The literature is unclear on the need for hip strengthening in persons with low back pain (LBP).
ObjectivesTo investigate the effectiveness of hip strengthening exercises when added to manual therapy and lumbar segmental stabilization in patients with chronic nonspecific LBP.
MethodsSeventy patients with chronic nonspecific LBP were randomly assigned to either the manual therapy and lumbar segmental stabilization group or the manual therapy and lumbar segmental stabilization plus specific hip strengthening group. A 10 cm visual analogue scale and the Rolland-Morris Questionnaire were the primary clinical outcome measures at baseline, at the end of treatment (posttreatment), and 6- and 12-months posttreatment. Hip strength and kinematics were measured as secondary outcomes .
ResultsWhile within-group improvements in pain, disability, and hip extensors strength occurred in both groups, there were no significant between-group differences at posttreatment or follow-ups. Mean difference in changes in pain level between groups at posttreatment and at 6- and 12-month follow-up were 0.5 points (95% confidence interval [CI]: -0.5, 1.5), 0.3 points (95% CI: -0.9, 1.5), and 0.0 points (95% CI: -1.1, 1.1), respectively. The mean differences in changes in disability were 0.8 points (95% CI: -1.3, 2.7), 0.0 points (95% CI: -2.4, 2.4), and 0.4 points (95% CI: -2.0, 2.8), respectively. Finally, we did not observe any between-group differences for any of the other outcomes at any timepoint.
ConclusionThe addition of specific hip strengthening does not appear to result in improved clinical outcomes for patients with nonspecific LBP.
Recommendations on physical therapy interventions to treat low back pain (LBP), such as manual therapy and lumbar segmental stabilization, often depend on the patient's classification (e.g. non-specific) and symptom duration (i.e. acute or chronic).1 However, given that exercise therapy provides, at best, small to moderate benefits and there is no clear evidence to support any specific type of exercise,1 new interventions are needed to be developed and tested in randomized controlled trials. Strong evidence has been found to support the use of hip muscle strengthening in persons with hip and knee injuries.2–6 However, it is still unclear whether the addition of hip strengthening exercises can reduce pain and disability in people with nonspecific LBP.7–10
A recent systematic review and meta-analysis7 found that the addition of specific hip strengthening exercises to conventional rehabilitation therapy may be beneficial for improving pain and disability. However, the quality of evidence was moderate for pain and low for disability, which suggests that high-quality research is still needed for more definitive conclusions.7 Furthermore, clinicians commonly examine and provide interventions directed at the hips for people with LBP.11 The rationale is that the gluteal muscles provide pelvic stability in the frontal and sagittal plane which, in turn, provides a stable base for the lumbar spine.8,12–14
Therefore, this study aims to determine if the addition of specific hip strengthening exercises to manual therapy and lumbar segmental stabilization exercise is effective in reducing pain and disability at short-term and long-term follow-ups compared to manual therapy and segmental stabilization exercises in patients with nonspecific LBP.
MethodsStudy designThis randomized clinical trial was conducted at Centro Universitário São Camilo (CUSC), São Paulo, Brazil. The study was approved by the CUSC Research Ethics Committee (protocol 53028116.0.0000.0062) and reported according to CONSORT guidelines.15 This project was funded by the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP) and prospectively registered at Clinicaltrials.gov (NCT02517606).
PatientsSeventy patients with nonspecific LBP were enrolled in this randomized clinical trial. Patients were randomly assigned to 1 of 2 groups: a manual therapy and lumbar segmental stabilization group (MTLS group, n = 35) or specific hip strengthening exercises plus manual therapy and lumbar segmental stabilization group (MTLSHS group, n = 35).
All volunteers were informed of the study procedures and signed the informed consent forms prior to data collection. To be included in this study participants had to report chronic nonspecific LBP for at least 3 months without radicular symptoms. Patients were eligible if they presented with a strength deficit greater than 20% using a hand-held dynamometer for at least one of the hip muscle groups (abductors or extensors) compared to our database of asymptomatic individuals collected in a previous study.16 Participants were recruited from the Rehabilitation Service at CUSC by a single physical therapist with more than 15 years of clinical experience and who did not participate in treatment sessions. Participants were referred to the study from waiting list and local and online advertisement. Participants were excluded if they had any contraindication to exercise, neurological disorders, severe spinal diseases (e.g. fractures, tumors, or inflammatory conditions such as ankylosing spondylitis), lumbar radiculopathy (i.e. pain radiating below the knee with neurological deficits such as muscle weakness, reflex changes, or sensory deficits), spondylolisthesis with neurological impairment or stenosis, or severe cardiorespiratory diseases. We also excluded pregnant women or those patients who were taking corticosteroids or anti-inflammatory medication.17 A standard spine and lower extremities clinical examination was performed to rule out concomitant pathologies.
