Adherence to the use of recommended measures/criteria for return to sport clearance after anterior cruciate ligament reconstruction is crucial for successful rehabilitation.
ObjectivesThe purpose of this study was to describe the current clinical practice of Brazilian physical therapists that treat patients after anterior cruciate ligament reconstruction, including the measures/criteria used to support the decision-making process regarding return to sport. The secondary aim was to investigate factors associated with the use of the most recommended measures/criteria for return to sport.
MethodsAn electronic survey questionnaire was sent to Brazilian physical therapists. The survey consisted of questions about demographics and professional and clinical practice data related to anterior cruciate ligament reconstruction postoperative rehabilitation and return to sport criteria. Descriptive statistics and chi-square tests were used for analyses.
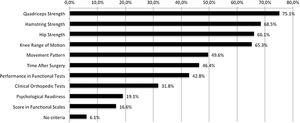
ResultsA sample of 439 professionals participated in the survey. Only 6.4% of the physical therapists use the most recommended measures/criteria for return to sport after anterior cruciate ligament reconstruction. Professional certification in Sports Physical Therapy was the only factor associated with the use of these recommended measures/criteria (p=0.02). The measures most used for return to sport clearance were related to physical factors (65.3% to 75.1%), such as range of motion and muscle strength. A small number of professionals use questionnaires to assess functional (16.6%) and psychological (19.1%) aspects of their patients to support the decision-making process.
ConclusionIn their clinical practice, most Brazilian physical therapists do not use the recommended measures/criteria for return to sport after anterior cruciate ligament reconstruction.
Anterior cruciate ligament reconstruction (ACLR) is a common intervention post anterior cruciate ligament (ACL) injury and associated restrictions in performing sports activities.1,2 Return to sport (RTS) after surgery is often one of the patient's main objectives,3 and it should therefore be one of the primary outcomes sought by physical therapists. Therefore, physical therapists should use validated measures and criteria to determine the patient's readiness to RTS.4,5
The criterion for RTS clearance most frequently used by professionals involved in rehabilitation of individuals post ACLR is the amount of time after surgery,6,7 as it reflects healing and graft maturation.8,9 In addition to time-based criterion, other objective criteria for RTS are necessary to ensure that the patient undergoing ACLR is capable of tolerating the physical demands usually imposed during sports activities.4,10–12 However, the authors of a systematic review reported that only 13% of reviewed studies used objective criteria for RTS, 32% used only a time-based criterion, and 40% did not report any criteria.6 While measures and criteria used to determine RTS after ACLR have been extensively investigated in recent years, there is considerable variation in published recommendations.10,13–16 For example, some studies only evaluated physical and functional factors, ignoring potential psychological aspects involved in RTS.14,15 Other studies also included measures of knee joint laxity17 or movement pattern13,16 in the battery of tests used for clinical decision-making about RTS. Although there is no consensus, the most recommended measures/criteria to assess readiness for RTS after ACLR are based on: quadriceps and hamstring strength, performance during functional tests (e.g., distance achieved during hop tests), patient-reported functional outcome measures, and psychological readiness.5,13,16,18 Thus, these measures should be routinely performed during the postoperative rehabilitation process.
The decision about an individual's readiness to RTS should be performed by professionals who regularly treat patients after ACLR.11,18 Recent data from surveys of American and Australian physical therapists indicate substantial differences in the measures and objective criteria used to define readiness to RTS after ACLR.19,20 However, there are no published data about the clinical practice and criteria used for professionals from other countries to define readiness for RTS. Physical therapists working in Brazil, for example, have difficulties in incorporating scientific evidence into the clinical decision-making process.21,22 Also, clinical experience, academic degree, and specialty certification can influence access to scientific evidence, including recommended criteria for RTS.23 Therefore, the purposes of this study were threefold: (1) to describe the current clinical practice of Brazilian physical therapists that usually treat patients after ACLR; (2) to investigate the measures/criteria that substantiate the decision-making process regarding RTS after ACLR; and (3) to investigate the factors associated with the use of the most often recommended measures/criteria for RTS clearance.
MethodsStudy designThis study was a cross-sectional survey of Brazilian physical therapists. Study protocol was approved by the Research Ethics Committee of the Universidade Federal de Minas Gerais (protocol number: CAAE 51018115.3.0000.5149).
