(1) To identify the type and frequency of interventions used by Brazilian physical therapists to treat and prevent the occurrence of patellar tendinopathy in athletes and the criteria used to return to sport; (2) to compare the interventions used to the grade of recommendation of current evidence.
MethodsDesign: cross-sectional study. Setting: online survey throughout sports physical therapy association. Participants: Physical therapists who were invited to complete a structured questionnaire. Main Outcome Measures: Interventions more frequently used for treating and preventing PT in athletes and the criteria used to define return to sport.
ResultsOne-hundred and twenty-one physical therapists participated in this study. Quadriceps eccentric strengthening (75.2%), education (61.2%) and lower limb joint/lumbo-pelvic stabilization/hamstrings stretching (59.5%) were more frequently cited for prevention purposes, while lower limb joint stabilization (81.8%), education (80.2%) and myofascial release (78.5%) were more frequently reported for treatment. The majority of the physical therapists based their decision of athlete discharge on a combination of pain intensity, function and functional test results (44.6%).
ConclusionThere was inconsistency between interventions used in clinical practice and interventions recommended by the best available evidence.
Patellar tendinopathy (PT) is a chronic condition that causes prolonged disability for athletes and that may be challenging to treat and prevent.1 Athletes with PT usually complain about pain and tenderness to palpation in the patellar tendon during sports-related activities, such as sprinting and jumping.1,2 The prevalence of PT in elite volleyball and basketball athletes is approximately 40%,2 in athletics is 22%2 and in soccer is 13%.2
The management of PT frequently involves a wide range of interventions, such as knee extensors eccentric strengthening, heavy-slow resistance training, extracorporeal shock wave therapy (ESWT) and low-intensity pulsed ultrasound.3,4 However, interventions commonly implemented in athletes with PT might not be supported by scientific evidence.5–7 For example, Gaida and Cook3 found that ESWT and low-intensity pulsed ultrasound have only short-term effects and consequently may not be a good option for long-term treatment of PT. On the other hand, scientific evidence supports the use of quadriceps eccentric-concentric loading for long-term treatment of PT.8 In addition to local interventions, physical therapists should also identify and treat possible non-local causes of PT based on clinical reasoning and on scientific evidence, such as hip muscles weakness and ankle dorsiflexion ROM.1,7,9,10 Finally, proper criteria to return to sport should be considered at the end of rehabilitation to promote a safe sport practice.1,7,11,12
Most of the clinical trials regarding the effects of different interventions on athletes with PT lack proper follow-up data.13 Moreover, a systematic review14 showed that physical therapists reported lack of time and inability to interpreted statistical results and a surveillance in Brazil15 demonstrated that 80% of the PTs have difficulty in obtaining full-text paper. Based on this data, it would be not surprising that the physical therapist may not use high quality clinical research routinely to treat and prevent PT. The purpose of this study were (1) to identify the type and frequency of interventions used by Brazilian physical therapists to treat and prevent the occurrence of PT in athletes and the criteria used to return to sport and (2) to compare the interventions used to the grade of recommendation of current evidence. Our hypothesis is that physical therapists do not discharge athletes from treatment and do not implement their interventions for rehabilitation and prevention according to the best scientific evidence.
MethodsThis cross-sectional study was reported in accordance with “the strengthening the reporting of observational studies in epidemiology (STROBE) statement”.16 This study was approved by the Ethics Committee of the Universidade Federal dos Vales do Jequitinhonha e Mucuri (Diamantina, Minas Gerais, Brazil) (55498416.1.0000.5108).
