Thoracic hyperkyphosis is related to different health conditions, requiring precise evaluation in clinical settings. Several instruments have been proposed for assessing thoracic kyphosis, and previous studies have investigated their reliability and validity.
AimsSystematically review studies evaluating the validity and reliability of instruments designed to measure thoracic kyphosis and classify their clinical utility.
MethodsMEDLINE and EMBASE (via Ovid) databases were used to search studies published until December 2023, and additional searches were conducted in Google Scholar and by hand search. Studies that analyzed the reliability and validity of noninvasive instruments for measuring thoracic kyphosis, regardless of population, study design, and language, were included. Two independent reviewers analyzed the titles, abstracts, and full text and assessed the methodological quality. Clinical utility was assessed using a 10-point scale.
ResultsSeventy-two studies were included, and 15 instruments had their measurement properties explored: seven were grouped in a meta-analysis for validity, seven for intra-rater reliability, and six for inter-rater reliability. Despite the heterogeneity of estimated data, they presented a strong to moderate correlation with the gold standard and excellent intra- and inter-rater reliability. The instruments most frequently studied were the Flexicurve Angle and the Analog Inclinometer.
ConclusionThe meta-analysis demonstrated that the Analog Inclinometer, Flexicurve Angle and Index, Photogrammetry, Smartphone applications, and Spinal Mouse were valid and reliable for assessing thoracic kyphosis. Also, the utility analysis suggested that the Analog Inclinometer, Flexicurve Angle, and Smartphone applications are recommended for clinical settings.
In clinical practice, physical therapists usually assess thoracic kyphosis using visual inspection.1 This method may not accurately quantify changes associated with different health conditions, aging, and treatments. Previous studies demonstrated that thoracic hyperkyphosis is associated with the presence of neck and low back pain,2–4 reduced lung function,5 impaired performance during gait,6 and increased risk of falls and mortality.7–8 Furthermore, evidence suggests that corrective exercises for thoracic hyperkyphosis can improve posture and balance in patients with kyphosis angles greater than 40°.9–10 Therefore, assessing thoracic kyphosis in clinical settings is essential for understanding, monitoring, and planning treatment for patients with several health conditions.
The Modified Cobb angle is the gold standard for measuring thoracic kyphosis using radiography (X-ray) due to its proven accuracy in assessing spinal curvature, its ability to provide detailed images of bone structures, and its widespread use in clinical practice as a reliable tool for diagnosis.11 However, this assessment has limitations, including the time required for X-ray acquisition and interpretation, high costs, limited equipment portability, and radiation exposure, which is particularly concerning for repeated assessments in pediatric populations and young individuals.12 Previous studies observed that the normal range of thoracic kyphosis varies between 20° and 40° in adolescents and younger adults.11,13 Although the definition of pathological hyperkyphosis is not a consensus, an angle greater than 50° has been adopted for this diagnosis.14 On the other hand, kyphosis angles < 20° characterize hypokyphosis.15
Using portable, easy-to-use, low-cost instruments may be beneficial for assessing thoracic kyphosis in clinical settings as it allows a quick, comfortable, and accurate measurement. However, instruments should not be used without evidence about their measurement properties.16 Previous studies investigated the validity and reliability of several instruments developed to assess thoracic kyphosis.12,17–39 Given the variety of instruments, clinicians must use instruments that ensure the proper assessment of thoracic kyphosis in clinical settings. This assessment enables monitoring to prevent or minimize negative consequences and evaluate treatment effectiveness related to thoracic hyper and hypokyphosis.
In 2014, a systematic review included 28 studies published up to October 2012 about the validity and reliability of non-radiographic methods for assessing thoracic kyphosis.40 Findings showed that the validity of methods varied from low to very high, with reliability levels ranging from high to very high; however, no meta-analysis was performed. Despite the substantial number of studies included in this review, several additional studies investigated the measurement properties of instruments that assess thoracic kyphosis from October 2012 to the present day.
Therefore, this systematic review performed a meta-analysis of studies that assessed the validity and intra- and inter-rater reliability of clinical instruments proposed to quantify thoracic kyphosis in any population and classified the instruments according to their clinical utility.
MethodsProtocolThis systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines41 and is registered in PROSPERO (CRD42019124956).
Search strategyThe search was initially conducted in March 2019 and updated in December 2023 in MEDLINE, EMBASE (via Ovid), and Google Scholar databases. In addition, the reference lists of previous reviews and included studies were also hand-searched. The search terms were related to thoracic kyphosis, thoracic posture, measurement properties (validity and reliability), and clinical instruments. The search strategy is detailed in Supplementary material 1.
Eligibility criteriaThe ideal instrument should be portable, precise, accurate, and affordable, thus allowing quick and safe assessment of thoracic kyphosis in clinical settings.42 Studies that assessed the validity or intra- or inter-rater reliability of clinical instruments proposed for measuring thoracic kyphosis were included. No language, publication date, sample characteristics, or study design restrictions were applied. Moreover, for the validity studies, instruments should be compared to an X-ray examination (gold standard) to be included. Studies that did not analyze the orthostatic posture of the thoracic region in the sagittal plane were excluded.
Study selection and data extractionTwo independent reviewers (APFAN and ACC) analyzed titles and abstracts; ineligible studies were excluded. Then, two reviewers (APFAN and ACC) performed the full-text analysis. A third reviewer (RAR) resolved any disagreements in these steps. Data extraction was performed by one reviewer (APFAN). Descriptive information included sample characteristics (e.g., number of participants, sex, age, health condition, height, and body mass) and the instrument used to assess thoracic kyphosis. When applicable, the values of concurrent validity (Pearson correlation – r), intra- and inter-rater reliability (intraclass correlation coefficient - ICC), standard error of measurement (SEM), minimum detectable change (MDC), and Bland-Altman agreement analysis [(Mean Difference (MD) ± Standard Deviation (SD) and limits of agreement (LA)] were extracted. When two references for intra-rater reliabilities were reported, the ICC value of the most experienced rater or the higher value was chosen.
In addition, when studies measured the erect and relaxed thoracic kyphosis, only the value of the relaxed posture was considered, as it was adopted in most studies. Data were analyzed independently in the meta-analysis when the same study evaluated two or more instruments and different populations. Authors of validity studies that did not present the Pearson correlation and reliability studies that did not present the ICC value and 95 % confidence interval (95 % CI) were contacted by email to request data.
Methodological quality assessmentTwo independent reviewers (APFAN and ACC) evaluated the methodological quality of the studies using the critical appraisal tool (CAT) checklist by Brink and Louw.43 A third reviewer (RAR) resolved disagreements regarding the scoring of the studies. The CAT was structured to critically evaluate the measurement properties of instruments used in clinical settings and encompasses 13 items related to characteristics of population and evaluators, risk of bias, and methodological quality of the studies. Following the procedures adopted in previous systematic reviews, studies scoring above 60 % were considered to have high methodological quality.40,44–45 In this assessment, Kappa showed an overall agreement of 0.89 between the two independent reviewers (APFAN and ACC).
Data analysisConcurrent validity and intra- and inter-rater reliabilities of individual studies were grouped using a random effects model and analyzed using Comprehensive Meta-analysis software (version 4.0). I² statistic was used to evaluate heterogeneity between studies.46 Findings of individual studies and combined estimates were presented in a forest plot with a 95 % CI.
The concurrent validity was classified as very low (r < 0.25), low to reasonable (0.25 ≤ r < 0.50), moderate to good (0.50 ≤ r < 0.75), and strong (r ≥ 0.75).16 In addition, we also reported Bland Altman's limits of agreement.16 The intra- and inter-rater reliabilities were classified as low (ICC < 0.40), good to moderate (0.40 ≤ ICC < 0.74), and excellent (ICC ≥ 0.75).47
To be recommended for clinical use, an instrument must meet rigorous criteria, including validity (r > 0.80), reliability (ICC > 0.80), sensitivity (MDC), and a score of 9 or higher on a 10-point clinical utility scale. This scale evaluates factors such as portability, cost, evaluation time, measurement analysis, and interpretation. Specifically, cost is scored as follows: 〈 £100 scores 3, £100 - £500 scores 2, £500 - £1000 scores 1, and 〉 £1000 or unknown scores 0. Evaluation time is evaluated based on duration: <10 min scores 3, 10–30 min scores 2, 30–60 min scores 1, and >1 h scores 0. The necessity of specialized equipment or professional training is also considered, with “No” scoring 2, “Yes, but only simple, easy to use equipment, which does not need specialist training” scoring 1, and “Yes” or “Unknown” scoring 0. Finally, portability is evaluated as follows: “Yes, easily (e.g., can fit in a pocket)” scores 2, “Yes, but requires a briefcase or trolley” scores 1, and “No or very difficult” scores 0.48–49
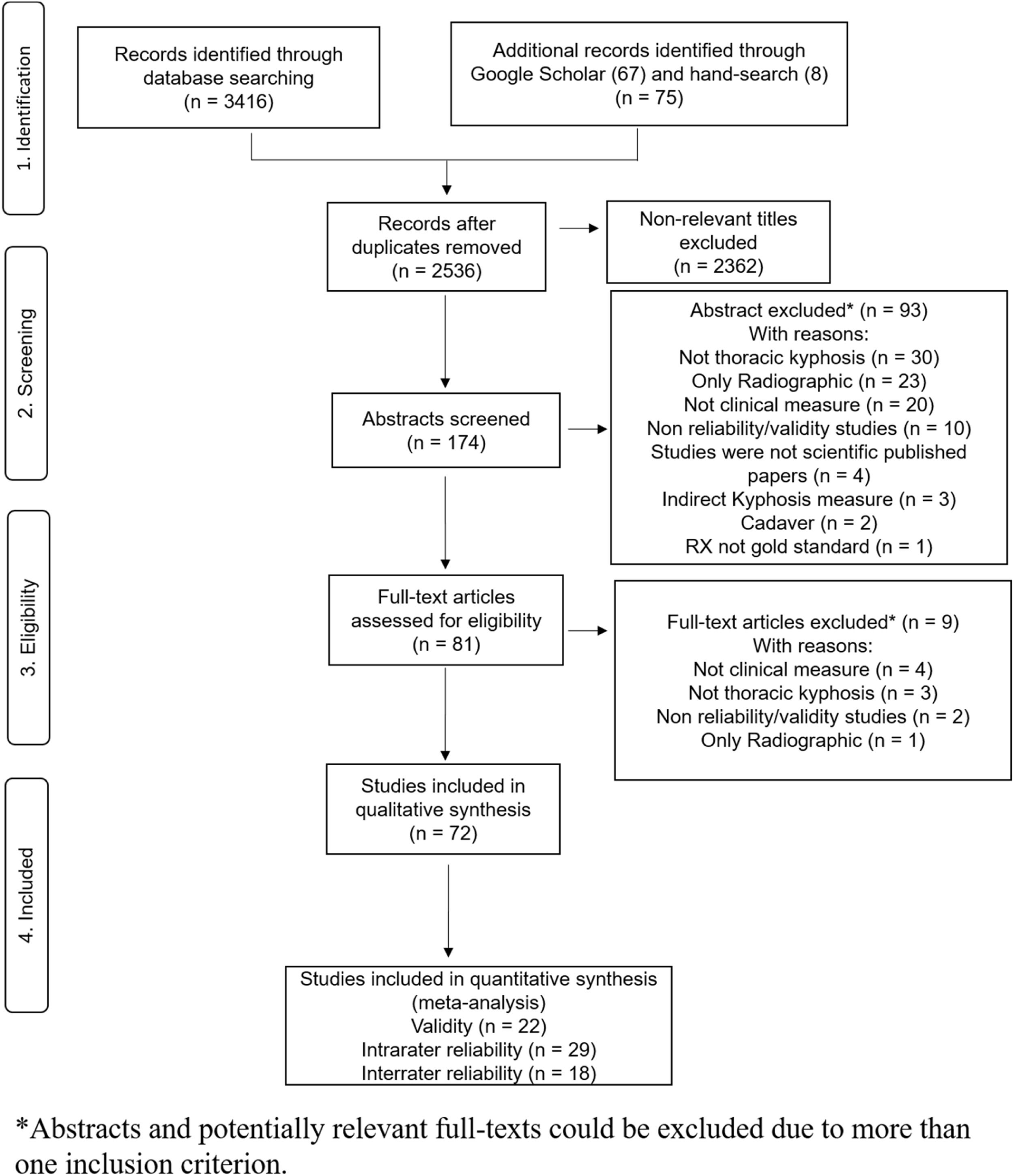
ResultsFlow of studiesThe search strategy identified 2536 titles after excluding duplicates. After screening titles and abstracts, 81 studies were included for full-text review. Four studies were excluded because they did not use clinical instruments, three for not measuring thoracic kyphosis, one because they were not validity or reliability studies, and one because thoracic kyphosis was measured only on the X-ray films. The studies excluded by full-text are listed in a table in the Supplementary material 2. Therefore, 72 studies were included. The review flowchart is presented in Fig. 1.