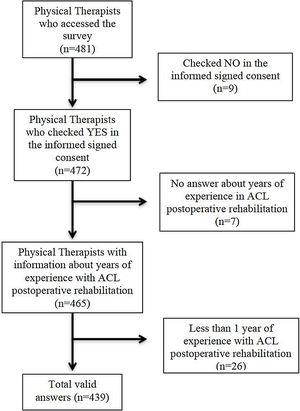
ParticipantsBrazilian physical therapists received an invitation with a link to an electronic survey using Facebook, Instagram, WhatsApp, or e-mail from the Physical Therapy Registration Boards of four Brazilian states (CREFITO) and the Brazilian Boards of Sports and Orthopedic Physical Therapy Specialists (SONAFE and ABRAFITO, respectively). The informed consent form was included in the survey. After selecting “yes” to the question about the informed consent to participate, the physical therapist accessed the survey. If he/she did not agree to participate, the questionnaire was ended. The responses were collected from November 2017 to May 2018. Surveys from physical therapists with less than one year of clinical experience in rehabilitation of ACL injuries, and those who did not answer the question regarding duration of clinical experience were excluded from analysis. A minimum of one-year experience with ACL postoperative rehabilitation was considered the minimal required clinical expertise.
ProceduresAn electronic survey questionnaire was developed on the online platform Google Forms according to evidence gathered from the literature. Six experienced physical therapists reviewed the questionnaire, and all suggestions were considered for the elaboration of the final version of the electronic survey (Appendix A). This survey contained items separated in four sections: (1) a brief description of the research purpose and procedures; (2) the informed consent form; (3) demographic and professional data, such as sex, age, primary practice setting, highest level of education, and years of experience in ACL injury rehabilitation; and (4) six questions about clinical practice related to ACLR postoperative rehabilitation, including the measures/criteria used to define RTS. In the survey, we considered RTS as the return to sports practice with an eventual goal to return to full participation. The physical therapist was allowed to select as many alternatives as he/she considered appropriate in the questions related to the measures/criteria for RTS clearance. The estimated time to complete the questionnaire was about 10–15min. Answers were automatically saved in an Excel spreadsheet and stored on the Google server.
This study followed the recommendations of the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) statement guideline.24
Data analysisDescriptive analysis was used to characterize the demographic and professional data of the participants. The responses about clinical practice post ACLR, including the criteria for RTS, were analyzed using frequency and percentage measures. Chi-square tests with Yates’ continuity correction tested the association between the use of the main measures/criteria recommended for RTS clearance and the academic degree, the level of experience, and the specialty certification of the physical therapist. The academic degree was operationally defined as a basic academic degree (bachelor's degree) versus a higher academic degree (master's or doctoral degree) practitioners. The amount of experience with ACL rehabilitation was classified into four categories, with a range of four years: 1–4 years; 5–8 years; 9–12 years; and ≥13 years. Level of experience was operationally defined as experienced (13 or more years of clinical experience) versus less experienced (1–4 years of clinical experience) practitioners. The probability of type I error was set at 0.05. All the statistical analyses were performed using SPSS Version 23.0 (Chicago, IL, USA).
ResultsA total of 481 physical therapists accessed the online questionnaire, but nine refused to participate. Of the remaining 472 physical therapists, twenty-six had less than one year of experience with ACLR postoperative rehabilitation, and seven did not answer how much experience they had in clinical practice. These data were excluded. Therefore, the final sample consisted of 439 participants (Fig. 1).
Demographic and professional characteristicsThe data on demographics and clinical practice of the physical therapists who participated in the survey are presented in Tables 1 and 2, respectively. There was a near equal distribution in relation to sex (51.5% female), and the majority (83.6%) of physical therapists were less than 40 years old (mean age=34.2±7.8 years), lived in the southeastern region of Brazil (75.4%), and had completed at least one specialization course (80.2%). Most of the respondents (70.2%) had at least five years of experience with postoperative ACLR rehabilitation (mean=8.4±6.3 years), practiced individualized sessions (62.6%) for recreational or amateur athletes (84.1%), and were in private clinics/offices (66.1%). Most of them did not have specialty certification in Orthopedic Physical Therapy (86.8%) or Sports Physical Therapy (80.6%). One-hundred and sixteen physical therapists worked with sports teams (26.4%). Of these, 50% worked with soccer teams, followed by basketball (15.5%), fighting sports (12.9%), and volleyball (12.1%).
