Cognitive Behavioural Therapy for Insomnia (CBT-I) is the first-choice treatment for insomnia disorders. Although CBT-I is primarily provided by trained psychologists, evidence shows that other healthcare providers can also successfully apply interventions based on CBT-I principles in absence of complex psychiatric comorbidities. Because insomnia and chronic pain often co-occur, integrating CBT-I-based interventions into physical therapy is relevant.
ObjectivesTo identify implementation barriers for CBT-I in physical therapist practice and to formulate implementation strategies to address them.
Methods16 stakeholders (8 physical therapists, 3 psychologists, 2 general practitioners, and 3 individuals with chronic pain and insomnia) were invited for 3 group-interviews and 1 online questionnaire. Implementation barriers were identified through thematic analysis according to the Consolidated Framework for Implementation Research (CFIR). Implementation strategies were matched to barriers and ranked based on evidence and stakeholder feedback.
Results33 implementation barriers were identified across all CFIR domains, and 13 final strategies were formulated to address these barriers. Key strategies included education and training for physical therapists, structural changes, and raising awareness among general practitioners and the public. Secondary strategies focussed on adaptability of CBT-I, developing supporting tools, and multidisciplinary collaboration.
ConclusionTo overcome barriers for the implementation of CBT-I-based interventions in physical therapy practice, it is important to involve educational institutions, research bodies, policymakers, and patient representatives in crafting effective strategies. The study findings can guide strategy selection promoting the adoption of physical therapist-led CBT-I-based interventions for chronic pain and insomnia.
Chronic pain poses an enormous health and socioeconomic problem being the leading cause of years lived with disability globally, and a major reason for sick leave and early retirement.1 It is a multifactorial problem,2,3 often triggered and sustained by factors like insomnia.4–6 Clinical insomnia symptoms affects up to 73 % of individuals with chronic pain,6 leading to daytime fatigue, sleepiness, emotional disturbances, memory issues, difficulty concentrating, and reduced quality of life.7–10 Research indicates a bidirectional relationship between sleep and pain,4,11 with disturbed sleep predicting chronic pain onset and persistence.4,12–15 Several mechanisms have been proposed, including disruptions in neurotransmission (serotonin, dopamine, norepinephrine), altered opioidergic signalling, central pain modulation changes, increased inflammation, and psychological factors like depression and maladaptive beliefs.8,16–19 However, the underlying processes remain unclear.20 This complex interaction also impacts key factors essential for pain management, including physical activity, emotional well-being, and coping strategies, emphasizing the need for integrated interventions that target both pain and insomnia.21
Healthcare providers delivering evidence-based care to individuals with chronic pain are developing cognitive-behavioural skills essential for psychologically informed pain management.22–25 Cognitive and behavioural change is fundamental in physical therapy for promoting physical activity and lifestyle modifications.23 As physical therapy increasingly integrates psychologically informed practice,22,26,27 professionals are developing competencies to apply cognitive behavioural strategies effectively. These competencies align with Cognitive Behavioural Therapy (CBT) principles, which help individuals modify unhelpful thoughts and behaviours to enhance emotional well-being and promote healthier coping. Considering the shared mechanisms between pain and sleep disturbances, CBT-principles used in pain management, such as altering unhelpful thought patterns, modifying behaviours, and enhancing coping, could also be effectively applied to insomnia in individuals with chronic pain. With appropriate additional training, healthcare providers could adapt these principles to address insomnia in individuals with chronic pain28 and absence of complex psychiatric comorbidities.
International clinical practice guidelines recommend Cognitive Behaviour Therapy for Insomnia (CBT-I) as a first-line treatment due to its clinical and cost-effectiveness.29–31 CBT-I is a multicomponent therapy that modifies unhelpful beliefs and behaviours towards sleep and replaces them with helpful ones. It has shown long-term effectiveness in improving sleep compared to pharmacological treatments in various clinical populations, including those with chronic pain and insomnia.29,32 Furthermore, CBT-I-based interventions can be effectively delivered by various healthcare providers,33–38 including physical therapists.39 Access to CBT-I in primary care is problematic worldwide,40–42 often leaving insomnia unaddressed in individuals with chronic pain and insomnia. When addressed, sedative-hypnotics are often prescribed,40 which carry risks including dependency, drug interactions, and overdose deaths when combined with analgesics.43,44
Physical therapists are accessible to individuals with chronic pain, including those with comorbid insomnia. Despite CBT-I's proven benefits, integrating CBT-I-based interventions into physical therapy practice remains challenging. To promote effective adoption, methodologically rigorous implementation research is needed. This study identifies barriers and propose strategies for overcoming them, guided by the Implementation Research Logic Model (IRLM).45 By understanding and addressing these barriers, this study aims to enhance the translation of evidence supporting physical therapist-delivered CBT-I-based interventions into clinical settings for individuals with chronic pain and comorbid insomnia.