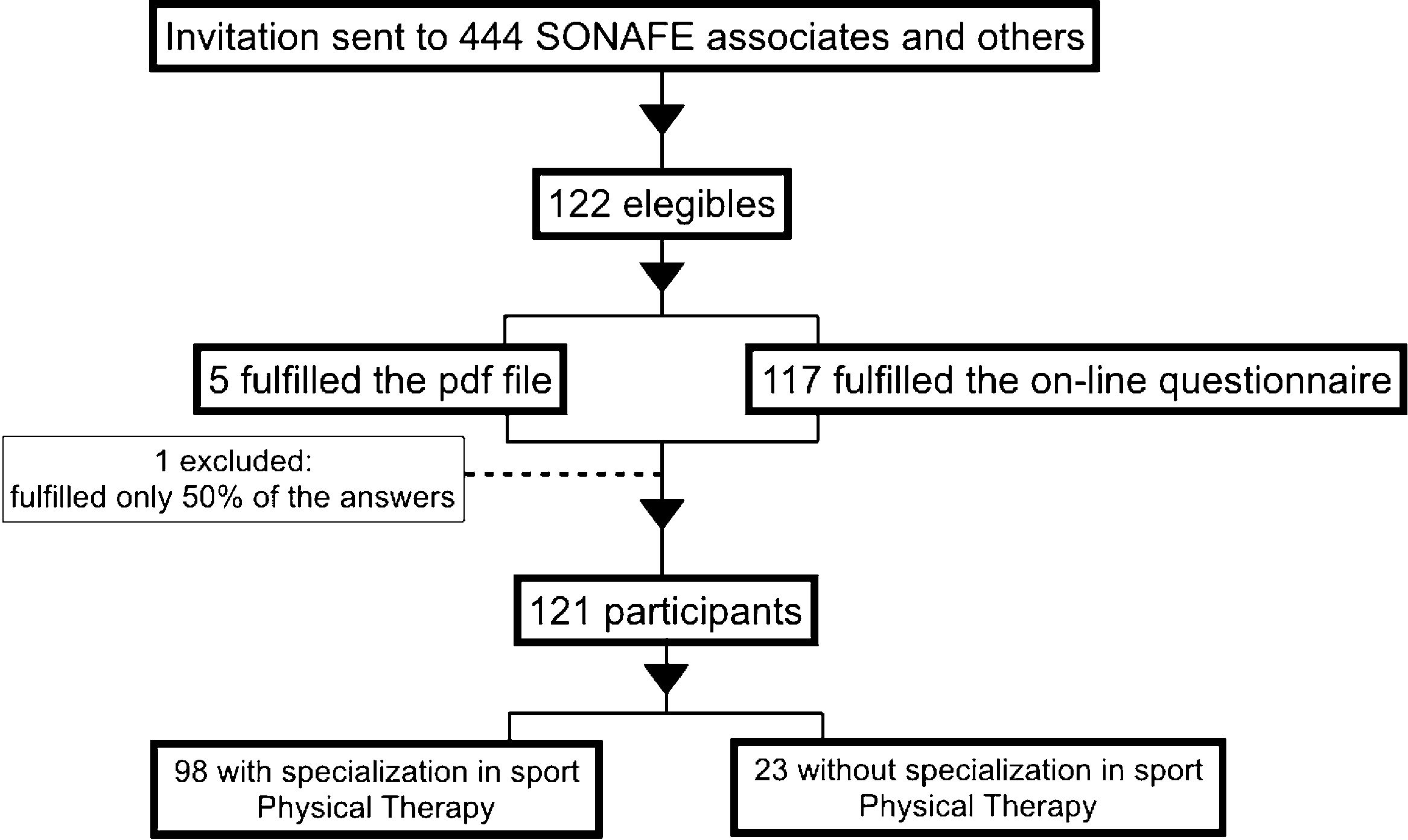
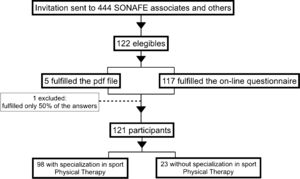
ParticipantsPhysical therapists were invited to participate in this study through the Brazilian National Society of Sport Physical Therapy (SONAFE-Brazil) database (electronic address and social media). SONAFE-Brazil had 444 associates. These associates were invited to participate in this study, as well as other professionals without membership, throughout SONAFE's social media. They were invited through cover letter sent by email by SONAFE's secretary, which had: (i) a short explanation of the study purposes, clinical relevance and inclusion criteria, ii) the consent form and iii) the structured questionnaire (assessed by clicking on a link or opening a PDF file). When a participant answered the entire questionnaire using the link, an automatic electronic message was sent to the examiner (L.D.M.), who was responsible for organizing the data sheet and analyzing it. On the other hand, the participants that fulfilled the PDF file sent that file back to the same examiner (L.D.M.). After sending the cover letters, we waited for three months to get the responses back from the potential participants. In addition, for those potential participants who did not answer back after one month, reminders were resent twice during the following two months. The inclusion criteria were as follows: (i) be a registered physical therapist at the Brazilian federal council of Physical Therapy and Occupational Therapy and (ii) have previous experience with rehabilitation of athletes (professional or amateurs) with PT (a minimum time of experience was not established). All participants read and signed the consent form and had their confidentiality protected.
