Although self-reported symptom duration of individuals with patellofemoral pain (PFP) is usually assessed for clinical and research purposes, its accuracy has never been investigated.
ObjectivesWe followed up individuals with PFP over 15 months to determine the agreement between self-reported symptom duration and calculated symptom duration.
MethodsSelf-reported symptom duration of 39 participants was assessed at baseline and re-assessed at follow-up. Calculated follow-up symptom duration was determined by the summation of baseline self-reported symptom duration with the known follow-up duration. The symptom duration difference was determined by the subtraction of the calculated follow-up symptom duration and the self-reported follow-up symptom.
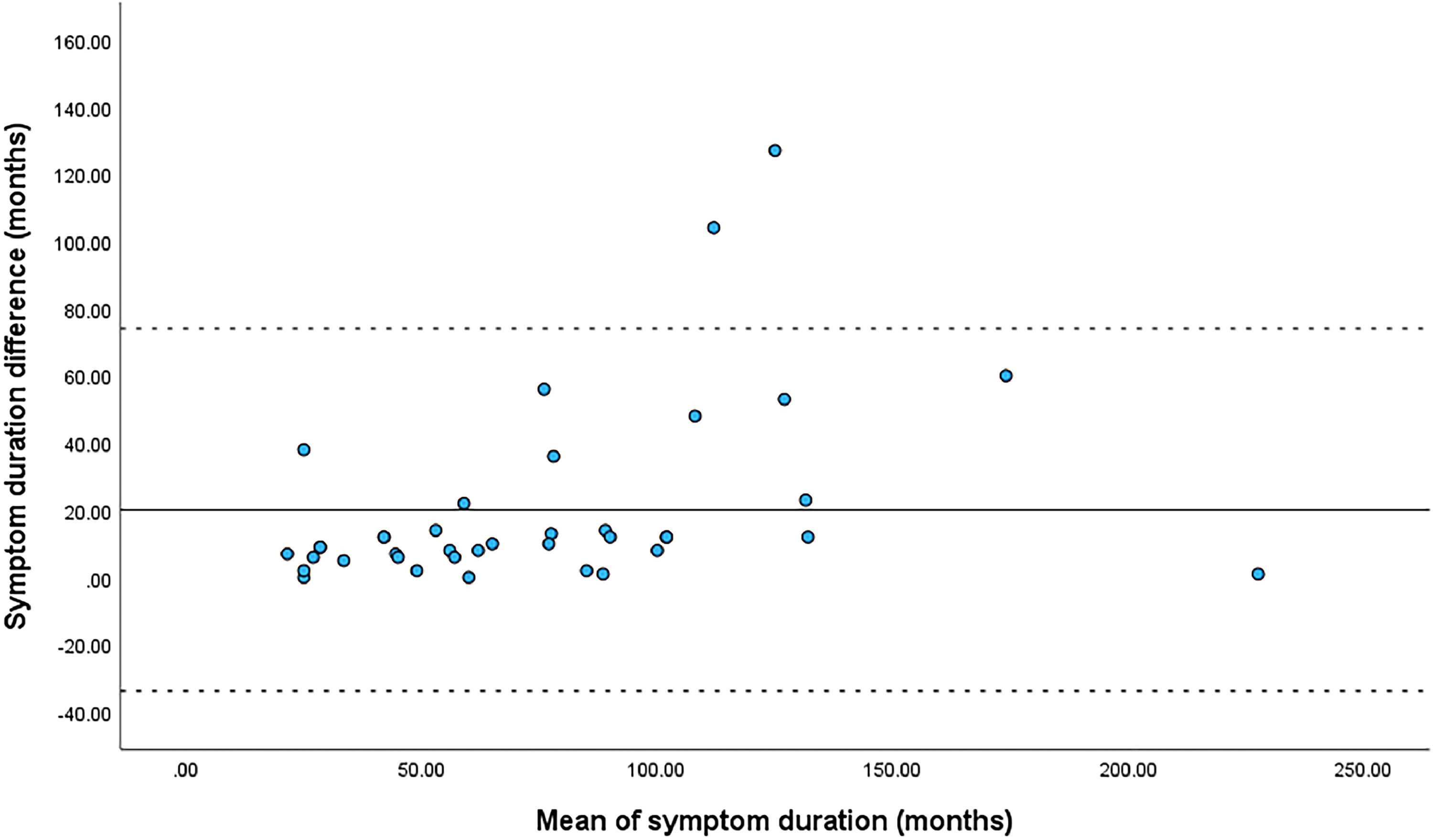
ResultsWe identified a symptom duration difference of 20.1 months (95 % confidence interval: 11.2, 29.1 months), with greater differences in individuals with longer symptom duration (r² = 0.12).