Characteristics of the included studiesThe characteristics of the studies are described in Tables 1 and 2. Fifteen instruments were identified: Analog Inclinometer, Archometer, Baseline® Body Level/ Scoliosis meter, Debrunner Kyphometer, Electrogoniometer, Digital Inclinometer, Dual Digital Inclinometer, Flexicurve (Angle and Index), Kypholordometer, Microsoft Kinect Sensor, Photogrammetry, Smartphone app, Spinal Mouse, Spinal Pantograph, and Spinal Wheel. Among the included studies, 31 verified the concurrent validity by comparing the instrument with an X-ray in the sagittal plane,12,17,19–20,23–24,29,31,33–34,50–70 57 evaluated the intra-rater reliability,12,17–18,20–28,30–32,35–39,42,50–52,54–57,63–65,67–69,71–94 and 40 the inter-rater reliability.12,17,20–24,27–28,30,32–33,35,51,54–57,64–65,68–74,78–80,82–83,87–91,93,95–96
Characteristics of the included validity studies.
| Authors and year of the study | Instrument | Study Population | Validity levels |
|---|---|---|---|
| Azadinia et al. 202150 | Photogrammetry(Digimizer Image Analysis Software version 5.3.4 -MedCalc Software; BVBA, Ostend, Belgium) | n = 50Mean age ± SD = 13.72 ± 1.85 years;BMI (kg/m²)19.37 ± 2.87Sex (M/F) 26/24Adolescents with hyperkyphosis | r = 0.94BA = 3.91° (MD); SD = NRLA = 10.2° to - 2.4° |
| Azadinia et al. 201451 | Dual Digital inclinometer (DDI)Flexicurve Angle (FA) | n = 81Mean age ± SD = 14.69 ± 4.11 years(range 10 - 30 years);height (cm) 157 ± 13.5; mass (kg) 50.7 ± 15.3BMIC (kg/m²) 20Sex (M/F) 26/55Patients with Hyperkyphosisn = 21Mean age ± SD = 65.76 ± 4.6 years (range 50 - 80 years); height (cm) 156.8 ± 5.7; mass(kg) 66.48 ± 8.93BMIC (kg/m²) 26Sex (M/F) 3/18Patients with Hyperkyphosis | r = NRICCDDIRX = 0.89BADDI = 4.85°(SD)MD = NR; LA = NRICCFARX = 0.51BAFA = 9.30° (SD)MD = NR; LA = NRr = NRICCDDIRX = 0.81BADDI = 4.93°(SD)MD = NR; LA = NRICCFARX = 0.50BAFA = 8.03° (SD)MD = NR; LA = NR |
| Barauna et al. 200552 | Kypholordometer | n = 30Mean age ± SD = 39 ± 15.8 yearsBMI = NRSex (M/F) NRScheuermann's Disease(n = 3)Postural kyphosis(n = 25)Ankylosing Spondylitis(n = 2) | r = 0.78BA = NR |
| Barrett et al. 201753 | AnalogInclinometer (AI)Flexicurve Angle (FA) | n = 11Mean age ± SD = 40.9 ± 20.1 yearsBMI (kg/m²) 24.4 ± 5.4Sex (M/F) 7/4Patients with pain(n = 6 low back pain;n = 4 with thoracic pain; n = 1 withinter-scapular pain) | rAIRX = 0.86BAAI = 4.8° ± 8.9°(MD ± SD)LA = 22.28° to −12.64°rFARX = 0.96BAFA = 20.2° ± 6.1°(MD ± SD);LA = 32.27° to 8.29° |
| Büyükturan et al.201854 | Spinal Mouse | n = 46Mean age ± SD = 68.12 ± 2.67 yearsBMI (kg/m2) 29.45 ± 4.67Sex (M/F) 17/29Healthy older individuals | r = 0.93BA = NR |
| Chaise et al. 201124 | Arcometer | n = 52Mean age ± SD = 53.7 ± 14.9 yearsBMI (kg/m2) 26.1 ± 4.4Sex (M/F) NRPersons with prescription for an X-ray | r = 0.94BA = −1.4° ± 6.06°(MD ± SD);LA = 10.53° to −13.24° |
| de Oliveira et al. 201,255 | Flexicurve Angle | n = 47Mean age ± SD = 44.9 ± 19.4 yearsBMI (kg/m2) 27.5 ± 5Sex (M/F) Both sexPersons with prescription for an X-ray | r = 0.70BA = 0.8° ± 8.0°(MD ± SD);LA = 17.0° to −15.3° |
| D'Osualdo et al.199756 | Arcometer | n = 32Mean age 15.5 yearsBMI = NRSex (M/F) 9/23Patients with kyphosis and scoliosis, and for postural rehabilitation | r = 0.98BA = NR |
| Faramarzi et al. 202057 | Smartphone app(Goniometer-Pro app) | n = 31Mean age ± SD = 25.09 ± 4.02 years;BMI (kg/m²) 22.07 ± 1.44Sex (M/F) NRPersons with prescription for an X-ray | r = 0.81BA = 1.79° ± 5.40°(MD ± SD)LA = NR |
| Fortin et al. 201034 | Photogrammetry(Fringes Acquisitionand Processing Software - InSpeck Inc., Montreal, Canada) | n = 70 (validity n = 40)Mean age ± SD = 15.7 ± 2.5 yearsBM (kg) 51.9 ± 9.3Height (cm) 161 ± 9.5BMIC (kg/m²) 20Sex (M/F) 10/60Children withScoliosis | r = - 0.77BA = NR |
| Giglio and Volpon, 200758 | Spinal Pantograph | n = 718 (validity = 20)Mean age 11.45 yearsBMI = NRSex (M/F) 350/368Normal subjects | r = 0.70BA = NR |
| Gravina et al. 201259 | AnalogInclinometer | n = 128Mean age 12.7 yearsBMI = NRSex (M/F) Both sexChildren/adolescents idiopathic scoliosis.Scheuermann or postural kyphosis | r = 0.89BA = - 0.3° (MD)SD = NRLA = 17.0° to −16° |
| Greendale et al. 201112 | Debrunner Kyphometer (DB)Flexicurve angle (FA)Flexicurve index (FI) | n = 113Mean age ± SD = 75.3 ± 7.5 yearsBMI (kg/m2) 26.5 ± 4.5Sex (M/F) 80.5 % were womenPersons withKyphosis>40° | rDBRX = 0.62BADK = 10.96° (SD); MD = NR; LA = NRrFARX = 0.68BAFA = 10.24° (SD); MD = NR; LA = NRrFIRX = 0.68BAFI = 11.26° (SD); MD = NR; LA = NR |
| Grindle et al. 202060 | Flexicurve angle (FA) | n = 40Mean age 55.9 ± 24.71 years.BMI (kg/m²) 24.7 ± 3.3Sex (M/F) 18/22Adult volunteers withhyperkyphosis | r = NRICC = 0.55(0.29 – 0.73)BA = NR |
| Hannink et al. 202261 | Dual Digital inclinometer (DDI)Flexicurve index (FI)Microsoft Kinect Sensor index (MKS) | n = 29Mean age 56.9 ± 18.2 yearsBMI (kg/m²) 24.7 ± 4.3Sex (M/F) 6/23Persons with spinal conditions | rDDIRX = 0.67BADDI = 3.51° (MD); SD = NR; LA = NRrFIRX = 0.54BAFI = 0.079°(MD); SD = NR; LA = NRrMKSRX = 0.70BAMKS = 0.004° (MD); SD = NR; LA = NR |
| Hunter et al. 201862 | Analog Inclinometer | n = 78- 39 with shoulder impingement syndromeMean age ± SD 57.1 ± 11.1 years;BMI (kg/m²) 29.3 ± 5.32Sex (M/F) 20/19- 39 no shoulder painMean age ± SD 55.7 ± 10.6 years;BMI (kg/m²) 25.7 ± 3.53Sex (M/F) 19/20 | r = 0.62BA = 2.45° ± 8.38°(MD ± SD);LA = 18.87° to −13.97° |
| Kado et al. 200619 | Debrunner Kyphometer | n = 120Mean age ± SD 68.6 ± 5.9 yearsBMI = NRSex (M/F) 0/120Women with low bonemineral density(0.68 g/cm2) | r = NRBA = NRICC = 0.68 |
| Korovessis et al. 200,120 | Debrunner Kyphometer | n = 90Mean age ± SD 15 ± 2.6 yearsBMI = NRSex (M/F) 44/46Adolescents with round back or poor sagittal back appearance | r = 0.75BA = NR |
| Perriman et al. 201031 | Electrogoniometer | n = 12Mean age 68.1 (50 - 80) years. BM (kg) 75.8 (62 - 94)Height (cm) 171.2 (160–190); BMIC (kg/m²) 25Sex (M/F) 6/6Healthy older individuals | r = 0,87BA = NR |
| Prowse et al. 201833 | Baseline® Body Level/Scoliosis meter | n = 31Mean age ± SD 13.6 ± 0.6 yearsBMI = NRSex (M/F) 4/27Adolescent with scoliosis | r = - 0.32BA = NR |
| Sangtarash et al.201463 | Dual Digital Inclinometer | n = 20Mean age ± SD 57.20 ± 7.67 yearsBMI (kg/m²) 27.75 ± 4.47Sex (M/F) 0/20Women with back pain | r = NRICC = 0.86BA = −1.55° ± 6.88° (MD ± SD)LA = 12.26° to −15.21° |
| Sedrez et al. 201423 | Arcometer | n = 40Mean age ± SD 10.7 ± 2.7 yearsBM (kg) 38.7 ± 13.1Height(m) 1.39 ± 0.17BMIC (kg/m²) 20Sex (M/F) 25/15Children (status not reported) | r = 0.40BA = NR |
