Existing mobility scales for hospitalized patients do not include assessment of tasks for the right and left side, ability to transfer from sitting to lying and from standing to sitting, ability to climbing steps and pick up an object from the floor in the same instrument.
ObjectiveEvaluate the reliability and validity of the hospital mobility assessment scale (HMob) according to the Consensus-based standards for the selection of health measurement instruments (COSMIN).
MethodsStudy conducted in three inpatient units (cardiology, neurology, and gastrohepatology) and one adult intensive care unit in a hospital. Patients of both sexes were included; age >18 years; collaborative and who obeyed commands, with different medical diagnoses and clinical release to leave their bed (provided by the doctor). Special populations such as those with burns and orthopedics were excluded.
ResultsThe sample consisted of 130 patients; 20 from the pilot study and 110 to assess the clinimetric properties of the HMob. Cronbach alpha coefficient was 0.949. Relative intra- (A1-A2) and inter-rater (A1-B; A2-B) reliability was excellent (A1-A2: ICC = 0.982, p-value < 0.0001; A1-B: ICC = 0.993, p-value < 0.0001; A2-B: ICC = 0.986, p-value < 0.0001.) The convergent criterion validity of HMob in relation to the ICU Functional Status Score was 0.967 (p-value < 0.0001) and for Functional Independence measure (MIF) was 0.926 (p-value < 0.0001).
ConclusionThe HMob scale showed excellent internal consistency, intra- and inter-rater reliability, and concurrent validity in the motor domain, which suggests that it can be used in daily practice to measure mobility in hospitalized patients.
Mobility is defined as the ability to move independently and safely to perform activities and functional tasks, as well as participate in activities of daily living at home, at work, and in the community.1 Hospitalization predisposes to a decline in this mobility,2-5 especially in patients with more severe conditions or those who spend longer periods in a low level of activity.6 This occurrence is associated with a higher risk of hospital readmission, long-term disability, and higher mortality one year after hospital discharge, making it important to measure mobility in the hospital environment.2,7
The purpose of mobility measurement is to accurately describe functional changes, stratify the risk of functional loss for each patient, direct interventions according to the degree of previous function, document the effectiveness of interventions, and compare to results in the literature.2,3,8 Some functional scales have been described in the scientific community and there are currently several scales that propose to assess aspects of mobility of hospitalized patients.9,10 However, none of them meets all the needs that help professionals in this task, in a feasible and objective way, while having strong measurement properties.10,11 To develop a reliable scale for evaluating mobility assessment in hospitalized patients, it is necessary to validate the characteristics of this scale according to Consensus-based Standards of the selection of health Measurement Instruments (COSMIN).12
Existing scales do not include assessment of tasks performed for the right and left side, ability to transfer from sitting to lying and from standing to sitting, ability to climb steps and pick up an object from the floor using the same instrument, skills related to an adequate level of independence for activities of daily living. Thus, the aim of this study was to develop and evaluate the reliability and concurrent validity of the hospital mobility assessment scale (HMob). With the formulation of the new instrument, it is expected to monitor specific aspects of the mobility of hospitalized patients more precisely, with the potential to significantly contribute to the diagnosis and physical therapy prognosis of these patients.
MethodsThis study was conducted in accordance with the COSMIN.12,13 The research project was approved by the ethics committee of the Hospital Universitário Professor Edgard Santos (HUPES) of the Universidade Federal da Bahia (UFBA) with opinion number 5.512.119. All participants signed the informed consent form before participating in this study.
Study setting, population, and data collectionThis study was conducted in three inpatient units (cardiology, neurology, and gastrohepatology) and an adult intensive care unit of a university hospital. The selected sample was patients hospitalized during the period from 2019 to 2022. Patients of both sexes were included; aged >18 years; collaborative and who obeyed commands; with different medical diagnoses; and with clinical release to leave their bed (provided by the doctor). Exclusion criteria were special populations such as burned and orthopedic patients or those who did not agree to participate in the study.
