Physical therapist-led treatment programs are recommended for patients with femoroacetabular impingement (FAI) syndrome. Views of people with FAI syndrome regarding such interventions are currently unknown, including perceptions of potential barriers and facilitators to participation and adherence to exercise programs.
ObjectivesTo explore participant perceptions of physical therapist-led programs for FAI syndrome, including barriers and facilitators for accessing physical therapy, and adhering to a rehabilitation program.
MethodsOur qualitative study used semi-structured interviews to explore the perceptions of patients with FAI syndrome undertaking physical therapy-led treatment, where treatment was ceased due to Coronavirus Disease 2019 (COVID-19). The interview topic guide was informed by the Theoretical Domain Framework. Interviews were transcribed verbatim and data categories were developed using inductive thematic analysis. Themes were discussed between researchers until consensus was reached.
ResultsFourteen participants (mean age: 30 years) with a range of physical activity backgrounds undertook interviews. We identified four key themes, 1) Patients believed their hip pain was caused by structural damage worsened through exercise; 2) Barriers and facilitators on the feasibility of physical therapist-led programs; 3) Participants held beliefs regarding the importance of adjunct treatments to exercise; and 4) Impact of FAI syndrome on physical activity participation.
ConclusionPeople with FAI syndrome believe they have structural damage which leads to their hip pain and are often afraid to exercise due to fear of causing more damage to their hip. Our findings suggest that people with FAI syndrome want clear education about exercise, imaging, and expectations of cost and duration of treatment.
Hip pain is a major cause of disability, significantly impacting quality of life, function, work capacity, and family life.1 It is commonly experienced by young to middle-aged adults (18–50 years), with the psychological and physical impact occurring at a time when major work and life responsibilities are experienced.1–4 High economic burden from hip pain is currently experienced worldwide, with this projected to increase exponentially over the next three decades.5,6 Surgical intervention is common in this population,7 while quality of life and function remain low for these patients following surgery.1,2,8 Understanding differing classifications of hip pain might assist in the development of effective interventions that reduce the burden of this condition.
The International Hip Pain Research Network consensus meeting recommended that hip pain in young and middle-aged adults be classified as either femoroacetabular impingement (FAI) syndrome, acetabular dysplasia/hip instability, or other pathologies with normal hip morphology.9,10 Of these, FAI syndrome is the most common cause of hip pain in young adults, with hip osteoarthritis (OA) a potential sequalae. People with FAI syndrome also have pain, poor quality of life, physical impairments including reduced hip and trunk muscle strength, and reduced functional task performance.9,11,12 Treatment for FAI syndrome include surgical and non-surgical options, such as physical therapist-led interventions. In recent years, arthroscopic surgery has become an increasingly common treatment of FAI syndrome. However, this type of surgery is associated with significant cost,13 inherent risks,14 potential risk to cartilage health,15 and its longer-term efficacy is uncertain.16 A greater understanding of alternative treatments to surgery is needed.
The term “Physical therapist-led intervention” is broad, and may include aspects such as exercise therapy, education, manual therapy, and other therapies. These interventions may preserve the joint,15 and are recommended as an effective, low risk, and cost-saving alternative to surgery to reduce the symptoms of FAI syndrome in active individuals, although the ideal design of programs is unclear.17 A recent qualitative study determined that people with persistent hip pain tended to avoid physical activity as they believed their condition was exercise-induced.18 Recent consensus recommendations outlined physical therapist-led treatment as a critical part of management for FAI syndrome and consist of primarily exercise-therapy for at least 3 months duration,17 but can take up to 6 months.19 The onset of Coronavirus Disease 2019 (COVID-19) meant that physical therapy treatment ceased around the world, providing an opportunity to reflect on past practices, and explore new technologies that might enable contactless physical therapist-led treatment options for patients. Understanding the perspectives of the end-users is of utmost importance to ensure successful implementation. However, no studies have investigated patient understanding of physical therapist-led treatment, outcomes expected following participation, or their perceived barriers to participation.
The objectives of our study were to explore patient perceptions of physical therapist-led programs for FAI syndrome, including barriers and facilitators for accessing physical therapy; adhering to a rehabilitation program, and the impact of FAI syndrome on physical activity.
