Mirror therapy shows promise in the treatment of phantom limb pain but lacks robust evidence.
ObjectivesTo address this gap, we conducted a scoping review aiming to comprehensively explore the landscape of mirror therapy practice, gather details about the session content, and offer recommendations for future research.
MethodWe searched seven databases for published work from 1995 to May 2023. Two independent reviewers selected, assessed, and extracted data from eligible articles. Articles, regardless of study design, were considered eligible if they investigated mirror therapy as an intervention for phantom limb pain.
ResultsA total of 44 articles were included, comprising 16 randomized control trials, 14 prospective cohort studies, 15 case reports, and 3 protocols. These studies collectively involved 942 patients, with male patients representing 70 % of the participants. Lower limb amputation, primarily attributed to trauma, accounted for 88 % of the included patients. Pain intensity was predominantly assessed by a visual analog scale (61 %). However, there was a notable absence of detailed descriptions regarding mirror therapy sessions, particularly concerning the number of exercises, duration per exercise, and repetitions. Typically, sessions lasted 15 min each, conducted once daily. The exercises primarily focused on motor exercises targeting the distal part of the limb.
ConclusionThe practice of mirror therapy was characterized by poor description, showed significant heterogeneity, and a lack of standardized protocols, which contributes to an overall low level of evidence. Addressing these gaps in practice description and standardization is crucial for improving reproducibility and strengthening the evidence base for the prescription of mirror therapy.
Phantom limb pain (PLP) is a complex condition where individuals experience pain in a limb that has been amputated, distinct from residual limb pain and phantom limb sensation.1,2 Recent meta-analyses suggest that PLP prevalence ranges from 64 % to as high as 85 %.3–5 However, understanding the precise mechanisms of PLP remains a challenge.
Current theories about PLP mechanism propose a combination of disruptions in both the peripheral and central nervous systems.6,7 Flor et al.8 suggest that PLP arises from changes in the functional organization of somatotopic maps in the primary somatosensory cortex (S1), where cortical reorganization correlates with pain intensity.8 This central maladaptive plasticity is suggested to be a consequence of the absence of afferent signals from the missing limb and spinal deregulation, resulting in the heightened transmission of pain signals.6 In addition, the reorganization of the motor cortex has been associated with phantom limb movements.9 Another theory links PLP severity to the preserved representation of the missing limb in the cortex and reduced inter-regional connectivity in the primary sensorimotor cortex.10 These two theories emphasize the complexity of the PLP phenomenon.
Numerous treatments for PLP have been investigated in recent years.3–5,11 However, evidence regarding the efficacy remains limited and conflicting, for both pharmacological12,13 and non-pharmacological treatments.14 Mirror therapy (MT) is a popular non-pharmacological treatment considered to be affordable and simple to implement by caregivers and patients.15 Systematic reviews on its efficacy yield mixed results due to study limitations such as small sample sizes and low levels of evidence.16–18 Since publication of these systematic reviews, new primary research has been conducted to evaluate the effectiveness of MT.19–24 Additionally, two recent meta-analyses have been conducted. One review suggests a positive effect of MT at one month but not at three and six months,5 the other review indicates a larger effect size in pain reduction compared to alternative techniques.4 These conclusions are questionable due to methodological and statistical choices, including the use of fixed-effect models in the meta-analyses, the incorporation of studies with low statistical power, strong heterogeneity in MT practice, and the interpretation of effects that may not be clinically relevant.25,26
To date, several challenges persist: (i) significant heterogeneity of practice, making study comparisons difficult; (ii) a lack of consensus on treatment frameworks; and (iii) difficulties in conducting high-quality randomized controlled trials (RCTs) due to low number of patients and diverse clinical presentation. To address these issues and establish a common framework for MT in treating PLP, a comprehensive overview of how MT has been investigated is needed. This involves identifying similarities across studies investigating MT, regardless of the type of study design, rather than solely relying on RCTs, which often lack quality and generalizability. Conducting a scoping review seems appropriate for this purpose, providing insight into current practices and identifying key elements for future research. The aim of this scoping review was to map the extent of MT practice in PLP treatment and gather details on the content and duration of sessions as well as the length of treatment.
MethodEligibility criteriaStudy designs eligible for this scoping review included all original research studies following JBI scoping review methodology recommendations.27 This included interventional research, such as randomized and non-randomized trials, case series, case reports, and case-control studies. Rehabilitation protocols that describe the intervention were also included. Studies published in English or French after 1995 (date of the first report on the MT technique) were deemed eligible. Retrospective studies, conference abstracts, and editorials were excluded. To be included, studies had to recruit participants who experienced PLP following upper or lower limb amputations, regardless of the level of amputation. Studies recruiting people with other pathologies such as hemiplegia were excluded. Studies had to provide information on MT as an intervention for PLP, including number of sessions, frequency and duration of treatment, exercises performed, repetitions, patient positioning, or mirror specifications. Studies had to evaluate PLP at least once, with clearly defined time points and methods of assessment, without restrictions to particular pain assessment methods. Secondary research such as reviews and guidelines were included to screen their bibliography for potential missing primary research.
Information sources and search strategyWe searched seven databases, including CENTRAL, Clinicaltrial.gov, Cochrane Database of Systematic Reviews, Physiotherapy Evidence Database (PEDro), PubMed, ScienceDirect, and Scopus. The detailed search strategy is provided in Table 1. Following the recommendations from the PRISMA checklist for scoping reviews,28 the initial search was conducted in March 2022 across the seven databases with an update in March 2023. Searches in CENTRAL, Cochrane Database of Systematic Reviews, ScienceDirect, and Scopus covered title, abstract, and keywords while PubMed searches were limited to title and abstract.
Search strategy for the different databases.
Two reviewers (MG and KA) independently conducted study selection and resolved disagreements through review meetings. Results from searches were stored in a shared Zotero 5.0 folder. Duplicate articles were removed during bibliographic research. Initial screening involved reviewing titles and abstracts, followed by a second screening of full-text articles to verify eligibility criteria and extract relevant data. Reference lists of included studies and systematic or narrative reviews or guidelines were also checked for potentially relevant studies missed during database research.
Assessment of risk of biasAssessment of risk of bias was conducted or reported exclusively for RCTs using the PEDro scale.29–31 Two reviewers (MG and KA) independently evaluated studies when the score was not available, and disagreements were resolved through consensus.
Data extractionTwo reviewers (MG and KA) independently conducted data extraction. A standardized Excel sheet was used to ensure consistency. Regular video conferences were scheduled between reviewers to update and discuss data extraction progress. The extraction sheet is available upon request.
