Femoroacetabular impingement (FAI) syndrome is a hip joint motion-related clinical disorder characterized by abnormal contact between the hip joint structures. Abnormal hip morphology and joint pain may impair the hip joint range of motion (ROM) and muscle function. However, FAI effects on hip joint ROM and muscle strength remain controversial.
ObjectivesThe purpose of this study was to compare hip joint ROM and muscle strength between FAI syndrome patients and healthy controls.
MethodsTwenty FAI syndrome male patients and 20 healthy male controls (CG) matched for age (FAI=28±6 years; CG=27±5 years), body mass (FAI=81±12kg; CG=80±13kg) and height (FAI=177±6cm; CG=178±6cm), participated in the study. Hip joint ROM for flexion, internal rotation and external rotation were assessed through goniometry. Maximal isometric strength for hip flexion, extension, abduction and adduction were evaluated through hand-held dynamometry.
ResultsHip joint ROM was significantly lower in FAI syndrome patients compared with CG for passive flexion (−4%; effect size – ES=0.65), active internal rotation (−42%; ES=1.60), active external rotation (−28%; ES=1.46) and passive external rotation (−23%; ES=1.63). FAI patients’ hip extensors (−34%; ES=1.46), hip adductors (−33%; ES=1.32), and hip flexors (−25%; ES=1.17) were weaker compared to the CG subjects.
ConclusionsFAI syndrome patients presented both hip muscle weakness and reduced joint ROM compared to match CG.
Femoroacetabular Impingement (FAI) syndrome is a hip joint motion-related clinical disorder with a triad of symptoms (i.e., pain related to position or movement), clinical signs, and imaging findings.1 FAI is characterized by the abnormal contact between the acetabular border and the cervicocephalic femur junction. This abnormal contact causes cartilage damage, and has been related to the early onset of hip degenerative disease.2,3 Moreover, it seems plausible that the both altered bone morphology and the hip pain may impair the joint mobility, the muscle strength and the patient's functional capacity.
Two systematic reviews provide conflicting conclusions regarding the effect of FAI on hip range of motion (ROM).4,5 Diamond et al.4 showed that FAI patients present a decreased ROM at the hip joint impingement directions, whereas Freke et al.5 found that hip joint ROM did not differ between symptomatic FAI and healthy subjects. The different methods used to assess the hip ROM (goniometry, inclinometer, 3D kinematic system, simulate 3D tomography, MRI-generated bony models),6–9 and the poor methodological quality of some studies might explain the divergent conclusions on these two systematic reviews.
Freke et al.5 reviewed six studies on FAI patients’ muscle weakness, and concluded that hip muscle strength is overall impaired in FAI patients. However, studies comparing FAI patients with a control subjects have presented no consensus on the most affected muscle groups.10–13 For instance, while Casartelli et al.10 showed that FAI patients had significantly lower isometric voluntary strength for the hip abductors, adductors, flexors and external rotators, Diamond et al.12 showed that only the hip abductors were weaker in FAI patients compared to asymptomatic subjects. These inconsistent results might be related to the different positions used during the strength tests, as well as the different evaluation tools (manual dynamometer or isokinetic dynamometer).
Knowing which movements and muscle groups are the most affected by FAI syndrome is imperative for developing effective physical therapy treatment programs. Considering the abovementioned literature divergences, high methodological quality studies are required. In addition, studies with FAI patients have greater practical applicability when using evaluation procedures that can be reproduced by physical therapists in the clinical setting. Therefore, the purpose of this study was to compare hip joint ROM and muscle strength between FAI syndrome patients and a CG.
MethodsStudy designA cross-sectional, case-control study was performed to identify possible deficits in hip ROM and muscle strength in FAI syndrome patients compared to their matched CG. All volunteers were submitted to a clinical evaluation protocol conducted by two physical therapists, who presented at least 10 years of clinical practice and more than 500 FAI patients that they assessed using the methods applied in this study. Hip joint ROM for flexion, internal rotation and external rotation were assessed through goniometry. Maximal isometric strength of the hip flexors, hip extensors, hip abductors and hip adductors was evaluated through hand-held dynamometry.
The study was conducted according to the revised Helsinki declaration. Ethical approvals for the study were obtained from the Universidade Federal do Rio Grande do Sul (Porto Alegre, RS, Brazil) ethics committee (reference number 1.871.372). All subjects agreed to participate by signing an informed consent form.