Randomization and allocationRandomization was conducted using a computer-generated randomized table of numbers created by an independent statistician. The allocation was conducted by an independent researcher who was not involved with other experimental procedures. Simple randomization results were concealed in sealed envelopes with consecutive numbers.15
ProceduresAll patients received a course of 10 treatment sessions, twice a week for 5 weeks. In the MTLS group, treatment sessions lasted approximately 30 min. In the MTLSHS group, sessions lasted approximately 45 min. Three physical therapists were trained in the study's intervention protocols and provided all treatment.
The MTLS group received a treatment consisting of a combination of manual therapy and lumbar segmental stabilization exercises. The manual therapy intervention delivered included joint mobilization in accordance with the Maitland method18 and myofascial release following the tender point principles.19 These manual techniques were intended to reduce muscle hyperactivity and joint stiffness as well as to improve lumbar spine range of motion. Posterior-anterior central mobilization was performed at selected segments between L1 to L5 that were considered stiff upon manual examination. The lumbar segmental stabilization focused on training the recruitment of the deep stabilizer muscles, such as transverse abdominal muscle, multifidus muscle, pelvic floor muscles, and diaphragm.20,21
Participants allocated to the MTLSHS group received the same treatment as described above with the addition of four exercises specifically designed to strengthen the hip muscles, performed at the end of the treatment session (Table 1).22,23 The load during training was standardized to 70% of the estimated 1-repetition maximum test, defined as the maximum load that can be lifted once while maintaining correct technique and without increasing pain. Exercises that used elastic resistance were standardized to the maximum resistance at which the patient was able to perform 10 repetitions. Patients performed these exercises solely during the physical therapy session and were not instructed to perform exercises at home.
Treatment Protocol Performed By the MTLS and MTLSHS Group.
| MTLS |
|---|
| Posterior-anterior-central (PAC) joint mobilization, grade III - L1-L5, 5 repetitions for 1-minute |
| Myofascial release - tender point type |
| Lumbar paravertebral muscles, 2 tender-points for 1-minute each |
| Quadratus lumborum, 1 tender-point for 1-minute |
| Piriformis, 2 tender-points for 1-minute each |
| Gluteus medius, 1 tender-point for 1-minute |
| Iliopsoas, 1 tender-point for 1-minute |
| Segmental stabilization exercises |
| Transverse abdominal activation, 10 isometric contractions for 10-seconds each |
| Transverse abdominal activation with alternating movements of the leg on the table, 10 repetitions on each side |
| MTLSHS |
| Same protocol as the control group |
| Hip strengthening exercises |
| Clam, hip lateral rotation and abduction in lateral decubitus against elastic resistance, 3 sets of 10-repetitions* |
| Lateral straight leg raise, hip abduction against ankle weight resistance, 3 sets of 10-repetitions** |
| Squatting with elastic resistance around the knees, 3 sets of 10-repetitions |
| Lateral stepping with elastic resistance around the knees, 3 steps for each direction, 10-repetitions |
Abbreviations: MTLS, Manual Therapy and Lumbar Stabilization; MTLSHS, Manual Therapy and Lumbar Stabilization plus Hip Strengthening.
* Maximum resistance that enables 10 repetitions.
** Load is 70% of the 1-repetition maximum.
All clinical tests and questionnaires were conducted by a single examiner at baseline, posttreatment, and 6- and 12-months posttreatment. This examiner was blinded to the patients’ group assignment and did not participate in the intervention sessions.
A 10 cm visual analog scale was used to quantify average pain intensity in the last 7 days,24 where 0 corresponded to no pain and 10 to the worst imaginable pain. A change of 2.0 cm or greater in the visual analog scale was considered the minimum clinically important difference.25 The Roland-Morris Questionnaire24,26 has been used to measure function in patients with LBP. The Roland-Morris is a 24-item functional assessment, with higher scores indicating greater disability. The minimal clinically important difference is 3.5 points in absolute values.25 These measures were administered before treatment, posttreatment, and at 6- and 12-months follow-up.