MethodsThis study was approved by the Social and Societal Ethics Committee, KU Leuven, with the reference number G-2022–5801-R2(MAR). The study’s findings from the focus groups were reported and written up following the guidelines provided by the Standards for Reporting Qualitative Research (SRQR)46 and the 32-item checklist from the Consolidated Criteria for Reporting Qualitative Studies (COREQ).47
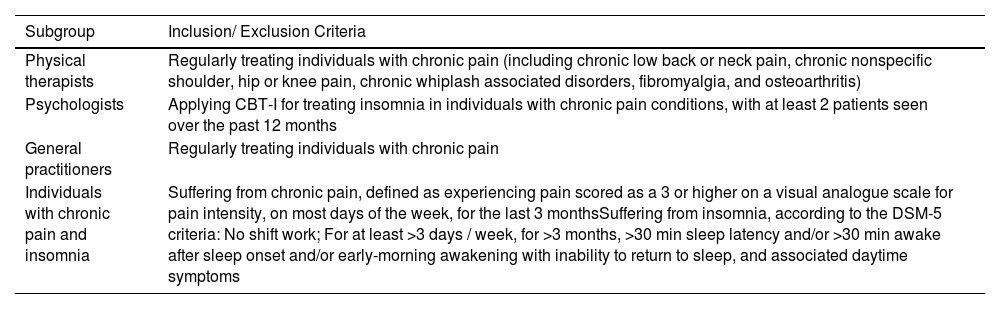
ParticipantsPurposeful sampling recruited a diverse group of stakeholders, including physical therapists, psychologists, general practitioners, and individuals with chronic pain and insomnia - based on predefined criteria (Table 1). The term stakeholder refers to both healthcare providers and patients, highlighting their shared role. Participants with and without CBT-I experience were recruited, and all participants were required to speak English fluently.
Inclusion and exclusion criteria for specific participant’s role.
CBT-I: cognitive behavioural therapy for insomnia.
Physical therapists, psychologists, general practitioners and individuals with chronic pain and insomnia were recruited between 1 and 31 January 2024. Recruitment occurred via flyers on social media and contacts with professional and patient organizations. Interested individuals received an email with study details, expected time commitment, and group discussion dates. They could contact the research team by email or phone for questions. After clarifications, those still interested received an informed consent form detailing recorded interviews, data protection, withdrawal rights, and a reimbursement of €60 per hour. All participants in the study signed the informed consent.
The implementation research logic modelThe IRLM45 is a tool to develop a logic model of an implementation intervention, with the aim of improving its efficacy (leading to improved implementation outcomes). It is principle-based and adaptable to the specific context of the intervention. The model links five core elements: (1) determinants; (2) clinical intervention; (3) implementation strategies; (4) mechanisms; and (5) outcomes.
- •
Determinants refer to the barriers and facilitators affecting clinical intervention adoption. This study used the Consolidated Framework for Implementation Research (CFIR)48 to identify them. CFIR divides barriers into five clusters: the intervention’s characteristics, inner and outer settings, involved individuals, and implementation process.
- •
Clinical intervention refers to any novel practice, approach, technique aimed at improving patient care. Here, CBT-I constituted the clinical intervention.
- •
Mechanisms explain why and how determinants influence intervention success or failure of intervention’s adoption.
- •
Implementation strategies are actions ensuring the clinical intervention’s adoption. Pre-selected implementation strategies from the Expert Recommendations for Implementing Change (ERIC)49,50 were adapted for the purpose of the study (Supplementary Material 1).
- •
Outcomes measure implementation success, including patient-related indicators (e.g., symptomatology, treatment satisfaction) and intervention sustainability.51
The components ‘mechanisms’ and ‘outcomes’ were beyond this study’s scope.
ProcedureParticipants were invited for 3 online semi-structured group interviews (focus groups) and 1 online questionnaire. Participants were divided in 4 teams, with each team conducting 3 interviews, to enable triangulation. A brochure about CBT-I was provided to participants lacking experience before the sessions (Supplementary Material 2).