| Schmidt et al. 202264 | Analog Inclinometer | n = 16Group 1 Risser 1 or 2Mean age ± SD 12.3 ± 1.0 yearsBMI (kg/m²) 20.3 ± 3.3Sex (M/F) NRAdolescent with idiopathicscoliosisn = 23Group 2 Risser 3 or 4Mean age ± SD 15.0 ± 1.7 yearsBMI (kg/m²) 24.1 ± 4.9Sex (M/F) NRAdolescent with idiopathicscoliosis | r group1 = 0.84BA = NRr group2 = 0.75BA = NR |
| Sharifnezhad et al. 202165 | Photogrammetry(Kinovea software) | n = 18Mean age ± SD 42.64 ± 21.67 yearsBMI (kg/m²) 23.48 ± 3.62Sex (M/F) 8/10Persons with prescription for an X-ray | r = 0.48BA = NR |
| Spencer et al. 201966 | Flexicurve Angle | n = 117Mean age ± SD 61.4 ± 7.0 yearsBMI (kg/m²) 29.0 ± 5.5Sex (M/F) 0/117Postmenopausal women with upper back pain | r = 0.64BA = −2.48° (MD) SD = NRLA = 14.92° to −19.88° |
| Tabard-Fougere et al. 201967 | Analog Inclinometer | n = 51Mean age ± SD 13.5 ± 2.0 yearsBMI (kg m²) 18.9 ± 2.8Sex (M/F) 19/32Adolescent with idiopathicscoliosis | r = 0.73BA = NR |
| Teixeira et al. 200768 | Flexicurve Angle | n = 56Mean age ± SD 66.7 ± 9.37 yearsBMI = NRSex (M/F) 21 /35Healthy older individuals | r = NRBA = NRICC = 0.90 |
| Todd et al. 201569 | Debrunner Kyphometer | n = 92Mean age ± SD 17.7 ± 1.39 yearsBMI (kg/m²) 22.9 ± 3.27Young athletic elite alpine skiers (n = 75)Sex (M/F) 30/35Non-athletic population (n = 27)Sex (M/F) 9/18 | r = 0.60BA = 4.5° (MD); SD = NRLA = 7.7° to −16.8° |
| Tran et al. 201670 | Debrunner Kyphometer (DK)Flexicurve Index (FI) | n = 72 (FI);n = 71 (DK)Mean age ± SD 77.8 ± 7.1 yearsBMI (kg/m²) 25.3 ± 4.6Sex (M/F) 20/52Persons recruited from Community with thoracic kyphosis | rDBRX = 0.65BA = NRrFIRX = 0.68BA = NR |
| Willner Stig, 198117 | Spinal Pantograph | n = 71 (n = 15 cases with a structural scoliosis of <30°;n = 41 cases without any visible spinal disorder on X-ray who served as "controls"; n = 15 cases with Scheuermann's disease)Mean age ± SD = NRBMI = NRSex (M/F) = NRTeenagers with or without visible spinal disorder | r = 0.97BA = NR |
| Yousefi et al. 201229 | Flexicurve Angle (FA)Spinal Mouse (SM)Photogrammetry (pH) | n = 20Mean age ± SD 26 ± 2 yearsBM (kg) 72 ± 2.5Height (cm)169 ± 5.5BMIC (kg/m²) 25Sex (M/F) 20/0Student volunteers | rFARX = 0.87BA = NRrSMRX = 0.76BA = NRrPHRX = 0.89BA = NR |
Note. NR, Not reported; BMI, Body Mass Index; BMIC, Body Mass Index calculated; SD, Standard deviation; BA, Bland-Altman analysis; BAAI, BA Analog Inclinometer; BADDI, BA Dual Digital Inclinometer; BAFA, BA Flexicurve Angle; BAFI, BA Flexicurve Index; BADB, Debrunner Kyphometer; LM, Limits of agreement; MD, Mean difference; ICC, Intraclass Correlation Coefficient; ICCDDIRX, Intraclass Correlation Coefficient Dual Digital Inclinometer x RX; ICCFARX, Intraclass Correlation Coefficient Flexicurve Angle x RX; r, Correlation; rAIRX, Correlation Analog Inclinometer x RX; rFIRX, Correlation Flexicurve Index x RX; rFARX, Correlation Flexicurve Angle x RX; rDKRX, Correlation Debrunner’s Kyphometer x RX; rDDIRX, Correlation Dual Digital Inclinometer x RX; rMKSRX, Correlation Microsoft Kinect Sensor x RX; rSMRX, Correlation Spinal Mouse x RX; rPHRX, Correlation Photogrammetry x RX.
Characteristics of the included reliability studies.
| Authors and year of the study | Instrument | Study Population | Intrarater and InterraterReliability | SEM/MDC |
|---|---|---|---|---|
| Alderighi et al. 201671 | Analog Inclinometer | n = 34Mean age ± SD 19.17 (4.52 years)BMI (kg/m2) 21.00 ± 2.60Sex (M/F) 0/34Heathy female football players (> 3 h/ week) ≥ 3 years (weekly sport hours mean 6.56) | ICCIAR = 0.9195 % CI (0.85 – 0.98)ICCIER = 0.8895 % CI (0.82 – 0.94) | SEMIAR = 2.09°SEMIER = 2.44°MDCIER = 6.77° |
| Amatachaya et al. 201672 | Flexicurve Angle | n = 21Mean age ± SD 74.1 ± 7.6 years;BMI (kg/m²)21.6 ± 3.7Sex (M/F) NROlder individuals with various degrees ofstructural kyphosis | ICCIAR = 0.9795 % CI (0.94 – 0.98)ICCIER = 0.9495 % CI (0.86 – 0.97) | SEMIAR = 2.69°MDCIAR = 7.43°SEMIER = 3.65°MDCIER = 10.08° |
| Azadinia et al.202150 | Photogrammetry Digimizer Image Analysis Software version 5.3.4 (MedCalc Software; BVBA, Ostend, Belgium) | n = 40Mean age ± SD 13.57 ± 1.99 years;BMI (kg/m²)19.28 ± 2.76Sex (M/F) 20/20Adolescents with hyperkyphosis | ICCIAR = 0.9795 % CI (0.94 – 0.98) | SEMIAR = 1.67°MDCIAR = 4.62° |
| Azadinia et al. 201451 | Flexicurve Angle (FA)Dual Digital inclinometer (DDI) | n = 81Mean age ± SD 14.69 ± 4.11 years (range 10 – 30); height (cm) 157 ± 13.5; mass (kg) 50.7 ± 15.3) BMIC (kg/m²) 20Sex (M/F) 26/55Patients with hyperkyphosisn = 21Mean age ± SD 65.76 ± 4.6 years; height (cm) 156.8 ± 5.7; mass(kg) 66.48 ± 8.93)BMIC (kg/m²) 26Sex (M/F) 3/18Patients with hyperkyphosis | ICCIARFA (10 – 30) = 0.87ICCIERFA (10 – 30) = 0.68ICCIARDDI (10 – 30) = 0.98ICCIERDDI (10 – 30) = 0.96ICCIARFA (50 – 80) = 0.86ICCIERFA (50 - 80) = 0.85ICCIARDDI (50 – 80) = 0.97ICCIERDDI (50 – 80) = 0.92 | SEM = NRMDC = NR |
| Barrett et al. 201373 | Analog Inclinometer (AI)Flexicurve Angle (FA)Flexicurve Index (FI) | n = 30 intrarater reliabilityMean age ± SD 45 ± 16 yearsBM (kg) 73.9 ± 11.1; Height (cm) 172.8BMIC (kg/m²) 24Sex (M/F) 18/12n = 12 interrater reliabilityMean age ± SD 49 ± 18 years. BM (kg) 74 ± 15; Height (cm) 172 ± 10 BMIC (kg/m²) 25Sex (M/F) 5/7Swimmers with or without shoulder pain (swimming at least 2 X week. Average Weekly swim distance (km) intrarater 9.9 (SD ± 14) and interrater 7 (SD ± 6) | ICCIARAI = 0.9295 % CI (0.84 – 0.96)ICCIERAI = 0.9095 % CI (0.68 – 0.97)ICCIARFA = 0.9495 % CI (0.88 – 0.97)ICCIERFA = 0.8695 % CI (0.51 – 0.96)ICCIARFI = 0.9495 % CI (0.88 – 0.97)ICCIERFI = 0.8695 % CI (0.51 – 0.96) | SEMIARAI = NRSEMIERAI = 2.2°MDC = NRSEMIARFA = NRSEMIERFA = 1°MDC = NRSEMIARFI = NRSEMIERFI = 0.4°MDC = NR |
| Barauna et al. 200552 | Kypholordometer | n = 30Mean age ± SD 39 ± 15.8 yearsBMI = NRSex (M/F) bothScheuermann's Disease (n = 3)Postural kyphosis (n = 25)Ankylosing Spondylitis (n = 2) | ICCIAR = NR | SEM = NRMDC = NR |
| Büyükturan et al. 201854 | Spinal Mouse | n = 46Mean age ± SD 68.12 ± 2.67 yearsBMI (kg/m2) 29.45 ± 4.67Sex (M/F) 17/29Healthy elderly | ICCIAR = 0.8595 % CI (0.80 – 0.89)ICCIER = 0.9095 % CI (0.88 – 0.91) | SEMIAR = 2.86°MDC = NRSEMIER = 3.14°MDC = NR |
| Carvalho et al. 201974 | Flexicurve Angle | n = 21Mean age ± SDM: 22 ± 0.71 years; BM (kg)78.25 ± 8.83;Height 1.82 ± 0.12 mBMIC (kg/m²) 23F: 22 ± 1.41 years; BM (kg) 53 ± 2.88;Height 1.61 ± 0.04 mBMIC (kg/m²) 20Sex (M/F) 4/17Healthy and asymptomatic | ICCIAR = 0.9495 % CI (0.87 - 0.98)ICCIER = 0.82IC (0.60 - 0.93) | SEMIAR = 2.3°MDCIAR = 6.4°SEMIER = NRMDCIER = NR |
| Chaise et al.201124 | Arcometer | n = 15 intrarater reliability; n = 30 interrater reliabilityMean age ± SD 53.7 ± 14.9 yearsBMI (kg/m2) 26.1 ± 4.4Sex (M/F) NR | ICCIAR = 0.99ICCIER = 0.98 | SEM = NRMDC = NR |
| Czaprowski et al. 201228 | Digital inclinometer | n = 30Mean age ± SD 23 ± 3.4 yearsBMI (kg/m2) 21.4 ± 2.4Sex (M/F) 5/25Healthy subjects | ICCIAR = NRICCIER = NR | SEM = NRMDC = NR |