SubjectsTwenty FAI syndrome male patients and 20 healthy male controls (CG) were assessed in this study. Male patients were selected due to the larger prevalence of FAI morphology in this population.14 Sample size calculation was determined based on hip adductor muscle weakness detected in FAI patients compared with matched controls.10 Power analysis indicated that a sample size of 20 subjects/group was required to detect significant hip adductors strength differences between FAI and CG (effect size d=0.8; α=0.05; power=0.8).
FAI syndrome patients were obtained from a local Physical Therapy Center. An orthopedic surgeon diagnosed FAI syndrome patients based on a symptoms triad, clinical signs and image findings.1 To be included, patients should present: (1) motion-related or position-related pain symptoms at the hip or groin; (2) positive hip impingement test (FADDIR) and limited ROM; and (3) an anteroposterior radiograph of the pelvis and a lateral neck view with a “pistol grip” (i.e. CAM deformity) and/or Pincer morphology (an over covered acetabular rim). Data collection occurred prior to the surgical treatment, and patients did not received any kind of physical therapeutic intervention before evaluations. The modified Harris Hip Score (mHHS),15 the Hip Outcome Score (HOS),16 and the International Hip Outcomes Tool (iHOT – Brazilian adapted version)17 were used to assess the patients’ functionality. These questionnaires were applied only to FAI patients, and were chosen because they evaluate different syndrome domains. While mHHS emphasizes the presence of pain, HOS emphasizes functionality in daily activities. The iHOT takes into account biopsychosocial aspects. In all three questionnaires, results close to 100 indicate an excellent result, where the hip problem does not affect the assessed domain. Patients with other lower limb injuries (e.g. ACL rupture, muscle strain, meniscal tear, tendinopathy) were excluded from the study, as well as patients with rheumatologic or neurological diseases.
CG subjects were recruited from the university community. To rule out the presence of intra-articular pathology (osteoarthritis – OA, labral lesions and FAI), all subjects were subjected to the flexion-adduction-internal rotation (FADDIR) test.18 This test, performed by the physical therapist, was chosen due to its potential for the determination of intraarticular pathology nonexistence (its screening ability with a sensitivity of 99 and a negative likelihood ratio of 0.15).19
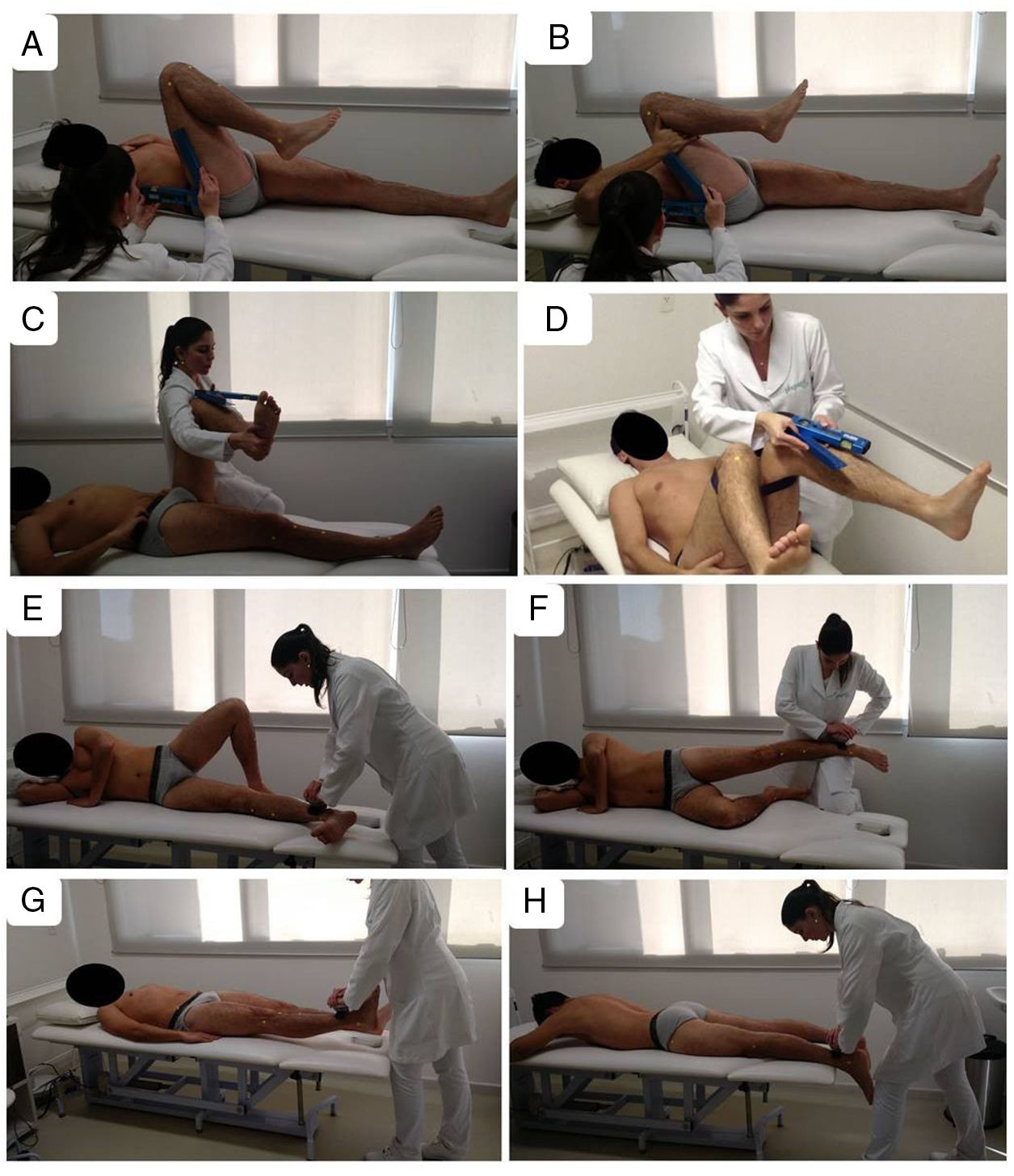
