Pulmonary and upper limbs function of children with Duchenne muscular dystrophy (DMD) are known to deteriorate throughout the disease process. However, there is a lack of information on the extent of impairments in the early stages of DMD when compared to healthy peers.
ObjectiveTo investigate to what extent pulmonary and upper limbs function of children with early stage DMD are impaired.
MethodsSixty-one children participated in the study: 31 with Grade 1 DMD (study group) according to the Brooke Upper and Lower Extremity Functional Classification Systems, and 30 age matched healthy peers (control group). Pulmonary function was determined with pulmonary function tests. The Performance of Upper Limb test was used to evaluate the upper limbs function.
ResultsStudy and control groups were homogenous in terms of physical characteristics (p>0.05). Pulmonary and upper limbs function of children with DMD were about 85% and 93% of healthy peers, respectively.
ConclusionThis study provides evidence for deterioration of pulmonary and upper limbs function in children with early stage DMD. Better knowledge of deterioration rate over time may help therapists to better plan and update their plan of care.
Duchenne muscular dystrophy (DMD) is a hereditary disease characterized by proximal muscle weakness with an incidence of 1 in 3600 male live births.1,2 The first symptoms of DMD are a positive Gowers’ sign and difficulty in climbing stairs and tip-toeing, frequent falls, and fatigue.3 Although DMD is generally diagnosed by genetic testing around the age of four to five years, new prenatal diagnostic tools have been developed in recent years.4,5 Loss of ambulation occurs at approximately 12–13 years of age, when children become wheelchair-bound. Life expectancy is less than 30 years due to pulmonary and cardiac complications.6,7
Pulmonary problems occur secondary to progressive respiratory muscle weakness, which leads to deterioration in the ability to inhale, exhale, and producing effective coughing, eventually resulting in progressive morbidity and eventually death.8,9 Ricotti et al.10 showed that pulmonary function declined in the early stage of DMD even with corticosteroid use.10 According to the guidelines for standards of care for DMD, pulmonary function tests (PFTs), including forced vital capacity (FVC), forced expiratory volume in one second (FEV1), and peak expiratory flow (PEF) values are required at least annually for ambulatory children aged six years and older, and at least every six months for non-ambulatory children.11
In recent years, the lifespan of children with DMD has increased as a result of the developments of new therapeutic approaches,12 and improved knowledge of families regarding care.13 Preservation of upper limbs function, which starts to be affected from the early stage of disease, is important for the ability to continue performing daily activities.14,15 Deterioration in upper limbs function becomes apparent as early as 12 years of age, after the loss of ambulation, and this adversely affects daily life.16,17 Excessive efforts to train upper limbs function have also been reported to cause fatigue and activity limitations.14,18 It is recommended that along with pulmonary tests, physical assessment that include evaluation of both upper and lower limbs function be conducted every four to six months.5,11
While it is known that pulmonary and upper limbs function start to show impairments in the early stage of DMD, as do trunk and lower limbs function,19,20 only one study evaluated the impairment of both pulmonary and upper limbs function at this stage in younger individuals.10 Determining the extent and rate of impairments in the early stage of DMD is critical to optimize therapeutic approaches. Thus, this study aims to investigate the extent of pulmonary and upper limbs function deficits in children with early stage DMD compared to healthy peers.
MethodsParticipantsA total of 61 participants, including 31 individuals with DMD and 30 age-matched healthy peers were included in the study. Inclusion criteria for individuals with DMD were: aged between 5 and 10 years, being on treatment with corticosteroids for more than six months, and being at Grade 1 based on the Brooke's Upper and Lower Extremity Classification Systems.21 For the healthy control group, criteria were being between 5 and 10 years of age and being free of any musculoskeletal, neurological, or cardiopulmonary diseases. Based on the data from a pilot study conducted with 10 participants (5 DMD and 5 healthy peers), it was determined that a total of 26 children (13 for DMD and 13 for control groups) would be needed for the power of the study to be 80%. The current study was completed with 61 participants.
Ethical approval for the study was given by the Hacettepe University, Ankara, Turkey Non-invasive Clinical Researches Ethical Committee (protocol number: GO16/773). Written consents were signed by both participants and their families.
AssessmentsAge (years), height (cm), weight (kg), and body mass index (kg/m2) of all participants were recorded. Moreover, corticosteroid treatment duration of children with DMD was reported by their families.