| Demir et al. 202075 | Spinal Mouse | n = 28Mean age ± SD 16.29 ± 1.08 yearsBMI (kg/m2) 21.14 ± 2.88Sex (M/F) 0/28Asymptomatic females | ICCIAR = 0.8695 % CI (0.54 – 0.88) | SEM = NRMDC = NR |
| de Oliveira et al. 201255 | Flexicurve Angle | n = 15 (intrarater reliability);n = 47 (interrater reliability)Mean age ± SD 44.9 ± 19.4BMI (kg/m2) 27.5 ± 5Sex (M/F) both sexPersons with prescription for an X-ray | ICCIAR = 0.8295 % CI (0.56 – 0.93)ICCIER = 0.9495 % CI (0.86 – 0.97) | SEMIAR = 1.3°MDC = NR |
| Devaney et al. 201776 | Analog Inclinometer | n = 51 intrarater reliability;Mean age ± SD 46.9 ± 20.2 yearsBMI = NRSex (M/F) 25/26Persons with orthopedic conditions | ICCIAR = 0.9495 % CI (0.89 - 0.96) | SEMIAR = 3.0°MDCIAR = 8.0° |
| D'Osualdo et al.1997 56 | Arcometer | n = 16 intrarater reliabilityMean age 13 yearsBMI = NRSex (M/F) 8/8n = 97 interrater reliabilityMean age/SD 14 yearsSex (M/F) 22/27BMI = NRPatients with kyphosis and scoliosis and for postural rehabilitation | ICCIAR = NRICCIER = NRrINTRA = 0.99rINTER = 0.99 | SEM = NRMDC = NR |
| Dunk et al. 200436 | Photogrammetry GOBER, Universityof Guelph, Guelph, ON | n = 14Sex (M/F) 7/7Female: Mean age ± SD 22.0 ± 0.8 years; BM (kg) 66.2 ± 12.0; Height (cm) 162.0 ± 9.9; BMIC (kg/m²) 25Male: Mean age ± SD 21.6 ± 1.3 years; BM (kg) 76.4 ± 5.2; Height (cm) 181.3 ± 4.4BMIC (kg/m²) 23Healthy and active young adults | ICCIAR = 0.51 femaleICCIAR = 0.35 male | SEM = NRMDC = NR |
| Dunk et al. 200577 | Photogrammetry GOBER, University of Waterloo, Waterloo, Ontario. | n = 20Mean age/SDSex (M/F) 10/10Female: Mean age ± SD 21.8 ± 0.6 years; BM(kg) 57.5 ± 8.5; Height (cm) 163.6 ± 6.8; BMIC (kg/m²) 21Male: Mean age ± SD 22.6 ± 1.3 years; BM (kg) 76.7 ± 5.1; Height (cm) 179.1 ± 3.3; BMIC (kg/m²) 23Healthy and active young adults | ICCIAR = 0.63 femaleICCIAR = 0.72 male | SEM = NRMDC = NR |
| Elpeze, G et al. 202378 | Flexicurve Angle (FA)Smartphone (SP-app) protractor software of smartphone inclinometer | n = 60Mean age ± SD 21.92 ± 1.50BMI (kg/m2) 22.74 ± 3.46Sex (M/F) 35/25Subjects with thoracickyphosis ≥ 30° | ICCIARFA = 0.9695 % CI (0.90 – 0.96)ICCIERFA = 0.9195 % CI (0.85 – 0.94)ICCIARSP = 0.9695 % CI (0.93 – 0.97)ICCIERSP = 0.9695 % CI (0.94 – 0.97) | SEM = NRMDC = NRSEM = NRMDC = NR |
| Faramarzi et al. 202057 | SmartphoneGoniometer-Pro app | n = 20 intraraterreliabilityn = 20 interraterreliabilityMean age ± SD 25.1 ± 2.1 years;BMI (kg/m²) 22.5 ± 2.Sex (M/F) NRPersons with prescription for an X-ray | ICCIAR = 0.8895 % CI (0.75 – 0.95)ICCIER = 0.9195 % CI (0.82 – 0.96) | SEM = NRMDC = NR |
| Gravina et al. 201779 | Analog Inclinometer | n = 139Mean age ± SD 12.5 ± 2.5 yearsBMI = NRSex (M/F) 40/99Normal subjects and with spinal deformities (n = 41 - no spine pathology; n = 11 - Scheuermann’s disease;n = 38 - postural hyperkyphosis; n = 49 - mild idiopathic scoliosis) | ICCIAR = NRICCIER = NRrINTRA = 0.83rINTER = 0.84 | SEM = NRMDC = NR |
| Greendale et al. 201112 | DebrunnerKyphometer (DK)Flexicurve index (FI)Flexicurve angle (FA) | n = 113 intrarater reliabilityMean age/SD 75.3 ± 7.5 yearsBMI (kg/m2) 26.5 ± 4.5Sex (M/F) 22/92n = 54 interrater reliabilityMean age/SD 75.5 ± 7.7 yearsBMI (kg/m2) 26.1 ± 4.3)Sex (M/F) 9/45Persons with kyphosis > 40° | ICCIARDK = 0.98ICCIARFI = 0.96ICCIARFA = 0.96ICCIERDK = 0.98ICCIERFI = 0.96ICCIERFA = 0.96 | SEM = NRMDC = NR |
| Hannink et al. 201980 | Microsoft Kinect Sensor index | n = 37Mean age/SD 51.7 ± 20.6 yearsBMI (kg/m2) 24.9 ± 3.3Sex (M/F) 57 % were femaleParticipants without neurological conditions | ICCIAR = 0.9695 % CI (0.92 – 0.97)ICCIER = 0.9795 % CI (0.95 – 0.98) | SEM = NRMDCIAR = 1.49°SEM = NRMDCIER = 1.50° |
| Heitz et al. 201837 | Photogrammetry Software Clinical Photographic Postural Assessment Tool | n = 41 (n = 35 - right side)Mean age/SD 13 ± 2 yearsBM (kg) 43 ± 10 Height (cm)152 ± 11BMIC (kg/m²) 18Sex (M/F) 3/38 | ICCIAR = 0.85 | SEM = 2.4°MDC(CI90 %) = 5.6° |
| Hinman et al. 200495 | Flexicurve Index | n = 51 (25 pre-menopausal/ 26 post-menopausal)Pre-menopausalMean age/SD 29.2 yearsBMI = NRSex (M/F) 0/25Healthy women | ICCIER = 0.9495 % CI (0.90 – 0.96) | SEM = NRMDC = NR |
| Post-menopausalMean age/SD 72.3 yearsBMI = NRSex (M/F) 0/26 | ||||
| Iunes et al. 200535 | Photogrammetry ALCimagem-2000 Manipulando Imagens, versão 1,5 | n = 21Mean age/SD 24.19 ± 1.3 yearsBM (kg) 59.10 ± 12.27Height (m)1.66 ± 0.05BMIC (kg/m²) 21Healthy adultsSex (M/F) 4/17 | ICCIAR = 0.32ICCIER = 0.60 | SEM = NRMDC = NR |
| Kellis et al. 200830 | Spinal Mouse | n = 81Mean age/SD 10.62 ± 1.73 yearsBM (kg) 41.8 ± 9.3; Height (m) 1.47 ± 0.12BMIC (kg/m²) 19Sex (M/F) 81/0Healthy boys | ICCIAR = 0.87ICCIER = 0.89 | SEMIAR = 2.79°MDC = NRSEMIER = 1.47°MDC = NR |
| Korovessis et al. 200120 | DebrunnerKyphometer | n = 90(n = 35 intrarater reliability. n = 90 interrater reliability)Mean age/SD 15 ± 2.6 yearsBMI = NRSex (M/F) 44/46Adolescents with round back or poor sagittal back appearance | ICCIAR = 0.92ICCIER = 0.84 | SEM = NRMDC = NR |
| Lewis et al. 201026 | Analog Inclinometer | n = 90 (n = 45 Adults with shoulder pain)Mean age/SD 43 (19 - 84) years; BM (kg) 71.4; Height (m) 1.7 (range 1.5 - 1.9)BMIC (kg/m²) 24Sex (M/F) 22/23n = 90 (n = 45 Adults without shoulder pain)Mean age/SD 32 (range 23–56) years; BM (kg) 70.4 Height(m) 1.7BMIC (kg/m²) 24Sex (M/F) 21/24 | ICCIAR = 0.9795 % CI (0.94 – 0.98)ICCIAR = 0.9795 % CI (0.95 – 0.99) | SEM = 1.7°MDC = NRSEM = 1.0°MDC = NR |
| Lewis et al. 200525 | Analog Inclinometer | n = 120(n = 15 Adults with shoulder pain)Mean age/SD 48.9 ± 15.2 years; BM (kg) 74.5 ± 12.7Height(m) 171.2 ± 9.7; BMIC (kg/m²) 25Sex (M/F) 35/25(n = 15 Adults without shoulder pain)Mean age/SD 34.1 ± 9.9 yearsBM (kg) 67.8 ± 13.4; Height (m) 170.9 ± 10.4BMIC (kg/m²) 23Sex (M/F) 29/31 | Subjects with symptomsICCIAR = 0.9495 % CI (0.83 – 0.98)Subjects without symptomsICCIAR = 0.9695 % CI (0.91 – 0.98) | SEM withsymptoms 2.5°MDC = NRSEM without symptoms 1.5°MDC = NR |
| Lundon et al. 199821 | Debrunner Kyphometer (DK)Flexicurve angle (FA) | n = 26Mean age/SD 18 - 56 yearsBMI = NRSex (M/F) 0/26Postmenopausal women with diagnosis of osteoporosis | ICCIARDK = 0.99ICCIARFA = 0.96ICCIERDK = 0.88ICCIERFA = 0.87 | SEM = NRMDC = NR |
| MacIntyre et al. 201481 | Digital inclinometer | n = 36Mean age/SD 69 ± 8.1 yearsBMI = NRSex (M/F) 86 % were womenAdults at risk for osteoporotic fracture (89 % osteoporotic/ 11 % osteopenic) | ICCIAR = 0.9195 % CI (0.84 - 0.95) | SEMIAR = 3.5° (2.90 - 4.6°)MDC(CI90 %) = 8.2° |