Data itemsData items included authors, publication year, country, study design, participant numbers, sex distribution, amputation type and level, etiology, time since amputation, study objectives, intervention details (session number, frequency, duration, length), follow-up period, exercise content, associated therapy, control group intervention, pain evaluation scales, main results, observed effects, effect sizes, side effects, and eligibility criteria. Additionally, items from the Template for Intervention Description and Replication (TIDier)32 were sought including: who provided the treatment, where the treatment was administered, whether tailoring was involved, and any modifications made to the intervention.
Synthesis of resultsFindings were summarized narratively and presented in tables. Detailed data were organized into multiple tables based on extraction categories. Values are expressed either as numbers (n) or percentages (%).
ResultsSearch resultsThe literature search was initially conducted in March 2022, with an update performed in March 2023 across seven databases. Search synthesis is illustrated in Fig. 1.33 Of the total 1152 records identified, 44 articles were considered eligible and included in this review.
Characteristics of included studiesThe included studies span from 2004 to 2023. Of the 44 included studies, 34 % of the studies (n = 15)15,34–47 were published between 2004 and 2013 and 66 % (n = 29)19–24,48–70 between 2014 and 2023. Included studies were conducted in 19 countries. Fourteen studies36,38,41,43,47–50,58,58–60,62,65,67 are from the United States of America. Four studies are from India24,53–55 and Japan39,42,44,63; 3 studies from the United Kingdom,34,35,56 Pakistan21,23,57 and Spain64,66,68; 2 studies from Iran69,70 and Turkey19,61; and 1 study from Austria,37 Cambodia/Norway,51 Ireland,46 Israel,22 Italy,15 South Korea,45 the Netherlands,20 South Africa,52 and Sweden.40
Thirty-six percent of the studies (n = 16)19–24,34–36,49–55 are randomized controlled trials (RCTs), 4 % (n = 2) are non-randomized control studies,60,62 25 % (n = 11)15,39–47,56,63–68 are case series, 25 % (n = 11) are case reports,15,43–47,64–68 and one is a case-controlled study.58 Seven percent (n = 3)48,69,70 are protocols of RCTs. This diversity of study designs reflects the heterogeneous nature of the evidence base for this treatment modality.
Among participants, 68.5 % were male (n = 684), 21.1 % females (n = 212), and sex was not reported for 10.3 % of the participants (n = 103). The most common etiology of the amputation, for 46.6 % (n = 472) of patients, was trauma, followed by peripheral artery disease for 22 % (n = 223), medical causes for 4.8 % (n = 49), and cancer for 3.7 % (n = 37). Less frequent 2.1 % of causes included infection (n = 21) and congenital condition (n = 1). Etiology information was missing for 20.7 % of patients (n = 209).
Among the included studies, 87 % were lower limb amputations (n = 831) and 12 % upper limb amputations (n = 113). One study did not specify the amputated limb (n = 13).59 Lower limb amputations included 58 % of amputations at the tibial level (n = 484), 30 % at the femoral level (n = 252), 2 % at the knee level (n = 16), 1 % at the hip or ankle level (n = 9), and the level was not reported in 8.4 % (n = 70). Upper limb amputations included 32 % at the humeral level (n = 36), 35 % at the radial level (n = 40), and 3.5 % at other levels (n = 4), such as wrist and shoulder disarticulation. The level of amputation was not reported for upper limb for 29 % of patients (n = 33).
Pain assessmentVarious tools were used to assess PLP, with seven different ones reported. In some studies, multiple tools were used. The Visual Analog Scale (VAS) was the most frequently used, present in 61 % of the studies15,19,21,34–37,40–45,47–51,53–56,58,59,68–70 (n = 27), followed by the Numeric Rating Scale (NRS) in 20 % of the studies20,23,24,38,39,57,61,66,68 (n = 9). Additionally, the Brief Pain Inventory (BPI) was mentioned in 9 % of the studies22,52,60,62 (n = 4) and the McGill Pain Questionnaire (MPQ) in 7 % of the studies22,34,55 (n = 3). One study reported each of the following tools: the Universal Pain Score (UPS),54 the Multidimensional Pain Inventory,59 and a 5-point Likert scale.63 Nine percent of the studies46,63,65,67 (n =4) did not report the tool used to assess PLP.
Mirror therapy interventionsDetailed information on MT sessions, including exercises, durations, series, repetitions, and modalities, was compiled when available (Table 2).
Studies characteristics.
| Authors Year Country | Study design | Participants characteristics Number of participants Sex (♂; ♀) Age (as reported in the studies) Amputation Characteristics UL or LL Level of amputation Etiology Time since amputation | Tools (Test group or subject) | Comparator | Performed by the patient alone or under the supervision of a therapist Intervention location | MT Intervention Number of sessions Intervention duration Frequency Session length Follow up | Components of MT sessions Time per exercise Number of exercises Series components Repetition components Exercises components | Evolution of the protocol | Pain evaluation Scales |
|---|---|---|---|---|---|---|---|---|---|
| Anaforoğlu Külünkoğlu et al. 201919 Turkey | RCT | n = 40 23 ♂; 17 ♀ 18 - 45 years 40 LL 40 TT 40 TR 13.25 (3 - 53) years | Mirror 120 × 40 cm | Mental visualization | Patient alone Home-based | / 4 weeks duration 1 per day (check daily for 4 weeks then once a week and biweekly) 15 min session duration 6 months follow up | / 6 exercises 1 set per exercise / Foot flexion/extension Foot inversion/eversion Foot rotation around the ankle Adduction with flexion of the toes like clenching Abduction (spreading) with extension of the toes like unclenching Relaxation of all muscles after strong contraction of all foot and ankle muscles of both the phantom and intact limbs | Modifications of the frequency after 4 weeks | VAS |