The functional level of the participants with DMD was assessed with the Brooke Functional Classification Systems for both upper and lower limbs. Only individuals with DMD whose functional level was classified as Grade 1 (starting the movement while arms are beside the trunk and folds hands completely above head, and walks and climbs stairs without assistance) were included in the study.21
Pulmonary function of the participants was evaluated with spirometry using the Spirobank G USB device, and the data were transferred to the computer via Winspro software. The tests were conducted in accordance with the American Thoracic Society guidelines.22 All participants were required to perform at least three force expiratory maneuvers, and the highest reproducible values of FVC, FEV1, and PEF were recorded. Normative values of pulmonary function are derived from a study that included healthy individuals aged 3–95 years.23
Upper limbs function was evaluated with the performance of upper limb (PUL) scale. This scale has a total of 22 items and has been shown to be reliable when used with individuals with DMD. It consists of three sub-scales: high (shoulder level), middle (elbow level), and distal (hand level). The PUL scale also has four items determining timed performance. The total score ranges from 0 to 74, where higher scores indicate a higher level of function.24
Assessment procedureAll assessments were performed by a physical therapist with four years of experience with pediatric patients with neuromuscular disorders. All assessments were conducted within a single session. There was a 5-min interval between tests to prevent fatigue. Assessment for each participant was performed according to the order above. All measurements were completed within one-hour.
Statistical analysisThe IBM SPSS Statistics 20 (Statistical Package for the Social Sciences) statistical analysis program was used to analyze the data. Descriptive characteristics were provided as mean±standard deviation or median and interquartile range (25th–75th percentiles) for the quantitative data, while number (n) and percentages (%) were used for qualitative data. Kolmogorov–Smirnov test was used to determine the conformity of the data to normal distribution. Because the variables did not fit the normal distribution, Mann–Whitney-U test for non-parametric conditions was performed to analyze the differences between both the groups. The statistical significance level was set at 0.05.
ResultsThe physical characteristics of the participants are shown in Table 1. Mean±standard deviation for treatment duration of corticosteroid was 23.35±12.04 months.
Physical characteristics of participants.
| DMD group (n=31) | Healthy peers (n=30) | p values | |
|---|---|---|---|
| Mean±SD | Mean±SD | ||
| Age (years) | 6.67±1.32 | 7.19±1.55 | 0.2 |
| Weight (kg) | 23.44±5.03 | 27.36±8.85 | 0.1 |
| Height (cm) | 118.54±11.20 | 129.40±11.07 | 0.001 |
| Body mass index (kg/m2) | 16.59±2.02 | 15.96±2.93 | 0.3 |
DMD, Duchenne muscular dystrophy. Data are mean±standard deviation.
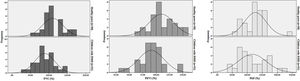
Data distribution for the PFTs for both groups is shown in Fig. 1. The results for the healthy group (FVC and FEV1) were higher than for those with DMD (p<0.05, Table 2). The values for the PFTs of children with DMD were approximately 85% of those of the healthy group.
Pulmonary function values of children with DMD and healthy peers.
| DMD Group (n=31) | Healthy peers (n=30) | p values | |||||
|---|---|---|---|---|---|---|---|
| Median | Percentiles | Median | Percentiles | ||||
| 25th | 75th | 25th | 75th | ||||
| FVC (%) | 85.0 | 71.0 | 106.0 | 102.0 | 90.7 | 130.5 | 0.009 |
| FEV1 (%) | 92.0 | 81.0 | 103.0 | 104.5 | 93.7 | 127.2 | 0.005 |
| PEF (%) | 107.0 | 80.0 | 157.0 | 129.5 | 95.7 | 147.7 | 0.3 |
DMD, Duchenne muscular dystophy; FVC, forced vital capacity; FEV1, forced expiratory volume in one second; PEF, peak expiratory flow. Normative values are derived from Quanjer et al.23
Table 3 provides the data for upper limbs function for both groups. Children with DMD scored 4.6 points lower than healthy children on the PUL total score (p<0.05), which was about 93% of the performance by their healthy peers. Healthy children completed the performance items that evaluate lifting and stacking of light and heavy cans (timed items of PUL) in a shorter time than children with DMD (p<0.05).