| Mannion et al. 200482 | Spinal Mouse | n = 20Mean age/SDMales 45.4 ± 7.7 yearsBMI (kg/m²) 26.5 ± 5.2Females 38.2 ± 7.6 yearsBMI (kg/m²) 22.9 ± 5.7Sex (M/F) 9/11Healthy volunteers | ICCIAR = 0.8895 % CI (0.67 - 0.94)ICCIER = 0.8795 % CI (0.70 - 0.95) | SEMIAR = 2.8°(2.1 - 4.0)MDC = NRSEMIER = 2.7°(2.0 - 3.9)MDC = NR |
| Mellin G, 198627 | Analog Inclinometer | n = 25 (n = 10 intratester reliability; n = 15 interrater reliability)Mean age/SD 31.3 ± 5.8 yearsBM (kg) 67.8 ± 15.4Height (cm)169.1 ± 9.1BMIC (kg/m²) 23Healthy adultsSex (M/F) 9/16 | rINTRA = 0.92rINTER = 0.83 | SEM = NRMDC = NR |
| Nair et al. 201796 | Analog Inclinometer | n = 28Mean age/SD 69.7 ± 10.6 yearsBMI (kg/m²) 26.3 ± 6.2Sex (M/F) 16/12Subjects with Parkinson Disease | ICCIER = 0.77995 % CI (0.57 – 0.89) | SEM = NRMDC = 13.9° |
| Ohlén et al.198922 | DebrunnerKyphometer | n = 31Mean age/SD 32 ± 11 yearsBMI = NRSex (M/F) 10/21Healthy adults | ICC = NRrIAR = 0.92rIER = 0.94 | SEM = NRMDC = NR |
| Perriman et al. 201031 | Electrogoniometer | n = 12Mean age/SD 40.7 (25–61) years;BM (kg) 70.9 (50–95)Height (cm) 170.0 (156–186);BMIC (kg/m²) 24.5Sex (M/F) 4/8Healthy adults | ICCIAR = 0.9095 % CI (0.70 – 0.97) | SEM = NRMDC = NR |
| Pakeloğlu et al. 202383 | Flexicurve Angle (FA)Smartphone-app (SP)Goniometer Pro app | n = 30Mean age/SD 21.13 ± 1.78 yearsBMI (kg/m²) 21.97 ± 3.17Height (cm) 173.23 ± 9.54Sex (M/F) 13/17Healthy and asymptomaticparticipants | ICCIARFA = 0.8795 % CI (0.75 – 0.93)ICCIERFA = 0.6295 % CI (0.20 – 0.82)ICCIARSP = 0.9095 % CI (0.80 – 0.95)ICCIERSP = 0.8795 % CI (0.73 – 0.94) | SEMIARFA = 1.73°MDCIARFA = 3.39°SEMIARFA = 1.59°MDCIARFA = 3.11°SEMIIARSP = 1.48°MDCIARSP = 2.90°SEMIIARSP = 1.60°MDCIARSP = 3.13° |
| Prowse et al. 201833 | Baseline® Body Level/Scoliosis meter | n = 31Mean age/SD 13.6 ± 0.6 yearsBMI = NRSex (M/F) 4/27Adolescent with scoliosis | ICCIER = 0.9495 % CI (0.87- 0.97) | SEM = 1.66cmMDCIER = 4.60cm |
| Purser et al. 199984 | Debrunner Kyphometer | n = 24Mean age/SD 68 ± 4 yearsBMI = NRSex (M/F) 3/21Community-dwelling elderlyn = 15Mean age/SD 75 ± 6 yearsBMI = NRSex (M/F) 13/2Community-dwelling with Parkinson diseasen = 12Mean age/SD 82 ± 4 yearsBMI = NRSex (M/F) 0/12Subjects with vertebral osteoporosisn = 14Mean age/SD 74 ± 6 yearsBMI = NRSex (M/F) 12/2Nursing home residents | Community-dwelling elderly personsICCIAR = 0.96Community-dwelling with Parkinson diseaseICCIAR = 0.95Subjects with vertebral osteoporosisICCIAR = 0.92Nursing home residentsICCIAR = 0.91Overall ICC = 0.95 | SEM = NRMDC = NR |
| Quek et al. 201738 | Flexicurve Angle (FA)Flexicurve Index (FI)Microsoft Kinect Sensor Angle (MKA)Microsoft Kinect SensorIndex (MKI) | n = 33 (n = 29 intrarater reliability)Mean age/SD 31 ± 11.0 yearsBM (kg) 64.2 ± 12.0Height (cm)170.2 ± 8.2BMIC (kg/m²) 22Sex (M/F) 17/16Healthy adults | ICCIARFA = 0.8395 % CI (0.63 – 0.92)ICCIARFI = 0.8395 % CI (0.63 – 0.92)ICCIARMKA = 0.9695 % CI (0.92 – 0.98)ICCIARMKI = 0.98 IC95 % CI (0.95 – 0.99) | SEMFA = 0.99°MDCFA = 2.7°SEMFI = 1.11°MDCFI = 3.1°SEMMKA = 0.69°MDCMKA = 1.9°SEMMKI = 0.53°MDCMKI = 1.5° |
| Raine and Twomey, 199,485 | PhotogrammetryGTCO digitiser of O.lmm resolution,a Hewlett-Packard HP9836CS computerand an IBM-compatiblecomputer | n = 38 (n = 29 intrarater reliability)Mean age/SD 22(17 - 48) yearsBMI = NRSex (M/F) 8/30Healthy adults | Upper thoracic curvatureICCIAR = 0.92Lower thoracic curvatureICCIAR = 0.94 | SEM = NRMDC = NR |
| Roghani et al. 201786 | Spinal Mouse | n = 19Mean age/SD 67 ± 5.0 yearsBMI (kg/m²) 28.5 ± 3.4Sex (M/F) 0/19Women with hyperkyphosisn = 14Mean age/SD 63 ± 6.0 yearsBMI (kg/m²) 26.7 ± 3.4Sex (M/F) 0/14Women with a normal curvature | HyperkyphosisICCIAR = 0.9495 % CI (0.86 – 0.98)Normal CurvatureICCIAR = 0.8995 % CI (0.69 – 0.96) | HyperkyphosisSEM = 1.56°MDC = 4.33°Normal Curvature SEM = 1.75°MDC= 4.86° |
| Saad et al. 201287 | PhotogrammetryCorelDRAW software (version 11.0) | n = 20Mean age/SD 23.1 + 9.0 yearsBMI (kg/m²) 22.28 ± 5.27Sex (M/F) 3/17Participants with scoliosis | ICCIAR = 0.93(right side)ICCIER = 0.97(right side) | SEM = NRMDC = NR |
| Şahinoğlu et al. 202388 | Digital Inclinometer (DI)Smartphone-app (SP) | n = 80Mean age/SD 20.42 ± 1.40 yearsBMI (kg/m²) 22.58 ± 3.16Sex (M/F) 42/38Height (cm)171.0 ± 0.09Young and healthy subjects | ICCIARDI = 0.9495 % CI (0.91 – 0.96)ICCIERDI = 0.8295 % CI (0.73 – 0.89)ICCIARSP = 0.9495 % CI (0.90 – 0.96)ICCIERSP = 0.8095 % CI (0.68 – 0.88) | SEMIARDI = 1.81°MDCIARDI = 5.04°SEMIERDI = 3.03°MDCIERDI = 8.39°SEMIARSP = 2.27°MDCIARSP = 6.30°SEMIERSP = 3.25°MDCIERSP = 9.02° |
| Sangtarash et al. 201463 | Dual Digital Inclinometer | n = 20Mean age/SD 57.20 ± 7.67 yearsBMI (kg/m²) 27.75 ± 4.47Sex (M/F) 0/20Women with back pain | ICCIAR = 0.92 | SEMIAR = 1.98˚MDC = NR |
| Sedrez et al. 201423 | Arcometer | n = 40Mean age/SD 10.7 ± 2.7 yearsBM (kg)38.7 ± 13.1Height(m) 1.39 ± 0.17BMIC (kg/m²) 20Sex (M/F) 25/15Children (status not reported) | ICCIAR = 0.50ICCIER = 0.25 | SEM = NRMDC = NR |
| Sedrez et al. 201689 | Flexicurve Angle | n = 40 (n = 38 intrarater reliability;n = 40 interrater reliability)Mean age/SD 10.2 ± 2.8 yearsBMI (kg/m²) 19.5 ± 2.8Sex (M/F) 25/15Children who had undergone X-ray examination | ICCIAR = 0.8295 % CI (0.65 – 0.91)ICCIER = 0.8395 % CI (0.61 - 0.92) | SEMIAR = 4.1°MDCIAR = 8.1°SEMIER = 4.1°MDCIER = 8.0° |
| Schmidt et al. 202264 | Analog Inclinometer | n = 16Mean age/SD 12.3 ± 1.0 yearsBMI (kg/m²) 20.3 ± 3.3Sex (M/F) NRAdolescent with idiopathicscoliosis - Group 1 Risser 1 or 2n = 23Mean age/SD 15.0 ± 1.7 yearsBMI (kg/m²) 24.1 ± 4.9Adolescent with idiopathicscoliosis - Group 2 Risser 3 or 4 | ICCIAR group1 = 0.88ICCIER group1 = 0.86ICCIAR group2 = 0.90ICCIER group2 = 0.85 | SEM = NRMDC = NRSEM = NRMDC = NR |
| Sharifnezhad et al. 202165 | PhotogrammetryKinovea software | n = 18Mean age/SD 42.64 ± 21.67 yearsBMI (kg/m²)23.48 ± 3.62Sex (M/F) 8/10Persons with prescription for an X-ray | ICCIAR = 0.9095 % CI (0.74 – 0.96)ICCIER = 0.8195 % CI (0.61 – 0.92) | SEM = NRMDC = NR |
| Sheeran et al. 201032 | Spinal Wheel | n = 17Mean age/SDMale 37 ± 10.4 years; BMI (kg/m²) 25.5 ± 6.1Female 40 ± 10.8 years; BMI (kg/m²) 24.5 ± 6.8Sex (M/F) 9/8Healthy volunteers | ICCIAR = 0.9895 % CI (0.92 – 0.99)ICCIER = 0.9895 % CI (0.95 – 0.99) | SEMIAR = 1.7°SEMIER = 2.0° |
| Stolinski et al. 201790 | PhotogrammetrySoftware SCODIAC | n = 91 (n = 20 intrarater reliability; n = 30 interrater reliability)Mean age/SD 8.2 ± 1.0 yearsBMI = NRSex (M/F) 47/44Healthy volunteers | ICCIAR = 0.93 /95 % CI (0.88 - 0.97)ICCIER = 0.9295 % CI (0.86 – 0.96) | SEMIAR = 1.1°MDC = NRSEMIER = 0.9°MDC = NR |
| Tabard-Fougere et al. 201,967 | Analog Inclinometer | n = 51Mean age/SD 13.5 (2.0) yearsBMI (kg/m²) 18.9 ± 2.8Sex (M/F) 19/32Adolescent with idiopathicscoliosis | ICCIAR = 0.9895 % CI (0.97 - 0.98) | SEM = NRMDC = NR |