Data collectionThe questionnaire had ten questions: (i) four questions related to clinical practice and the characteristics of the treated athletes, (ii) two multiple choice questions about interventions more frequently used for athletes with PT, (iii) two questions about the frequency of the implemented interventions and the duration of the treatment, (iv) one multiple choice question about the time loss from practice and (v) one question about the criteria used to define return to sport. The majority of the questions were answered by checking boxes.
The answer options regarding the questions about interventions most frequently used were: eccentric protocol,17–19 eccentric/isometric/concentric strengthening,20–23 stretching,10,20,24 joint mobilization,20,25 foot orthotics,20,26 electrotherapy,27–30 lumbo-pelvic stabilization,1,3,9 miofascial release,31 functional training,1,7,13 lower limb stabilization,1,7,13,32 taping,33,34 transverse friction,3,9,35 plyometric,1,3,9 load control,1,3,8,9 education,1,3,9 cryotherapy1,3,9,36 and others. The physical therapist could select multiple interventions. The definition of the intervention options to include in the questionnaire was based in the literature,1,7,8,21,37 common sense, and in the clinical experience of the authors.
The answer options regarding the question about the criteria used to return to sport were: pain,1,3,4,9 function,1,3,9 the Victorian Institute of Sport Assessment – Patella (VISA-P) score,1,3,9,11 performance in a functional test and others. Finally, we asked about the athletes’ amount of time loss from sport due to PT.
Data analysisDescriptive analysis was performed to define the characteristics of the participants, the absolute and relative frequency of responses related to used interventions, time to return to play and discharge from treatment criteria. The different interventions were clustered in the following groups of interventions: Electrothermal Phototherapy, Strengthening exercises, Stretching exercises and Others.
Considering that there is no guideline38 for PT treatment, the authors searched for the best available evidence for each group of interventions. This simple search was performed in PUBMED using the term “patellar tendinopathy” combined by the Boolean operator “AND” with the name of the group of intervention (e.g. patellar tendinopathy AND strengthening exercises) to identify systematic reviews and/or meta-analysis that assessed the efficacy of the interventions cited by the participants of this study. We have also indicated the grade of recommendation, when available, for each group of interventions. Therefore, grade A indicates strong evidence, B indicates moderate evidence, C, weak evidence, D, conflicting evidence, E, theoretical/foundational evidence and F, expert opinion. Grades E or F were provided for the groups of interventions that we did find scientific evidence from systematic reviews and meta-analysis.
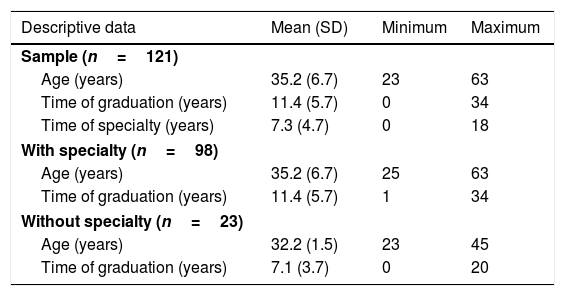
ResultsSample characteristicsOne hundred and twenty-one Brazilian physical therapists participated in this study (95 males and 26 females). Questionnaires with one-third or more of the questions unanswered were excluded from analysis (n=1). Fig. 1 shows the flow diagram of the study and Table 1 indicates descriptive data and clinical practice characteristics of the participants.
Descriptive data and clinical practice characteristics of the participants.
| Descriptive data | Mean (SD) | Minimum | Maximum |
|---|---|---|---|
| Sample (n=121) | |||
| Age (years) | 35.2 (6.7) | 23 | 63 |
| Time of graduation (years) | 11.4 (5.7) | 0 | 34 |
| Time of specialty (years) | 7.3 (4.7) | 0 | 18 |
| With specialty (n=98) | |||
| Age (years) | 35.2 (6.7) | 25 | 63 |
| Time of graduation (years) | 11.4 (5.7) | 1 | 34 |
| Without specialty (n=23) | |||
| Age (years) | 32.2 (1.5) | 23 | 45 |
| Time of graduation (years) | 7.1 (3.7) | 0 | 20 |
| Clinical practice characteristics | Frequency (n(%)) |
|---|---|
| Sample (n=121) | |
| Sports modality attended | |
| Soccer | 40 (19.3%) |
| Running | 27 (13.0%) |
| Volleyball | 24 (11.6%) |
| Martial Arts | 19 (9.1%) |
| Swimming | 17 (8.2%) |
| Tennis | 15 (7.2%) |
| Basketball | 13 (6.2%) |
| Athletics | 10 (4.8%) |
| Others | 42 (20.3%) |
| Clinical practice experience | |
| Private practice | 65 (38.0%) |
| Sports event | 41 (23.9%) |
| Sports team | 27 (15.8%) |
| All | 26 (15.2%) |
| Others | 12 (7.0%) |
SD, standard deviation.
