Aging is associated with an increased risk of accidental falls. Falls in older people have been widely studied in nursing homes and in the elderly with poor functionality, but there have been few investigations into functionally independent community-dwelling older adults.
ObjectiveTo determine the predictive factors for falls in functionally independent community-dwelling older adults.
MethodsA cohort trial-nested case–control study was carried out. The participants were community-dwelling people aged 70 and over who were treated in primary care centers from December 2012 to May 2014 in la Ribera (Valencia, Spain).
ResultsThere were a total of 374 participants, with a mean age of 76.1 (SD 3.4) years (63.8% females). The subjects presented high functionality scores: Barthel 96.5 (SD 9.4), Lawton 7.2 (SD1.2), Tinetti 25.6 (SD 3.3). The mean number of prescribed drugs was 4.7 (SD 2.9). The cumulative incidence of falls was 39.2%, and 24.1% of these older adults suffered falls. The number of falls in the previous 12 months (OR=1.3; 95%CI: 1.11–1.53; p<0.001) and alpha-blockers (OR=6.72; 95%CI: 1.62–27.79; p=0.009) were predictors of falls. The presence of previous fractures (OR=9.55; 95%CI: 4.1–22.25; p<0.001), a body mass index of ≥30kg/m2 (OR=1.09; 95%CI: 1.01–1.19; p=0.035), and who are using benzodiazepines and beta-blockers (OR=2.77; 95%CI: 1.53–5.02; p<0.001), were predictors of recurrent fallers.
ConclusionsOlder people who use alpha-blockers, benzodiazepines and beta-blockers, had previous fractures, with increased body mass index are more likely to fall.
The mean age of the world population is increasing. Indeed, 11.5% of the global population is over 60 years of age, and this percentage is expected to double by 2050. The evaluation of the health conditions of the older population is an important challenge for health professionals.1 Advancing age is not only associated with increased morbidity but also with gait alterations, cognitive and mood state disorders, pain caused by diminished functionality, and increased frailty and dependency.2–5
Aging is associated with an increased risk of accidental falls, and one-third of all autonomous people over 65 years of age can expect to suffer a fall in the course of a year.6 Dependent and frail older individuals have a greater prevalence of risk factors for falls than the rest of community-dwelling older people.7 Despite this, community-dwelling older adults are also at risk of suffering falls, and adequate assessment by the health professionals is needed in order to predict such risk.8
The American Geriatric Society and the Centers for Disease Control and Prevention (CDC) recommend screening of fall risk in older adults at least annually, though effective screening is still underutilized and not routinely integrated in clinical practice. Overreliance on unreliable subjective measures, the ceiling effect in some geriatric tests, the lack of cost-effective assessment technology, and clinical time constraints are several reasons for the lack of fall risk assessment in current practice.9,10
Recurrent falls have a high prevalence, affecting up to 25% of all older individuals, and they are associated to increased morbidity and mortality.11
In fact, falls constitute a considerable healthcare problem due to their medical, psychological, social-familiar and economic consequences.12 Despite this, falls are an underdiagnosed and undertreated geriatric syndrome, since little importance has been given to such accidents, their consequences, and their predictive risk factors within the clinical setting.13
Falls in older people have been widely studied in nursing homes and in the elderly with poor functionality, but there have been few investigations into functionally independent community-dwelling older adults.14,15
The present study was designed to investigate the factors associated with isolated or recurrent falls in community-dwelling older people with a good degree of functional independence, and to develop a predictive model that may be used as a screening instrument in the healthcare management of this specific population.
MethodsStudy design and participantsA prospective, longitudinal observational study was carried out in which a cohort trial-nested case–control design was used to develop predictive models for isolated falls (one or two falls in the course of one year of follow-up) and also recurrent falls (three or more falls in the course of one follow-up year) in non-institutionalized older people with functional independence. To be included in the study, subjects were required to be aged 70 and over, with a Barthel Index score of 60 points and above. Additionally, subjects were required to be independent for walking (with possible technical aids, but not assisted by another person) and reside in the region of la Ribera – a rural area with several cities and villages totaling about 250,000 inhabitants in Valencia, Spain.