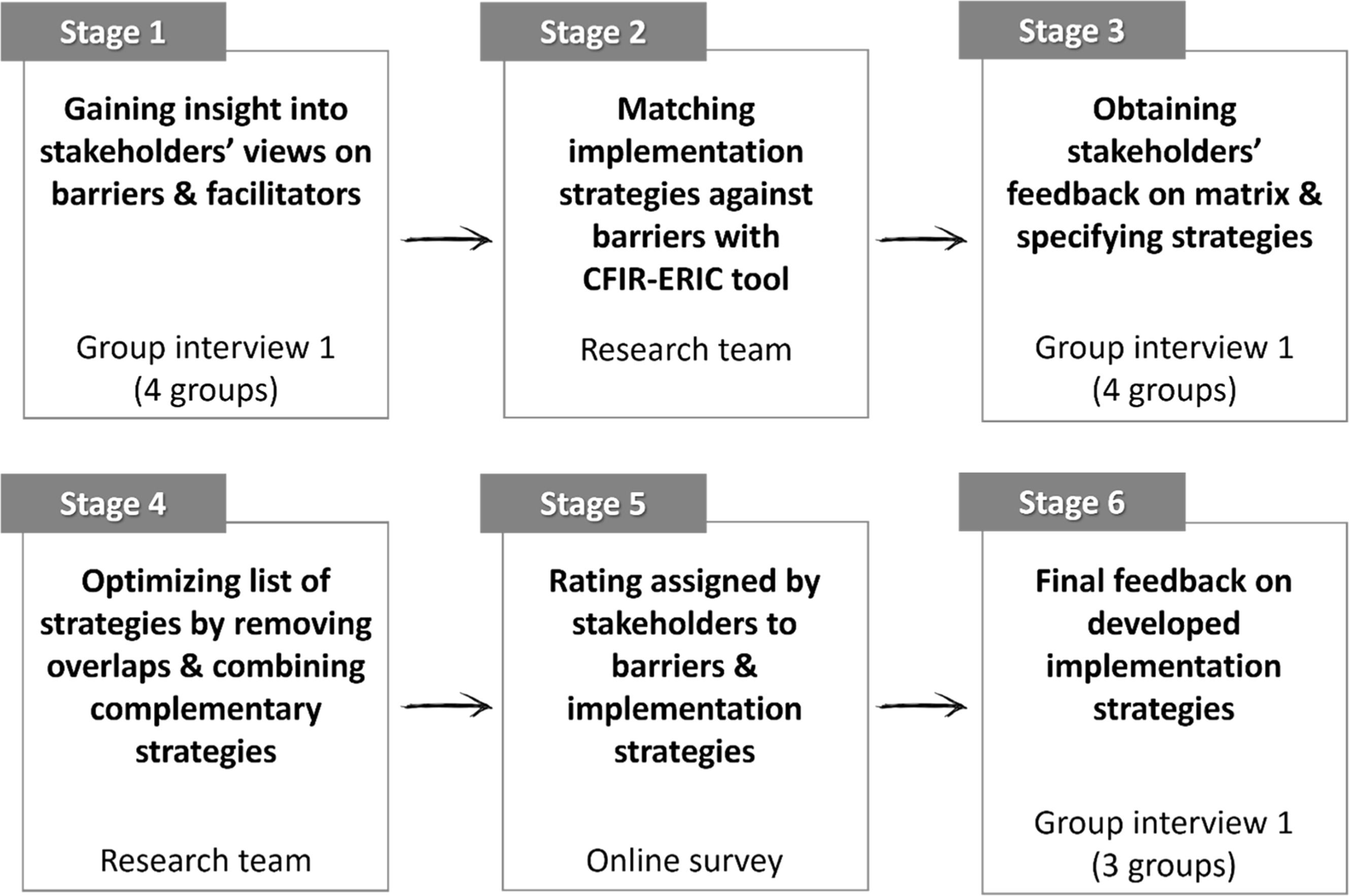
The seven-stage procedure developed by Knapp and colleagues52 to select implementation strategies was adapted to six stages. This procedure represents an integration of different approaches under the IRLM, resulting in a rigorous, iterative process to identify barriers and select strategies to address them. It incorporates user-centered design,53,54 a modified version of a Delphi approach,55 and the ERIC protocol.49,50 This procedure engaged stakeholders at multiple stages (i.e., identifying barriers, developing and fine-tuning implementation strategies, ranking the barriers and prioritizing the strategies) while allowing adaptation to evidence-based practice.53,54 It also provided multi-stage feedback opportunities, increasing the credibility of research findings.
- •
Stage 1 involved semi-structured group interviews with physical therapists, psychologists, general practitioners, and individuals with chronic pain and insomnia, to discuss the determinants of CBT-I implementation.
- •
Stage 2 was conducted by the research team, and involved mapping barriers with potential implementation strategies using the CFIR-ERIC tool, an online tool56 and consists of 73 strategies identified by the ERIC collaboration.57
- •
Stage 3 was a semi-structured group interview aimed to obtain the participants’ feedback on the map from stage 2 and elaborate on selected strategies. Elaboration involved defining and specifying strategies in terms of actor, action, dose, temporality, justification, and expected outcomes, following Proctor et al.58
- •
Stage 4 involved optimizing the map by merging and excluding overlapping strategies.
- •
Stage 5 prioritized strategies and barriers using an online survey via Qualtrics. The questionnaire had two sections: barriers and strategies. Barriers were rated on a four-point scale (1 = not important, 4 = very important). Strategies were assessed across three dimensions (importance, feasibility, and effectiveness) using a similar four-point scale. The top 10 strategies were selected based on their scores across all dimensions. Background information, such as professional discipline, was collected for subgroup analyses. The 10 highest-scoring strategies were selected among each group of stakeholders separately (i.e., among physical therapists, psychologists, general practitioners, and individuals with chronic pain and insomnia). Strategies that were in the top 10 for a specific group of stakeholders but not the general list were added. Finally, the top 10 barriers were reviewed to ensure a corresponding strategy was identified for each.