ConclusionOur findings suggest that the accuracy of self-reported symptom duration measures in individuals with PFP is questionable and techniques should be used to improve it.
Patellofemoral pain (PFP) is a highly prevalent musculoskeletal disorder (23 % in the general population) characterized by pain in the anterior or retropatellar regions of the knee.1 PFP is not self-limiting and symptoms may persist for up to 18 years after diagnosis.1 Longer symptom duration, measured via self-report, has been previously associated with quadriceps weakness,2 lower self-reported function,2 and disease progression.3 Clinicians and researchers are often interested in assessing patient's symptom duration,4 which is strongly recommended in the REPORTing of quantitative PatelloFemoral Pain (REPORT-PFP) checklist.5
Symptom duration in individuals with PFP is usually measured by simply asking patients to recall how long they have had knee pain (i.e., self-reported time since onset).2,3 However, by definition, PFP is a condition of insidious onset, making the actual duration difficult for patients to specify.1 Pain intensity is also highly variable in these individuals and fluctuates depending on the exposure to increased physical activity and pain-provoking tasks.6 It is not uncommon for individuals with PFP to report no pain at all in a given day, when not being exposed to pain-provoking tasks.6 The addition of pain variability to the inherent flaws of recalled memory of pain might considerably compromise an individual's ability to provide an accurate estimate of symptom duration.7 This may be particularly problematic for those with longer symptom duration as lengthy musculoskeletal pain is poorly remembered.8 To date, no study has investigated whether self-reported symptom duration provides an accurate estimate of PFP chronicity.
Therefore, the purpose of this study was to determine the agreement between self-reported symptom duration and calculated symptom duration of individuals with PFP following a 17- to 36-month follow-up period. We hypothesized that there would be poor agreement between measures.
MethodsThis observational longitudinal study followed the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) guideline and REPORT-PFP.5 This study was approved by the Sao Paulo State University Institutional Review Board (Presidente Prudente, Brazil, number: 4.649.629) and all participants provided written informed consent to participate.
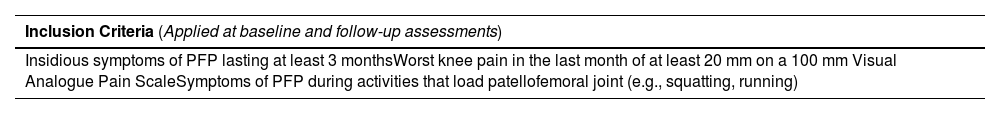
Participants were recruited through advertisements on social media, and at universities, gyms, and public parks. Based on the latest consensus statement on clinical examination of PFP,1 participants had to meet the eligibility criteria presented in Table 1 to be included in the study (i.e., baseline assessment). Participants were re-assessed after 15+ months (i.e., follow-up assessment) using the same eligibility criteria, and additional exclusion criteria for the follow-up period (Table 1). Participants who no longer met all eligibility criteria at follow-up assessment (e.g., no longer had pain) were not included in this study, whereas those who met them were included.
Eligibility criteria for participation in the study.
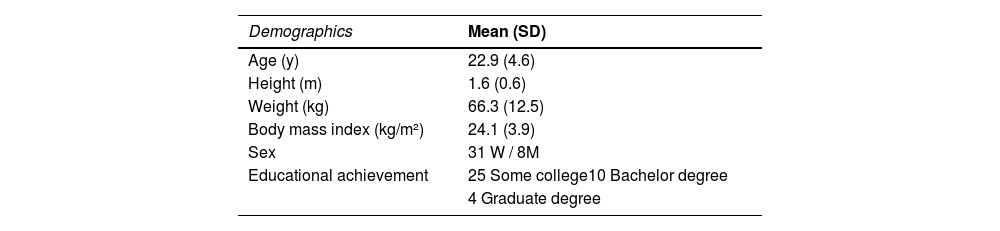
Self-reported pain and symptom duration were assessed at baseline and re-assessed at follow-up. The worst pain level in the previous month was obtained using the 0 − 100 mm visual analog scale, with 0 representing no pain and 100 the worst pain imaginable. Baseline demographics and educational level were assessed and are described in Table 2. Symptom duration was assessed by inquiring of the participants “How long have you had knee pain?” Time since onset was recorded in months. The assessments were performed identically by one assessor at baseline and a second assessor at follow-up. Both assessors were instructed and trained identically by a senior author.