| Brodie et al. 200734 UK | RCT | n = 80 (Test 41; Control 39) 63 ♂; 17 ♀ 55 (20 - 83) years 80 LL 35 TF; 45 TT 49 Medical; 26 TR; 4 Cancer; 1 Congenital 9 (1 – 50) years | Virtual limb boxes with mirror 64×90 cm | Obscured mirror | Instructed by the therapist Hospital | 1 session 1 day / / / | / 10 exercises 1 set 10 repetitions Knee flexion / extension Knee flexion / extension as if walking Foot flexion/extension Foot inversion/eversion Foot rotation around the ankle Foot walking movements Toes flexion / extension Toes adduction (clenching) / abduction (unclenching) Spread out toes and relax Big toe flexion with other toes extension / Big toe extension with other toes flexion | / | VAS MPQ |
| Finn et al. 201749 USA | RCT | n = 15 15 ♂ 18 - 70 years 15 UL 6 TH; 7 TRU; 2 WD 15 TR 0.55 - 24 months | Mirror | Covered mirror or Mental visualization | Instructed by the therapist Hospital | 20 sessions 4 weeks duration 5 per week 15 min session duration / | / 6 exercises / / Abduction/adduction of the thumb and fifth finger Flexion/extension of the thumb Flexion/extension of the fingers Pronation/supination of the hand Flexion/extension at the wrist Flexion/extension of the elbow (for trans-humeral amputees) | / | VAS |
| Gunduz et al. 202150 USA | RCT | n = 112 74 ♂; 38 ♀ 44.3 years 112 LL 65 TF; 47 TT 112TR > 3 years | Mirror + Soterix Medical 1 × 1 tDCS device | MT + tDCS Covered MT + tDCS Covered MT + Sham tDCS | Instructed by the therapist and then patient alone Hospital and then home-based | 20 sessions 4 weeks duration 5 per week 12 to 15 min session duration 2 months follow-up | / 3 exercises / / Light tactile stimulation Flexion / extension of the relevant body part Write the alphabet with the lower limb | First at the hospital under the supervision of the therapist and after two weeks home-based alone | VAS |
| Ol et al. 201851 Norway Cambodia | RCT | n = 45 (Test 15; Control 30) 44 ♂; 1 ♀ MT: 57.5 years Tactile: 52 years MT + tactile: 57.6 years 45 LL 45 TT 45 TR MT: 23.1 years Tactile: 23.2 years MT + tactile: 22.5 years | Mirror 30×80 cm | Tactile therapy or Combined MT and tactile therapy | Patient alone Home-based | / 4 weeks duration 2 per day 5 min session duration 4 months follow up | 5 min per exercise 1 exercise / / Flexion / extension of the foot | / | VAS |
| Limakatso et al. 202052 South Africa | RCT | n = 21 (Test: 11; Control: 10) 16 ♂; 5 ♀ Test group: 63 (53–65), Control group: 62 (59–67) 1 UL; 20 LL 1 TH; 10 TF; 10 TT 16 PAD; 2 TR; 3 infection Test group: 17 months (13–28), Control group: 20 months (12–36) | Tablet with RecogniseTM software application + Photographs + Mirror (300 mm × 300 mm) | Routine physical therapy Care | Instructed by the therapist and then patient alone Hospital for two separate days and then home-based | / 2 weeks (included in a 6 week protocol, 2 weeks of left/right judgement, 2 weeks of imagined movements, and 2 weeks of MT) 12 sessions per day 10 - 30 min session duration 6 months follow-up | / / / / Replicate a position seen on photographs by moving the contralateral limb and the amputated limb (no details) | First at the hospital under the supervision of the therapist and then home-based alone Modifications of the session duration from 30 min at the hospital to 10 min at home. | BPI |
| Mallik et al. 202053 India | RCT | n = 92 (Test: 46; Control: 46) 73 ♂; 19 ♀ 34.79 years 22 UL; 70 LL 16 TH; 6 TRU; 22 TF; 48 TT 12 PAD; 65 TR; 9 cancer; 6 infection / | Mirror | Mental visualization | / Hospital and then home-based | / / / 30 min session duration 1 year follow-up | / 1 exercise / / / | Treatment delivered in the hospital and then at home (no timeline provided) | VAS |
| Moseley 200635 UK | RCT | n = 9 / / UL; LL / / / | Photographs + Mirror 300 mm x 300 mm | Standard medical and physical therapy care | / / | 140 2 weeks (included in a 6 week protocol, 2 weeks of left/right judgement, 2 weeks of imagined movements, and 2 weeks of MT) 5 per day during 4 days, 10 per day during the 4 next days, and 12 per day for the next 6 days / 6 months follow up | / / / / / | Modification of the daily frequency | VAS |
| Noureen et al. 202223 Pakistan | RCT | n = 36 (Test group: 18; Control group: 18) 33 ♂; 3 ♀ (Test group : 35.22; Control group : 36.33) 36 LL 26 TT; 10 TF 30 TR (Test group : 2.83 years; Control group : 2.67) | Flat mirror (640×900 mm) | Routine physical therapy | / / | 20 sessions 4 weeks 1 per day / 5 per week 15 min / | / 10 exercises / 10 repetitions Knee flexion/extension Knee flexion/extension like walking Foot flexion/extension Foot pronation/supination Circle with the feet Foot flexion/extension like walking Toes flexion/extension Clamp and unclamp the toes Expand the toes and relax Raise the big toe while pointing the other toes down, and reverse | / | NRS |
| Segal et al. 202122 Israel | RCT | n = 30 23 ♂; 7 ♀ 58.1 ± 10.9 years 30 LL 13 TF; 17 TT 23 PAD; 2 TR; 2 cancer; 3 infection < 8 weeks | Mirror 150×80 cm | MT + sham tDCS MT + tDCS | Patient alone but nurse in attendance to ensure compliance and to assist the patient if needed Hospital | 10 sessions 2 weeks duration 5 per week 20 min session duration 3 month follow up | / 2 exercises / / Foot flexion/extension Foot inversion/eversion | / | SF-MPQ BPI |
| Tilak et al. 201554 India | RCT | n = 26 23 ♂; 3 ♀ Mirror therapy 42.62 ± 10.69 years TENS 36.38 ± 9.55 years 7 UL; 19 LL 2 TH; 5 TRU; 14 TF; 5 TT / 45 days | Mirror | Contralateral limb Transcutaneous electrical nerve stimulation | / Hospital | 4 sessions 4 days duration 1 per day 20 min session duration / | / / / / / | / | VAS UPS |
| Zaheer et al. 202121 Pakistan | RCT | n = 24 17 ♂; 7 ♀ 42,9 years 24 LL TF; TT (no precision about proportions) PAD; TR < 2 years | Mirror 130×46 cm | MT + Mental visualization | Instructed by the therapist Hospital | 28 sessions 4 weeks 1 per day 15 min session duration / | / / / / / | / | VAS |