- •
Stage 6 occurred after preparing the final top 10 strategy list. In this stage, one more set of group interviews were conducted. Group interviews were used to fine-tune strategies, outline implementation challenges, and further prioritize strategies qualitatively.
Graphical representation of this stage-by-stage procedure is shown in Fig. 1. The developed guiding questions for the discussions of the first and third stages are provided in Supplementary Material 3. The group interviews were recorded so that researchers could resort to them for notetaking and transcribing.
Six-stage procedure, adopted from Knapp and colleagues52.
Online focus groups were conducted in English via Microsoft Teams between February till August 2023 by two interviewers (MM and TJ). MM holds a Master’s in Psychology, and TJ is a Postdoctoral Fellow in Health Psychology, both trained in qualitative data collection and implementation sciences. The interviewers had no prior connection with the participants. Video recordings were transcribed manually. The deductive Rapid Turnaround Qualitative Analysis method was used59 for fast, efficient, and structured data processing.60 This method offers comparable rigor to traditional qualitative analysis and is both time- and cost-efficient.61 Two researchers independently coded and analysed the data initially, resolving disagreements through discussion. After reaching consensus, one researcher (MM) completed the analysis, supervised by TJ, before results were shared with participants for validation.
ResultsParticipantsA panel of 16 stakeholders (8 physical therapists, 3 clinical psychologists, 2 general practitioners, and 3 individuals with chronic pain and insomnia) was included in the study. An overview of the participants’ characteristics is provided in Supplementary Material 4.
Regarding the group interviews in stages 1, 3, and 6, the first team included 1 physical therapist, 2 clinical psychologists, and 1 individual with chronic pain and comorbid insomnia. This team focused on the determinants related to patient-therapist interactions, inner settings, and the intervention itself. The second team consisted of 2 physical therapists and 2 general practitioners and focused on the determinants related to interactions between general practitioners and physical therapists, thus addressing barriers and facilitators related to inner and outer settings. The third team was composed of 2 physical therapists from Cyprus and Canada and 2 from Belgium and focused on the process of implementation. A fourth team, similar in composition and scope to the first, included a clinical psychologist, a physical therapist, and two individuals with chronic pain and comorbid insomnia, all from Belgium.