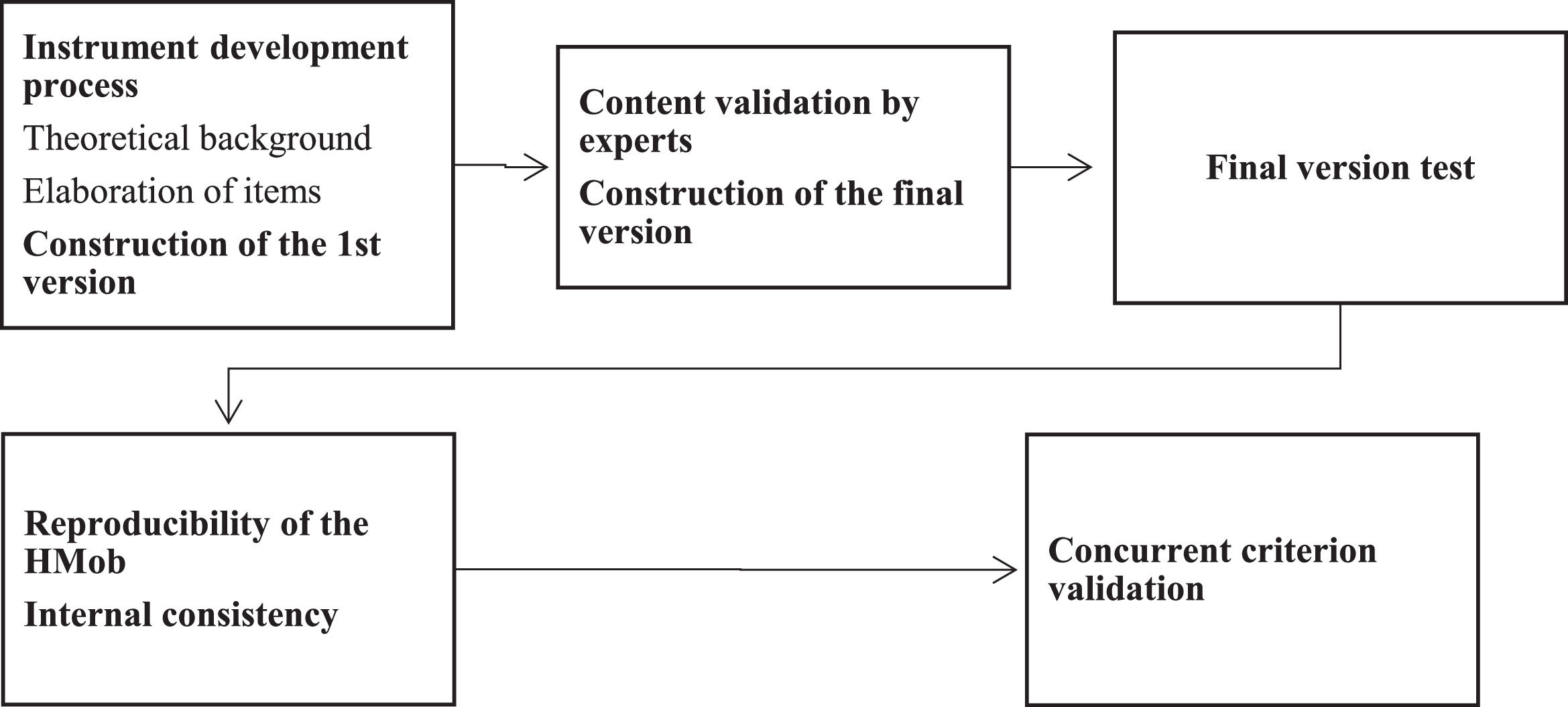
Study proceduresThe scale was developed based on the mobility-related domains of the International Classification of Functioning, Disability and Health (ICF) and on previous scales on mobility, and was modified throughout phase 1 of the study and subsequently assessed by 5 specialist physical therapists with >10 years of expertise in hospital care. After final analysis, the instrument was submitted to Phase 2.14Fig. 1 describe all methodological procedures for the initial development and the reliability and validity assessment of the HMob scale.