| Purushothaman et al. 202324 India | RCT | n = 128 (but 120 analyzed) 95 ♂; 33 ♀ Test group 51.3 ± 10.7 years Control group 53.5 ± 9.9 years 120 LL 120 TT 106 PAD; 5 TR; 9 infection / (post-operative period) | Mirror box was prepared with a mirror on one side and an opaque surface on the other side of the mirror | Not received mirror therapy in the post-operative period | / Hospital | 14 sessions 7 days 2 per day 20 min session duration 6 months | / 4 exercises / / Ankle flexion / extension Ankle rotations Knee flexion / extension Hip flexion / extension | / | NRS |
| Rothgangel et al. 201820 Netherlands | RCT 3 arms | n = 75 (Test 25; Control 50: 26 Traditional MT followed by teletreatment, 24 sensorimotor exercises) 52 ♂; 23 ♀ 61.1 years 75 LL 1 HD; 45 TF; 5 TK; 22 TT; 2 PF 30 PAD; 25 TR; 10 cancer; 10 others Traditional MT: 56.5 months Traditional MT followed by teletreatment: 38 months sensomotor exercises: 31 months | Mirror at the hospital and no training material provided at home | Four weeks of traditional MT followed by six weeks of teletreatment using augmented reality MT Four weeks of sensomotor exercises to the intact limb followed by six weeks of self-delivered exercises | Instructed by the therapist Hospital and then Home-based | / 10 weeks duration (4 weeks of traditional MT followed by 6 weeks of self-delivered traditional MT) / 30 min session duration / | / / / / / | After 4 weeks, home-based MT realized as much as they want | NRS |
| Ramadugu et al. 201755 India | RCT crossover | n = 60 (Test 32; Control 28) / 17 - 62 years 10 UL; 50 LL 5 TH; 5 TRU; 20 TF; 25 TT; 5 CE / / | LL: Standing mirror (130 cm × 46 cm) with wooden frame and base (62 cm × 65 cm) UL: Mirror (44 cm × 46 cm) placed on one side of partition at the center of a plywood box (65 cm × 48 cm × 46 cm) | Covered mirror | Instructed by the therapist Hospital | 28 sessions Test group: 4 weeks duration Control group: 8 weeks duration (4 weeks covered mirror, followed by 4 weeks without the cover) 7 per week 15 min session duration Test group 16 weeks follow up Control group 20 weeks follow up | / 5 exercises / / Flexion / extension knee/elbow Wrist supination / pronation or Foot inversion / eversion Circle around the wrist / ankle Flexion / extension of toes / fingers Clench / unclench toes/fingers | Control group : After 4 weeks, MT without the cover | VAS MPQ |
| Chan et al. 200736 USA | RCT 3 arms crossover | n = 18 (Test 6; Control: 6 covered mirror, 6 mental visualisation) / / 18 LL / / / | Mirror | Covered mirror followed by MT Mental visualization followed by MT | Under direct observation Hospital | / 8 weeks duration / 15 min session duration / | / / / / / | At 4 weeks, patients in covered mirror and mental visualization groups switched to the MT treatment for the last 4 weeks | VAS |
| Houston et al. 201660 USA | Non-randomized controlled study | n = 14 8 ♂; 6 ♀ Acute group: 58.2 years Sub-acute group: 61.6 years 14 LL 3 TF; 11 TT 14 PAD Acute group: 35.5 (26 – 48) h Sub-acute group: 18.2 (8 – 28) months | 1/8″ plexi-glass mirror (27 × 15″) + Farabloc cover | / | / / | / 4 weeks duration 1 per day 15 min session duration 8 weeks follow up | / / / 15 repetition Active range of motion exercises for each joint | / | BPI |
| Houston et al. 201662 USA | Non-randomized controlled study | n = 14 8 ♂; 6 ♀ Acute group: 58.2 years Sub-acute group: 61.6 years 14 LL 3 TF; 11 TT 14 PAD Acute group: 35.5 (26 – 48) h Sub-acute group: 18.2 (8 – 28) months | 1/8″ plexi-glass mirror (27 × 15″) + Farabloc cover | / | / / | / 4 weeks duration 1 per day 15 min session duration 8 weeks follow up | / / / 15 repetition Active range of motion exercises for each joint | / | BPI |
| Chan et al. 201958 USA | Case controlled study | n = 18 (Test 9 amputees; Control 9 healthy) 10 ♂; 8 ♀ Test: 50 (30 - 75) years Control: 44 (24 - 58) years 9 LL 3 TF; 1 TK; 5 TT 7 TR; 1 infection; 1 cancer 0 - 21 years | Mirror | Healthy subjects | / / | 20 sessions 4 weeks duration 5 per week 15 min session duration 4 weeks follow up | 5 min per exercise 3 exercises / / Foot flexion / extension Foot rotation around the ankle | / | VAS |
| Wareham et Sparkes 202056 UK | Case series | n = 16 / 31 years 16 LL 4 TF; 10 TK; 2 TT 16 TR 0.95 years (5 days-11.78 years) | Mirror box | / | Patient alone Hospital | / 1 day / 10 min session duration / | / / / / Movements at the discretion of patients | / | VAS |
| Sumitami et al. 200839 Japan | Case series | n = 22 (11 amputees) 9 ♂; 2 ♀ 32 - 74 years UL - LL / 5 TR; 6 cancers 181.81 ± 345.17 weeks | Mirror board | / | Patient alone Hospital | / Mean 20.4 weeks duration 1 per day 10 min session duration 3 - 78 weeks follow up | / / / / Movements at the discretion of patients | / | NRS |
| Seidel et al. 201137 Austria | Case series | n = 8 8 ♂ 50 (31 - 78) years 8 LL / / 162 (27 - 624) months | Mirror 77×58 cm | / | Instructed by the therapist Hospital | 12 sessions 21 days duration 2 per week, 2 per day (spaced by 2 h) 26 - 31 min session duration / | 1 min per exercise 6 exercises 2 series / Hip abduction / adduction Hip external rotation / internal rotation Hip and knee flexion / extension Foot dorsiflexion/supination - plantar flexion / pronation Foot dorsiflexion / pronation – plantar flexion / supination Toes flexion / extension | / | VAS |
| Iqbal et al. 201557 Pakistan | Case series | n = 35 35 ♂ 36 ± 11 (17 - 60) years / / 8 Non-TR; 27 TR / | Mirror 244×152 cm | / | Under direct observation Hospital | 15 sessions 3 weeks duration 5 per week 15 min session duration / | / / / / Movements at the discretion of patients | / | NRS |
| Foell et al. 201459 USA | case series | n = 13 9 ♂; 4 ♀ 50.6 (26 - 74) years 13 UL / / > 2 years | Mirror 30 × 50 cm | / | Patient alone Home-based | 20 sessions 4 weeks duration 5 per week 15 min session duration 2 weeks follow up | 3 min per exercise 5 exercises / / Open / close the hand Flexion / extension of the fingers Pronation / supination at the wrist Touch the fingertips with the thumb Tracing figures with fingers | / | VAS MPI |