MethodsStudy designThis qualitative study conducted semi-structured interviews with people taking part in the PhysioFIRST study for people with FAI syndrome.19 Ethics approval was obtained from La Trobe University Human Research Ethics Committee (#HEC17080) in compliance with the Helsinki declaration. The reporting of the study was undertaken according to the COnsolidated criteria for REporting Qualitative research (COREQ-32) criteria.20 Inception of this study was derived as a means of continuing to engage participants who had received minimal physical therapy intervention at the onset of the COVID-19 lockdown in Melbourne beginning in March 2020. This study did not alter the delivery of the intervention within the PhysioFIRST study, as the PhysioFIRST study was suspended while the current study was being conducted.
ParticipantsAll participants provided written informed consent prior to the study and were reminded of their rights prior to their interview. All participants were adults aged 18–50 years, males and females, recruited from the existing PhysioFIRST study cohort.19 Prior to the onset of COVID-19 restrictions, participants in this RCT had consented and just begun to undertake a physical therapist-led exercise program and education.
Full details of the exercise components of the two study arms are described in the published protocol paper as well as details of the cohort, recruitment procedures, and inclusion and exclusion criteria.19 A brief description is outlined below.
Inclusion criteriaDetails of inclusion into the physioFIRST study have been reported previously.19 Briefly, adults with i) activity-related hip and/or groin pain for more than 6 weeks, ii) a positive Flexion-Adduction-Internal Rotation (FADIR) test,9 and iii) indication of cam morphology, defined by an alpha angle greater than 60° on a supine anteroposterior pelvic or Dunn 45° radiograph were considered eligible.9,21
Recruitment proceduresThe initial COVID-19 lockdown occurred in Melbourne, Victoria between March and June 2020. Government regulated closure of gymnasiums and restriction of access to allied health services significantly impacted the PhysioFIRST trial participants. All participants in this study were individuals whose participation in the PhysioFIRST study was suspended due to these restrictions, whereby participation aimed to maintain engagement of participants during the lockdown and improve delivery of future physical therapist-led programs. They were receiving no active physical therapy at the time of the study. They were contacted by email in April 2020 and invited to participate in this qualitative study. Interviews were conducted in May 2020 via the Zoom platform during the COVID-19 lockdown.
Data collectionThe topic guide (Supplementary material) for the interview questions was developed by four authors (EB, AM, CB, JK) based on the Theoretical Domain Framework22 and included questions relating to knowledge, skills, identity, beliefs, and goals. Interview schedules were developed in consultation with an experienced qualitative researcher (CB) and experienced FAI syndrome clinicians and researchers (JK and AM). The authors have a range of 4–28 years of clinical experience treating patients with hip pain. Semi-structured interviews allowed us to explore key themes related to people with FAI syndrome and allowed flexibility for participants to discuss what they felt was important to them in relation to FAI syndrome.
Demographic data including age, sex, body mass index (BMI), duration of symptoms (months) and International Hip Outcome Tool (iHOT-33)23,24 were collected to characterise the cohort. The iHOT-33 is a recommended measure of hip-related quality of life in young adults with hip pain and is scored from 0 to 100, where 100 is the best possible score.23,24
Interviews utilised open-ended questions and were conducted via Zoom by a female physical therapist (EB) with previous qualitative study experience25,26 and no prior relationship with any study participants. Interviews were audio recorded, no repeat interviews were conducted, and field notes were not collected. To facilitate ongoing engagement with the physioFIRST trial at the onset of the COVID-19 lockdown in Melbourne, Australia, we included all eligible participants who consented.
Data analysisFrom an epistemological perspective, the approach used during the interviews was interpretive/constructive, because the study aimed to gather information from the perspective of the interviewed participants. The interview questions were open ended with no right or wrong answer but provided a framework for the descriptive process. Interviews were transcribed verbatim by an experienced research assistant at La Trobe University and imported into the NVivo qualitative data analysis software (QSR International Pty Ltd, Melbourne, Australia, Version 12, 2020). Participants were provided with their interview transcript immediately following transcription and given the opportunity to elaborate on statements made in their interview. No participants made amendments. Qualitative analysis of the interview data commenced with a close review of each transcript by one researcher (EB) to gain familiarisation with the dataset. Relativism was the ontological philosophical approach which guided the coding such that the responses of the participants created the constructs and developed the themes for the analysis.