Demographic characteristics of the Brazilian physical therapists (n=439).
| Demographic characteristics | Frequency, n (%) |
|---|---|
| Sex | |
| Female | 226 (51.5) |
| Male | 213 (48.5) |
| Age | |
| 21–30 years | 156 (35.5) |
| 31–40 years | 212 (48.3) |
| 41–50 years | 49 (11.2) |
| 51–60 years | 19 (4.3) |
| 61–70 years | 3 (0.7) |
| Mean±Standard Deviation | 34.2±7.8 years |
| Region of practice | |
| Southeast | 331 (75.4) |
| South | 75 (17.1) |
| Midwest | 12 (2.7) |
| Northeast | 9 (2.1) |
| North | 8 (1.8) |
| Outside Brazil | 4 (0.9) |
| Highest level of education | |
| Bachelor's Degree | 87 (19.8) |
| Specialization Course | 272 (62.0) |
| Master's Degree | 61 (13.9) |
| Doctoral Degree | 19 (4.3) |
Professional characteristics of the Brazilian physical therapists (n=439).
| Professional characteristics | Frequency, n (%) |
|---|---|
| Amount of experience with ACL rehabilitation | |
| 1–4 years | 131 (29.8) |
| 5–8 years | 136 (31.0) |
| 9–12 years | 80 (18.2) |
| ≥13 years | 92 (21.0) |
| Mean±Standard Deviation | 8.4±6.3 years |
| Clinical practice settinga | |
| Private Clinic/Office | 290 (66.1) |
| Clinic/Office with health insurance | 160 (36.4) |
| Sports team | 116 (26.4) |
| Rehabilitation public service | 96 (21.9) |
| Clinic school | 58 (13.2) |
| Home care | 30 (6.8) |
| Others | 28 (6.4) |
| Patients’ activity level profile | |
| Sedentary individuals | 27 (6.2) |
| Recreational athletes | 195 (44.4) |
| Amateur athletes | 174 (39.6) |
| Professional athletes | 43 (9.8) |
| Type of treatment | |
| Collective | 22 (5.0) |
| Individual | 275 (62.6) |
| Individual and Collective | 142 (32.3) |
| Certification in sports physical therapy | |
| Yes | 85 (19.4) |
| No | 354 (80.6) |
| Certification in orthopedic physical therapy | |
| Yes | 58 (13.2) |
| No | 381 (86.8) |
Abbreviation: ACL, anterior cruciate ligament.
38.5% of the respondents indicated that postoperative ACLR rehabilitation is initiated less than one week after hospital discharge; 47.8% indicated that rehabilitation started between 1 and 2 weeks post surgery; and 13.7% indicated starting after three weeks. In the study, 62.1% of participants indicated that the RTS clearance is determined by a multidisciplinary team, 25.1% indicated it is made by the physical therapist, with another 12.8% answering that the decision is made by the orthopedic surgeon.
Most physical therapists recommended a maximum time off sports of 7 months or less (15.3%, 1–3 months; 21.2%, 4–5 months; 41.0%, 6–7 months). Only 21.9% of the physical therapists recommend 8 months or more (17.8%, 8–9 months; 4.1%, 10–12 months) prior to resuming sports activities.
Only 6.1% of the physical therapists who answered the survey do not use any specific measure/criteria for RTS clearance. Most of the measures/criteria used for RTS clearance are related to physical factors, and the majority of physical therapists (>50%) reported frequent use of the following measures: strength of quadriceps, hamstrings, and hip muscles, and knee range of motion (65.3–75.1%) (Fig. 2).
Twenty-eight (6.4%) Brazilian physical therapists reported using all the five measures most often recommended in the literature to determine readiness for RTS after ACLR (quadriceps and hamstring strength, performance during functional tests, score on functional questionnaires, and psychological readiness). Analysis of the factors related to the application of these criteria by the physical therapists showed no association with academic degree (p=0.28), amount of experience (p=0.17), and specialty certification in Orthopedic Physical Therapy (p=0.64). The only factor that was associated with the use of all recommended measures/criteria was having a specialist certification in Sports Physical Therapy (p=0.02).