| Takatalo et al. 202091 | Digitalinclinometer | n = 32Mean age/SD 39 ± 9.2 years; BMI (kg/m²) 24.5 ± 3.2Sex (M/F) 16/16Persons with pain in thoracic spine | ICCIAR = 0.8395 % CI (0.66 - 0.92)ICCIER = 0.8295 % CI (0.64 – 0.91) | SEMIAR = 3.09°MDC = NRSEMIER = 3.18°MDC = NR |
| Teixeira et al. 200768 | Flexicurve Angle | n = 56Mean age/SD 66.7 ± 9.37 yearsBMI = NRSex (M/F) 21/35Healthy elderly | ICCIAR = 0.87ICCIER = 0.94 | SEM = NRMDC = NR |
| Temporiti et al. 202392 | PhotogrammetryBHOHB system (Bhohb S.r.l., Italy) | n = 30Mean age/SD 22.3 years ± 9.0 years;Mean weight 64.9 kg, SD:9.04 kgMean height 173.2 cm, SD: 8.1 cmBMIC (kg/m²) 21.7Sex (M/F) 15/15Healthy adult volunteers | ICCIAR = 0.9895 % CI (0.96 – 0.99) | SEM = 0.78°MDC = NR |
| Todd et al. 201569 | Debrunner Kyphometer | n = 102 (n = 10 intrarater reliability; n = 10 interrater reliability)Mean age ± SD (reliability) 18.3 ± 1.13 yearsBMI (kg/m²) 22.9 ± 3.12Sex (M/F) NR for reliabilityYoung athletic elite alpine skiers | ICCIAR = 0.8395 % CI (0.30 – 0.96)ICCIER = 0.9695 % CI (0.85 – 0.99) | SEM = NRMDC = NR |
| Tran et al. 201670 | Debrunner Kyphometer (DK)Flexicurve Index (FI) | n = 71 (DB); n = 72 (FI);Mean age/SD 77.8 ± 7.1 yearsBMI (kg/m²) 25.3 ± 4.6Sex (M/F) 20/52Persons recruited from community with thoracic kyphosis | ICCIERFI = 0.93ICCIERDB = 0.99 | SEM = NRMDC = NR |
| van Baalen et al. 202393 | Analog Inclinometer AI)Smartphone (SM-app) | n = 17Mean age/SD 23.7 ± 2.3 years;BMI (kg/m²) = 22.3 ± 1.6;Height 1.69 (m) ± 0.1Sex (M/F) 13/4Asymptomatic volunteers | ICCIARAI = 0.9295 % CI (0.84 – 0.97)ICCIERAI = 0.8195 % CI (0.55 – 0.93)ICCIARSP = 0.9495 % CI (0.87 – 0.97)ICCIERSP = 0.6795 % CI (0.08 – 0.89) | SEMIARAI = 1.7°MDCIARAI = 4.7°SEMIERAI = 2.6°MDCIERAI = 7.1°SEMIARSP = 1.5°MDCIARSP = 4.3°SEMIERSP = 3.2°MDCIERSP = 9.0° |
| van Blommestein et al. 201294 | Analog Inclinometer | n = 30Mean age/SD 33 ± 11.23 years; BM (kg) 72 ± 12; Height 172 (cm) ± 11BMIC (kg/m²) 24Sex (M/F) 15/15Asymptomatic volunteers | ICCIAR = 0.9695 % CI (0.92 – 0.98) | SEM = 1.7°MDC = NR |
| Was et al. 201639 | Digital Inclinometer (DI)Smartphone (SP-app)Android 4.0.3software with a built-in accelerometer | n = 40 (n = 20 intrarater reliability)Mean age/SD 23.2 ± 3.4 yearsBMI (kg/m²) 24.9 ± 3.6 (male)BMI (kg/m²) 22.5 ± 4.5 (female)Sex (M/F) 14/26Healthy students | ICCIARDI = 0.8ICCIARSP = 0.8 | SEM = NRMDC = NR |
| Willner and Johnson, 198,318 | Spinal Pantograph | n = 1101 (n = 10 intrarater reliability)Mean age/SD ages of 8–16BMI NRSex (M/F) 565/536Healthy children | ICCIAR = NR | SEM = NRMDC = NR |
| Willner Stig, 198117 | Spinal Pantograph | n = 71Mean age/SD NRSex (M/F) NRTeenagers with or without visible spinal disorder | ICCIAR = NRICCIER = NR | SEM = NRMDC = NR |
| Yanagawa et al. 200042 | Flexicurve index | n = 26Mean age/SD 67.1 yearsBM (kg) 59.9 ± 10.6Height (cm)158.6 ± 7.7BMIC (kg/m²) 23Sex (M/F) 0/26Women who were enrolled in the Trym Gym Osteoporosis Exercise Program | ICCIAR = 0.9395 % CI (0.85 – 0.97) | SEM = NRMDC = NR |
Note. NR, Not reported; BM, Body mass; BMI, Body mass index; BMIC, Body mass index calculated; 95 % CI, 95 % confidence intervals; ICC, Intraclass correlation coefficient; ICCIAR, Intrarater ICC; ICCIER, Interrater ICC; ICCIARFA, Intrarater ICC flexicurve angle; ICCIERFA, Interrater ICC flexicurve angle; ICCIARFI, Intrarater ICC flexicurve index; ICCIERFI, Interrater ICC flexicurve index; ICCIARDDI, Intrarater ICC dual digital inclinometer; ICCIERDDI, Interrater ICC dual digital inclinometer; ICCIARI, Intrarater ICC analog inclinometer; ICCIERAI, Interrater ICC analog inclinometer; ICCIARSP, Intrarater ICC smartphone-app; ICCIERSP, Interrater ICC smartphone-app; ICCIARDK, Intrarater ICC debrunner kyphometer; ICCIERDK, Interrater ICC debrunner kyphometer; ICCIARMKSA, Intrarater ICC microsoft kinect sensor angle; ICCIERMKSI, Interrater ICC microsoft kinect sensor index; ICCIARDI, Intrarater ICC digital inclinometer; CI, Confidence interval 95 %; SEM, Standard error of measurement; SEMIAR, Standard error of measurement of intrarater ICC; SEMIER, Standard error of measurement of interrater ICC; SEMIARFA, SEMIAR flexicurve angle; SEMIERFA, SEMIER flexicurve angle; SEMIARFI, SEMIAR flexicurve index; SEMIERFI, SEMIER flexicurve index; SEMIARMKA, SEMIAR microsoft kinect sensor angle; SEMIERMKI, SEMIER microsoft kinect sensor index; SEMIARSP, SEMIAR smartphone app; SEMIERSP, SEMIER smartphone-app; MDC, Minimal detectable change; MDCIAR, Intrarater MDC; MDCIER, Interrater MDC; MDCIARFA, MDCIAR flexicurve angle; MDCIARFI, MDCIAR flexicurve index; MDCIARMKA, MDCIAR Microsoft kinect sensor angle; MDCIARMKI, MDCIAR microsoft kinect sensor index; rINTRA, Intrarater Correlation; rINTER, Interrater Correlation.
The studies sample size ranged from 11 to 139 participants. Regarding the sample of the studies, 33 (45.83 %) evaluated healthy individuals, 20 (27.77 %) included patients with kyphosis or scoliosis, eight (11.11 %) included patients with musculoskeletal pain in different body regions, five (6.94 %) included patients with osteoporosis or reduced bone mass, five (6.94 %) included individuals who had been referred for a thoracic spine X-ray, three (4.16 %) evaluated athletes, two (2.77 %) evaluated patients with Parkinson's, one (1.38 %) evaluated individuals with some orthopedic condition and one (1.38 %) did not characterize the sample. Regarding the age group, 14 studies (19.44 %) evaluated individuals aged ≥ 60 years, 40 (55.94 %) evaluated adults aged between 18 and 60 years, and 20 (27.77 %) evaluated children and adolescents. Regarding sex, 56 (77.77 %) studies included individuals of both sexes, nine (12.50 %) included only women, two (2.77 %) included only men, and five (6.94 %) studies did not report the sex of the individuals.
Between the studies that reported the type of orthostatic posture during the measurement of thoracic kyphosis, 43 (59.72 %) evaluated the relaxed orthostatic posture, 16 (22.22 %) the upright orthostatic posture, and 4 (5.55 %) evaluated both postures.
Methodological quality of included studiesThe methodological quality is reported in Supplementary material 3. Of the 72 studies, 62 (86.11 %) had high quality. Regarding validity, of the 31 studies, 26 (83.87 %) had high methodological quality. Of the 58 intra-rater reliability studies, 50 (86.20 %) were of high quality and 33 (82.50 %) out of the 40 inter-rater reliability studies were of high quality. The CAT items with the worst scores were related to the lack of randomization of evaluators or individuals and the lack of information about the qualifications and experience of the raters, the rater blinding process, and the time interval between the measurement by the instrument and the gold standard.