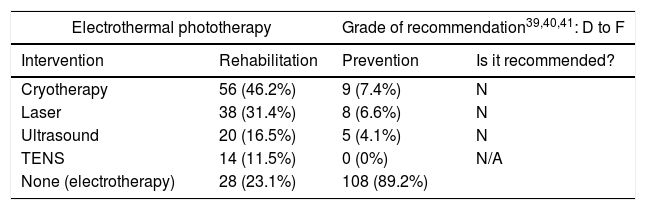
Table 2 shows the frequency of interventions used by the participants for rehabilitation and prevention purposes. Information about grade of recommendation was extracted on October 21st through consecutives simple search of systematic reviews and meta-analysis.
Frequency (n (%)) of interventions targeting rehabilitation and prevention and grade of recommendation.
| Electrothermal phototherapy | Grade of recommendation39,40,41: D to F | ||
|---|---|---|---|
| Intervention | Rehabilitation | Prevention | Is it recommended? |
| Cryotherapy | 56 (46.2%) | 9 (7.4%) | N |
| Laser | 38 (31.4%) | 8 (6.6%) | N |
| Ultrasound | 20 (16.5%) | 5 (4.1%) | N |
| TENS | 14 (11.5%) | 0 (0%) | N/A |
| None (electrotherapy) | 28 (23.1%) | 108 (89.2%) | |
| Stretching exercises | Grade of recommendation40,41: C to F | ||
|---|---|---|---|
| Intervention | Rehabilitation | Prevention | Is it recommended? |
| Quadriceps | 91 (75.2%) | 59 (48.7%) | Y |
| Hamstrings | 75 (61.9%) | 72 (59.5%) | Y |
| Iliotibial band | 70 (57.8%) | 55 (45.4%) | N/A |
| Plantar flexors | 51 (42.1%) | 51 (42.1%) | N/A |
| None (stretching) | 18 (14.8%) | 39 (32.2%) | |
| Strengthening exercises | Grade of recommendation40,41,42: A to F | ||
|---|---|---|---|
| Intervention | Rehabilitation | Prevention | Is it recommended? |
| Quadriceps concentric | 38 (31.4%) | 43 (35.5%) | Y |
| Hamstrings concentric | 56 (46.2%) | 44 (36.3%) | N/A |
| Abdominal concentric | 15 (12.4%) | 18 (14.8%) | N/A |
| Plantar flexors concentric | 47 (38.8%) | 25 (20.6%) | N/A |
| Hip abductors concentric | 63 (52.0%) | 63 (52.0%) | N/A |
| Hip ER concentric | 66 (54.5%) | 52 (42.9%) | N/A |
| Hip extensors concentric | 62 (51.2%) | 55 (45.4%) | Y |
| None (concentric) | 20 (16.5%) | 29 (23.9%) | |
| Quadriceps isometric | 61 (50.4%) | 22 (18.1%) | Y |
| Hamstrings isometric | 17 (14.0%) | 7 (5.7%) | N/A |
| Abdominal isometric | 27 (22.3%) | 17 (14.0%) | N/A |
| Plantar flexors isometric | 8 (6.6%) | 5 (4.1%) | N/A |
| Hip abductors isometric | 25 (20.6%) | 24 (19.8%) | N/A |
| Hip ER isometric | 26 (21.4%) | 17 (14.0%) | N/A |
| Hip extensors isometric | 25 (20.6%) | 18 (14.8%) | N/A |
| None (isometric) | 39 (32.2%) | 63 (52.0%) | |
| Quadriceps eccentric | 88 (72.7%) | 91 (75.2%) | Y |
| Hamstrings eccentric | 35 (28.9%) | 43 (35.5%) | N/A |
| Abdominal eccentric | 11 (9.1%) | 11 (9.1%) | N/A |
| Plantar flexors eccentric | 27 (22.3%) | 29 (23.9%) | N/A |
| Hip abductors eccentric | 40 (33.0%) | 47 (38.8%) | N/A |
| Hip ER eccentric | 37 (30.5%) | 41 (33.8%) | N/A |
| Hip extensors eccentric | 36 (29.7%) | 45 (37.2%) | Y |
| None (eccentric) | 6 (4.9%) | 17 (14.0%) | |
| Plyometric | 53 (43.8%) | 42 (40.5%) | Y |
| Single-Leg decline squat | 59 (48.7%) | 42 (34.7%) | Y |
| Others | Grade of recommendation39,40,41: D to F | ||
|---|---|---|---|
| Intervention | Rehabilitation | Prevention | Is it recommended? |
| Taping | 75 (61.9%) | 12 (9.9%) | N |
| Foot orthotics | 35 (28.9%) | 21 (17.3%) | N |
| Education | 97 (80.1%) | 74 (61.1%) | Y |
| Load control | 66 (54.5%) | 33 (27.2%) | Y |
| Transverse friction | 54 (44.6%) | 1 (0.8%) | N |