DiscussionBrazilian physical therapists were surveyed about their current clinical practice in the rehabilitation of patients following ACLR. The survey included questions about their measures/criteria currently used in the decision-making process regarding readiness for RTS. A small number of physical therapists reported using all five primary measures recommended in the literature. Most practitioners indicated the use of criteria related to physical aspects, but the assessment of self-reported functional status and psychological readiness to RTS was neglected by more than 80% of physical therapists. Thus, the results of the present study indicate that there is a wide disparity between the clinical practice of most Brazilian physical therapists and the current scientific evidence in the use of criteria to determine readiness to RTS after ACLR.
Measures and criteria for readiness to RTS after ACLR should not be restricted to physical assessment, as it should also include the evaluation of the athlete's functional and psychological attributes.5,11 In the present study, only a minority of physical therapists (6.4%) reported using a combination of the main measures/criteria recommended in the literature for decision about RTS. The use of the recommended measures/criteria was only associated with the physical therapist being certified specialist in Sports Physical Therapy. Conversely, the amount of time in clinical practice, academic degree, and having a specialty certification in Orthopedic Physical Therapy were not associated with the use of recommended measures/criteria. This result suggests the importance of specialized, practice-oriented continuing education because recommendations based on evidence about RTS appear to be more widely disseminated among members of scientific associations of Sports Physical Therapy. Events and other informative actions (e.g., books and other materials published for professional updates) promoted by these organizations allow frequent updating of the professionals’ knowledge and may facilitate access to high-quality evidence.
Amount of time after surgery was considered a criterion for RTS by approximately half of the physical therapists interviewed (46.5%), and most respondents (approximately 80%) recommended time away from the sport lower than seven months. Traditionally, the recommended period of time prior to RTS has been six months.6 However, Grindem et al. showed that, after six months post ACLR reconstruction, there is a 51% reduction in the risk of new knee injuries for each month RTS is further posponed.14 As there was no additional risk reduction beyond nine months after surgery, this was the period recommended prior to RTS.14 Many authors have argued against an early RTS post ACLR.14,25,26 A systematic review on the ligamentization process in human ACLR demonstrated that this biological process continues for much more than six months.8 However, only about 20% of the participants in the present study reported recommending a time away from sport of 8 months or more, showing the lack of adherence of Brazilian physical therapists to the most recent recommendations. Considering that this recommendation against an early RTS was new when data collection was performed for this study, the majority of respondents may not have had access to this information at the time of the survey.
The amount of time post surgery should not be the only criterion used to evaluate patient's readiness to RTS.5,13,16,18 The return to unrestricted sports activities is a crucial stage in the rehabilitation process.27 Therefore, physical therapists should perform a comprehensive evaluation.5,13,16,18 Although some measures/criteria are widely recommended, the present study showed that most physical therapists prioritize physical parameters to establish the patient's readiness for RTS. In addition, almost one third of the physical therapists utilize clinical orthopedic tests as parameters for RTS. However, these tests (e.g., Lachman and anterior drawer tests) inform only about the passive mechanical stability of the knee joint, not providing information about the improvement on physical attributes and functional status of the patient.28,29 On the other hand, new evidence suggest that post surgery time is an important criterion to guide RTS decisions.14,25,26 However, this criterion should not be used in isolation because it does not in itself ensure physical, functional, and psychological readiness to RTS are met.
In the present study, less than a quarter of physical therapists reported assessing psychological factors potentially associated with RTS. The inclusion of psychological function during the rehabilitation process is essential in this population.30–33 In contrast to the present study, a survey conducted in Australia found that almost 90% of Australian physical therapists consider psychological readiness as part of the criteria to establish RTS after ACLR.19 Several researchers have examined the psychological aspects that impact RTS in individuals undergoing ACLR.30–36 Self-efficacy (ability perceived by the individual to perform a task that exerts demands on the knee) and kinesiophobia (fear of rupture of the graft or contralateral ligament) are psychological factors that can potentially interfere with RTS.34–36 Accordingly, the Anterior Cruciate Ligament – Return to Sport after Injury Scale (ACL-RSI) was developed specifically to assess the psychological readiness to RTS of patients post ACLR.37 Some studies have shown that this scale is capable of discriminating individuals who returned or not to sport after ACLR.30,33 Also, a score higher than 56 points on this scale was suggested as a criterion for RTS clearance.13,16 To facilitate its use by Brazilian physical therapists, the ACL-RSI was recently translated and adapted to Brazilian Portuguese.38 Therefore, physical therapists should add this instrument to the assessment procedures during ACL postoperative rehabilitation.