Subjects were excluded from the study in cases of associated disease conditions resulting in a life expectancy of under 6 months, blindness and deafness, serious psychiatric problems diagnosed by a psychiatrist (schizophrenia, major depression, bipolar disorder, panic disorder) or moderate to severe cognitive impairment (diagnosed by the general practitioner or geriatrician). Individuals failing to sign the informed consent document for participation in the study were also excluded.
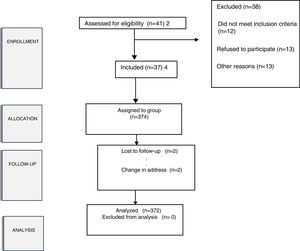
The minimum sample size was determined via the Schlesselman method for a 35% incidence of older adults with falls and a minimum estimated relative risk of 2, with a statistical power of 80% and an alpha probability of less than 95% error. The resulting minimum sample size was 270 subjects. To compensate for potential dropouts, an oversample of 20% was adopted, bringing the final minimum sample to 324 subjects for follow up.
A publicity strategy was designed to facilitate recruitment from December 2013 to May 2014, which consisted of posters and notifications in retired people centers, meetings with the managing authorities of retired people associations and centers, and telephone calls to people inscribed in different primary care centers. Family telephone calls were also used in an attempt to avoid future dropouts in cases where individuals lacked the physical means to attend health education sessions on fall risk-free environments on their own.
The study was approved by the Clinical Research Ethics Committee of Hospital Universitario de la Ribera (Valencia, Spain), and each participant signed an informed consent document before inclusion in the study or statistical processing of the data obtained.
Data collectionGeriatric assessment was carried out by a nurse in each primary care center, with collection on the baseline visit of sociodemographic variables, anthropometric data (body weight, height, and dominant grip strength measured with a dynamometer), functional variables (Barthel index, Lawton scale, Tinetti test), cognitive information (MEC-Lobo, a Spanish adaptation of the Mini-Mental State Examination (MMSE) – moderate to severe cognitive impairment being considered as MEC-Lobo <24 points), nutritional data (short Mini-Nutritional Assessment (sMNA)) scale, body mass index (BMI) (obesity being defined as BMI≥30kg/m2) and clinical parameters (comorbidities, 4 or more disease conditions). Information was also noted on the number of previous fractures, presence of ulcers, foot hygiene (correct nail cutting [short and without thickening] and correct skin hydration; if any of these were missing, foot care was considered inadequate), adequacy of footwear (adapted to foot morphology, closed, heel closed and correct heel height: no more than two centimeters; if any of these were missing, footwear was deemed inadequate), fear of falls (modified Falls Efficacy Scale, mFES), number of falls in the 12 months before inclusion in the study (a fall was considered as an unexpected event in which the person comes to rest on the ground, floor, or lower level),16 number of risk factors,17 extrinsic risks (related to the environment: lack of stair handrails, poor stair design, lack of bathroom grab bars, dim lighting or glare, obstacles and tripping hazards, slippery or uneven surfaces, improper use of assistive devices), and intrinsic risks (related to the individual: advanced age≥80 years, previous falls, muscle weakness, gait and balance problems, poor vision, postural hypotension, chronic conditions including osteoarthritis, diabetes, stroke, Parkinson's disease, incontinence, dementia, fear of falling). Visual impairment was assessed considering whether the individual could indicate that he or she had difficulty seeing (while wearing glasses if appropriate). Hearing impairment was assessed considering whether the individual could indicate that he or she had difficulty hearing. Physical activity was divided into three categories: <3h/week, 3–6h/week, >6h week.
Lastly, the use of drugs with actions upon the central nervous system (benzodiazepines, antidepressants, anticholinergic agents and medication for vertigo) was documented.
A monthly telephone call was made by the nurse who had carried out the geriatric assessment and was known to the elderly participant, in order to determine the number of falls over the last 30 days.
