This statistical analysis plan details the Coaching for Healthy AGEing (CHAnGE) trial analysis methodology.
ObjectiveTo investigate the effect of a combined physical activity and fall prevention program on physical activity and falls compared to a healthy eating among people aged 60 years and over.
MethodsThe CHAnGE trial is a pragmatic parallel-group cluster-randomised controlled trial with allocation concealment and blinded assessors. Clusters are allocated to either (1) a physical activity and fall prevention intervention or (2) to a healthy eating intervention. The primary outcomes are: objectively measured physical activity at 12 months post-randomisation, and self-reported falls throughout the 12-month trial period. Secondary outcomes include the proportion of participants reporting a fall, the proportion of participants meeting the Australian physical activity guidelines, body mass index, eating habits, mobility goal attainment, mobility-related confidence, quality of life, fear of falling, risk-taking behaviour, mood, well-being, self-reported physical activity, disability, and use of health and community services.
AnalysisWe will follow the intention-to-treat principle. All analysis will allow for cluster randomisation using a generalised estimating equation approach. The between-group difference in the number of falls per person-year will be analysed using negative binomial regression models. For the continuously scored primary and secondary outcome measures, linear regression models adjusted for corresponding baseline scores will assess the effect of group allocation. Analyses will take into account cluster randomisation and will be adjusted for baseline scores. A subgroup analysis will assess differential effects of the intervention by baseline physical activity levels and history of falls.
Physical inactivity is a major public health concern, and older adults in particular are at the highest risk for inactivity.1,2 Inactivity is an important contributor to several chronic diseases and functional impairments more common in older age.3 Additionally, inactivity significantly reduces strength and balance which increases the risk of falls and fall-related injury.4 Falls have devastating consequences among older people, including serious injury and lasting disability, admission to a residential aged care facility, and even death.5
There is a high level of evidence showing that exercise is effective in preventing falls.4 A recent systematic review and meta-analysis6 found that exercise programs are effective in reducing the fall rate by at least 21%, with greater effects (up to a 39% reduction in fall rate) obtained from exercise that includes a higher challenge to balance and higher dose of training. Conversely, there is some evidence that increasing overall physical activity participation (in particular, brisk walking) in older age may lead to a greater likelihood of falls, due to the increased exposure to fall hazards in the environment.7,8
Therefore, there is some evidence that physical activity interventions should provide fall prevention advice to optimise safety and health benefits. However, there is a lack of large randomised controlled trials that have investigated the effect of a combined physical activity and fall prevention intervention among older people.
The Coaching for Healthy AGEing (CHAnGE) trial is a cluster-randomised controlled trial designed to measure the effect of a physical activity and fall prevention program among people aged 60 years and over. Participant recruitment commenced in September 2015 and finished in September 2018. The present article is the detailed statistical analysis plan (SAP) to support transparency and reproducibility of data analysis. The SAP was approved by the study investigators and gives details of the statistical methods that will be used to analyse the primary and secondary outcomes. Details of the planned health economic analysis will be published in a separate manuscript.
MethodsTrial designThe CHAnGE trial is a pragmatic, parallel-group cluster-randomised controlled trial with allocation concealment and blinded assessors. The CHAnGE trial evaluates the effect and cost-effectiveness of a combined physical activity and falls prevention intervention compared with a healthy eating intervention. The study received ethics approval from the University of Sydney Human Research Ethics Committee (protocol number 2015/ 517). In addition to prospective registration at the Australian and New Zealand Clinical trials Registry (ACTRN12615001190594), a detailed protocol describing the methods of the study was published and is freely available online.9
Study populationSeventy-two clusters (605 people) of eligible consenting community-dwelling people were recruited from two locations in New South Wales (NSW), Australia: the metropolitan city of Sydney and regional town of Orange and surrounds, via established community-based organisations for older people (e.g. Women's Shed, Men's Sheds, Rotary and Probus) that held meetings or other events (at least once every two months) for cluster members. Participants were included if they were aged 60 years and over; living at home or in a retirement village; regularly attended meetings or other activities (at least once every 2 months) at one of the included community-based clusters.
Participants were ineligible if they: (1) had a cognitive impairment (a diagnosis of dementia or a Memory Impairment Screen10 score of less than 5); or (2) had insufficient English language skills to fully participate in the program; or (3) had a progressive neurological disease (e.g., Parkinson's disease); or (4) had a medical condition precluding exercise (e.g., unstable cardiac disease); or (5) were unable to leave the house without physical assistance from another person; or (6) were already meeting the Australian Physical Activity Guidelines for older adults11 (operationalised as 150 min of moderate intensity physical activity per week, assessed using the Incidental and Planned Exercise Questionnaire (IPEQ))12; or (7) had undergone a fall risk assessment and intervention program in the past year. If it was unclear whether a potential participant met the eligibility criteria, we sought the participant's permission to discuss this with a family member, other carer, or healthcare professional (e.g., general practitioner).