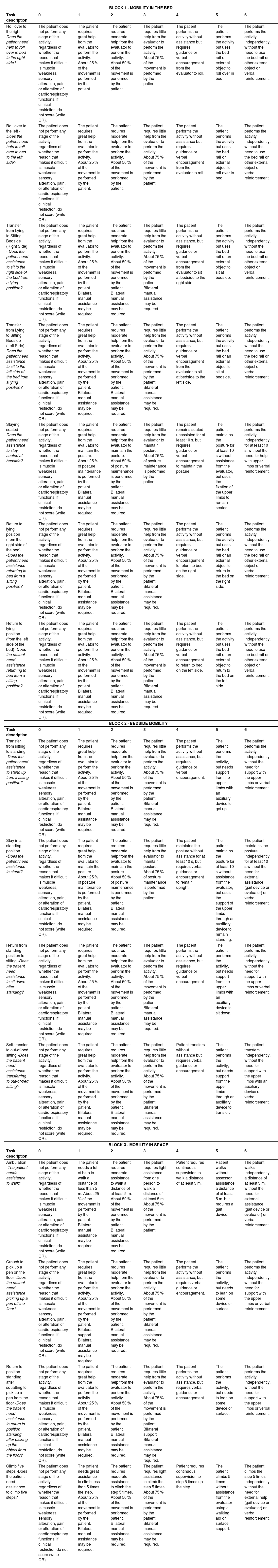
The HMob scale consists of an alphanumeric scoring instrument divided in 3 blocks to more easily identify the patient's function:
- •
Block 1 (mobility in bed): rolling on the right and left side, moving from lying down to sitting (on the right and left side of the bed), remaining seated at the edge of the bed and returning to lying in bed (on the right and left side), evaluating the patient's performance for both sides, as well as the ability to return to bed after sitting. The score ranges from 0 to 42 points.
- •
Block 2 (bedside mobility): transfer activities to standing, stay in a standing position, transferring to sitting in a chair next to the bed, and sitting after standing. The score ranges from 0 to 24 points.
- •
Block 3 (mobility in space): ability to walk at least 5 m, climb steps 5 times, pick up a pen from the floor, and return to orthostasis after picking up the pen from the floor. The score ranges from 0 to 24 points.
The score ranges from 0 to 6 points for each item, with a score of 0 when the patient does not perform the activity and 6 when the patient performs the activity independently, with a total possible HMob score ranging from 0 to 90 points. In case of clinical restrictions preventing assessment of a given task, the acronym “CR,” which indicates Clinical Restriction, was used. The complete description of the Hmob scale is in Table 1.
Full description of the Hmob scale.
In phase 2, bedside mobility was assessed using the new instrument (HMob Scale) and the Functional Status Score for the Intensive Care Unit scale (FSS-ICU)3 to determine concurrent criterion validity. Clinical and sociodemographic data were gathered from the medical records, muscle strength was measured using the Medical Research Council Score (MRC), and mobility prior to hospitalization was recorded using the Barthel index.15,16
The evaluators were composed of the hospital's physical therapists, physical therapy students, and the primary researcher, all previously trained in the application of the HMob Scale. To assess reliability, the HMob was applied by 2 independent evaluators, one of which evaluated the patient on two occasions for intra-examiner evaluation, with no contact between them during the measurement interval. Physical therapist A1 performed the Hmob (test 1) and physical therapist B performed the other assessment with the Hmob (test 2) to assess inter-rater reliability. One of the evaluators completed the 2nd evaluation (A2 re-test) during the opposite shift. Assessments were conducted in the morning before any rehabilitation session and in the afternoon, where patients may or may not have already undergone a rehabilitation session. Assessments were conducted at different times, but under similar conditions, to minimize bias in the assessment. The research hospital rooms are spacious and allow patients to be transferred to both sides, which minimizes measurement bias. The safety criteria adopted for interrupting the mobility evaluation were peripheral oxygen saturation (SpO2) <92 %; respiratory rate (RR) >35 breath per minute (bpm); report of dyspnea; use of accessory breathing muscles or paradoxical pattern; symptomatic postural hypotension; systolic blood pressure (SBP) < 90 or >160 mmHg; heart rate (HR) <50 or >130 beats per minute (bpm); cardiac arrhythmia; and pain.17
Statistical analysisData were analyzed with SPSS Statistics version 22.0 (SPSS, Inc, Chicago, Ill). Content validity was assessed through the qualitative assessment of a committee of experts composed of four physical therapists (three PhDs and one specialist). Reliability and validity were the clinimetric properties analyzed on HMob. Interrater reliability of the Hmob was tested by the calculation of intraclass correlation coefficients (ICC) and internal consistency was assessed using Cronbach's coefficient α. Cronbach's coefficient α values between 0.81 and 1: almost perfect; 0.61 to 0.80: substantial; 0.41 to 0.6: moderate; 0.21 to 0.40: fair; 0 to 0.21: small.18 To assess the relative intra- and inter-rater reliability, the ICC was used, with the following interpretation (0.76 to 1: excellent; 0.61 to 0.75: good; 0.4 to 0.6: fair; < 0.4: poor).19,20 To assess absolute reliability, Bland-Altmann was used to analyze the precision between the intra- and inter-examiner measurements. The concurrent criterion validity was assessed using Pearson's correlation analysis for the HMob scores and those obtained on the Functional Status Score for the Intensive Care Unit (FSS-ICU), a validated instrument that evaluates the same construct (mobility), as well as with the Functional Independence Measure (FIM), for the motor domain, which assesses functional independence.18,21 Ceiling and floor effects were tested by frequency and considered present if 15 % or more of the items reached the maximum or minimum scores on the instrument. A p-value <0.05 was considered statistically significant.