Data analysis followed reflexive thematic analysis,27 which included i) a code being assigned to each key issue, ii) similar codes were grouped and findings were identified as subthemes, and iii) subthemes were grouped to form overarching themes. All transcripts contributed to the final themes identified, themes were not predetermined. As data saturation is not aligned with reflexive thematic analysis,28 we did not seek data saturation. To ensure data accuracy, a random sample of 50 % of transcripts were also coded independently by a second researcher (AM). Generation of initial themes took place between researchers (EB, AM, CB, JK). Themes evolved during four online meetings every two weeks, to ensure a deep, nuanced understanding of the data.
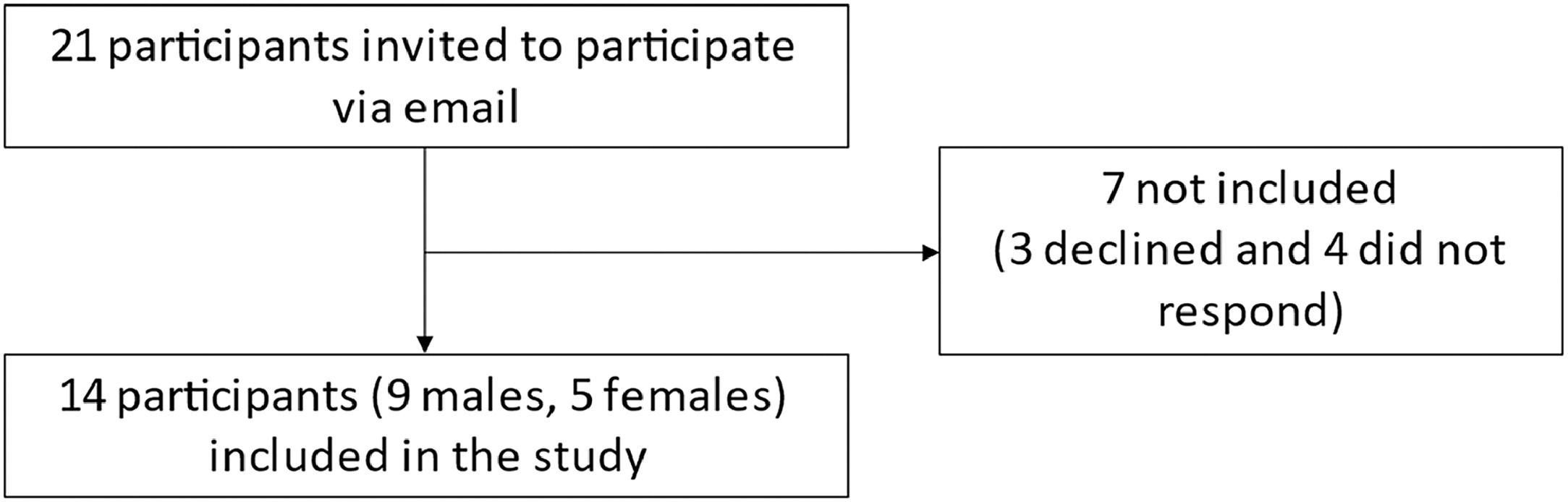
ResultsTwenty-one participants were invited to participate in this study via email. Fourteen participants responded to the invitation and agreed to take part in the study, three declined and four did not respond (Fig. 1). Interviews were conducted and analysed for all 14 respondents (9 males and 5 females). Interviews lasted an average of 19 min (range 12–31). Participants interviewed had a mean age of (standard deviation) 30 (10) years of age, BMI of 23.2 (3.5) kg/m2, and 51 (43) months of symptoms. Participants had been undertaking the PhysioFIRST exercise protocol for a mean of two weeks (2), and the mean baseline iHOT-33 score for this cohort was 55.4 (18.9).