DropoutsOne physical therapist dropped out for undisclosed reasons after the second stage. Another physical therapist dropped out due to health issues after stage 5 and was therefore not at the final group interview (stage 6). There was one participant (physical therapist) who did not fill in the ranking stage (stage 5) due to maternity leave, but she was present in all three group interviews.
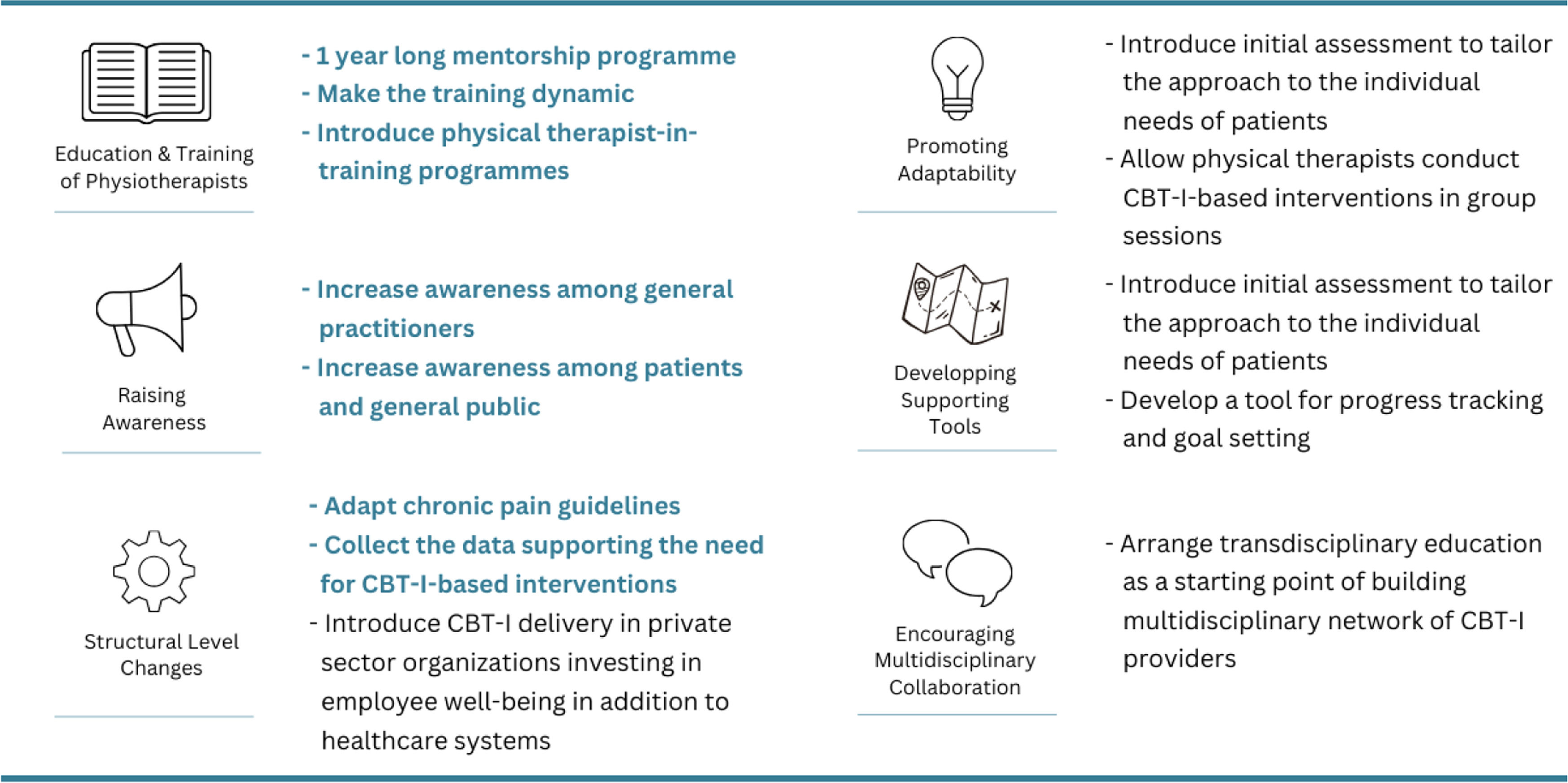
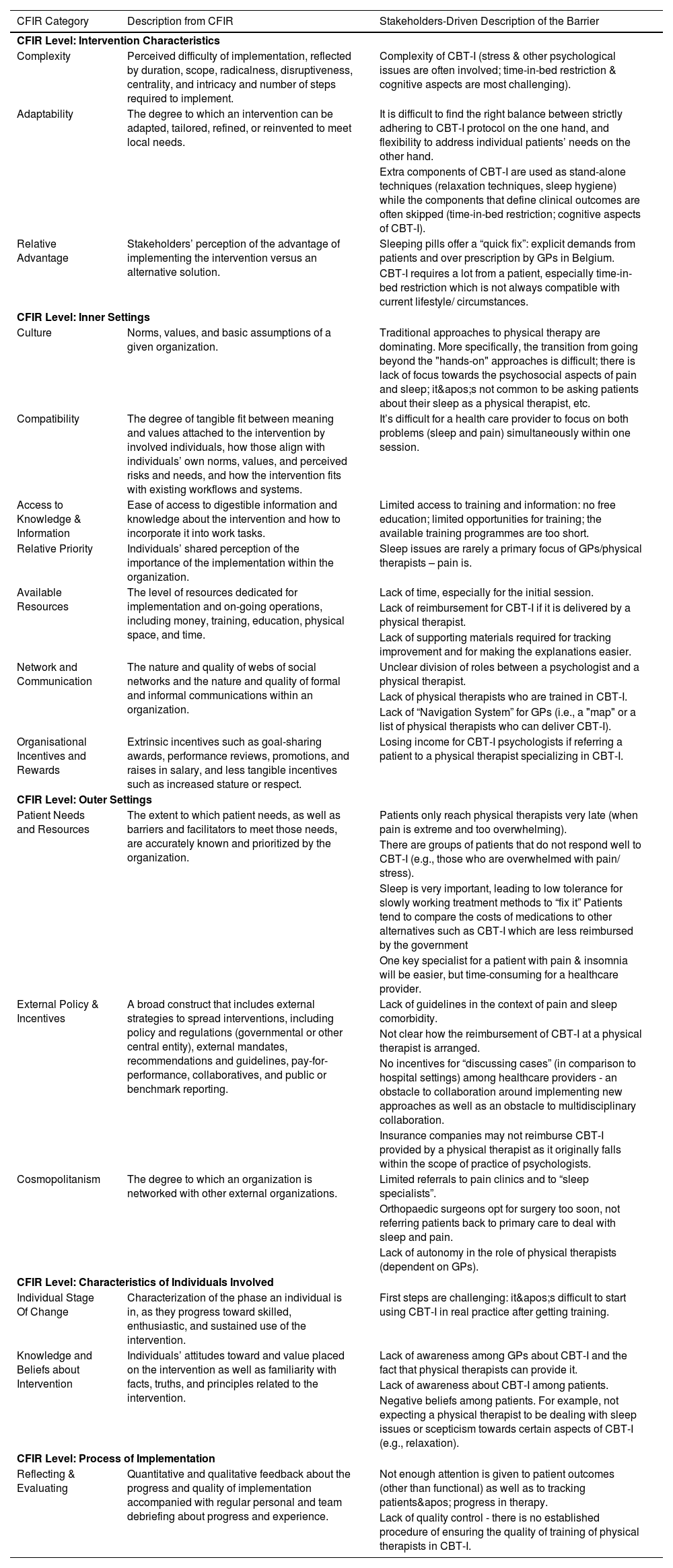
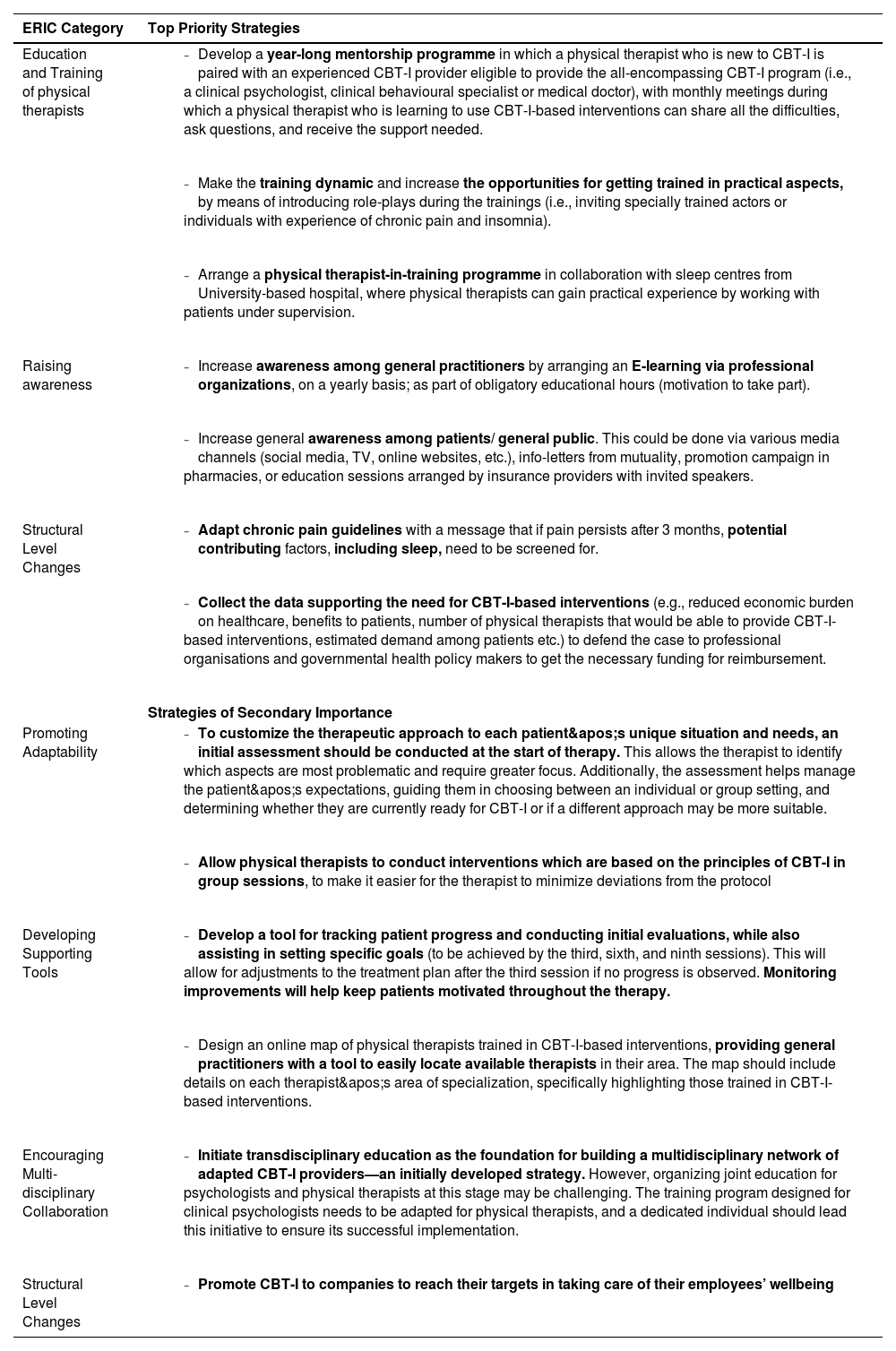
Results of the 6-stage procedureThirty-three barriers across all domains of CFIR framework (stage 1) and 21 strategies to address them (stages 2, 3, 4) were identified. Barriers identified in the first stage are described in Table 2. The detailed results of stages 2 to 4 are provided in Supplementary Materials 5 and 6. In stage 5, the list of 21 strategies was reduced to 13, based on the sum score on assigned feasibility, importance, and effectiveness derived from the online survey (Supplementary Material 7). The 13 strategies were fine-tuned during the final group interview (stage 6) and divided into first-priority and second-priority strategies. Strategies related to education and training of physical therapists, structural level changes and raising awareness among general practitioners and patients were designated as top priority. Strategies related to promoting adaptability of CBT-I, developing supportive tools, and encouraging multidisciplinary collaboration were assigned as second priority. A detailed outline of the 13 implementation strategies is provided in Table 3 and Fig. 2, and Supplementary Material 8.