ResultsThe final version of the HMob consisted of the evaluation of 15 mobility-related tasks, which were divided into three blocks (mobility in bed, bedside, and space), with a score from 0 to 6 for each task. We identified excellent clinimetric properties of internal consistency, intra- and inter-rater reliability, and validity in relation to the FSS and MIF scales.
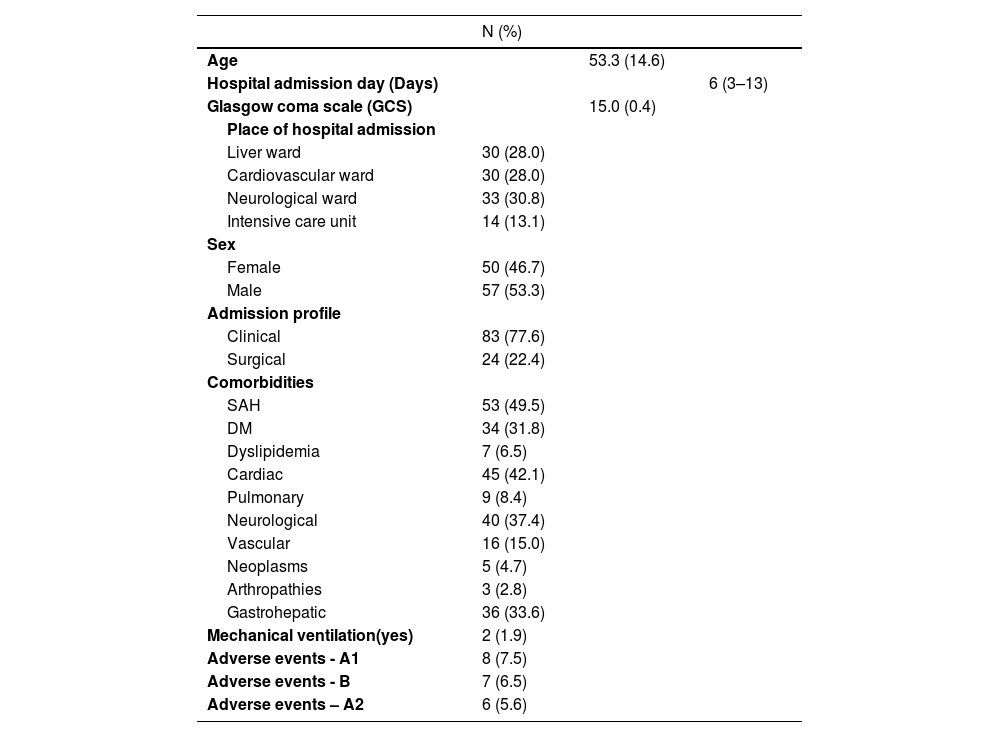
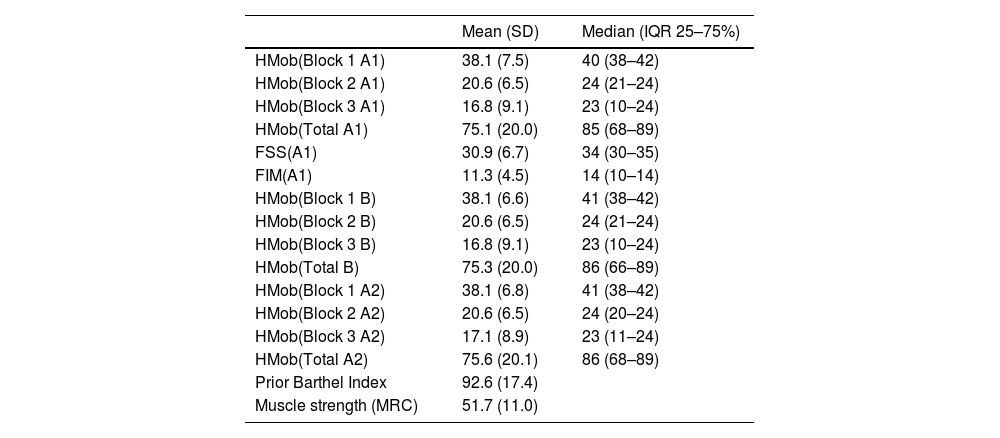
The testing of items in an independent sample was performed on 110 patients with a mean (standard deviation) age of 53.3 (14.6) years, most of whom had an admission diagnosis for a clinical (non-surgical) reason (77.6 %). Table 2 shows the baseline characteristics of the patients included in this study. The mean previous functional independence measured prior to hospitalization by the Barthel index was 92.6 (17.4), with a mean muscle strength score (MRC) of 51.7 (11.0). There were 21 adverse events during the examiners' assessments (A1, B, A2), eight for A1 (4 hypotension and 4 hypertension events); 6 for A2 (1 hypotension, 2 hypertension, 1 pain, 1 dizziness, 1 respiratory distress); and 7 for B (2 hypertension, 2 pain, 3 respiratory distress). All adverse events improved after interruption of the assessment, with no worsening of cases or need for invasive interventions. Table 3 describes the data for muscle strength and mobility assessment scales. The description of the most frequent reason for admission and the characteristics of age, muscle strength, and mobility are provided in the Supplementary Material Online.