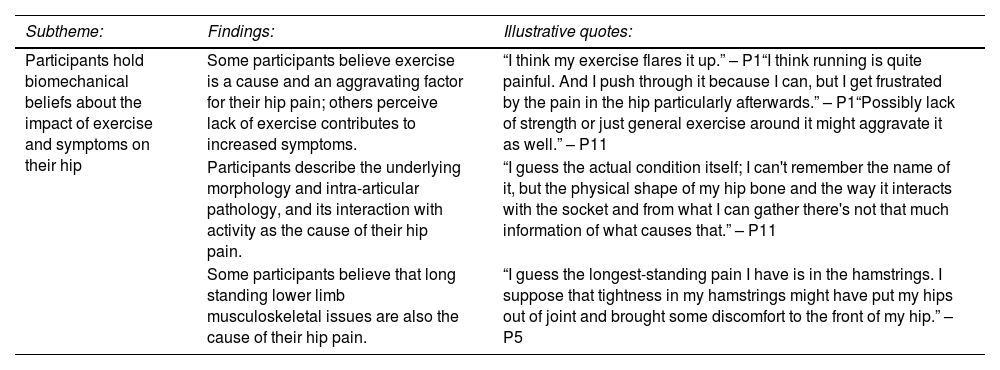
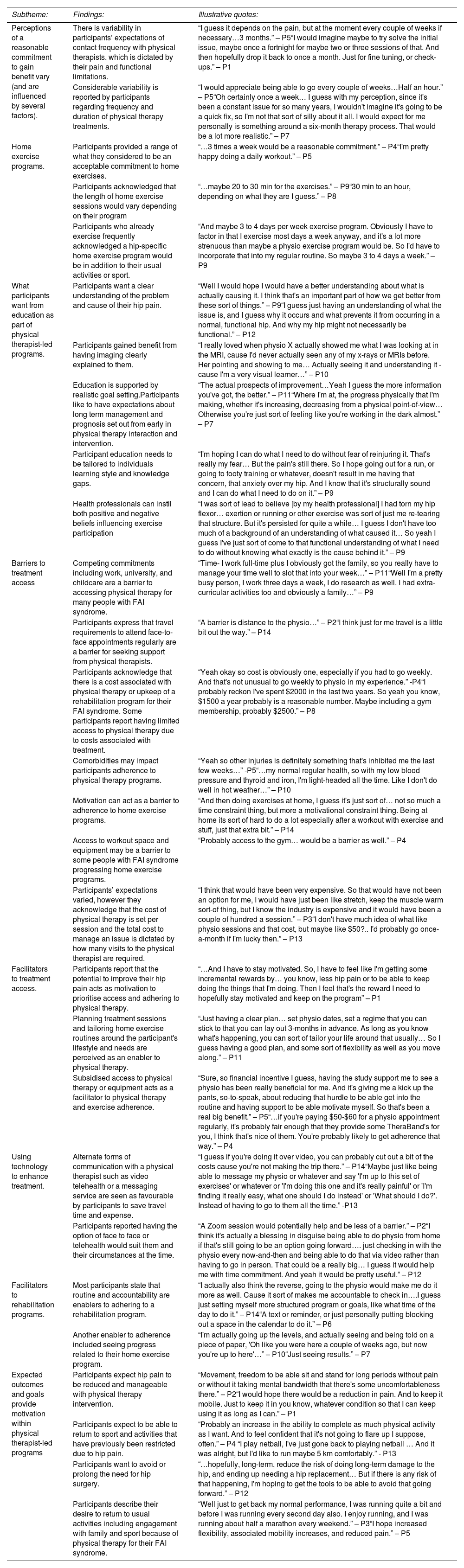
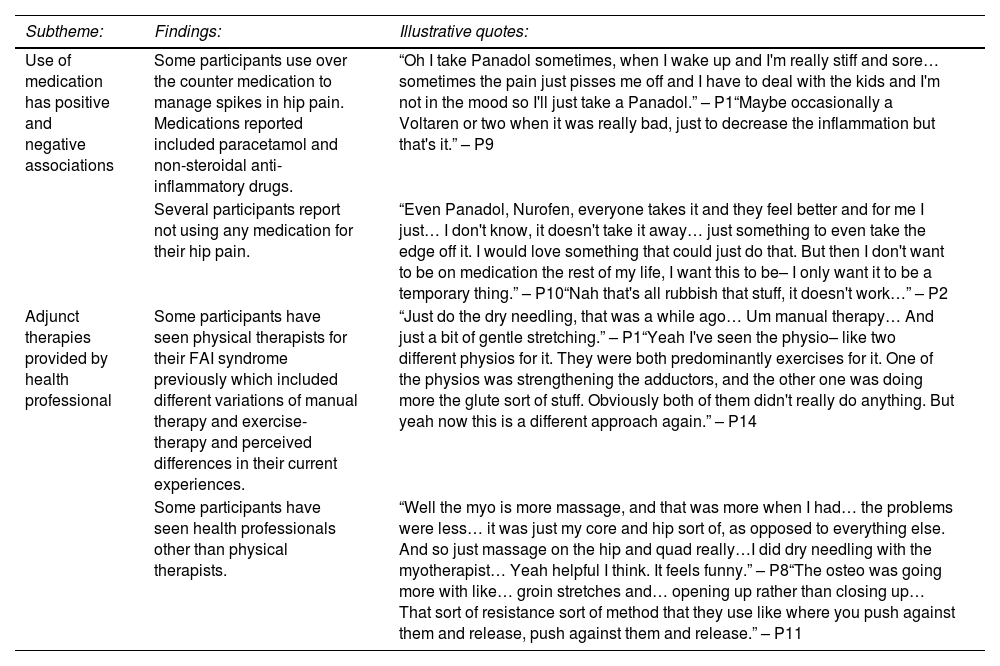
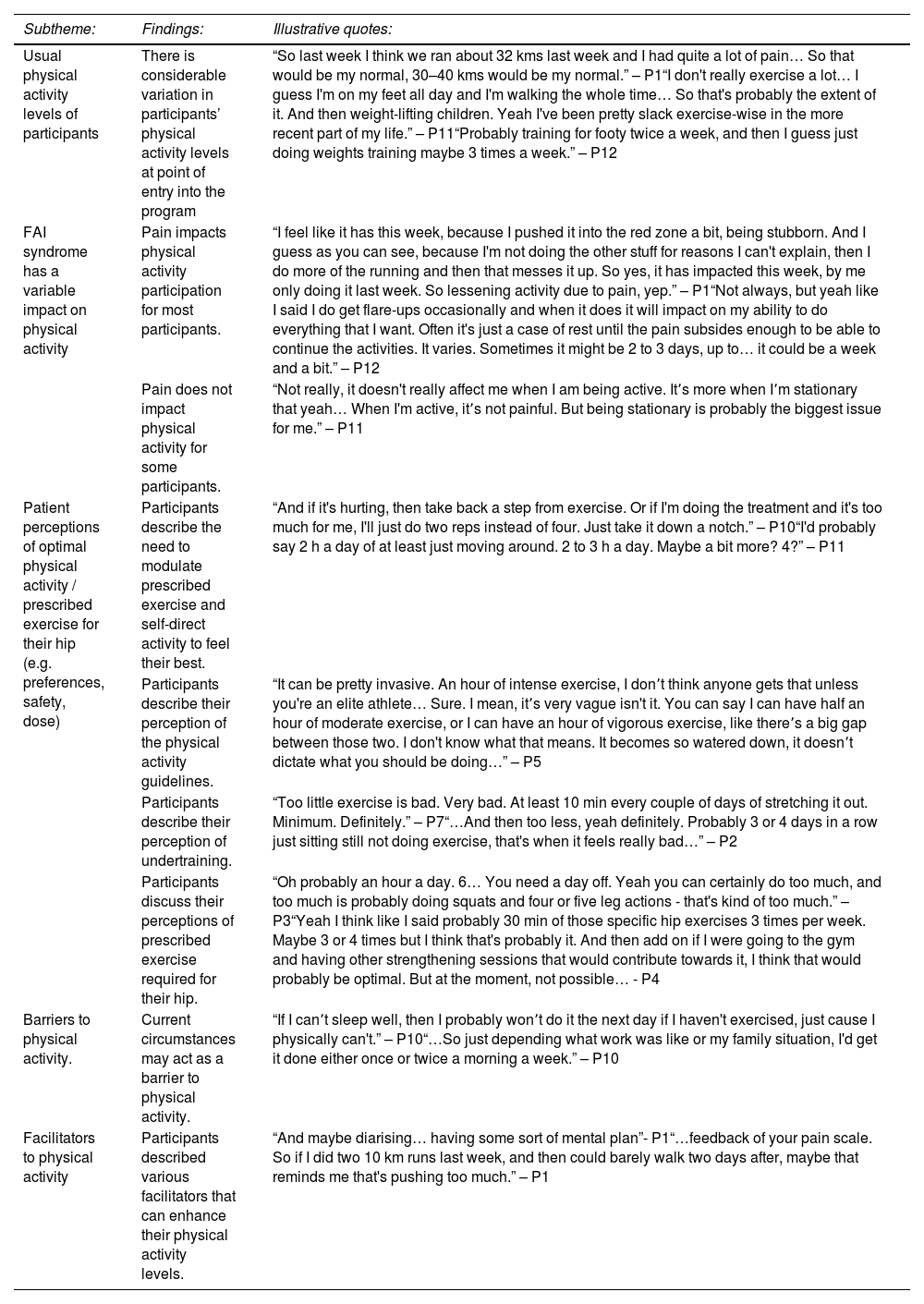
Summary of themesFour themes were identified from interviews. 1) Patients believed that their hip pain was caused by structural damage and worsened through exercise (Table 1). 2) Barriers and facilitators on the feasibility of physical therapist-led programs (Table 2); 3) Participants held beliefs regarding the importance of adjunct treatments to exercise (Table 3); and 4) Impact of FAI syndrome on physical activity participation (Table 4). Within each theme a number of subthemes emerged, providing a more detailed and nuanced understanding of participants’ perceptions of physical therapist-led programs for FAI syndrome, barriers and facilitators that exist for accessing physical therapy, and challenges and successes for adhering to a rehabilitation program.
Patients believed their hip pain was caused by structural damage and worsened through exercise.
Barriers and facilitators on the feasibility of physical therapist-led programs.
Participants held beliefs regarding the importance of adjunct treatments to exercise.
Impact of FAI syndrome on physical activity participation.
An association between undertaking exercise and provoking symptoms was identified, with some participants suggesting that a lack of exercise had the potential to exacerbate symptoms. In contrast, strong biomechanical beliefs about the impact of exercise on hip pain were voiced, with other participants believing that exercise may damage