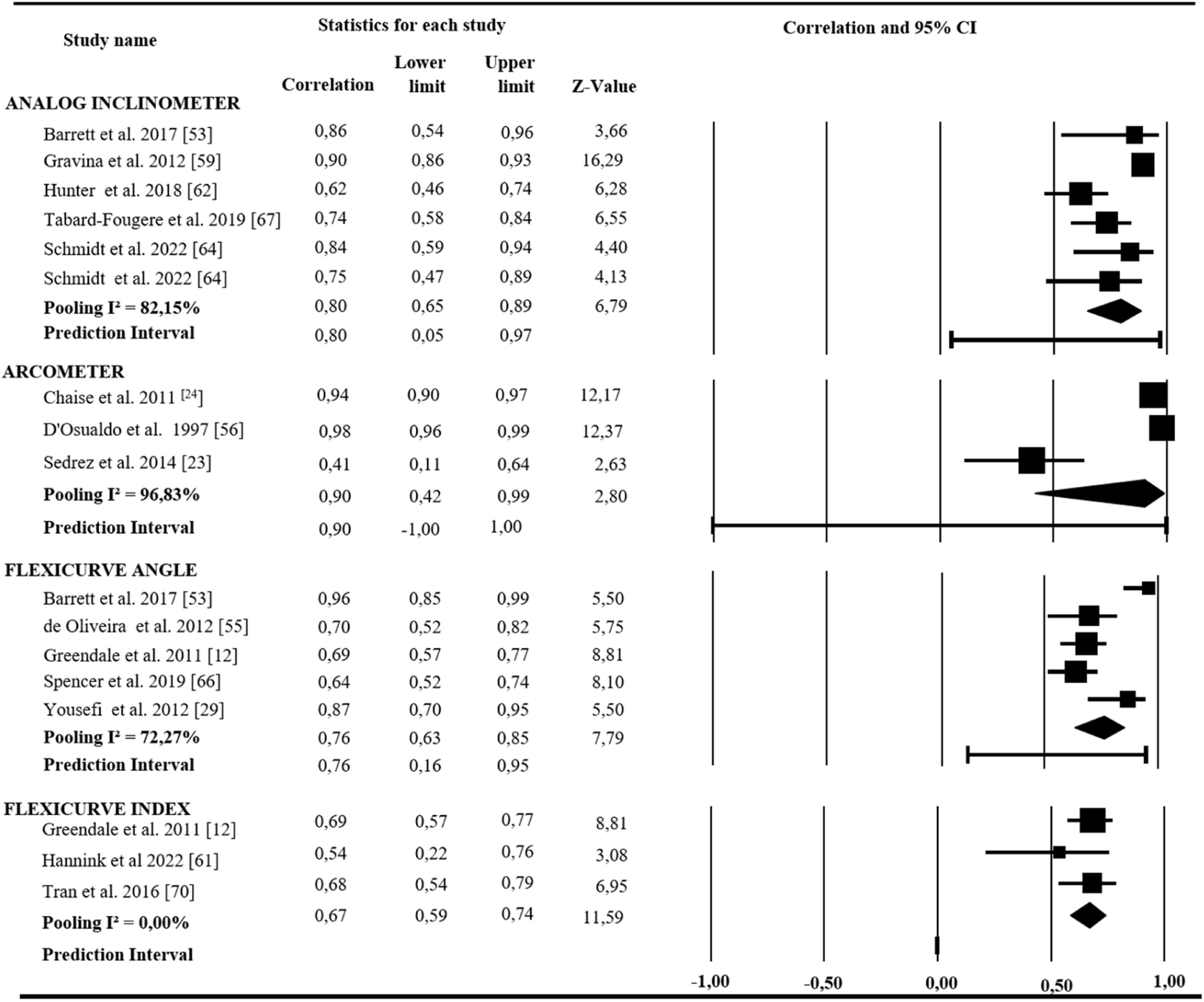
ValidityA total of 13 instruments had concurrent validity assessed in 31 studies (Table 1). The most investigated were the Analog Inclinometer and Flexicurve Angle. On the other hand, the validity of the Digital Inclinometer and Spinal Wheel was not investigated. The Baseline® Level/Scoliosis meter (r = 0.32),33 Kipholordometer (r = 0.78),52 Electrogoniometer (r = 0.87),31 Dual Digital Inclinometer (r = 0.67),61 Microsoft Kinect Sensor (r = 0.70),61 and the Smartphone app (r = 0.81)57 had the validity tested in only one study; thus, they were not included in the meta-analysis. Seven instruments presented the correlation coefficient with the X-ray examination reported by at least two studies; therefore, they were grouped into seven meta-analyses, one for each instrument (Fig. 2). The meta-analysis demonstrated that the Analog Inclinometer, Arcometer, Flexicurve Angle, Photogrammetry, Spinal Mouse and Spinal Pantograph presented strong concurrent validity with the X-ray. The Debrunner Kyphometer and Flexicurve Index demonstrated moderate levels of concurrent validity with the X-ray (Fig. 2). Bland-Altman analysis was described for nine instruments and is presented as the mean difference between measurements (Table 1).
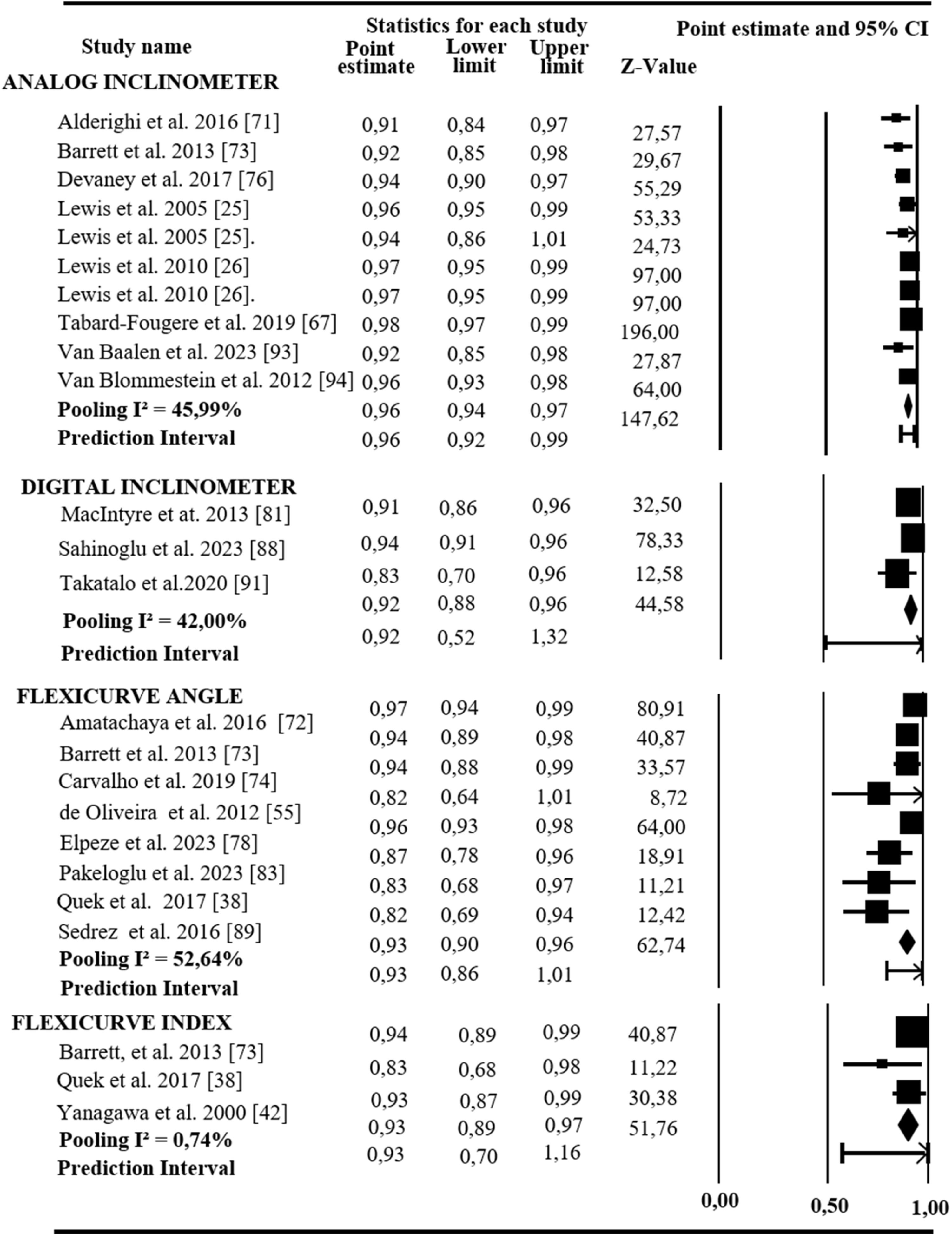
Intra-rater reliabilityFourteen instruments had their intra-rater reliability assessed in 55 studies (Table 2); the Analog Inclinometer, Flexicurve Angle, and Photogrammetry were the most investigated. Seven instruments had the 95 % CI of the ICC reported by at least two studies and were grouped into seven metanalyses, one for each instrument. The following instruments demonstrated an excellent level of intra-rater reliability: Analog, Digital Inclinometer, Flexicurve Angle, Flexicurve Index, Photogrammetry, Microsoft Kinect Sensor, Smartphone app, and Spinal Mouse (Fig. 3). This analysis was not performed in studies that used the Baseline ® Level/Scoliosis meter.33 The Kipholordometer52 and Spinal Pantograph17 instruments did not have the ICC reported. The Electrogoniometer (ICC = 0.90)31 and Spinal Wheel (ICC = 0.98),32 evaluated in only one study each, showed excellent intra-rater reliability. The Arcometer was evaluated in three studies: one did not report the ICC,56 and the other two demonstrated levels of intra-rater reliability ranging from good to excellent (0.50 to 0.99) but did not report the 95 % CI of the ICC23–24; therefore, they were not included in the meta-analysis. The Debrunner Kyphometer12,20–21,69,84 and the Dual Digital Inclinometer51,63 were evaluated in five and two studies, respectively, and demonstrated excellent levels of intra-rater reliability. However, they also did not present the 95 % CI of the ICC and were not grouped in the meta-analysis. The MDC and SEM were reported for six and eight instruments, respectively (Table 2).