Sociodemographic and clinical characteristics of patients (n = 110).
A1, evaluator A first test; A2, evaluator A retest; B, evaluator B; DM, diabetes mellitus; SAH, systemic arterial hypertension.
All data are N(%) except for hospital admission day [median (interquartile range 25 %−75 %)] and age and Glasgow Coma Scale [mean (standard deviation)].
Values of the measurements of the muscle strength and mobility assessment scales in the study sample (n: 110).
A1, evaluator A first test; A2, evaluator A retest; B, evaluator B; FIM: functional independence measure, FSS, Functional Status Scale measure; MRC: medical research council.
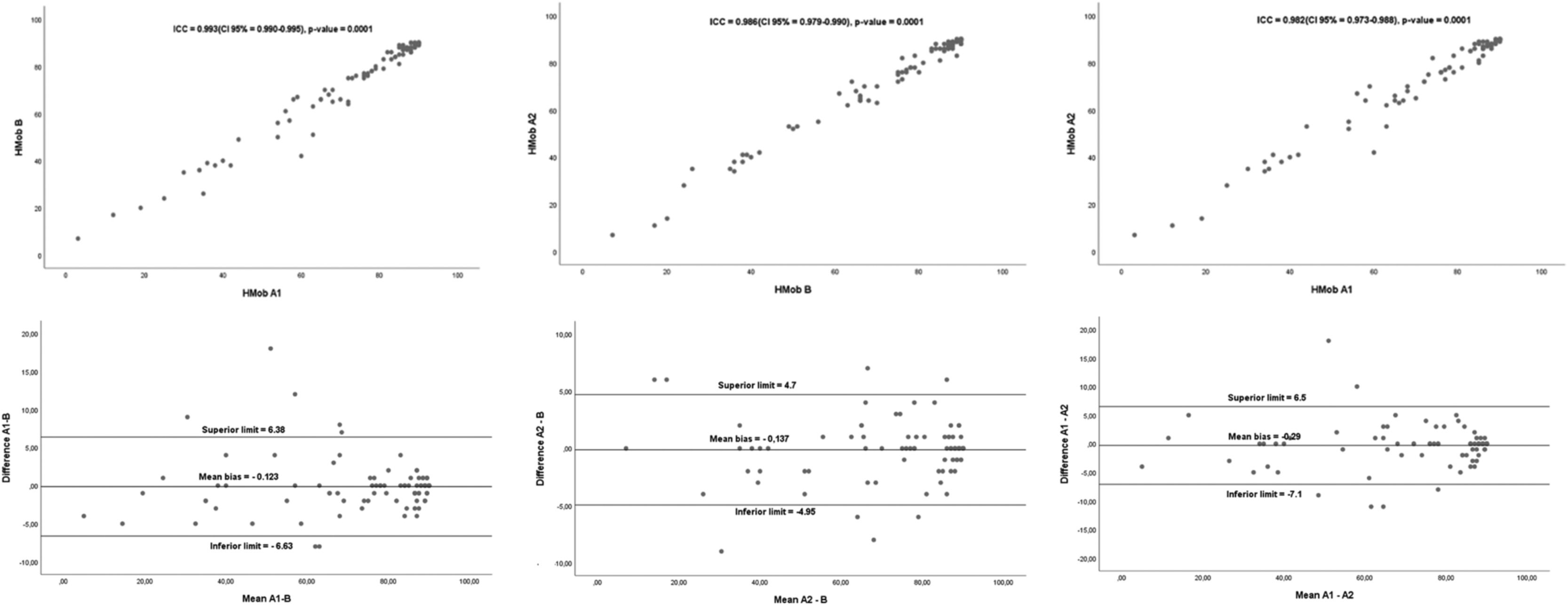
Internal consistency assessed by Cronbach's alpha coefficient was 0.949. Relative intra (A1-A2) and inter-examiner (A1-B; A2-B) reliability was excellent (A1-A2: ICC = 0.982, 95% CI = 0.973, 0.988, p-value , 0.0001; A1-B: ICC = 0.993, 95 % CI = 0.990, 0.995, p-value < 0.0001; A2-B: ICC = 0.986, 95%CI = 0.979, 0.990, p-value < 0.0001). For analysis of absolute reliability using the Bland-Altmann method, the following mean biases and limits of agreement between raters were observed (A1- A2: −0.29, upper limit: 6.5, lower limit: - 7.1, p-value: 0.703; A1-B: −0.123, upper limit: 6.38, lower limit: −6.63, p-value: 0.394; A2-B: −0.137, upper limit: 4.7, lower limit: −4.95, p-value: 0.575), which are described in Fig. 2. The criterion validity of HMob through Pearson's correlation analysis was 0.967 (p-value < 0.0001) when compared to the FSS and 0.926 (p-value < 0.0001) for the MIF. The ceiling effect was 20.9 % while the floor effect was 0 %.
DiscussionIn this study, a new scale was developed to assess mobility in hospitalized patients, to address relevant aspects of this important variable that must be measured during hospitalization. We identified high internal consistency, intra- and inter-rater reliability, and validity in relation to the FSS and MIF scales. The final version of the HMob consisted of 15 mobility-related tasks, which were divided into three blocks (mobility in bed, bedside, and space), with a score from 0 to 6 for each task.
The main advantages of HMob compared to other instruments were the assessment of laterality in the execution of tasks, in addition to including the main tasks related to basic mobility, from those in bed to those involving displacement in space. It is essential to monitor patients with laterality changes, such as patients with stroke, which was the most frequent population in the neurological ward. Based on this information, we can suggest placing the patient in a bed which makes their movement easier and safer. Another positive aspect of this study was