their hip and worsen symptoms (Table 1). Influence from health professionals may lead to positive or negative beliefs about the safety and benefits of exercise. Interpretation of imaging findings further enhanced belief in the ‘cause and effect’ biomechanical model.
Theme 2: barriers and facilitators on the feasibility of physical therapist-led programs (Table 2)Variability in perceptions of a feasible and reasonable commitment to a physical therapy-led program was a key finding, influenced by several factors. Commonly, participants thought physical therapist-led programs should include more frequent physical therapist contact during initial rehabilitation. Expectations for the duration of physical therapy sessions were influenced by participants prior experience and were less than one hour. Greater differences were evident in relation to home exercise programs, potentially reflective of the range of physical activity undertaken by participants outside the parameters of the physical therapist-led program. An acceptable duration for home exercise sessions ranged between 20 min and 1 h, with a handful of participants suggesting that combining their rehabilitation exercises with their usual routine may facilitate adherence.
Education provided by a physical therapist contributed to participant's expectations of management and prognosis and provided reassurance. Participants suggested that appealing to different learning types (e.g. audio, visual, tactile) would facilitate understanding. Barriers to physical therapist-led programs included opportunity (competing commitments), perceived lack of time, access (requirement for travel, access to equipment/space), cost, and motivation. While facilitators included use of technology assisting to address opportunity and access barriers, improvements seen from participation in physical therapist-led programs, motivation to prolong or prevent the need for surgical intervention, and motivation to return to usual activities.
Diversity in the delivery of components of a physical therapy-led program were valued, with technology and telehealth enhancing opportunities for education, motivation, reassurance, and minimisation of cost. Expected outcomes of physical therapist-led programs for FAI syndrome included reduced pain and symptoms, the ability to return to activities of daily living and sport (if applicable), as well as the potential to delay or eliminate the need for surgical intervention. The likelihood of meeting expectations and joint goal setting impacts feasibility of physical therapist-led programs as people with FAI are more likely to engage in programs that meet their expectations. Facilitators for treatment access included motivational factors such as ability to reduce hip pain. Subsidised cost of physical therapy and access to equipment increased the likelihood of participating in physical therapy treatment, and increased exercise adherence. Facilitators to rehabilitation programs included accountability through supervised exercise and seeing progress towards their goals. Routine was perceived as a facilitator to rehabilitation programs and physical activity participation.