Data analysisThe study data were entered into MS Excel spreadsheets, followed by statistical analysis using the SPSS® version 19.0 statistical package (SPSS, IL, USA).
The variables were reported as proportions and/or means and standard deviations. Parametric tests (Student t-test and Fisher-Snedecor ANOVA test) were used for the comparison of means, while nonparametric tests (chi-squared test and linear trend test) were used for the comparison of proportions. The association between falls and the different risk factors, based on the odds ratio (OR) were then analyzed. A binary logistic regression model was developed to explore the importance of the risk factors, defined according to the falls observed during the 12-month follow-up period of the study. Firstly, the complete model, with all the variables in the bivariate analysis, was found to be significantly associated to the presence of falls during follow-up. In a second step, all those variables failing to produce a significant change (defined as the absence of an adjusted effect of >10%) were eliminated from the model, including those which did not result in an improved standard error when omitted. Consensus was sought among the investigators in those cases where two or more subsets of variables with the same degree of fit were obtained.
The following variables were entered into the model: age groups, sex, cohabitation, hearing problems, vision problems, inadequate foot hygiene, fear of falls, previous fractures, anxiety-depressive syndrome, use of alpha-blockers, use of benzodiazepines and beta-blockers, use of drugs with actions upon the central nervous system, multiple drug use, comorbidity, orthostatic hypotension, obesity, and physical activity.
Two binary logistic regression models, adjusted by age and gender, were generated. We used two predictive models in order to distinguish between the predictors of falls. In the first model, a binary variable (1 or 0) was used, as fallers were compared with non-fallers, whereas the variable in the second model compared recurrent fallers (3 or more falls) with non-fallers and isolated fallers (≤2 falls) over the 12-month follow-up period. Our study varied the definition of recurrent falling by varying the time unit between falls and by varying the number of falls per time unit. We collected the number of falls in the previous 12 months and the definition (at least two falls within 12 months) showed the lower association between the predictors for falls in a sample with high functionality. Previous studies by our research group,18 and other studies found in the literature,19 support a greater predictive value of fall risk profiles using the outcome variable “at least three falls (>2 falls) within 12 months”. This definition was therefore adapted for this study, with falls being stratified into three categories: non-fallers, isolated fallers (1 or 2 falls) and recurrent fallers (>2 falls).
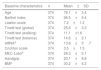
ResultsThe study population consisted of 374 participants between 70 and 85 years of age, with a mean age of 76.1 (SD 3.4) years, and with a predominance of females (63.8%). As seen in Table 1, most of the older adults were functionally independent. In addition to the functional variables, the table reports data relating to risk factors for falls. Of note in this respect are sensory defects (hearing and vision problems), previous falls and fractures, and multiple drug use 4.7 (SD 2.9) prescribed medications per patient (Table 2). Only two subjects abandoned in the course of the study, as a result of a change in address (Fig. 1). Both of these individuals had high functionality at the start of the study (baseline). They were women over 80 years of age who lived alone, and following hospital admission unrelated to falls, they went to live with their offspring in an area outside the study setting.
Characteristics of the population at the start of the study.
| Baseline characteristics | n | Mean±SD |
|---|---|---|
| Age | 374 | 76.1±3.4 |
| Barthel index | 374 | 96.5±9.4 |
| Lawton scale | 374 | 7.2±1.2 |
| Tinetti test (global) | 374 | 25.6±3.3 |
| Tinetti test (walking) | 374 | 11.1±1.6 |
| Tinetti test (balance) | 374 | 14.6±2.1 |
| sMNAa | 374 | 13.6±0.7 |
| Crichton scale | 374 | 3.5±1.5 |
| MEC-Lobob | 374 | 28.3±3.1 |
| Handgrip | 374 | 20.1±8.8 |
| BMIc | 374 | 30.2±4.3 |
| Sex | n | Percentage |
|---|---|---|
| Male | 137 | 36.2% |
| Female | 237 | 63.8% |
| Living conditions | n | Percentage |
|---|---|---|
| Lives alone | 103 | 27.5% |
| Lives with partner | 240 | 64.2% |
| Lives with offspring | 31 | 8.3% |
Risk factors for falls.