Secondary outcome measuresA previously calibrated hand-held dynamometer (Lafayette Instrument Company, Lafayette IN, USA) was used to measure hip muscle strength.16 Two submaximal trials were used to familiarize the patient with each test position followed by two maximal isometric contractions for each muscle group on both sides. The tested side (right or left) and the order of muscle testing were randomized. To stabilize the lower limb, a rigid band was employed around the treatment table. Data from the two maximum effort trials were averaged and used for statistical analyses. Each contraction was held for 5 s, with a 30-second rest period between trials. Strength values were measured in kilograms and were normalized to body mass index. The position of the patient and resistance application were based on a previous study by Magalhães et al.16
Two-dimensional kinematic analysis of the lower limb, pelvis, and trunk were assessed using the Myovideo system (Noraxon, Scottsdale, AZ, USA) while the patient walked on a treadmill and while performing a single-limb stepdown, a detailed description of these procedures is in Supplementary Material. The measures of strength and the kinematic parameters were analyzed at pretreatment and posttreatment. Although the reliability of strength assessment and kinematics has already been tested in previous studies,27,28 a pilot study was conducted 1 month prior to data collection with 10 asymptomatic individuals to evaluate the test-retest reliability in the laboratory. The individuals were tested according to the protocol described in the supplementary material, with a 1-week interval between the 2 testing sessions. We found in the pilot study that all comparisons of strength and kinematic data showed excellent reliability with intraclass correlation coefficients between 0.83 and 0.98.
Statistical analysisDescriptive statistics for demographic data and all outcome measures were expressed as mean ± standard deviation (SD). The normality of distribution was verified through the visual inspection of histograms and assessed with the Shapiro-Wilk test. Data from the visual analogue scale and the Rolland-Morris Questionnaire were analyzed using separate 2-by-4 (group-by-time) mixed model analyses of variance. The factor of group had 2 levels (MTLS and MTLSHS) and the repeated factor of time had 4 levels (pretreatment, posttreatment, and 6- and 12-months posttreatment). Between-group difference in change scores were expressed as mean difference and 95% confidence interval (CI). Measures of strength and kinematic data at baseline and posttreatment were evaluated using pairwise comparisons. All participants were analyzed in the group they were randomized, following the intention-to-treat approach. Missing data were imputed using the last observation carried forward method. Statistical significance was set at 0.05. Data were analyzed with SPSS Version 20.0 (SPSS Inc, Chicago, IL, EUA). The sample size calculation was based on the pain visual analog scale (average pain in the last 7 days) with 80% power to detect an intervention effect that would generate a difference between groups of 1.5 ± 2.1 cm29,30 with an alpha value set at 0.05. A total of 31 participants per group was estimated. To allow for potential dropouts, 70 participants were recruited for this study.
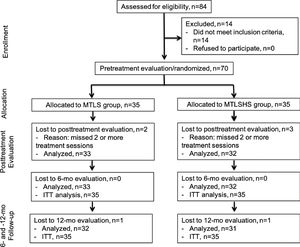
ResultsA total of 84 potential participants were recruited between June 2016 and January 2019. Of these, 14 were excluded because they did not meet the inclusion criteria. The remaining 70 participants (37 females and 33 males) were divided into the MTLS (n = 35, mean age=35 years) and the MTLSHS groups (n = 35, mean age=40 years). Three patients in the MTLS group and four patients in the MTLSHS group dropped out of the study (Fig. 1). The participants’ demographic characteristics at baseline are shown in Table 2.
Demographic and Baseline Characteristics of the MTLS and MTLSHS Groups*.
| MTLS (n = 35) | MTLSHS (n = 35) | |
|---|---|---|
| Demographic | ||
| Age, y | 35.2 ± 12.5 | 40.2 ± 12.4 |
| Body mass, kg | 72.6 ± 15.6 | 75.8 ± 15.9 |
| Height, m | 1.69 ± 0.1 | 1.71 ± 0.1 |
| Body mass index, kg/m2 | 25.3 ± 4.6 | 25.9 ± 5.4 |
| Duration of symptoms, mo | 6.9 ± 8.1 | 8.1 ± 8.9 |
| Baseline | ||
| Visual Analogue Scale (0–10)** | 5.6 ± 2.1 | 5.5 ± 2.1 |
| Roland-Morris (0–24)*** | 9.1 ± 4.7 | 8.5 ± 4.6 |
Abbreviations: MTLS, Manual Therapy and Lumbar Stabilization; MTLSHS, Manual Therapy and Lumbar Stabilization plus Hip Strengthening.