Having the choice of face-to-face treatment or telehealth was perceived as a facilitator to accessing physical therapy, allowing participants to choose what catered best to their individual needs.
Theme 3: participants held beliefs regarding the importance of adjunct treatments to exercise (Table 3)Participants engaged in additional treatments including; medications and adjunct therapies. Perceived effect of over-the-counter medications such as paracetamol and ibuprofen varied. Some participants described self-dosing as they felt it was necessary, while others described choosing not to use them with the belief that they don't help their hip pain.
Adjunct therapies participants described having tried included dry needling, massage therapy, and stretching. No participants mentioned previous visits to general practitioners or orthopaedic surgeons when asked if they had seen other health professionals for their FAI syndrome.
Theme 4: impact of FAI syndrome on physical activity participation (Table 4)Participants reported dramatically contrasting levels of usual physical activity, ranging from minimal activity aside from occupational activity; to running more than 30 kms per week. Perceived optimal physical activity levels depended on the individual participant's lifestyles and pain levels. Some participants described the need to gradually build the strength and exercise tolerance with graded programs. Participants cited perceived risks of over- or under-exercising, with varied perceptions of what was an appropriate level of physical activity or exercise. Barriers to physical activity included individual circumstances such as work commitments or poor sleep. Facilitators included routine, accountability (e.g. diary), and pain tracking.
DiscussionWe explored the beliefs of people with FAI syndrome who had just commenced a physical therapist-led treatment program. Specifically, we sought to understand patient perceptions of physical therapist-led treatment for FAI syndrome, including barriers and facilitators for accessing physical therapy, adhering to a rehabilitation program, and the impact of FAI syndrome on physical activity. Interestingly, our findings are similar to qualitative studies of people with shoulder, low back, and knee pain, which imply that clinicians should be aware of the large psychosocial impact of musculoskeletal pain and the positive and negative influences that clinicians can have, supporting the need for patient-informed treatments for FAI syndrome.29–31
All participants held strongly to a biomedical model of pain, believing that their hip pain was related to bony morphology and intra-articular soft tissue pathology reported in imaging, and that exercise would damage already-damaged hip joint structures further. These beliefs are consistent with an older cohort of people with hip pain who had been referred to an orthopaedic surgeon.18 The expressed belief in the biomedical model of pain is likely to have influenced the barriers to exercise identified in Themes 2 and 4, suggesting an intersection of these themes, and a strong need for education in these patients. Substantial evidence indicates that the relationship of hip pain with hip joint morphology and pathology is poor. A recent systematic review indicates the prevalence of labral tears in symptomatic individuals is higher (62 %; 95 % CI: 47 %, 75 %), and similar to those without symptoms (54 %; 95 % CI: 41 %, 66 %).32 Additionally, while cam morphology typically seen in FAI syndrome appears to be more common in people with symptoms compared to those without (49% vs 23 %),33 prevalence in athletes is high at approximately two-thirds regardless of symptoms.34–36 People with FAI syndrome should be informed of the uncertain relationship between hip pain and structure, and be given the opportunity to discuss this relationship with their treating clinician.
Interestingly, our participants’ identified that they expect pain to be reduced following exercise intervention (Theme 2) but also that pain was a barrier to performing physical activity (Theme 4) Contrary to popular belief that exercise worsens hip pain, exercise-based treatment is recommended as a key intervention for young and middle-aged adults with FAI syndrome.17 Current evidence demonstrates that exercise-therapy improves pain and function with moderate effect,16 and may preserve the joint.15,16 Our findings suggest that the sports medicine community needs to work hard to change commonly held negative beliefs about the relationship between exercise and joint health in people with FAI syndrome. Education elements (e.g. audio, visual, tactile) within physical therapist-led programs for FAI syndrome need to inform patients of the benefits of exercise-therapy for pain and function, and that activity such as running may actually protect the joint against deterioration in joint structure, as recently reported in relation to knee joint health.37,38 Physical therapists should also consider exploring with patients why they maintain beliefs about the danger of exercise, and ensure that education is tailored to address individual patient's beliefs.