Randomisation and blindingAfter all participants within a cluster had provided individual consent and completed the baseline assessment, clusters were allocated to either the physical activity and fall prevention intervention or to the healthy eating intervention. To ensure allocation concealment, randomisation was determined by an automatic phone-based randomisation service (NHMRC Clinical Trial Centre). We used a computer-generated schedule stratified by three variables: rural/ urban location, socioeconomic status of the cluster, and whether the cluster gathering purpose involved physical activity or not.
Due to the nature of the intervention, it was not possible to blind participants and health coaches. Data for the primary (falls and physical activity) and secondary outcomes were collected by a research assistant who was blinded to group assignment throughout the trial.
Physical activity and fall prevention intervention (experimental group)Participants in the physical activity and fall prevention intervention received: (1) printed educational material about increasing physical activity and preventing falls; and (2) a home visit by a trained physical therapist which included: (a) assessment of fall risk with the QuickScreen assessment13; (b) a fall prevention and physical activity plan (co-developed by the participant and the health coach) using a motivational interviewing approach and goal setting; and (c) provision and set up of an activity tracker device (Fitbit) or pedometer for those without access to the internet.
The home visit session was followed by fortnightly telephone health coaching for a period of 12 months, delivered by the same research physical therapist who conducted the home visit. The health coaching aimed to identify barriers and facilitators to physical activity participation, and to support participants to achieve their goals. During the telephone contact, health coaches also discussed strategies to reduce the risk of falls.
Healthy eating intervention (active control group)Participants in the healthy eating intervention group received: (1) printed educational material about healthy eating; and (2) access to the Get Healthy Information and Coaching Service (Get Healthy Service) which is a telephone-based health coaching service delivered to users free of charge by the NSW Ministry of Health that focuses on healthy eating, getting active, healthy weight, and reducing smoking. We used only the service that focused on healthy eating to avoid contamination. The Get Healthy Service contacted participants approximately once a fortnight for the first 6 months, then monthly for the remaining 6 months. Although we included an active comparator, it is unlikely that the primary outcomes would be influenced by this control intervention.
Outcomes measuresThe two primary outcomes measures were: (1) physical activity, measured with the ActiGraph GT3X+, assessed over a 7-day wear period and expressed as mean counts/min/day, measured at baseline and at 12-months post randomisation; (2) falls rate recorded with monthly postal calendars over 12 months.
The secondary outcomes, measured at baseline and at 3, 6, and 12 months post-randomisation were: (1) body mass index, calculated from self-reported height and weight; (2) eating habits, assessed with questions from the Australian Health Survey; (3) quality of life, assessed with the The EuroQol-5 Dimension (EQ-5D-5L)14; (4) fear of falling, assessed using the short-form Falls Efficacy Scale International15; (5) mood, assessed with the Positive and Negative Affect Schedule16; (6) risk-taking behaviour, assessed with a 5-item self-report tool 17; (6) well-being, assessed with a 26-item composite scale of wellbeing (the COMPAS-W scale)18; (7) mobility-related confidence, assessed with the Modified Gait Efficacy Scale 19; (8) self-reported physical activity, assessed with the Incidental and Planned Exercise Questionnaire (IPEQ)12; (9) and disability, assessed with the WHO Disability Assessment Schedule II.20
Our secondary outcomes also included (10) the proportion of participants reporting a fall and (11) health and community service, both assessed using monthly calendars as described above; (12) the proportion of ActiGraph wear time in sedentary, light, moderate, and vigorous physical activity measured at baseline and at 6 and 12 months post randomisation; (13) mobility-related goal attainment, assessed using the Goal Attainment Scale21 measured at 6 and 12 months post randomisation.
Power and sample sizeA required sample size of 30 clusters per intervention group (a total of 60 clusters) with an average of 10 participants in each cluster (i.e., 600 participants) was calculated with 90% power to detect a 10% between-group difference in the primary physical activity outcome at the 5% two-sided significance level. This assumed a between-group difference of 23 mean counts/min during wear time, standard deviation of 120, dropout rate of 20%, 0.6 correlation between baseline and final measures and an intracluster correlation (ICC) of 0.01. For this calculation, we used the sampsi command in Stata V.13 and we used the estimates of mean accelerometer counts per minute for people aged 60–75 years from a large sample of accelerometer data.22
For the primary falls outcome, the 60 clusters were expected to provide 80% power to detect as significant, at the 5% two-sided significance level, a 30% lower rate of falls in intervention group participants than control participants (IRR=0.67). For this calculation, we used PASS V.14 (Power Analysis and Sample Size) Software (2015, NCSS, LLC, Kaysville, Utah, USA). We used coefficients from previous studies: overdispersion in the negative binomial regression model was assumed to be 0.65 based on a previous trial.23 We assumed: a control group rate of falls of 0.06 per person-month over the follow-up period, as this was the rate in a study of a similar population24; a design effect of 1.09 with an ICC of 0.01; and withdrawal of six clusters. An average follow-up period of 11 months was used to account for loss to follow-up. This sample size was also expected to be sufficient to detect between-group differences in the order of 10–15% for the secondary outcome measures.