having applied this scale in different clinical settings in the hospital environment, including patients with cardiovascular, neurological, clinical and critical problems, both in inpatient units and in adult intensive care units. Unlike the FSS scale, for example, its use is not restricted only in situations where the cause of the change in mobility was muscle weakness, but also in situations where the cause encompassed other problems such as sensorineural changes, motor control, and cardiorespiratory changes, for examples.11
With this new scale, the score for each task was also simplified in relation to other instruments such as the FSS, which has 8 scoring levels, whereas the HMob has 7 scoring levels. Although there are good levels of reliability for FSS and FIM21, there is some difficulty in levels 0, 1, and 2, which can be minimized by reducing it to 2 levels (0 and 1), still including the qualification of clinical restriction (CR) for situations where the evaluation was not possible due to this reason.11
From the point of view of its applicability, there was a 6.36 % occurrence of adverse events during the evaluation, all resolving after interruption of the evaluation, without serious complications. Although the use of the scale is safe, caution must be taken when applying it because it involves basic activities performed with a greater intensity in relation to day-to-day activities such as climbing stairs and squatting. The low floor effect found in this study suggests good use of the instrument in most patients. The ceiling effect of approximately 20.9 % was equivalent to other studies and can be explained by the fact that most of the evaluated patients were in the inpatient units and had a better level of mobility.22,23
One of the limitations of the study was the percentage of ceiling effect, which may suggest a low ability to identify improvements, but it has a low impact because the purpose of the instrument is to be used in the assessment of basic mobility. Another limitation was the adverse events found, but these resolved quickly after rest.
ConclusionThe HMob scale showed excellent internal consistency, intra- and inter-rater reliability, and convergent validity with the FSS scales and the FIM (motor domain), which suggests that it can be used in daily practice to measure mobility in hospitalized patients. New studies are needed to assess HMob responsiveness and prognostic ability with post-discharge outcomes.
The study received support from the Conselho Nacional de Desenvolvimento Científico e Tecnológico – Brasil(CNPq) and from the Fundo de Amparo à Pesquisa do Estado da Bahia(FAPESB). “Bolsista do CNPq – Brasil” and “Bolsista da FAPESB”