Range of motion (ROM) evaluationHip joint ROM was assessed using a goniometer for flexion (active and passive), internal rotation (only active) and external rotation (active and passive). Goniometry was chosen to assess hip ROM because it is a widely used and clinician-friendly tool, and is a reliable and valid method to assess FAI patients’ ROM.8 According to Nussbaumer et al.,8 who used goniometry and clearly described the positioning during the ROM tests, goniometer-based assessments considerably overestimate hip ROM due to uncontrolled pelvic rotation and pelvic tilt. We tried to solve some of these problems by using a bilateral movement, so that the patient could not compensate with a pelvic tilt or pelvic rotation during internal rotation ROM measurements. Therefore, the subjects’ positions were chosen to favor pelvis stabilization (Fig. 1). For hip flexion, the contralateral leg was maintained fully extended to reduce the posterior pelvic tilt. For external rotation, the contralateral leg was maintained fully extended in neutral position to control the pelvic inclination. For internal rotation, the movement was performed bilaterally to neutralize the pelvic inclination, and the subject maintained the hip and knee flexed in 90° throughout the test. We did not measure passive internal rotation ROM because it is not possible for the physical therapist to force passive bilateral ROM at the same time that he/she is measuring hip ROM with a goniometer. We chose not to use help from another evaluator during the tests because we wanted the tests to be easily reproducible in the clinical setting.
Subjects’ positions during hip range of motion assessments (A–D) and isometric muscle strength measurements (E–H). Active flexion (A), passive flexion (B), passive external rotation (C) and active internal rotation (D) were measured with a goniometer. Hip adductors (E), hip abductors (F), hip flexors (G) and hip extensors (H) strength measurements with a hand held dynamometer.
Nussbaumer et al.8 have already demonstrated that passive hip joint goniometry was reliable between days (intra-rater reliability). Healthy subjects hip ROM inter-rater reliability was previously established in our laboratory using the same methodology here presented and was considered excellent for hip rotations and satisfactory for hip flexion.20 The inter-rater intraclass correlation coefficient (ICC) values were superior to 0.84 for hip flexion and hip rotations.20
Hip extension, hip abduction and hip adduction ROM tests were not included due to difficulties in obtaining a good testing position with the pelvis stabilized, which increases measurement errors and/or data dispersion. In addition, hip flexion and hip rotations appeared to be good representatives of hip mobility related to the morphological abnormalities that cause FAI.