| Darnall et al. 201238 USA | Case series | n = 31 18 ♂; 13 ♀ 32 - 74 years 11 UL; 20 LL / 17 No-TR; 14 TR 0.2 - 59 years | Mirror + Study binder + DVD for participants enrolled remotely | / | Patient alone Home-based | / 1 or 2 months duration 1 per day 25 min session duration 1 month follow up | / / / / / | / | NRS |
| Yildirim et al. 201666 Turkey | Case series | n = 15 13 ♂; 2 ♀ 52.13 ± 16.68 years UL; LL / 7 PAD; 8 other / | Mirror + Booklet | / | Instructed by the therapist and then patient alone Hospital and then Home-based | / 4 weeks duration / 40 min session duration / | / / / / / | Instructed by the therapist at the hospital and patient alone at home when the researcher was convinced that the patient was capable of continuing mirror therapy alone correctly | NRS |
| Schmalzl et al. 201340 Sweden | Case series | n = 6 2 ♂; 4 ♀ 55 (39 - 80) years 6 UL 3 TH; 3 TRU 5 TR; 1 cancer 1.5 - 50 years | Mirror 35×55 cm + Small paintbrushes | Covered mirror | Instructed by the therapist Hospital | 1 session 1 day / 15 min session duration / | 60 s per exercise 8 exercises / / / | / | VAS |
| Hanling et al. 201041 USA | Case Series | n = 4 4 ♂ 22 - 27 years 4 LL 4 TT 4 TR No amputation at the intervention | Mirror | / | Instructed by the therapist and then patient alone Hospital | 14 sessions 2 weeks duration 7 per week 30 min session duration / | / / / / / | From instructed MT to patient alone after 5 or 6 MT sessions | VAS |
| Imaizumi et al. 201763 Japan | Case series | n = 9 9 ♂ 64.78 (46 - 80) years 9 UL / 1 PAD; 8 TR 17 - 62 years | Portable glass mirror 267 mm x 368 mm | / | Instructed by the therapist Hospital | 1 session 1 day / 15 min session duration / | / 3 exercises / / Moving the intact hand toward or away from the mirror Moving it forward or backward along the sagittal plane Opening / closing the fingers | / | Questionnaire on the senses of agency and ownership over the phantom limb and phantom limb pain. Pain intensity: How intense is the pain from your phantom limb? 1: Not at all. 5: Extremely. Unpleasantness: To what extent do you feel your phantom limb pain unpleasant? 1: Not at all. 5: Extremely |
| Kawashima et al. 201342 Japan | Case series | n = 13 ♂ 56.5 ± 16.49 (33 - 77) 13 UL 13 TRU 12 TR, 1 sarcoma / | Mirror | Without the mirror | Instructed by the therapist / | 1 session 1 day / 30 s / | 30 s for the exercise 1 exercise 1 set / Wrist flexion / extension | / | VAS |
| Clerici et al. 201215 Italy | Case report | n = 1 ♂ 39 years LL TF Cancer 22 years | Mirror 108 × 37.5 cm | / | / / | / 26 weeks duration 2 per day 30 min session duration 6 months follow-up | / 5 exercises / / Looking at his leg Touching his leg Caressing his leg Scratching his leg Moving his leg | / | VAS |
| Darnall. 200943 USA | Case report | n = 1 ♂ 35 years LL TF TR 1 year | Full-length mirror 122×30 cm | / | Patient alone Home-based | / 3 months duration 5 per week then 3 per week after 1 month 20 - 30 min then after 1 month 30 min 3 months follow up | / 5 exercises / / Foot flexion/extension Foot rotation around the ankle Touching the big toe in the mirror Knee flexion / extension Hip flexion / extension | Decrease the frequency and stabilization of the session length after 1 month | VAS |
| Folch et al. 202164 Spain | Case report | n = 1 ♀ 53 years LL TF Infection / | Mirror box | / | Instructed by the therapist Hospital | 120 sessions 24 weeks 5 per week 10 - 12 min session duration 2 years follow-up | / 3 exercises 1 set 10 repetitions Foot inversion Foot eversion Foot flexion/extension | Alternating periods without and with TM | IPT-R |
| Kawashima et al. 200944 Japan | Case report | n = 1 ♂ 60 years UL TRU TR 2 months | Mirror | / | Instructed by the therapist Hospital | / 3 months duration 1 h per week / 6 months follow-up | / / / / / | / | VAS |
| Kim et al. 201245 Korea | Case report | n = 1 ♂ 30 years UL TH TR 8 months | Mirror | / | / Hospital and then home-based | / / 4 per week and after 3 months 3 to 4 times per week 15 min session duration / | / / / / / | 4 times per week during 3 months at the hospital and then at 3 to 4 times per week at home | VAS |
| MacLachlan et al. 200446 Ireland | Case report | n = 1 ♂ 32 years LL HD Infection / | Full length mirror 36 x x120 cm + TENS | / | Instructed by the therapist and then patient alone Hospital | / 19 days duration 2 per day the first week; 4 or 5 per day the second week (2 with therapist, 2 or 3 on his own); 2 or 3 per day the third week / / | / 10 exercises 10 Series 10 Repetitions Knee flexion / extension Knee flexion / extension alternately as if walking Foot flexion/extension Foot inversion/eversion Foot rotation around the ankle Foot walking movements Toes flexion / extension Toes adduction (clenching) / abduction (unclenching) Spread toes and relax Big toe flexion with other toes extension / Big toe extension with other toes flexion | Modifications of the number of daily sessions at the second and the third week | Unprecised scale: 1 = None at all 10 = excruciating |
| Ramsey et al. 201765 USA | Case report | n = 1 ♂ 7 years UL TH Cancer / | Mirror | / | / Hospital and then Home-based | / / 2 per day 10 min session duration / | / / / / / | / | / |
| Yildirim et al. 202066 Spain Turkey | Case report | n = 1 ♀ 24 years UL TH TR 3.5 months | Mirror 40×120 cm | / | Patient alone Home-based | / 4 weeks / 20 - 30 min session duration / | / 6 exercises / / Moving the fingers Touch the fingertips with the thumb Opening and closing the interdigital space Open / close the hand Pronation / supination at the wrist Flexion / extension at the wrist | / | NRS |
| Thomas. 201567 USA | Case report | n = 1 ♂ 48 years UL SD TR / | Mirror + Third party to perform tactile stimulation | / | Instructed by the therapist and then patient alone / | / 8 weeks duration 1 or 2 per week / / | / 3 exercises 2 series 40 repetitions Wrist extension / flexion Elbow flexion / extension Wrist radial / ulnar deviation | Change of the frequency between weeks (1 or 2 per week) Instructed by therapist and then alone | / |