Upper limbs function in children with DMD and healthy peers.
| DMD group (n=31) | Healthy Peers (n=30) | Difference between groups | p values | |
|---|---|---|---|---|
| Mean±SD | Mean±SD | Mean (95% CI) | ||
| PUL – high level (0–16 points) | 11.8±2.5 | 15.5±1.3 | 3.5 (2.5, 4.5) | <0.001 |
| PUL – middle level (0–34 points) | 33.4±0.8 | 33.9±0.4 | 0.5 (0.3, 0.8) | 0.001 |
| PUL – distal level (0–24 points) | 23.6±0.6 | 23.9±0.3 | 0.3 (0.1, 0.6) | 0.006 |
| PUL – total score (0–74 points) | 68.8±2.9 | 73.4±1.6 | 4.4 (3.2, 5.6) | <0.001 |
| Timeditems of PULa | ||||
| Lifting light cans (item I) | 5.1±1.0 | 4.5±1.0 | 0.5 (0.0, 1.1) | 0.02 |
| Lifting heavy cans (item J) | 6.3±1.4 | 4.9±1.0 | 1.3 (0.6, 2.0) | <0.001 |
| Stacking light cans (item K) | 7.8±1.0 | 7.0±1.2 | 0.9 (0.3, 1.4) | 0.004 |
| Stacking heavy cans (item L) | 8.9±1.4 | 7.3±1.7 | 1.5 (0.6, 2.4) | <0.001 |
DMD, Duchenne muscular dystrophy; PUL, the performance of upper limb. Data are mean±standard deviation.
This study investigated the difference in pulmonary and upper limbs function in children with early stage DMD in comparison to healthy, age-matched children. Pulmonary and upper limbs function in children with DMD were found to be 15% and 7% lower, respectively.
Meier et al. showed that the deterioration in pulmonary function of children with DMD between 10 and 18 years of age progressed with age.20 Others have reported that pulmonary function starts declining at about 10 years of age with the loss of ambulation.11,25 In addition, a recent study suggested that pulmonary function declined in the early stage of DMD when compared to normative values, although healthy peers were not included in the study.10
Our study found that pulmonary function of children with DMD was significantly worse than that of healthy children, even at six to seven years of age. Moreover, in the current study, children with DMD had lower pulmonary function not only compared to their healthy peers but also when compared to normative values.26,27 Typically, training to enhance pulmonary function is not done in the early stage of the disease; because the primary deficits at that time are weakness in the lower limbs and trunk muscles. Because weakness primarily affects the antigravity muscles, physical therapy interventions tend to focus on improving ambulatory activities. Therefore, pulmonary interventions, such as manually assisted coughing and respiratory muscle training, are provided primarily after the loss of ambulation. However, the results of the current study suggest the clinical importance of timely intervention to maintain pulmonary function starting in the early stage of DMD.
Authors of a study that evaluated upper limbs function in adults with DMD, reported better function in early adulthood compared to late adulthood.17 Moreover, shoulder level activities have been found to be affected as soon as muscle weakness appears in the proximal muscles of the upper limbs, even in the early stages of the disease and to worsen with the loss of ambulation.28,29 In another recent study, the decrease in the total score for the PUL scale over 24 months was 2.07 points in ambulatory boys with DMD and 4.36 points in non-ambulatory boys.30 The current study shows a more than 4 points lower total PUL scores in children in early stage of DMD, which should be considered in the clinical management of these children.
There is also conflicting evidence in the literature regarding distal upper limbs function at the later stages of DMD. A group of researchers noted the preservation of distal upper limbs function responsible for manipulation of devices, such as wheelchair joysticks, while another group reported weakness related to pinch strength.17,31 Therefore, except for the distal aspect of the upper limbs, there is a consensus in the literature that upper limbs function starts declining in the early stage of DMD and deficits progress with age.14,18,32
It has also been reported that upper limbs function is impaired in the early stages of DMD even with corticosteroid usage.10 Although the clinical implications are unclear taking into account group differences regarding timed items, sub and total scores of PUL, the current study found lower upper limbs function in children with DMD compared to their healthy peers. While a 7% impairment between groups may not yet be clinically significant, it was present despite the approximate 24-month corticosteroid usage of the DMD group.
Based on the results of this study, children who have DMD are at risk of experiencing deterioration in their upper limbs function at the early stage of the disease, even if they start using steroids at an average of four years of age, and these results are consistent with the literature. Assessment of upper limbs function at the early stage may help improve awareness of any functional losses and promote early intervention.
A limitation of this study is that it did not include evaluation of upper limbs and respiratory muscles strength. The difference in height between groups is another limitation, as height is known to influence pulmonary function.
ConclusionThe results of this study indicate pulmonary and upper limbs function deficits in children with early stage DMD. These deficits existed despite the absence of any symptoms or complaints related to pulmonary and upper limbs function. This work suggests the need to perform regular thorough evaluation of these children starting early in the disease process to better document the disease course and plan and update physical therapy interventions to improve the quality of life in children with DMD.
Conflicts of interestThe authors declare no conflicts of interest.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.