* Values are mean ± SD.
** Score from 0 to 10, where 0 is no pain and 10 is the worst imaginable pain during last week.
*** Lower score represents better function.
Both groups showed improvements in pain and disability relative to baseline, however, there was no meaningful difference between groups at posttreatment and follow-ups (Table 3). The mean difference in changes in pain level between groups at posttreatment, and at 6- and 12-month follow-up were 0.5 points (95%: −0.5, 1.5), 0.3 points (95% CI: −0.9, 1.5), and 0.0 points (95% CI: −1.1, 1.1), respectively. The mean differences in disability were 0.8 points (95% CI: −1.3, 2.7), 0.0 points (95% CI: −2.4, 2.4), and 0.4 points (95% CI: −2.0, 2.8), respectively (Table 3).
Outcome Measures (Pain and Function).
| MTLS (n = 35) | MTLSHS (n = 35) | Between-group difference in change scores | |
|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean (95% CI) | |
| VAS (0–10)* | |||
| Pretreatment | 5.6 ± 2.1 | 5.5 ± 2.1 | |
| Posttreatment | 2.9 ± 2.0 | 2.3 ± 2.2 | 0.5 (−0.5, 1.5) |
| 6 mo posttreatment | 3.9 ± 2.7 | 3.5 ± 2.7 | 0.3 (−0.9, 1.5) |
| 12 mo posttreament | 3.3 ± 2.7 | 3.2 ± 2.5 | 0.0 (−1.1, 1.1) |
| Roland-Morris (0–24)** | |||
| Pretreatment | 9.1 ± 4.7 | 8.5 ± 4.6 | |
| Posttreatment | 4.3 ± 3.5 | 4.5 ± 4.4 | 0.8 (−1.3, 2.7) |
| 6 mo posttreatment | 5.7 ± 5.7 | 5.1 ± 5.4 | 0.0 (−2.4, 2.4) |
| 12 mo posttreament | 4.7 ± 5.5 | 4.5 ± 5.3 | 0.4 (−2.0, 2.8) |
Abbreviations: MTLS - Manual Therapy and Lumbar Stabilization, MTLSHS - Manual Therapy and Lumbar Stabilization plus Hip Strengthening, VAS - Visual Analogue Scale.
* Score from 0 to 10, where 0 is no pain and 10 is the worst imaginable pain during last week
** Lower score represents better function
Although normalized hip extensor strength increased at posttreatment in both groups, we observed no difference in either hip extensor or abductor strength between the two groups. The mean difference in hip extensors strength posttreatment was 0.8 (95% CI: −13.9, 15.5) (Table 4). There was no significant intra and between-group interaction observed for any of the kinematic variables (p > .05) (Table 4).
Outcome measures (Strength and Kinematics).
| Pretreatment | Posttreatment | Between-group difference in change scores | |
|---|---|---|---|
| Analysis / Measures* | Mean ± SD | Mean ± SD | Mean (95% CI) |
| Strength* | |||
| Hip Abduction | |||
| MTLS | 32.0 ± 10.7 | 33.3 ± 11.2 | 0.9 (−0.5, 1.4) |
| MTLSHS | 32.4 ± 11.5 | 34.6 ± 11.3 | |
| Hip Extension | |||
| MTLS | 22.0 ± 12.0 | 27.7 ± 12.0 | −0.8 (−1.2, 0.4) |
| MTLSHS | 23.6 ± 12.3 | 28.5 ± 13.3 | |
| Kinematics - Gait⁎⁎ | |||
| Contralateral pelvic drop | |||
| MTLS | 4.2 ± 2.5 | 4.3 ± 2.7 | −0.2 (−1.5, 1.1) |
| MTLSHS | 4.3 ± 2.8 | 4.6 ± 2.6 | |
| Ipsilateral trunk lean | |||
| MTLS | 5.4 ± 2.5 | 4.8 ± 2.6 | 0.4 (−0.9, 1.7) |
| MTLSHS | 4.9 ± 2.9 | 4.7 ± 2.9 | |
| Kinematics - STD⁎⁎ | |||
| Knee Valgus | |||
| MTLS | 8.1 ± 7.3 | 7.9 ± 6.9 | 0.6 (−2.5, 3.7) |
| MTLSHS | 6.4 ± 6.1 | 6.8 ± 5.5 | |
| Contralateral pelvic drop | |||
| MTLS | 1.8 ± 3.3 | 2.1 ± 3.5 | 0.2 (−1.5, 1.9) |
| MTLSHS | 1.5 ± 3.8 | 2.0 ± 3.7 | |
| Ipsilateral trunk lean | |||
| MTLS | 6.4 ± 3.9 | 6.0 ± 4.0 | −0.4 (−2.2, 1.4) |
| MTLSHS | 6.2 ± 4.1 | 5.4 ± 3.2 |
Abbreviations: MTLS, Manual Therapy and Lumbar Stabilization (n = 35); MTLSHS, Manual Therapy and Lumbar Stabilization plus Hip strengthening; STD - Stepdown test.