| Myofascial Release | 95 (78.5%) | 45 (37.2%) | N |
| Lower limb joint stabilization/proprioception/balance | 99 (81.8%) | 72 (59.5%) | Y |
| Functional training | 64 (52.9%) | 59 (48.7%) | Y |
| Lumbo-pelvic stabilization | 76 (62.8%) | 72 (59.5%) | Y |
| Ankle dorsiflexion mobilization | 68 (56.2%) | 48 (39.6%) | N/A |
Y, yes; N, no; N/A, not investigated. Grade of recommendation (based on the references indicated) was A in case of strong evidence, B if moderate evidence, C if weak evidence, D if conflicting evidence, E if theoretical/foundational evidence and F in case of expert opinion. The interventions recommended for athletes with PT based on systematic reviews and meta-analysis are marked as “yes” and for those interventions not recommended or not investigated in the cited references, we indicated as “no” and “N/A”, respectively.
Most of the participants reported that the frequency of rehabilitation sessions was one to three times per week (48.8%), followed by four to six times per week (37.20%). In addition, the duration of the rehabilitation treatment was five to eight weeks (43.8%), followed by two to four weeks (24%) and nine to twelve weeks (19%). The mean time loss from training was more than fifteen days for 50.4% and only 6.6% allow athletes to keep training during the treatment period. The frequency of prevention sessions was mainly one to three times per week (66.1%), followed by no specific frequency (23.1%).
Only twenty physical therapists (16.5%) indicated the use of the single-leg decline squat as an eccentric protocol and only fifteen (12.4%) indicated the heavy-slow resistance training. Twenty-four (19.8%) participants used the muscle strengthening in specific lengths (e.g. elongated or shortened).
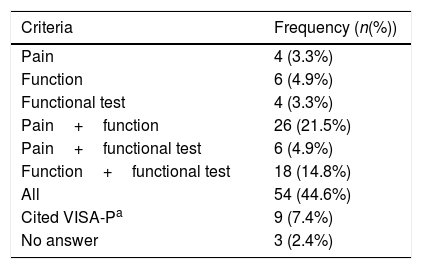
Return to play criteriaThe participants reported that the most cited criteria to define return to sport was the combination of pain intensity, function and performance in a functional test (Table 3). The top three functional tests indicated by the participants were hop test (n=28; 23.2%), single-leg decline squat/single-leg squat (n=13; 10.8%) and step-down test (n=8; 6.6%).
Return to sport criteria (n=121).
| Criteria | Frequency (n(%)) |
|---|---|
| Pain | 4 (3.3%) |
| Function | 6 (4.9%) |
| Functional test | 4 (3.3%) |
| Pain+function | 26 (21.5%) |
| Pain+functional test | 6 (4.9%) |
| Function+functional test | 18 (14.8%) |
| All | 54 (44.6%) |
| Cited VISA-Pa | 9 (7.4%) |
| No answer | 3 (2.4%) |
This study showed the profile of Brazilian physical therapists that work with athletes with PT, capturing interventions related to rehabilitation, prevention and criteria to decide about return to play. The Brazilian physical therapists that participated in this study were mainly sport specialists working in private practices with more than ten years of clinical experience. Education, myofascial release and stabilization were used for PT rehabilitation and strengthening, education, stabilization and stretching were used for PT prevention. It was possible to indicate that the physical therapist's choices weren’t in accordance to current evidence.
