreted with caution, considering the sample size of each group, with only 15 participants who did not have neck pain compared to 88 who had neck pain. However, these results are in agreement with previous epidemiological studies, which suggested that more than 75% of patients with migraine report neck pain6,48 and that cervical musculoskeletal dysfunction is present in the migraine clinical presentation independently of the report of neck pain.9,10
This study has some limitations. It did not include men, so the results cannot be generalized to both sexes. There is a higher occurrence of migraine among women than men, and there is no difference in performance in the CCFT between men and women.49 Another limitation is that the CCFT is a tool that has subjective components making it difficult for patients to perform the necessary movement and for clinicians to ensure that compensations are not taking place. The gold standard method for assessing deep flexor muscles is through intranasal EMG, but it is an invasive procedure that creates discomfort for patients.11,51,50 In addition, despite adhering to the COSMIN checklist for the study of measurement properties,25 we did not use tools to objectively measure the maintenance of the patients’ state of health. Although the assessment of the patients’ health status was based solely on self-report, which may have influenced the study methodology, the patient's perspective during the migraine cycle is important because it ensures applicability in real-world clinical settings. Additionally, it is important to acknowledge that the MVIC cervical measurement did not involve trunk stabilization, potentially allowing for the participation of trunk flexors in the effort exerted during the test. This aspect may influence the test's ability to exclusively assess neck flexors. Despite these limitations, this study, to our knowledge, was the first to determine the reliability and construct validity of the CCFT in patients with migraine.
ConclusionThe intra- and inter-rater reliability of the CCFT was considered good and moderate, respectively, for patients with migraine. The intra- and inter-examiners SEM were equivalent to less than one test stage, while both MDC were equivalent to two CCFT stages. Construct validity showed a significant positive but weak correlation with cervical endurance and a significant negative and weak correlation with headache disability.
This Project was supported by São Paulo Research Foundation (FAPESP) (grant number 2021/14588-6). The funders did not have any influence on study design, data collection and/or analysis, decision to publish, or preparation of the manuscript.