Muscle strength evaluationMaximal isometric hip strength was assessed through hand-held dynamometry (MICROFET – Hoogan Scientific, Salt Lake City, USA). Hip flexors, extensors, abductors and adductors were evaluated in different positions (Fig. 1). In all tests, the dynamometer was placed distally (close to the ankle joint), with a great lever arm to favor the evaluators’ stabilization. The evaluator holds the dynamometer pad 5cm proximal to the lateral (hip abduction) and medial (hip adduction) malleoli. For the hip flexors and extensors, a horizontal line was drawn from the lateral malleolus to the anterior (hip flexors) or posterior (hip extensors) part of the leg and the dynamometer was placed proximal to this line.
For each muscle group, subjects completed two maximal voluntary isometric contraction (MVICs) trials. If the difference between the two MVICs was higher than 10%, another trial was performed. Subjects were asked to perform maximal efforts with the following sequence: 2s to build up to maximal force, 2s of isometric contraction, and 2s to relax. The between-trials rest interval was set at 120s. Additional measurements were taken if poor stabilization occurred or if participants failed to achieve a maximum effort. Participants received standardized verbal encouragement to produce maximal effort by the physical therapist, who used the following expression: “Come on, full effort, full effort!” The highest effort of the two valid measures was converted to torque value (Nm) by multiplying the force in Newtons by the lever arm length (distance between approximate joint axis of rotation and the point of force application). Normalized to body mass (Nm/kg) data were analyzed.
Thorborg et al.21 and Pua et al.22 have shown good to excellent reliability for intra-rater hip strength measurements, but did not evaluate the inter-rater reliability. However, their methodology used to determine this intra-rater reliability differs from the one used in the present study. Healthy subjects hip muscle strength intra-rater and inter-rater reliability was previously established in our group using the same methodology here presented. Our results agreed with those of the abovementioned studies for the intra-rater reliability, and added new information for the inter-rater reliability. ICC was considered excellent (intra-rater superior to 0.89, inter-rater superior to 0.90) for all tested muscle groups.20
Statistical analysisThe symptomatic (for unilateral FAI patients) or the most symptomatic (for bilateral FAI patients) hip was used for analysis. Since CG subjects presented no differences for the between-legs comparison, data from the right leg were used for analysis. Data normal distribution was assessed using the Shapiro–Wilk test. Independent t-tests were used to compare FAI and CG for age, body mass, height, ROM, and strength. Cohen's “d” effect size was used to determine differences on the hip ROM and strength values between the two groups. Effect size results were interpreted based in the following classification: trivial (<0.2), small (>0.2), moderate (>0.6), large (>1.2), very large (>2.0).23,24
ResultsAll twenty subjects from each group completed the evaluation session. The two groups were matched for age (FAI=28.1±6.0 year, CG=27.0±5.0 years, p=0.232), body mass (FAI=81.5±12.1kg, CG=80.0±13.1kg, p=0.367) and height (FAI=1.77±0.06m, CG=1.78±0.06m, p=0.416). All FAI patients’ questionnaires presented reduced values compared to the full score. The mean±SD values for the questionnaires were 45.5±14.3 for iHOT, 73.8±13.8 for MMHS, and 80.6±19.4 for HOS.
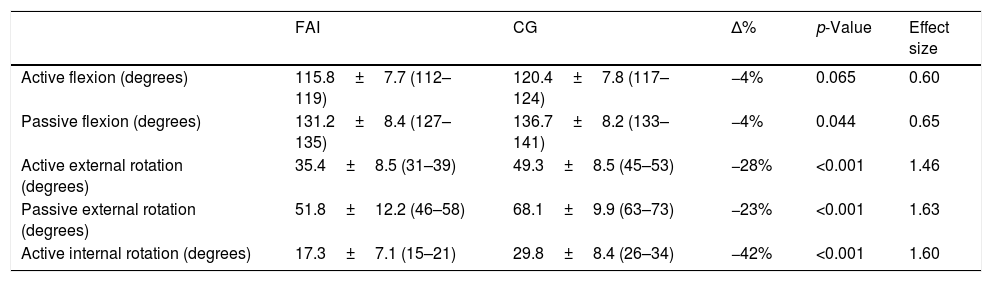
FAI patients presented significantly smaller hip ROM for passive flexion, passive and active external rotation, and active internal rotation compared to CG (Table 1). Active flexion was similar between the two groups. The effect size was considered large for hip internal and external rotation and moderate for hip flexion (Table 1).