RehabilitationThe participants based their rehabilitation program on education, myofascial release, lower limb joint stabilization/proprioception/balance, and quadriceps stretching and eccentric exercises. Education improves athlete's adherence during rehabilitation and eighty percent of the physical therapists reported using this intervention.9,43,44 Myofascial release is a manual technique with recent studies demonstrating that it increases range of motion and reduces delayed onset of muscle soreness of recreational to highly active individuals.31 Although there is no evidence of the benefits for athletes with PT, future studies are necessary to validate (or refute) the benefits of this intervention for this population. Interestingly, lower limb stabilization was selected by 81.8% of the physical therapists, even though previous studies have not demonstrated the benefits of this intervention to tendinopathy.32 A systematic review published in 201120 indicated that quadriceps flexibility is a risk factor for PT, which could explain why most of the participants mentioned the use of quadriceps stretching. Seventy-two percent of the physical therapists chose quadriceps eccentric strengthening exercise, which agrees with scientific evidence.21 For example, Kongsgaard et al.21 demonstrated that eccentric training decreased tendon pain and improved collagen remodeling short and after a 12 months follow-up. Moreover, Yu et al.27 found that almost half of the randomized controlled trials that investigated the effectiveness of physical agents for the management of lower-limb soft tissue injuries, such as PT, had a high risk of bias. Moreover, the authors didn’t find randomized clinical trials investigating the effects of laser therapy in patients with PT.27
PreventionThe participants of the present study reported that they frequently use quadriceps eccentric strengthening, education, lower limb joint/lumbo-pelvic stabilization and hamstrings stretching. Quadriceps eccentrics strengthening was indicated as a usual preventive intervention by the participants of the present study.8,17,18 Eccentric is a proper intervention to enhance tissue energy absorption.45 The adherence of preventive programs is directly related to their effectiveness and education influences this process.9,43,44 Lower limb joint stabilization and lumbo-pelvic stabilization exercises are usually included in general preventive programs in sports, since it aims to improve functional capability of the athlete.46–48 However, this type of general preventive program has no evidence specifically related to PT.49 Hamstring stretching is adopted based on a systematic review published in 2011 about risk factors for PT.20
Return to sportReturn to sport for athletes with PT can be slow and is often dependent on severity of the tendon pain, dysfunction and the quality of the rehabilitation. Our results indicated that the physical therapists chosen a combination of pain, function and functional tests to decide about return to sport. The presence of pain and dysfunction could be assessed through VISA-P, since it is largely used to assess PT severity in athletes and its responsiveness in athletes has been reported.12,19,27,50 Despite this, approximately 10% of the participants cited VISA-P as a criterion to define return to sport. The main functional tests used by the participants (hop test, single-leg decline squat/single-leg squat and step-down test) are standardized and indicated to PT management.1,44
Our study was capable to capture the viewpoints of different competences to know how physical therapists act when dealing with athletes in rehabilitation, prevention and return to play. This information could help physical therapists to identify their state of evidence-based practice when dealing with patients with PT. Moreover, we could recommend strategies to enhance the implementation of scientific evidence on physical therapists’ clinical practice, such as organize study groups to discuss new evidence and scientific events to share experiences and knowledge with each other. Future studies could investigate the relationship between the interventions used to treat or prevent PT and the barriers to access scientific literature.
This study had some limitations. Although all of the participants had experience with PT, it is not clear that their main expertise was athletes with PT. We instructed the physical therapists to consider their clinical experience with professional and amateur athletes. Therefore, the athletes’ training level and dedication may have influenced the results. Moreover, the questionnaire was self-administered and filled by Brazilians physical therapists. Thus, we were not able to solve possible doubts of the participants to answer the questionnaire and our results may not be applied to physical therapists from other countries.
ConclusionThe most frequently interventions used by Brazilians physical therapists to treat PT were education, myofascial release and lower limb joint stabilization. Considering prevention of PT, the most used interventions were quadriceps strengthening, education, lower limb joint and lumbo-pelvic stabilization and hamstring stretching. In relation to return to sport, combined criteria (pain, function and functional tests) were used. Finally, there was inconsistency between interventions used in clinical practice and interventions recommended by the literature.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interestThe authors declare no conflicts of interest.
The authors would like to thank the Brazilian National Society of Sport Physical Therapy (SONAFE-Brazil) for their support and all physical therapists that participated in this study.