Barriers identified in the first stage of this study with the split by levels of CFIR framework.
CFIR: Consolidated Framework for Implementation Research.
CBT-I: Cognitive behavioural therapy for insomnia.
GP: General practitioner.
The description of developed strategies and their priorities as defined in stage 6.
ERIC: Expert Recommendations for Implementing Change.
CBT-I: Cognitive behavioural therapy for insomnia.
In this study, a panel of 16 stakeholders identified 33 barriers for the implementation of CBT-I in routine physical therapy practice and formulated 13 implementation strategies to overcome these. Priorities belonging to ‘education and training of physical therapists’, ‘structural level changes’, and ‘raising awareness among general practitioners and the general population’ were assigned as top priority strategies.
Education and training of physical therapistsPhysical therapists are increasingly providing psychologically informed treatments. However, in our study, stakeholders identified adherence to the traditional biomedical model as a barrier to integrate sleep management into physical therapy practice. This was primarily due to a lack of confidence in addressing the psychosocial contributors to pain and limited knowledge about the impact of sleep on pain and vice versa. The literature already indicates that developing new attitudes and knowledge to shift from a disease-centered practice to a biopsychosocial focus is often insufficient among physical therapists.62,63 In parallel, although studies indicate that physical therapists recognize the importance of addressing sleep in patient care, research also reveals that they feel inadequately trained in sleep pathophysiology during their education.64–68 This highlights the need for enhanced educational initiatives that target the acquisition of skills and competences necessary to provide cognitive behavioural treatments69,70 as well as improving knowledge of sleep medicine.71
Extensive training, emphasizing hands-on experiences, collaborative interactions, and critical reflection, is essential for developing appropriate competencies and skills such as effective communication, shared-decision making, and behavioural change.72 One proposed implementation strategy for improving physical therapist education and training is a fellowship program where CBT-I experts mentor therapists who lack prior experience in CBT-I-based interventions. This approach aims to accelerate skill development, build confidence, promote evidence-based practice, and foster professional networking,73,74 which aligns with the recommendations of the European Academy for CBT-I.75 Yet, it should be in line with the local legislation regarding the practice of health professions. The stakeholders also emphasized the need for dynamic training methods such as role-playing, live demonstrations, reflection, feedback, and multisensory learning to enhance experiential learning.74,76 Finally, spacing out training sessions to allow time between the learning moments was proposed to facilitate the integration of newly acquired skills into practice.69
Structural level changesStakeholders underscored that sleep disturbances, when a comorbidity with chronic pain, are often deprioritized by policy regulations. Practice guidelines for integrating CBT-I-based principles into the management of individuals with chronic pain (for example Van Looveren et al., 202,228) are either rather inaccessible or lacking altogether.70 Also, the legal framework defining the role of physical therapists in delivering CBT-I-based interventions, along with financial incentives such as reimbursement, remains unclear for the stakeholders. Participants emphasized that time constraints pose a significant barrier for general practitioners to screen for sleep disorders in patients with chronic pain and for physical therapists to integrate CBT-I-based interventions within the limited available time during consultations.
To effectively advocate for the implementation of CBT-I-based interventions in physical therapy practice to policymakers and government agencies, robust trial data are needed to demonstrate the effectiveness and cost-efficiency of CBT-I-based interventions provided by physical therapists for individuals with chronic pain and comorbid insomnia. This is needed not only for sleep- and pain- related outcomes, but equally important for quality of life, physical activity, and psychological-related aspects. One high-quality trial is currently available, showing clinically relevant improvements in sleep quality in individuals with nonspecific chronic spinal pain and comorbid insomnia who received a physical therapist-delivered CBT-I-based intervention integrated within best evidence pain management as compared to pain management alone.39 Other studies, assessing the clinical as well as cost-effectiveness of a physical therapy-delivered CBT-I-based intervention integrated into pain management, are underway,77,78 and their results will further inform policymakers and government agencies. These findings should be interpreted cautiously, as randomized controlled trials evaluating the performance of specific healthcare professionals or interventions often have strict inclusion criteria that limit ecological validity. Trials typically include patients with limited psychiatric comorbidities, whereas real-world patients often have more complex psychiatric issues. There is insufficient evidence suggesting these can be managed effectively without additional involvement or guidance of mental health professionals. Recognizing these limits could lead to improved regulatory measures for reimbursement and a clearer definition of the physical therapist’s role in sleep management, increasing their confidence in providing CBT-I interventions.