| Risk factors for falls | n | Mean |
|---|---|---|
| Number of risk factors | 368 | 3.1±1.9 |
| Number of falls in previous 12 months | 141 | 2±1.7 |
| Type of risk factors | n | Percentage |
|---|---|---|
| None | 6 | 1.6% |
| Intrinsic (related to the individual)a | 325 | 86.9% |
| Extrinsic (related to the environment)b | 10 | 2.7% |
| Both | 33 | 8.8% |
| Risk factors | n | Prevalence |
|---|---|---|
| Vision problems | 333 | 89% |
| Corrective lenses | 315 | 84.2% |
| Hearing problems | 139 | 37.2% |
| Hearing aids | 25 | 6.7% |
| Active ulcers | 15 | 4% |
| Inadequate footwear | 27 | 7.2% |
| Inadequate foot care | 24 | 6.4% |
| Previous fractures | 92 | 24.6% |
| Falls in the previous 12 months | 141 | 37.7% |
| Fall syndrome | 65 | 17.4% |
| Fear of falling (mFESc<70) | 121 | 32.4% |
| Anxiety-depressive syndrome | 86 | 22.9% |
| Alpha-blockers | 9 | 2.4% |
| Benzodiazepines | 142 | 38% |
| Beta-blockers | 72 | 19.3% |
| Drugs with actions upon the central nervous system | 174 | 40.1% |
| Comorbidity (≥4 diseases) | 94 | 25.1% |
| Orthostatic hypotension | 66 | 17.4% |
| Obesity (BMI≥30kg/m2)d | 190 | 50.8% |
| Physical activity | ||
| <3h/week | 161 | 43.0% |
| 3–6h/week | 113 | 30.2% |
| >6h week | 100 | 26.7% |
| Risk factors | n | Mean |
|---|---|---|
| Number of drugs | 372 | 4.7±2.9 |
The incidence of falls was 39.2% (95% CI: 34.1–44), and 24.1% of the subjects had suffered from falls (95% CI: 19.7–28.4). Table 3 shows the results of the analysis of the risk factors underlying isolated and recurrent falls. In the case of isolated falls, the female sex was predictive of a two-fold increase in the risk of new falls over the following 12 months among those individuals who had suffered falls the previous year.
Risk factors in older people with isolated and recurrent falls.
| Predictor variables | Isolated falls (1 or 2) | Recurrent falls (≥3) | ||||
|---|---|---|---|---|---|---|
| OR | 95%CI | p-Value | OR | 95%CI | p-Value | |
| Sex | ||||||
| Female | 1.94 | 1.01–3.70 | 0.045 | 4.02 | 1.64–9.87 | 0.02 |
| Living conditions | ||||||
| Lives alone | 2.38 | 0.91–6.22 | 0.077 | 6.55 | 1.57–27.21 | 0.01 |
| Lives with partner | 1.09 | 0.54–2.19 | 0.795 | 3.73 | 1.37–10.14 | 0.01 |
| Lives with offspring | 2.67 | 0.30–23.42 | 0.376 | 2.11 | 0.29–9.22 | 0.69 |
| Risk factors | ||||||
| Previous fractures | 2.67 | 0.54–13.19 | 0.229 | 8 | 1.47–43.4 | 0.02 |
| Hypotension | 2.2 | 0.96–5.02 | 0.061 | 6.11 | 1.33–28.03 | 0.02 |
| Fear of falls | 2.09 | 0.85–5.17 | 0.109 | 4.72 | 1.39–9.36 | 0.01 |
| Hearing problems | 1.49 | 0.87–2.54 | 0.142 | 4.34 | 1.36–13.9 | 0.01 |
| Previous falls | 1.49 | 0.85–2.63 | 0.163 | 3.39 | 1.59–7.22 | 0.01 |
| Vision problems | 1.52 | 0.77–2.98 | 0.225 | 3.31 | 1.51–7.27 | 0.01 |
| Multiple drug use | 1.12 | 0.55–2.29 | 0.756 | 3.31 | 1.42–7.70 | 0.01 |
| Hypertension | 1.33 | 0.54–3.29 | 0.538 | 2.88 | 1.17–7.08 | 0.02 |
| Comorbidity | 2.11 | 0.75–5.89 | 0.154 | 3.81 | 1.28–11.26 | 0.02 |
| BMI>25kg/m2a | 2.01 | 0.94–4.28 | 0.07 | 3.77 | 1.44–9.88 | 0.01 |
| Sedentary lifestyleb | 4.84 | 0.62–37.6 | 0.131 | 0.85 | 0.22–3.35 | 0.82 |
| Anxiety-depressive syndrome | 3.1 | 0.92–10.41 | 0.067 | 0.8 | 0.26–2.55 | 0.72 |
The risk factors significantly associated to multiple falls in older adults were the female sex, living alone or with a partner, previous fractures, hypotension, fear of falls and hearing problems (Table 3).