Almost half of the physical therapists indicated movement patterns as a measure/criterion for RTS (49.7%). Some authors propose the inclusion of the Landing Error Scoring System (LESS), which assesses the movement pattern during jumping, as a measure that may indicate the readiness to RTS after ACLR.13,16 There is still no consensus on its use to decide RTS clearance, as opposed to measures of performance in functional tests. Tests that mechanically stress knee structures to simulate sports activities demands are often recommended as a method of objective evaluation of the functional outcome of ACLR and as a criterion of RTS.13,16,39,40 In the present study, unexpectedly, less than half of physical therapists (42%) reported the use of functional tests for RTS clearance. Possible explanations for this result are the lack of information about the use of functional tests to determine the patient's readiness to RTS after ACLR or the amount of time required to perform these tests.
Among the main measures/criteria recommended in the literature for RTS, the option indicated by the smallest number of physical therapists (16.6%) was the score on self-report functional scales/questionnaires. However, patient-reported outcome instruments, such as the Knee Outcome Survey – Activities of Daily Living Scale (KOS-ADLS) and the International Knee Documentation Committee (IKDC) subjective form, should be used to assist in documenting functional status from the patient's perspective.14,41–44 A consensus of experts indicated the IKDC questionnaire as an essential measure of self-reported knee function to define success after ACLR and ligament injury.18 Additionally, IKDC scores higher than the 15th percentile score of uninjured individuals45 was proposed as a criterion for RTS.13,16,41 Thus, measures related to the patient's appraisal of their functional status should also be included in a more comprehensive assessment of the individual's readiness to RTS.
The present study has some limitations related to the method of data collection. Due to the nature of the survey, a tendency to respond based on what is expected and not what is actually practiced cannot be ruled out. Moreover, the questionnaire was composed of closed-ended questions, and differences in the interpretation of questions may occur. The method of solicitation of information may also not have been optimal, but while not reaching all physical therapists, electronic surveys can reach a high number of respondents, at a low cost. Another limitation refers to the higher concentration of respondents in the southeastern region of the country. However, this is the most populous region in Brazil and also has the largest number of physical therapy education programs and registered physical therapists.46 Additionally, it was not possible to calculate the survey respondent rate. When the study was conducted, the Brazilian Boards of Sports and Orthopaedic Physical Therapy Specialists were composed, respectively, by 159 and 206 partners, thus corresponding to a 53% and 28% participation of its associates in the survey. Some of these associates did not respond to the questionnaire because they did not practice with the ACL postoperative rehabilitation population, and therefore, did not meet the inclusion criteria of the study. Nevertheless, the possibility of selection bias cannot be ruled out since respondents are possibly the professionals with the most interest in the topic of the questionnaire. Conversely, physical therapists who are not concerned with ACL postoperative rehabilitation possibly apply the recommended measures/criteria for RTS even less.
The results of the present study provide new data regarding the current clinical practice of Brazilian physical therapists that usually work with ACL rehabilitation. This information may encourage the use of appropriate measures/criteria for RTS. However, further research should be performed to identify how the application of these measures/criteria may affect the success of postoperative ACL rehabilitation.
ConclusionsLess than 10% of Brazilian physical therapists use all of the primary measures/criteria recommended in the scientific literature to determine readiness to RTS after ACLR. Although most practitioners use measures related to physical factors in this decision-making process (e.g., muscle strength and knee range of motion), only a small number of physical therapists use validated self-report functional and psychological questionnaires. The use of recommended measurements to determine RTS was associated with certification in Sports Physical Therapy, but not years of experience or academic degree.
Conflicts of interestThe authors declare no conflicts of interest.
The authors thank the Physical Therapy Registration Boards (CREFITO of Minas Gerais, Paraná, Santa Catarina, and São Paulo states) and the Brazilian Boards of Sports and Orthopaedic Physical Therapy Specialties (SONAFE and ABRAFITO, respectively), for sending the link of the electronic survey to their members. This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES - Grant number: Code 001), by the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq - Grant number: 306477/2019-0) and by the Fundacao de Amparo a Pesquisa do Estado de Minas Gerais (FAPEMIG - Grant Number: PPM-00364-18).