The known follow-up duration was calculated as the difference in months between baseline and follow-up assessments, rounding up or down considering 15 days (e.g., 21 months and 18 days = 22 months). Mean [standard deviation (SD)] follow-up time was 25 (4.9) months (median = 24 months) (Fig. 1). Baseline self-reported symptom duration was summed with the known follow-up duration to determine the calculated follow-up symptom duration (e.g., 24 months of baseline self-reported symptom duration + 24 months of follow-up = 48 months of calculated follow-up symptom duration). The calculated follow-up symptom duration was then subtracted from the self-reported follow-up symptom duration to determine their difference (e.g., 48 months of calculated follow-up symptom duration – 52 months of self-reported follow-up symptom duration = 4 months symptom duration difference (absolute value)). The symptom duration difference was used for statistical analysis.
A paired t-test was conducted to compare baseline and follow-up worst pain level in the previous month. Cohen's d effect size (ES) was calculated and categorized as trivial (<0.2), small (≥0.2), moderate (≥0.5), large (≥0.8), and very large (≥1.3). A one-sample t-test was conducted to compare the symptom duration difference with a reference of zero (i.e., zero represents no difference between calculated and self-reported symptom duration at follow-up). A Bland-Altman plot was created to investigate the agreement between calculated and self-reported symptom duration at follow-up. A linear regression was performed to determine the presence of proportional bias between measures (i.e., whether the agreement varied through the range of measurements). Statistical analyses were performed with the IBM SPSS Statistics for Windows Statistical Version 20.0 (SPSS Inc. Chicago, IL, USA). Sample size calculation for this study was performed in MedCalc® Version 22.023 (MedCalc Software, Mariakerke, Belgium) and is described in detail in the Supplementary online material.
ResultsThirty-nine participants were re-assessed at follow-up and included in the present study. Reasons for dropout are presented in the Supplementary online material. Mean (SD) symptom duration of the 39 participants at baseline was 49.3 (46.8) months, ranging from 3 to 204 months. There was a statistically significant symptom duration difference of 20.1 (27.5) months [95 % confidence interval (CI) = 11.2, 29.1] between calculated and self-reported symptom duration. The calculated 95 % limits of agreement depicted in Fig. 2 further highlight how far apart the calculated and self-reported symptom duration were for most individuals. There was a positive association between symptom duration difference and mean symptom duration (i.e., mean of calculated and self-reported symptom duration at follow-up) (r² = 0.12), indicating the existence of proportional bias (i.e., the longer the symptom duration, the higher the difference between calculated and self-reported symptom duration).
There was a small decrease in the worst pain level between baseline [52.5 (20.2)] and follow-up [44.8 (19.6)] assessments (mean difference = 7.6; SD = 21.9; ES = 0.39; 95 %CI = 0.53, 14.7). Individual participant data is presented in online material 3.
DiscussionWe observed an inaccurate symptom duration recall, with a mean difference of 20 months. The slight decrease in pain observed in our study in addition to the high variability of PFP symptoms may have decreased one's ability to accurately self-report symptom duration. Other studies on the accuracy of pain recall have also reported that retrospective assessment of pain have poor validity.7,9 In a cohort of 538 workers followed up for 6 years, 72 % of them did not recall having had experienced pain at baseline assessment.8 Forgetting reached 100 % in those with no current symptoms, but was also considerable (45 %) in those with current symptoms.8
We were also able to corroborate in PFP that the length of the time since symptom onset can influence the accuracy of recall, as has been previously reported.7 While only 8 % of those with history of low back pain have forgotten it after 12 months,10 31 % have forgotten sciatic pain after 3 years11 and 72 % musculoskeletal pain in general after 6 years.8 Most of the 39 participants of our study (71 %) had symptoms for >24 months. Accuracy of self-reported symptom duration should be cautioned in those with long-standing PFP.
Some techniques can be used to provide more accurate reports. First, we recommend the use of anchor points, which are memorable, personal, or cultural events that occurred during the period in question.9 Patients remember health events more easily the closer they fall to landmark events, which may improve symptom onset recall.9 Recall may also be improved by asking patients to recall their symptom history backwards, from the most recent to the most distant memory of knee pain.9 Another aid may be to assist patients in partitioning generic memories of pain into smaller units and finding features that distinguish them from one another (e.g., a series of recurrent knee pain episodes).9
It is important to highlight that participants from our study may have provided inaccurate reports of symptom duration at baseline. Although we cannot confirm or refute this assumption, its occurrence would further corroborate that self-reported symptom duration is an inaccurate measure. Potential drawbacks of this study are the high dropout rate and that the exact onset of PFP symptoms is unknown. However, these limitations do not affect the results and their interpretations.
ConclusionOur findings suggest that the accuracy of self-reported symptom duration measures in individuals with PFP is questionable and techniques should be used to improve its accuracy.
We would like to thank Sao Paulo Research Foundation (FAPESP) for funding this study (process number: 2020/14715–5). The financial sponsors played no role in the design, execution, analysis and interpretation of data, or writing of the study.