Predictive modelsOur first predictive model of isolated falls in older adults showed a sensitivity of 10%, a specificity of 98.2%, a positive predictive value of 75.2% and a negative predictive value of 77.5%. The model explained 47% (Nagelkerke R2) of the variance of isolated falls and correctly classified 77% of the cases. The model allowed us to predict that older adults who have suffered a fall in the last year and who are using alpha-blockers have a 24% probability of suffering another fall. The number of falls in the previous 12 months (OR=1.3; 95%CI: 1.11–1.53; p<0.001) and alpha-blockers (OR=6.72; 95%CI: 1.62–27.79; p=0.009) were predictors of falls (Table 4).
Predictive models: falls and recurrent falls.
| OR | 95%CI | p-Value | |
|---|---|---|---|
| Model 1: Falls (yes versus no) | |||
| Number of falls in previous 12 months | 1.3 | 1.11–1.53 | 0.01 |
| Alpha-blockers | 6.72 | 1.62–27.79 | 0.01 |
| Constant | |||
| Model 2: Recurrent falls (≥3) | |||
| Body mass index (BMI≥30kg/m2) | 1.09 | 1.01–1.19 | 0.03 |
| Benzodiazepines and beta-blockers | 2.77 | 1.53–5.02 | 0.01 |
| Previous fractures | 9.55 | 4.1–22.25 | 0.01 |
| Constant | 0.01 | ||
The second predictive model, corresponding to recurrent falls in older adults, showed a sensitivity of 15.2%, a specificity of 98.8%, a positive predictive value of 58.8% and a negative predictive value of 92.3%. The model explained 39.4% (Nagelkerke R2) of the variance of recurrent falls and correctly classified 91.4% of the cases. The model allowed us to predict that older adults with recurrent falls, in the presence of previous fractures (OR=9.55; 95%CI: 4.1–22.25; p<0.001), a body mass index of ≥30kg/m2 (OR=1.09; 95%CI: 1.01–1.19; p=0.035), and who are using benzodiazepines and beta-blockers (OR=2.77; 95%CI: 1.53–5.02; p<0.001), have a 99.98% probability of suffering further falls (Table 4).