Raising awareness among general practitioners and the general populationIn accordance with previous studies,79,80 participants noted that sleep is rarely a primary focus for patients, general practitioners, and physical therapists, as pain often takes precedence. This can lead to patients with chronic pain and insomnia not discussing their sleep disturbances during consultations or clinicians not assessing sleep.
Overprescription of sleeping medications by general practitioners is another significant barrier to implementing CBT-I in primary care. Patients might prefer rapid results and therefore choose medication instead of behavioural change approaches.81,82 General practitioners may incorrectly assume that patients will not accept non-pharmacological behavioural approaches and that patients expect a quick fix through medication.83 Additionally, general practitioners often lack awareness about CBT-I approaches and the role that physical therapists can play in the integration of CBT-I principles for individuals with chronic pain and comorbid insomnia. This is consistent with other studies reporting ‘unfamiliarity of general practitioners with CBT-I’ as a barrier for implementing CBT-I as first line treatment.84 For example, a survey of Belgian general practitioners found that only 35 % fully agreed their knowledge of non-pharmacologic approach for insomnia was sufficient.80
By changing attitudes and beliefs about managing insomnia and increasing knowledge of patients and clinicians about the content, use, modalities, access, effectiveness, cost-efficiency but also limits of CBT-I-based interventions for individuals with chronic pain, the barrier to refer to or to be referred for non-pharmacological management will decrease. Disseminating this information to patients, healthcare professionals, institutions, and the general population is crucial to improve access to CBT-I for individuals with chronic pain and clinical insomnia. Lastly, the strength of the combined use of CBT-I-based interventions by various healthcare providers within transdisciplinary collaboration will enable a cohesive approach to addressing the multidimensional aspects of a patient’s condition, ultimately leading to more personalized and effective care outcomes. A stepped care approach, starting with low-intensity treatments like sleep education and behaviour change, can address sleep difficulties, while more intensive CBT-I can be introduced to address higher levels of clinical complexity.85,86 This model improves access to care, especially where CBT-I specialists are scarce, and gives allied healthcare professionals, like physical therapists, a key role in managing insomnia in individuals with chronic pain.
Strengths and limitationsThe use of advanced implementation research methods to identify barriers and develop strategies for integrating CBT-I-based interventions into physical therapy practice. The stakeholder’s feedback at multiple stages refined findings, ensuring relevance for clinicians and patients applying CBT-I interventions in primary care. Additionally, the diverse stakeholder participation provided valuable insights into barriers from multiple perspectives.87 Involvement of physical therapists from countries with advanced CBT-I implementation enriched local perspectives, leading to contextually adaptable strategies. While our study focuses on insomnia, physical therapists may also contribute to managing other sleep disorders, such as sleep apnea or sleep bruxism, in individuals with chronic pain.88–91 Future research could explore this broader role. Although conducted in Belgium, the findings are likely transferable to other healthcare settings. The study primarily involved primary care providers but may not fully capture challenges in private or secondary care. Triangulation mitigated researcher bias, and the group interview format enhanced data richness and validity by fostering participant interaction. Moderation ensured equal contributions from all participants, reducing response bias. While online settings may limit non-verbal cues, they enhanced accessibility and reduced participant burden.
ConclusionThis study led to the identification of 13 strategies to address barriers to implementing CBT-I-based interventions within the domain of physical therapy. The top priority strategies focused on education and training of physical therapists, structural changes and raising awareness among general practitioners and the general population. While this approach is innovative, it also presents certain opportunities and challenges related to transdisciplinary care, which should be taken into consideration while adopting it in further implementation studies.
Declaration of generative AI and AI assisted technologies in the writing processChatGPT was used during the preparation of this work to correct grammatical errors, check language, and refine writing. After using this tool, the authors reviewed and edited the content as needed and take full responsibilities for the content of the publication.
Several authors contribute to research on sleep interventions targeting patients with chronic pain, with financial support for their institutions provided by various organizations, among them the Research Foundation Flanders (FWO). Furthermore, Jo Nijs and Vrije Universiteit Brussel have been compensated for delivering lectures and educational activities by multiple professional and educational organizations.
The authors thank the 16 stakeholders for their time and insights during the focus groups, and Ms. Marleen Corremans (EBMPracticeNet vzw) for her guidance and assistance. This work was published with the support of the University Foundation of Belgium and funded by grants from the Applied Biomedical Research Program, Research Foundation Flanders (Fonds voor Wetenschappelijk Onderzoek Vlaanderen), Belgium (FWO-TBM project No TBM2021 - T000521N - 54252, “Towards PREcision MEdicine for Osteoarthritis: Added value of cognitive behavioural therapy for insomnia (the PREMEO trial)”). It is furthermore supported by the Strategic Research Program SRP90 (“Pain Never Sleeps: Unravelling the Sleep-Pain Interaction in Patients with Chronic Pain”) funded by the Research Council of the Vrije Universiteit Brussel, Brussels, Belgium.