⁎ Strength values (kg) are normalized with the body mass.
The results of this prospective, randomized, and assessor-blinded clinical trial demonstrated that specific hip strengthening exercises do not provide additional benefits to clinical and kinematic outcomes in patients with chronic nonspecific LBP.
Rehabilitation programs that involve exercise and manual therapy have previously been shown to reduce symptoms and disability and improve functional ability in persons with LBP.31,32 However, there is no evidence to support the use of one exercise approach over another because the relative effectiveness of different approaches has been shown to be comparable.20,33,34 Manual therapy and segmental stabilization were selected for this study as they are widely used in clinical practice,1 and are considered the first line treatment for this population.
To our knowledge, there is currently only one systematic review with meta-analysis related to LBP and hip weakness.8 This review reported that patients with LBP exhibited diminished hip abductor and hip extensor strength compared to healthy controls, but did not explore the effects of treatment on this population.8 Hip muscle strengthening has recently been suggested for the management of LBP.9,10 A study by Bade et al9 reported significant improvements with the addition of hip strengthening exercises, however this study also included mobilization techniques to improve hip range of motion. Although limited hip internal rotation may be associated with nonspecific LBP, we did not add mobilization techniques due to the low-quality evidence.35 Our results corroborate those of Kendall et al,36 who found no additional effects of hip strengthening when associated with physical therapy focused to the lumbar region.
The fact that there were no between-group differences in hip strength shows that the proposed hip strengthening protocol (10 sessions, 2 times a week for 5 weeks) was not effective in this population. This may be because it does not provide adequate time for motor learning. Nevertheless, it is important to highlight that this protocol was successfully used and validated in previous studies.2,5,22,23,37 These exercises were performed only at the clinic and patients were instructed not to perform them at home. It is important to note that all patients were instructed not to use anti-inflammatory or analgesic medication during treatment, but this was not enforced after treatment. Future studies should explore alternate hip strengthening programs with variation in frequency of sessions, time, intensity, or types of exercises in this population. The absence of kinematic changes in both intra-group and inter-group analyses showed that providing simple and isolated hip strengthening exercises was not able to change kinematics during functional tasks, however future studies exploring functional movement control exercises or gait retraining are necessary.
This study presents some limitations. The protocol was designed to minimize sources of bias however, given the nature of the intervention, blinding the treating therapists and patients was not possible. Another limitation is that the study measured limited demographic factors and a small number of participants, although we used a pragmatic sample size calculation. Manual therapy focused on hip range of motion was also not applied, because the scope of the study was to evaluate the addition of isolated hip strengthening. Patients only performed 2 exercises for the lumbar segmental stabilization. It is known that the focus of the early phases is on the deep muscles but progression towards superficial trunk muscles could have been added. Furthermore, given that the cause of chronic low back pain may be multi-factorial, biopsychosocial factors, pain-related fear, or kinesiophobia assessments could have been incorporated.
ConclusionThese findings indicate that the addition of specific hip strengthening exercises to a MTLS program did not significantly improve the outcomes of pain and function. Therefore, clinicians should rethink the use of these exercises since hip strengthening confer no benefit over the first year.
This study received financial support from Fundo de Amparo e Pesquisa do Estado de São Paulo - FAPESP, Brazil - project #2015/07302-8.
TRIAL REGISTRATION: NCT02517606, https://clinicaltrials.gov/ct2/show/NCT02517606?term=NCT02517606&cond=low+back+pain&cntry=BR&draw=2&rank=1.