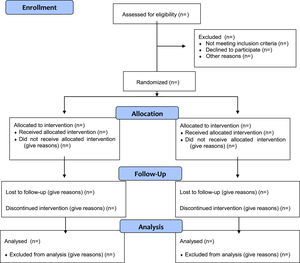
Statistical analysisAnalysis principlesThe analysis of the primary and secondary outcomes will be performed by a blinded analyst with code reviewed by the lead investigator. We will follow the intention-to-treat principle (Fig. 1). All statistical tests will be two-tailed. Data normality of baseline characteristics and process measures will be analysed by visual inspection of histograms. We will summarise continuous variables using standard measures of central tendency and dispersion, either as mean and standard deviation for normally distributed variables, or median and interquartile range for non-normally distributed variables. We will summarise dichotomous or categorical variables using frequencies or denominators and percentages. We will calculate percentages using the number of participants for whom data are available as the denominator.
Data integrityWe have monitored the integrity of trial data regularly by inspecting data files for omissions and errors. Double data checking will be conducted for all the primary (physical activity and falls) and secondary outcomes. All inconsistencies or implausible values will be investigated and rectified. Missing and out-of-range data will be checked against paper data collection forms to confirm values, and correct them if necessary.
BlindingResearchers involved in the preparation of the analysis plan remained blinded to all outcomes by study group. Blinded research assistants will check data quality and quantification of missing data using the entire dataset not broken down by group allocation. Once this process is completed, analysis and interpretation of data will be conducted using dummy group names (e.g. group 1 and group 2), and group allocation will only be unmasked after the statistical report has been completed and interpretation agreed upon.
Methods for handling missing dataWhere data are missing due to participant withdrawal or loss to follow-up, we will report the number of observations. We will not impute missing values for the primary analysis. If more than 10% of the outcome data are missing, we will use multiple imputation of missing data to conduct sensitivity analyses.
Trial profile and evaluation of demographics and baseline characteristicsWe will comply with the Consolidated Standards of Reporting Trials (CONSORT) statement25 and report the flow of participants through the study (Fig. 1). Participants’ baseline characteristics will be presented in a table stratified by treatment group (Table 1).
Participant characteristics at baseline (n = xx).
Continuous variables will be presented as means and standard deviations (mean ± SD) for normally distributed variables and median, minimum, maximum and interquartile range (median [min-max] or median [P25-P75]) for non-normally distributed variables. Frequencies and proportions will be used to summarise categorical variables (n (%)).
We will use ActiLife 6.13.3 software to analyse accelerometer data, and acceptable wear time for analysis will be defined as 4 days or more of 10 hours or more per day. Intervention effects will be assessed by means of generalised estimating equations (GEE) models using an exchangeable correlation structure to account for correlation between individuals within the clusters. The number of falls per person-year will be analysed using negative binomial regression models to estimate the difference in rates between the groups after one year (primary outcome). For the continuously scored primary (device-measured physical activity) and secondary outcome measures, Gaussian GEE regression adjusted for baseline values will be used to assess the effect of group allocation. Log-binomial GEE regression, or robust Poisson regression in case of convergence issues, will be used to compare groups on dichotomous outcome measures (proportion of fallers, proportion meeting physical activity cut-points). Group data will be presented in Table 2. Fall outcome data will be present in Table 3. Secondary analysis will be conducted to establish intervention effects in people with greater adherence by performing causal modelling.