| Villa-Alcazar et al. 201868 Spain | Case report | n = 1 ♂ 9 years LL TF Cancer 10 days | Mirror | / | / / | / 8 weeks duration 5 per week at the beginning, then only days with pain 15 min / | / / / / / | Change of the frequency after the pain decrease. Only performed if pain felt by the patient | VAS NRS |
| Wilcher et al. 201147 USA | Case report | n = 1 ♂ 24 years UL STD TR / | Mirror + Third party creating auditory feedback + TENS | / | / / | 10 sessions 2 weeks duration 2 per day 15 min session duration / | / 3 exercises / / Elbow flexion / extension Open / close the hand Pronation / supination at the wrist | / | VAS |
| Alirezataheri 202169 Iran | RCT Protocol (Not published) | / ♂ / LL TT TR 10 years | Mirror | Standard physical therapy care | Patient alone Home-based | 28 sessions 6 weeks 7 per week 14 min session duration 6 weeks follow-up | / 4 exercises 1 set / Finger movements Bending and straightening of the wrist Rotation of a healthy limb Looks at healthy foot movements in a mirror | / | VAS |
| Mansour-ghanaei 202170 Iran | RCT Protocol (Not published) | / ♂ / LL TF / / | Mirror 30×30 cm | / | Patient alone Home-based | 20 sessions 4 weeks 5 per week 15 min session duration / | 5 min per exercise 3 exercises 1 set / Opening and closing the healthy foot Rotating the ankle inward Rotation of the ankle outward | / | VAS |
| Baker48 2008 USA | RCT Protocol (Not published) | / ♂♀ / UL/LL / / / | Mirror | Healthy subjects | / / | 20 sessions 4 weeks 5 per week 15 min session duration (20 for TF patients) / | 5 min per exercise 3 exercises 1 / Ankle flexion / extension Moved the foot from side to side (“windshield wiper”) Rotated the foot in a circle (“as if drawing a circle with your toes”) For TF amputees: Knee flexion / extension | / | VAS SF-MPQ |
"/" was noted if the information was not provided or not presented in the study; ♂, male; ♀, female; AD, ankle disarticulation; BPI, Brief Pain Inventory; HD, hip disarticulation; IPT-R, Revised Iowa Pain Thermometer; LL, lower limb; MPI, Multidimensional Pain Inventory; MPQ, McGill Pain Questionnaire; MT, mirror therapy; NRS, Numeric Pain Rating Scale; PAD, peripheral artery disease; PLP, phantom limb pain; RCT, randomized controlled trial; SD, shoulder disarticulation; SF-MPQ, Short-form McGill Pain Questionnaire; STD, scapulo-thoracic disarticulation; tDCS, transcranial direct current stimulation; TENS, transcutaneous electrical nerve stimulation; TF, transfemoral; TH, transhumeral; TK, through knee; TR, traumatic; TRU, transradio-ulnar; TT, transtibial; UL, upper limb; UPS, Universal Pain Score; VAS, visual analogic scale
The most common intervention duration was four weeks, used in 34.1 % of the studies (n = 15).19,21,23,49–51,54,55,58–62,66,70 Thirty-four percent of the studies (n = 15) reported the duration of the intervention being less than 4 weeks, ranging from 1 to 21 days.22,24,34,35,40–42,46,47,52,54,56,57,63,63 Twenty-five percent of the studies (n = 11) reported a duration of more than 4 weeks, ranging from 6 to 24 weeks.15,20,36,38,39,43,44,64,67–69 Intervention length was not reported in 7 % of the studies (n =3).45,53,65
FrequencyFrequency of intervention was described in 84 % of the studies15,19,21–24,35,37–52,54,55,57–60,62–65,67–70 (n = 37). Reported frequencies range from 12 sessions per day52 to 1 session per week.44,67 The most common frequency was 1 MT session per day, reported in 41 % (n = 18) of studies.19,21–23,38,39,48–50,54,57–60,62,64,68,70 Two sessions per day was reported in 14 % of the studies (n = 6).15,24,37,47,51,65 Seven sessions per week was used in 7 % of the studies (n = 3),41,55,69 and 1 study reported using four sessions per week.45 Frequency was not reported in 16 % of the studies (n=7).20,34,36,53,56,61,66
A change in the frequency of sessions was used in 9 % of the studies (n = 4).19,43,45,46 For example, Darnall et al.43 used a protocol with five sessions per week for the first month, followed by three sessions per week for the next two months. MacLachlan's protocol46 was even more complex. In the first week, patients underwent two assisted sessions per day with a therapist for five days, followed by two independent sessions per day during the weekend. In the second week, patients completed two assisted sessions per day with a therapist, along with two to three independent sessions per day, and three to four daily independent MT sessions during the weekend. In the third week, a patient completed two to three daily MT sessions on their own.
Session lengthApproximately 45 % of the included studies (n = 20)19,21,23,36,40,45,47–50,55,57–60,62,63,68–70 reported MT sessions lasting 15 min. Another 25 % of the studies (n = 11)15,20,22,24,37,38,41,43,53,54,66 reported session duration between 20 and 30 min, and 4 studies39,56,64,65 used 10 min sessions. Modifications to the duration of sessions within a study were reported in 2 studies.43,52 For example, Darnall et al.43 suggested a session duration of 20 to 30 min in the first month and 30 min for the next two months. Limakatso et al.52 used a decreasing approach, starting with 30 min sessions at the hospital followed by 10 min sessions at home. Other reported session durations include five minutes,51 and 40 min.61 Duration was either not reported or unclear in 16 % of the studies (n = 7).34,35,42,44,46,67
Number of exercises per sessionThe number of exercises varied from 1 to 10 with the most common being 3 exercises in 18 % of the studies (n = 8).47,48,50,58,63,64,67,70 Half of the studies included 3, 5, or 6 different exercises (Table 2). For detailed exercise content, see the exercise detail paragraph and Table 2. Notably, 41 % of the studies (n = 18)20,21,35,36,38,39,41,44,45,52,54,56,57,60–62,65,68 did not report the number of exercises in their protocol.