Several non-surgical treatment options were perceived as helpful in conjunction with exercise. Participants described a willingness to use over the counter medication to reduce pain and facilitate greater physical activity participation. In people with hip OA, non-steroidal anti-inflammatory medications have greater benefits than paracetamol, but also have a higher risk profile.39 Clinicians should consider encouraging patients to consult their general practitioner about safe and effective use of over-the-counter medication. Several participants reported seeing clinicians for other therapies such as massage, dry needling, and stretching. Patients perceived varied levels of benefit from adjunct therapies. To date, there is no evidence whether these adjunct therapies provide additional benefit over exercise-therapy for patients with FAI syndrome.17 Interestingly, a recent study of people with hip OA found that while both exercise therapy and manual therapy were cost effective compared to usual care provided by a general practitioner, the cost effectiveness was superior in the exercise therapy group and only exercise therapy proved to be clinically effective.40 While these findings have not yet been confirmed in younger people with FAI syndrome, they suggest that clinicians should consider treatments such as manual therapy as adjuncts only, and should not be prioritised over exercise-based treatments.17
Although the participants in this study represented a wide range of activity involvement, some demonstrated a hesitancy to undertake physical activity due to fear of creating more damage, while others were more confident to push into pain. This finding supports recently published work where an older group of patients (mean age 51 years) with hip pain who had been referred to an orthopaedic surgeon were also afraid of exercise and its effect on joint damage.18 The World Health Organisation's 2020 guidelines for physical activity stated that all adults should undertake 150–300 min of moderate-intensity, or 75–150 min of vigorous-intensity physical activity each week, as well as regular muscle strengthening activities.41 It is imperative that physical therapists ensure that patients with FAI syndrome are working towards this goal.42 Reassurance and education is essential17 to guide patients that moderate amounts of targeted and guided physical activity and exercise do not cause joint damage, instead they may help maintain a healthy joint as tissues respond to load.15,37,43 Physical therapists should also adapt exercise programs to suit the individual patient's preferences, which may include a graded approach to the resumption of activity to help overcome patients’ fears.19
In summary, tips for physiotherapists to use when designing rehabilitation programs for patients with FAI syndrome include (i) providing clear education about the benefits of exercise and physical activity, and the poor relationship between structure and symptoms; (ii) inform patients of the costs and duration of treatment required, and the commitment to exercise required (2–3 times/week for at least 3 months); (iii) embrace technologies such as exercise apps and telehealth appointments; (iv) make sure patients have access to equipment needed for rehabilitation; (v) make sure return to sport and physical activities are prioritised; (vi) consider using adjunctive therapies and referring for simple analgesia
Strengths and limitationsOur study has several strengths and limitations that should be highlighted. Our study includes a somewhat diverse population of people with FAI syndrome, including a large variation in symptom duration which may have contributed to varied perspectives and experiences. We included 14 participants which might be considered a smallish sample for qualitative research. We used Zoom to conduct and record the qualitative interviews. It is possible that participants may have provided different responses if the interviews were conducted via telephone call or in person. We used a Theoretical Domain Framework approach and reported our findings according to the COREQ-32 criteria. The population we recruited responded to advertising to participate in a clinical trial of physical therapy for FAI syndrome, meaning that they might have preferred not to undergo surgery, and may be more enthusiastic towards physical therapist-led treatment and exercise therapy. Our cohort was more likely to perceive prolonged physical therapist-led treatment as acceptable compared to people who are seeking a fast solution. Lastly, and possibly most importantly, we only included white patients from a large metropolitan area in a high-income country. The findings of our study and recommendations made may not be appropriate or possible for people living with FAI syndrome who are less well-resourced. A recent systematic review showed that physical therapy is most likely to be accessed by people who are white, well-educated, live in an urban environment, have access to transport, are employed, have high socioeconomic status, and are privately insured.44
ConclusionOur findings indicate that people with FAI syndrome who had just commenced a physical therapist-led treatment program believe hip pain is caused by structural features and that they are often afraid to exercise due to fear of causing more damage to their hip. Not all patients have the resources to be able to undertake physical therapist-led treatment. Our study findings reveal important insights about how to facilitate successful implementation of best-practice physical therapist-led treatment for people with FAI syndrome. We recommend physical therapists provide clear education about the benefits of exercise and the poor relationship between structure and symptoms, inform patients of the costs and duration of treatment required, and embrace technologies such as exercise apps and telehealth appointments.
JK was funded by the NHMRC (Australia)APP1119971. The NHMRC was not involved in the conception, design, execution or writing of this study.