Mean ± SDa or n (%) of groups at baseline and 6 and 12-month follow-up, mean difference (95% CI) or OR (95% CI) between groups.
| Outcome measures | Groups | Difference between groups (baseline adjusted) or odds ratio | ||||||
|---|---|---|---|---|---|---|---|---|
| Month 0 | Month 6 | Month 12 | Month 6 minus month 0 | Month 12 minus month 0 | ||||
| Int (n=xx) | Con (n=xx) | Int (n=xx) | Con (n=xx) | Int (n=xx) | Con (n=xx) | Int minus Con or Int relative to Con | Int minus Con or Int relative to Con | |
| CPM from accelerometer*,1 | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | mean (95% CI) | mean (95% CI) |
| IPEQ (hours/week)* | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | mean (95% CI) | mean (95% CI) |
| Meets recommendation of 150 min per week of MVPA | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | OR (95% CI) | OR (95% CI) |
| Daily steps (number)* | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | mean (95% CI) | mean (95% CI) |
| BMI | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | mean (95% CI) | mean (95% CI) |
| Meets Australian Dietary Guidelines | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | OR (95% CI) | OR (95% CI) |
| EQ-5D-5L quality of life* | ||||||||
| Mobility domain (1–5) | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | mean (95% CI) | mean (95% CI) |
| Self-care domain (1–5) | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | mean (95% CI) | mean (95% CI) |
| Usual activities domain (1–5) | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | mean (95% CI) | mean (95% CI) |
| Pain or discomfort domain (1–5) | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | mean (95% CI) | mean (95% CI) |
| Anxiety or depression domain (1–5) | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | mean (95% CI) | mean (95% CI) |
| VAS score (0-100) | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | mean (95% CI) | mean (95% CI) |
| Health utility score (−0.68 to 1) | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | mean (95% CI) | mean (95% CI) |
| Falls efficacy scale(7-28)§ | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | mean (95% CI) | mean (95% CI) |
| PANAS scale, (10–50)* | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | mean (95% CI) | mean (95% CI) |
| Risk-taking bahavior (5-20)¿ | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | mean (95% CI) | mean (95% CI) |
| COMPAS-W scale (raw score 26-130)* | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | mean (95% CI) | mean (95% CI) |
| Modified Gait Efficacy Scale (10–100)* | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | mean (95% CI) | mean (95% CI) |
| WHO Disability Assessment Schedule 2.0 (raw score 12–60)§ | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | xx ± xx | mean (95% CI) | mean (95% CI) |
1CPM (counts/minute) = primary outcome
Int=intervention group, Con= control group, CPM: Counts per minute, Incidental and Planned Exercise Questionnaire MVPA: Moderate to vigorous physical activity, BMI=Body Mass Index, PANAS: Positive and Negative Affect Schedule (Positive affect subscale score), COMPASS=composite scale of wellbeing
Continuous variables will be presented as means and standard deviations (mean ± SD) for normally distributed variables and median, minimum, maximum and interquartile range (median [min-max] or median [P25-P75]) for non-normally distributed variables. Frequencies and proportions will be used to summarise categorical variables (n (%))
Fall outcomes at 12 months.
| Intervention | Control | |
|---|---|---|
| Number of participants | xx | xx |
| Number of falls | xx | xx |
| Participants with at least 1 fall, n (%) | n (%) | n (%) |
| Participants with 2 or more falls, n (%) | n (%) | n (%) |
| Participants with 3 or more falls, (n (%) | n (%) | n (%) |
| Participants with 4 or more falls, n (%) | n (%) | n (%) |
| Number of injurious falls# | xx | xx |
| Participants with injurious falls#, n (%) | n (%) | n (%) |
| Mean ± SD surveillance period (weeks) | xx±xx | xx±xx |
| IRR (95% CI) | xx (xx to xx) | |
We will categorise adverse events (AEs) as minor AEs or serious AEs. A minor AE is defined as an incident that occurs while the person is participating in the intervention that results in no injury or minor injury. For example, a fall where the person sustains a small cut or bruise that requires none or minor medical intervention. A serious AE (SAE) is defined as an incident that occurs while the person is participating in the intervention that results in death, serious injury, or require prolong inpatient hospitalisation. Examples of SAEs are death, myocardial infarction, falls leading to serious injuries including fractures, and epilepsy/seizures. Deaths in both groups will also be documented. We will report the frequency and proportion of participants who experience minor AEs and/or serious AEs.
Subgroup analysisPlanned subgroup analyses will assess differential effects of the intervention by baseline physical activity levels and history of falls.
ConclusionThe CHAnGE trial aims to provide rigorous direct evidence about the effectiveness and cost-effectiveness of a healthy ageing program targeting falls and inactivity among older people. This statistical analysis plan details the analyses planned for the study, to support transparency of results, and may assist the design of future studies.
Trial statusParticipant recruitment was completed in September 2018 and follow-up outcomes were completed in September 2019. Data cleaning and preparation were completed in October 2020.
Ethics approvalThe trial was approved by the Human Research Ethics Committee at the University of Sydney (protocol number 2015/ 517)
Source(s) of supportA.T., C.S. and S.R.L are supported by grants and research fellowships from the National Health and Medical Research Council (NHMRC), Australia.