Time duration per exerciseOnly 18 % of the studies (n = 8) detailed the time allocated per exercise, ranging from 30 s to 5 min.37,40,42,48,51,58,59,70 For instance, Chan et al.58 outlined three exercises, each lasting five minutes for the lower limb, while Foell et al.59 described five exercises, each lasting three minutes. However, time duration per exercise was not described in 86.7 % of the studies (n = 36).15,19–24,34–36,38,39,41,43–47,49,50,52–57,60–69 For example, Wilcher et al.47 reported that the duration of the MT session should be around 15 min and should include movements such as biceps curls, opening and closing the fist, pronating and supinating the outstretched ‘arms’,47 without further detail. Because execution duration varies between participants, specificity may be lacking. Clinicians may prefer detailing repetitions instead.
RepetitionsPatients often inquire about the repetition of movements. Because describing the duration of each exercise can be challenging, documenting the number of repetitions could help in standardizing protocols. Unfortunately, this detail is inconsistently documented, with the number of repetitions described in only 16 % of the studies (n = 7).34,35,46,62,64,67 For instance, both studies by Houston et al.60,62 outlined 15 repetitions per movement. The study by Thomas67 reported the highest number of repetitions, with the patient performing two series of 40 repetitions for wrist and elbow movements during the first five weeks of treatment. Afterward, the patient added movements within the frontal plane (ulnar and radial deviation) with the same repetition count. The remaining four studies23,34,46,64 report using 10 repetitions per movement.
Follow-upFollow-up was described in 43 % of the studies (n = 20).15,19,22,24,35,38,39,43,44,50–53,55,58–60,62,64,69 The time period varied from 2 weeks59 up to 2 years,64 with 6 studies15,19,24,35,44,52 reporting a follow-up period of six months. However, 54 % of the studies (n = 24)20,21,23,34,36,37,40–42,45–49,54,56,57,61,63,65–68,70 did not report this information (Table 2).
Place of practiceMT was administered either at the Hospital (41 % of the studies, n = 18),21,22,24,34,36,37,39,41,44,46,49,54–57,63,64 or home-based (18 %, n = 8).19,38,43,51,59,66,69,70 In 16 % of the studies (n = 7),20,45,50,52,53,61,65 the setting changed starting at the hospital and continuing at home. However, the setting was not specified in 25 % of the studies (n = 11).15,23,35,42,47,48,58,60,62,67,68
TailoringIn terms of practice, 32 % of the studies (n = 14)20,21,34,36,37,40,42,44,49,55,57,63,64 indicated that MT was administered according to the therapist's guidance. In 23 % (n = 10),19,38,39,43,51,56,59,66,69,70 patients conducted MT independently. Notably, in 11 % (n = 5),41,46,50,52,61 the approach shifted from therapist-supervised sessions to independent patient-led sessions.41,46,50,52,66 However, 32 % of the studies (n = 14)15,23,24,35,45,47,48,53,54,58,60,62,65,68 did not provide this information.
ComparatorsSeven different comparators are reported in 48 % of the studies (n = 21).19–24,34–36,40,42,48–55,58,69 The most common were (i) covered/obscured mirror34,36,40,49,50,55 and (ii) mental visualization,19,36,49,53,69 followed by the standard physical therapy treatment.23,35,52,70 Other comparators like tactile discrimination of the residual limb,51 sensorimotor exercise of the intact limb,20 transcutaneous electrical nerve stimulation,54 and transcranial direct current stimulation (TDCS)22 were reported once (Table 2).
Exercise descriptionTable 3 summarizes session content, including motor and sensory exercises. Our scoping review found that exercises were not reported in 31 % of the studies (n = 14).20,21,35,36,38,40,41,44,45,53,54,61,65,68 All included studies described 15 lower limb motor exercises, encompassing mobility exercises for the hip, knee, foot, and toes. Foot flexion and extension were the most common exercises reported in 27 % of the studies (n = 12),19,22–24,34,37,43,46,48,51,58,64 foot rotation and inversion/eversion were reported in 16 % (n = 7), and knee flexion and extension were reported in six studies23,24,34,38,46,55 (i.e., referred to as straighten and bend in some publications). Additionally, 14 % of the studies (n = 6) instructed patients to move their limb without specific instructions.15,21,39,53,60,62
Presentation of the diversity of motor and sensory exercises description found in the literature.
For the upper limb, 14 movements were detailed, involving thumb to elbow mobility. No shoulder movements were described. The most common exercises were pronation/supination (11 % of the studies, n = 5)47,49,55,59,66 followed by elbow flexion/extension (9 %, n = 4),47,49,55,67 and opening/closing of the hand.66 Some exercises focused on functional tasks, such as “Touch the fingertips with the thumb; tracing figures with fingers” described by Foell et al.,59 or moving the hand toward and away from the mirror as used by Imaizumi et al.63
Sensory exercises were less prevalent, featured in 9 % of the studies (n = 4),15,19,43,50 all focused on the lower limb. Six different sensory exercises were identified, with four originating from Clerici et al.’s15 case report: looking at the limb, touching it, caressing it, and scratching it. Additionally, Darnall et al.62 described an exercise involving touching the big toe, and Anaforoğlu et al.19 detailed muscle relaxation following foot and ankle muscle contraction.
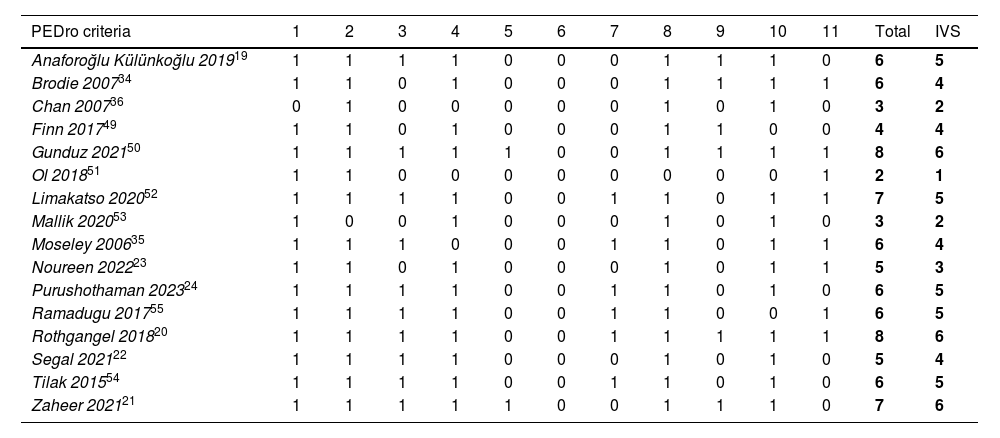
Methodological qualityMethodological assessment of the 16 included RCTs19–24,34–36,49–55 using the PEDro scale is reported in Table 4. The mean PEDro score was 5.5/10, with a standard deviation of 1.75. Only three studies34,42,50 received a score of six which corresponds to a high-quality study, while 9 studies19,22,24,34,35,49,52,54,55 obtained a score of 4 or 5 corresponding to a moderate quality study, and 4 studies23,36,51,53 were of poor quality with a score below 4.