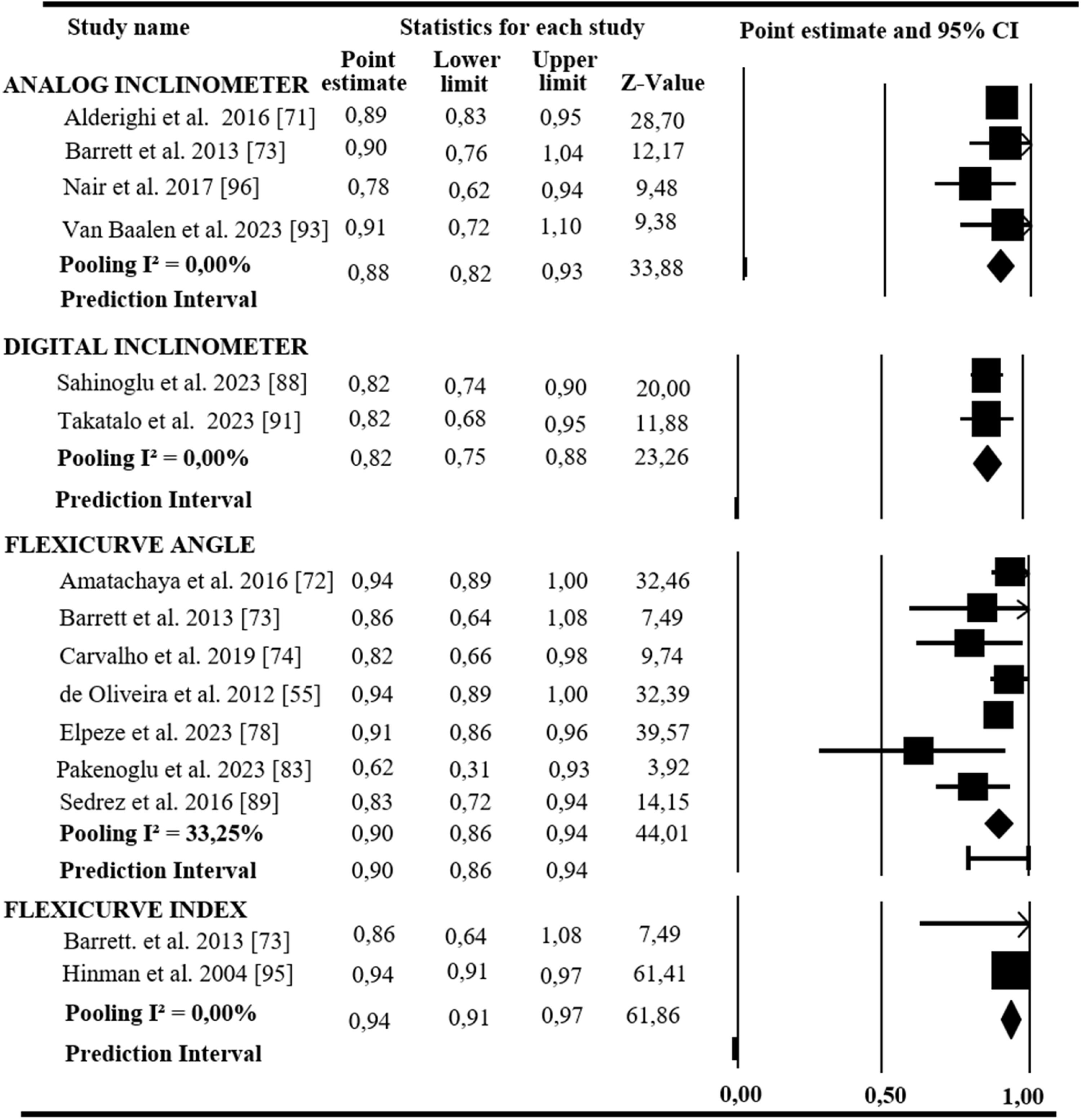
Inter-rater reliabilityTwelve instruments had their inter-rater reliability assessed by 40 studies (Table 2); the Flexicurve Angle, the Debrunner Kyphometer, and the Analog Inclinometer were the most investigated. Six of these 12 instruments had ICC and 95 % CI of the ICC data reported by at least two studies. These data were grouped into six meta-analyses, one for each instrument. The following instruments demonstrated excellent inter-rater reliability: Analog Inclinometer, Digital Inclinometer, Flexicurve Angle, Flexicurve Index, Photogrammetry, Smartphone app, and Spinal Mouse (Fig. 4). Moreover, the inter-rater reliability was not assessed in studies that used the Kypholordometer52 and Electrogoniometer.31 The Baseline® Level/Scoliosis,33 Dual Digital Inclinometer,51 Microsoft Kinect Sensor,80 and Spinal Wheel32 were investigated in only one study each, showing excellent inter-rater reliability (Table 2). The Spinal Pantograph was explored in only one study,17 but the ICC was not performed. The Arcometer was evaluated in three studies: one did not report the ICC,56 and two demonstrated levels of inter-rater reliability ranging from low to excellent (0.25 to 0.98)23–24; however, they did not report the 95 %CI of the ICC, making the meta-analysis unfeasible. The Debrunner Kyphometer was evaluated in six studies,12,20–22,69–70 but only one reported the 95 % CI of the ICC69; the meta-analysis was not performed. One study did not report the ICC,22 and the other five showed excellent inter-rater reliability (Table 2).12,20–21,69–70 The MDC and SEM were reported for five and seven instruments, respectively (Table 2).
Utility of the instrumentAll instruments' measurement properties were investigated and classified according to clinical utility (Supplementary materials 4 and 5). Only the Analog Inclinometer, Flexicurve Angle, and Smartphone app demonstrated excellent levels for all measurement properties (> 0.80) and reported MDC data. The Microsoft Kinect Sensor did not present excellent validity; thus, this instrument was not considered. The Arcometer, Photogrammetry, and Spinal Mouse demonstrated excellent validity and reliability but did not have MDC data reported; therefore, they were not considered. Last, the instruments Baseline® Body Level/Scoliosis meter, Kypholordometer, Debrunner Kyphometer, Digital Inclinometer, Dual Digital Inclinometer, Electrogoniometer, Flexicurve Index, Spinal Pantograph, and Spinal Wheel did not present excellent validity and reliability levels or one or more measurement properties and cannot be considered helpful for clinical practice. Therefore, only the Analog Inclinometer, Flexicurve Angle, and Smartphone app are recommended for use in clinical settings (scores ≥ 9).
DiscussionThe present review with meta-analysis investigated the validity, intra- and inter-rater reliability, and clinical utility of instruments designed to measure thoracic kyphosis. In the 72 included studies, 15 instruments had their measurement properties investigated; the Flexicurve Angle and Analog Inclinometer were the most investigated. Data from seven instruments were grouped in a meta-analysis for validity and intra-rater reliability and from six instruments for inter-rater reliability.
Most studies investigating validity demonstrated a moderate to strong correlation with the gold standard measure. Some factors may interfere with the correlation between noninvasive instruments and X-ray examinations. For instance, The Cobb angle quantifies the thoracic kyphosis by locating the positioning of the vertebrae on the X-ray. In contrast, the instrument is positioned on the skin and suffers the interference of soft tissue artifacts, which may generate discrepancies between measures.24 Although all studies included in this review described the procedures for assessing thoracic kyphosis, four studies did not declare which vertebral limits were used to measure thoracic kyphosis by X-ray examination.34,56,58–59 In addition, clinical measurements and imaging examinations are generally not standardized. Some studies measured thoracic kyphosis with the instrument positioned between C7 and T12,53 T2/T3 and T11/T12,69–70 and from C7 to the curve inflection point.70 Although the measurement recommended by Cobb for X-ray examination is from T4 to T12, some measurements presented variations, such as from T1 to T1062 and T1 to T12.23 Another aspect that may interfere with validity is the time interval between the clinical and the gold standard measurement. Although 10 studies did not report this interval, most performed both measurements on the same day. Finally, a strong correlation with the gold standard does not ensure good agreement and measurement accuracy between the two methods.50 A few instruments were analyzed using the Bland-Altman to verify the agreement limits. Therefore, further validity studies must perform the Bland-Altman analysis.
The Analog Inclinometer, Digital Inclinometer, Flexicurve Angle and Index, Photogrammetry, Microsoft Kinect Sensor, Spinal Mouse, and Smartphone app showed excellent levels of intra-rater reliability. Examiner experience and lack of blinding of the examiner and the time interval between measurements may help to explain these findings. Most of the studies included in the intrarater reliability analysis (65.51 %) declared that the rater was experienced in clinical practice or in using the instrument. Regarding blinding, only 14 studies declared the rater was blind to the measurements. Furthermore, most studies (86.20 %) adopted a time interval of up to seven days, allowing control over changes in posture resulting from flexibility and body mass index.33
The Analog Inclinometer, Digital Inclinometer, Flexicurve Angle and Index, Photogrammetry, Smartphone app, and Spinal Mouse demonstrated excellent inter-rater reliability. Although differences between examiners’ experience may hinder inter-rater reliability, eight studies included in the meta-analysis (44.44 %) used examiners with different experience levels, which suggests that these instruments are user-friendly.65,71,73,78,88,90–91,93 Few studies investigated the SEM and the MDC of the instruments. Some measurement errors may include the experience of the examiner in locating reference points on the skin,71 the positioning, pressure, and speed in which the instrument is slid over the skin,32 transfer the measurement to the paper (e.g., Flexicurve measurement),73 the location of markers in the software,77 and the positioning of the individual.20 Most studies evaluated individuals in a relaxed orthostatic posture. Some studies have observed a positive correlation between thoracic curvatures measured from upright and relaxed postures and noted that the measurement is significantly smaller when performed from an upright posture.76,96 Therefore, the choice of which posture to evaluate should consider that the measurement of the thoracic kyphosis in an upright orthostatic position will reflect structural kyphosis and minimize the effects of muscle weakness.72
Regarding clinical utility, this review identified that the Analog Inclinometer, Flexicurve Angle, and Smartphone app are suitable for clinical practice. Although the Flexicurve Angle presents MDC and excellent levels of reliability and validity, the agreement between this instrument and the modified Cobb angle by the X-ray using the Bland Altman demonstrated wide limits of agreement.53,55,66 Furthermore, the Flexicurve underestimates the magnitude of the thoracic kyphosis angle in the sagittal plane to X-ray, and this may be a problem in clinical settings when precise measurements are required.66 Future studies could explore the measurements properties of the Digital Inclinometer and Dual Digital Inclinometer, which have a moderate cost, are portable, easy to administer, do not require specific training, and are often used in clinical settings.
The use of low-cost, portable, and precise clinical instruments can significantly improve patient outcomes by enabling quick, objective assessments and early detection of thoracic kyphosis severity, facilitating timely interventions. Continuous monitoring across various settings, such as clinics or patients' homes, supports frequent adjustments to treatment plans, resulting in better functional and postural outcomes while enhancing treatment adherence. Reliable, standardized measurements reduce intra- and inter-rater variability, ensuring consistent data and evidence-based clinical decisions. Combining precision with efficiency, these tools enable personalized rehabilitation strategies that adapt to changes in the patient’s condition.
This review had some limitations. Data extraction was conducted by only one author. In addition, when studies reported the experience of the rater, only the intra-rater reliability from the most experienced was extracted. When not reported, the highest reliability value was extracted, which may have overestimated the intra-rater reliability levels. Furthermore, the meta-analysis did not differentiate between ICC models due to limitations in the available data and the number of included studies, which may have impacted the interpretation of reliability measures. Additionally, subgroup analyses were not conducted due to the limited number of studies and concerns about insufficient statistical power, which could lead to unreliable and non-robust conclusions.97
Compared with the Barret et al. review, the present review found a higher number of studies on the topic not only in healthy individuals, but also in patients with disabilities and athletes. However, the reliability and validity of the instruments are generally specific to the investigated sample. Therefore, generalization of these findings to populations not considered in this review must be conducted cautiously.
ConclusionsThe present review demonstrated the validity and intra and interrater reliability of 15 clinical instruments for assessing thoracic kyphosis in the sagittal plane. The meta-analysis demonstrated that the Analog Inclinometer, Flexicurve Angle and Index, Photogrammetry, and Spinal Mouse are valid and reliable for evaluating thoracic kyphosis in the sagittal plane. The analysis of the instruments’ utility suggests using the Analog Inclinometer, Flexicurve Angle, and the Smartphone app to measure thoracic kyphosis in the sagittal plane in clinical settings.
The authors declare no competing interest.