DiscussionThis study has analyzed the factors predictive of falls in functionally independent, community-dwelling older people. We found that in these adults, a distinction can be made between recurrent and isolated falls, where the use of alpha-blockers is the main predictor, with a high predictive value. In contrast, gait alterations and the rest of the drug groups were not identified as risk factors. A history of previous fractures, a BMI≥30kg/m2 and the use of benzodiazepines and beta-blockers were identified as predictors of falls in recurrent elderly fallers. The risk factors predicting accidental falls in functionally independent community-dwelling older adults recorded in our study differ from those identified in older adults with different levels of dependency20 or who are institutionalized.21 In such cases, the predictors of falls are fragility, the male sex, gait alterations and sarcopenia.22
The predictive models developed in our study offer greater reliability in predicting recurrent falls in older adults, but are less reliable in predicting isolated falls or the absence of falls. The variables initially included in the models were similar to those included in previous models in community-dwelling older populations,11 though the predictive variables finally identified by the models were different. The use of alpha-blockers was found to be a predictor of falls, in contrast to the literature, where a review23 reported that it is not clear whether the use of antihypertensive medications is associated to a risk of falls in older people. This discrepancy could be due to a possibly greater use of alpha-blockers in our sample than in other studies.24 In agreement with most studies, the existence of previous falls in older adults increases the risk of further falls, and this is also reflected by the enhanced risk perception among patients who have already experienced a fall in the past.25
The model with the greatest predictive capacity was the model of recurrent falls in older adults, allowing for greater precision in predicting falls than in other studies,11 with superior specificity and a higher effective total percentage. Furthermore, the model offered greater simplicity thanks to the inclusion of fewer variables, and also greater predictive capacity.
The existence of previous fractures was found to be a robust risk factor, in agreement with most studies found in the literature.26 Furthermore, in contrast to the remaining studies which considered denutrition to be a risk factor,27 a high BMI was seen to be predictive of recurrent falls. This could be related to the functionality of the sample, given that the subjects were able to cook or shop for themselves and hence maintained a self-controlled diet following their tastes and appetite, in contrast to dependent older adults.
Isolated drug use was not correlated to a risk of falls, though the combined use of benzodiazepines and beta-blockers showed a significant association to the risk of falls, in agreement with the observations of other authors.28 Moreover, the use of benzodiazepines and beta-blockers was higher than in other samples.29 This could be due to the presence of high BMI values, which might be associated to the use of antihypertensive drugs and polymedication practices.30 All these factors are modifiable, and preventive measures can therefore be adopted to reduce the risk of falls and their consequences.31
The different functional characteristics of older populations described in the literature could explain the different variables included in the predictive models published to date. In contrast to the model developed by Stalehoef et al.,32 depressive symptoms and postural and balance disorders were not identified as predictors in our study, perhaps due to the ceiling effect and relatively unchallenging conditions which many gait and balance tools may present. The model developed by Kabeshova et al.11 included similar variables, though these were fewer in number. The fear of falls, multiple drug use and depression were found to be predictive of falls in older adults with recurrent falls.
As predictors of falls in functionally independent, community-dwelling older adults differ from the risk factors in older adults with different levels of dependency or who are institutionalized, it is necessary to improve research on falls in independent older adults in order to identify the best preventive strategies for nurses, physical therapists, general practitioners, pharmacists and other care providers.33
LimitationsOur study has a number of limitations. Firstly, the data relating to drugs associated with falls in older adults corresponded to those pharmacotherapeutic groups most commonly associated to falls, and which had been prescribed by the physician (not taken sporadically and/or upon personal decision by the patient). Secondly, the doses of the drugs with effects upon the central nervous system were not documented. Thirdly, the time, weather conditions and place of the fall were not recorded, and the follow-up period was limited to 12 months. Furthermore, monthly reporting of falls by the older adults was affected by bias resulting from a possible lack of information. Finally, adherence to drug treatment was not taken into account, and there may have been bias in the information collected from the case histories and from the patients. These circumstances may produce measurement bias in the variables that influence the risk of falls.
ConclusionsThe incidence of falls is high in functionally independent, community-dwelling older adults. The predictors of falls differ from the risk factors in older adults with different levels of dependency or who are institutionalized. Comprehensive geriatric assessment needs to be undertaken in functionally independent, community-dwelling older adults in order to detect risk factors for falls, such as the use of medications, obesity and previous fractures and falls. These factors can be prevented and modified in order to avoid falls and consequently dependence and disability.
ContributorsEach of the authors significantly contributed to the study design, data collection, analysis and discussion of the results and to drafting of the manuscript.
FundingThis study received no funding.
Conflicts of interestNone of the authors declare any conflict of interest with the study.
The authors wish to thank all the members of the Departamento de Salud de la Ribera for helping to make this study possible.