Range of motion of femoroacetabular impingement (FAI) patients and control group (CG) subjects [mean±SD (95% CI)].
| FAI | CG | Δ% | p-Value | Effect size | |
|---|---|---|---|---|---|
| Active flexion (degrees) | 115.8±7.7 (112–119) | 120.4±7.8 (117–124) | −4% | 0.065 | 0.60 |
| Passive flexion (degrees) | 131.2±8.4 (127–135) | 136.7±8.2 (133–141) | −4% | 0.044 | 0.65 |
| Active external rotation (degrees) | 35.4±8.5 (31–39) | 49.3±8.5 (45–53) | −28% | <0.001 | 1.46 |
| Passive external rotation (degrees) | 51.8±12.2 (46–58) | 68.1±9.9 (63–73) | −23% | <0.001 | 1.63 |
| Active internal rotation (degrees) | 17.3±7.1 (15–21) | 29.8±8.4 (26–34) | −42% | <0.001 | 1.60 |
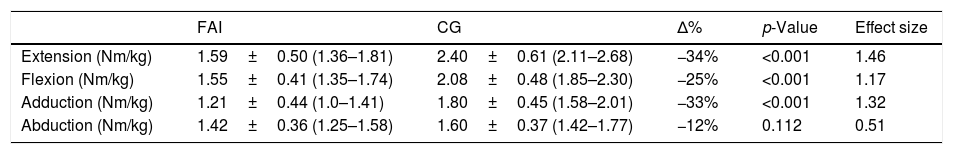
FAI patients were weaker (smaller relative strength) compared to CG subjects for hip flexors, hip extensors, and hip adductors (Table 2). Hip abductors relative strength was similar between FAI patients and CG. The effect size was considered large for hip extensors and hip adductors, moderated for the hip flexors and small for the hip abductors (Table 2).
Hip strength relative to body mass (Nm/kg) of femoroacetabular impingement (FAI) patients and control group (CG) subjects [mean±SD (95% CI)].
| FAI | CG | Δ% | p-Value | Effect size | |
|---|---|---|---|---|---|
| Extension (Nm/kg) | 1.59±0.50 (1.36–1.81) | 2.40±0.61 (2.11–2.68) | −34% | <0.001 | 1.46 |
| Flexion (Nm/kg) | 1.55±0.41 (1.35–1.74) | 2.08±0.48 (1.85–2.30) | −25% | <0.001 | 1.17 |
| Adduction (Nm/kg) | 1.21±0.44 (1.0–1.41) | 1.80±0.45 (1.58–2.01) | −33% | <0.001 | 1.32 |
| Abduction (Nm/kg) | 1.42±0.36 (1.25–1.58) | 1.60±0.37 (1.42–1.77) | −12% | 0.112 | 0.51 |
Our results on hip ROM disagree from those reported by Freke et al.,5 who suggested that no differences in hip ROM existed between FAI patients and CG asymptomatic subjects. Our results for internal rotation (∼17° for FAI and ∼30° for CG) were a little smaller than Nussbaumer et al.8 results (∼26° for FAI and ∼34° for CG). For hip flexion, while using the same position as Nussbaumer et al.,8 we tried to neutralize the lumbopelvic movement by placing a lumbar cushion at the lumbar region. Although this lumbar cushion limited pelvic tilt, our results (∼116° for FAI and ∼120° for CG) for hip flexion were superior than those described in some studies.8,25 The reason for this difference is not completely clear. However, these studies present hip flexion ROM values inferior to those described by normative ROM studies.26 For external rotation, our values (∼35° for FAI and ∼49° for CG) are like those from Nussbaumer et al.8 (∼36° for FAI and ∼45° for CG).
The losses in hip ROM confirmed the initial hypothesis presented by Ganz et al.3,27 that FAI syndrome patients had reduced hip flexion and internal rotation. Hip internal rotation reduction, frequently cited in different FAI studies,6,7,9 seems to be highly related to the morphological abnormality at the femoral-neck junction, which blocks the internal rotation especially when the hip is flexed by 90°.27 The hip external rotation reduction, however, cannot be explained by the presence of CAM morphological abnormality. It appears that this hip ROM limitation is more related to a movement restriction caused by skeletal soft tissues (e.g. joint capsule, ligaments and muscle fiber length).28–30 Joint effusion should be considered an intervenient factor on FAI patients hip ROM,31 as well as kinesiophobia (i.e. fear of movement). Therefore, the reduced hip ROM observed in FAI patients might be related to several factors, and physical therapists should investigate the main movement restriction factors in each patient (e.g., soft tissues adaptation to disuse, effusion, pain, or kinesiophobia) to offer an individualized and assertive treatment.
Our results for the hip strength measurements agree with those reported by Freke et al.5 FAI patients were weaker than the CG, and our effect size results showed that strength losses in FAI patients’ hip muscle groups are clinically relevant, and not only statistically significant as traditionally reported by clinical trials through the “p-values”. Interestingly, we were unable to show a consistent loss on the hip abductors strength in FAI patients (no between-groups statistical difference with a small effect size). Casartelli et al.10 showed that patients with symptomatic FAI presented muscle weakness for all hip muscle groups (except for internal rotators and extensors) using hand-held and isokinetic dynamometers, while Diamond et al.12 showed that only hip abduction strength was lower in FAI patients compared to controls when testing with a hand-held dynamometer. Apparently, the testing method and the subject's positioning are strong intervening factors for detecting FAI patients muscle weakness. FAI patients’ pain or discomfort at some positions, their restricted ROM and kinesiophobia may negatively affect muscle strength evaluation.
Muscle strength reduction has been demonstrated in patients with hip and knee disorders,32,33 and associated with muscle weakness and generalized reduced muscle mass in the affected lower limb of patients with unilateral hip OA.32 Muscle weakness mechanisms are multifactorial, and include reduced muscle mass, presence of muscle inhibition and decreased muscle quality, which are common to disuse situations.30 It is interesting to note that many of the FAI patients end up leaving their sports/exercise practice at a life stage when they are physically active or even athletes. Considering that FAI patients remain for many years with pain (e.g., FAI syndrome patients in our study had a mean pain symptom of ∼50 months), pain-induced neuromuscular inhibition34 might partly explain the strength losses. In addition, FAI abnormal morphologies have been related with the early onset of hip OA,2,27 which is known to cause muscle inhibition. However, to date there appears to be no study assessing muscle inhibition in FAI patients.
FAI syndrome patients experience disability and functional limitations while performing daily living movements that have high hip ROM demands (e.g., putting pants or tying shoelaces),35 which can worsen during demanding physical activities.36,37 Since hip ROM and muscle strength losses have an important role in functional limitations and disability, improvements in these outcomes have been recommended in physical therapy programs.38–40 There is a consensus that muscle strengthening plays a key role in these patients’ recovery in both conservative and surgical treatments, but ROM recovery is a controversial point.38–40 As part of the hip ROM limitation is related to the bone structure and to the joint lesions (labrum and cartilage), one could argue that full ROM recovery might not be achievable with conservative treatment. However, apparently surgical intervention also does not guarantee hip ROM increase.5 Therefore, further high-quality methodology studies are needed to clarify the best procedures for the recovery of the FAI patients’ hip ROM.
A crucial limitation of this study was that evaluators were not blinded to the subjects’ group allocation. In addition, the CG subjects’ evaluation used to exclude hip pathology was performed based on clinical exams. A health-lifestyle questionnaire could have been used for the CG to better describe their health status; and the hip morphology imaging analysis would have helped to eliminate any chance of morphological abnormality in the control subjects. The ROM measurements were made only for hip flexion and rotational movements due to the difficulty in obtaining a good pelvis stable position for testing the hip abduction and adduction ROM. The poor stability during tests also prevented the strength tests for hip internal and external rotators through the hand-held dynamometer. Despite our limitations to test ROM and strength for all hip movements and muscle groups, we used a reliable testing procedure easily executable in the clinical setting.
ConclusionFAI syndrome patients presented hip muscle weakness and reduced ROM compared to controls. These deficiencies may be detected in the clinical setting using simple and reliable tests with a goniometer and a hand-held dynamometer. Strength deficits in hip adduction, hip flexion and hip extension can be resolved during rehabilitation programs. However, deficits in hip internal and external rotation ROM might be emphasized after FAI surgical correction.
Conflicts of interestThe authors declare no conflicts of interest.
VBF receive scholarship from CAPES-Brazil, and MAV is a researcher 1D from CNPq-Brazil.