PEDro evaluation for the randomized controlled trials included.
| PEDro criteria | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total | IVS |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Anaforoğlu Külünkoğlu 201919 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 6 | 5 |
| Brodie 200734 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 | 4 |
| Chan 200736 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 3 | 2 |
| Finn 201749 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 4 | 4 |
| Gunduz 202150 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 8 | 6 |
| Ol 201851 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 2 | 1 |
| Limakatso 202052 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 | 5 |
| Mallik 202053 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 3 | 2 |
| Moseley 200635 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 6 | 4 |
| Noureen 202223 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 | 3 |
| Purushothaman 202324 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 6 | 5 |
| Ramadugu 201755 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 6 | 5 |
| Rothgangel 201820 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 | 6 |
| Segal 202122 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 5 | 4 |
| Tilak 201554 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 6 | 5 |
| Zaheer 202121 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 7 | 6 |
IVS, internal validity score (i.e., the total score obtained by summing items 2 to 9).
Our findings revealed that significant heterogeneity exists in MT practice for treating PLP. Factors such as session frequency, duration, repetitions, and exercises vary widely. Despite the heterogeneity, MT practice tends to focus on daily sessions (i.e. between five to seven days a week) lasting about 15 min. However, there was a lack of details regarding the specific exercises performed, including time allocated per exercise, number, and repetitions, which vary considerably across studies. The effect of treatment on PLP was often assessed using VAS or NRS. Furthermore, the quality of included RCTs remains generally low, highlighting the need for improvement to enhance the credibility of MT implementation in clinical practice.16,17
It is worth noting that repetition plays a crucial role in the treatment, supported by evidence suggesting that better results in neurorehabilitation and plasticity are associated with early initiation of treatment, high intensity, and an active therapy.71 The short treatment duration (15 min) may stem from reported fatigue, but no comparative analysis of different durations has been conducted to find the optimal MT dose-effect ratio.
Most exercises described in MT focused on the distal limb region like the hand and foot, with fewer proximal and functional movements documented, possibly due to challenges with patients having high amputation levels. These exercises primarily involved motor functions such as limb movement in an analytic manner (e.g., flexion/extension), with sensory exercises less commonly reported.15,19,43,50 However, sensory exercises hold potential for reducing PLP magnitude.72 Incorporating movements in the presence of the limb generates numerous efferent and afferent signals, which may enhance MT efficacy for PLP by closing the sensory-motor loop and providing feedback, even indirectly from the deafferented limb.
The study's primary strength lies in methodological adherence to guidelines like PRISMA-Scr and JBI,27,28 ensuring rigor and comprehensiveness. A broad study selection encompassing all study designs using MT for PLP treatment makes it possibly the most exhaustive investigation on the topic to date. However, limitations exist. The research strategy could have been enhanced by exploring additional databases and validating search equations with a professional librarian. The exclusion of grey literature and preprints from appropriate databases may have overlooked valuable insights from studies not accepted by peer-reviewed journals. Language constraints also limit the study, eligibility criteria included articles wrote in English and French only, but no studies were found in French. Articles in other languages encountered during the literature search as Chinese or Turkish could have offered additional content, but language barriers prevented inclusion as reviewers lacked those language proficiencies. Additionally, when disagreements arose, resolution involved discussion between the two reviewers without consulting a third party, which may have led to some misinterpretations.
PerspectivesWhile MT shows promise in non-invasive therapy for cortical maladaptation,59,73 alternative approaches should be considered to tailor treatment to individual patient needs. The true effect size of MT may be overestimated, and limitations could arise due to its restricted range of motion. Other non-invasive methods like sensory discrimination,72 TENS,74 hypnosis,75 vibration therapy,76 and acupuncture77 show promise, but evidence supporting their efficacy is limited. Ongoing research explores novel approaches like virtual reality.78–83 Integrating these techniques rather than viewing them as competing modalities could benefit patients. MT could serve as an initial step followed by VR-MT, leveraging virtual reality's advantages in diverse exercises and enhancing engagement. VR could be particularly useful for patients facing challenges using a real mirror due to unresolved feelings about their amputation. It enables the modeling of a simplified arm, whose movements and appearance are enough to create an illusion and alleviate PLP. However, research in this field remains limited to case studies and case series,78–84 necessitating further investigation with higher levels of evidence.
Invasive approaches for alleviating PLP are also used. Techniques like deep brain stimulation,85 targeted muscle reinnervation (TMR),86 targeted sensory reinnervation (TSR),87,88 Regenerative Peripheral Nerve Interface (RPNI),89–91 and Agonist-antagonist Myoneural Interface (AMI)89,92 show promising results. Combining invasive and non-invasive methods may offer favorable outcomes, allowing selection from various therapeutic approaches to accommodate individual patient preferences.
ConclusionTo enhance MT's effectiveness for PLP, rigorous RCTs or single case experimental design (SCED) trials are crucial. Standardised RCT protocols can minimize confounding factors, while comparing MT to a placebo may help clarify its effects and establish efficacy.93 Alternatively, SCEDs offer personalized approaches, identifying patient subgroups for precise treatment.94,95 A significant gap is the insufficient description of MT interventions, hindering replication of this intervention in clinical practice. Authors are encouraged to provide detailed information about MT interventions to facilitate implementation by clinicians. Patient adherence is often overlooked, impacting outcomes. Interventions, including home-based ones, lacked adherence assessment, leaving treatment fidelity unclear. Future research should incorporate tools like phone calls, messages, or web applications to monitor adherence effectively. Follow-up assessments are crucial for evaluating MT's long-term effects. Many studies lacked data beyond immediate post-treatment, hindering the assessment of sustained benefits. Including three to six months follow-ups could provide valuable information about long term effectiveness. Current works tend to take the direction of 15 min daily MT sessions involving sensory-motor movements of the distal limb. This appears to be well-tolerated by patients and supports the implementation of home-based MT programs. This framework should now guide future interventions and research program to be able to establish the size effect of MT.
The authors would like to thank Jérome Arnaud, Johana Roberston, Jonathan Stammers, and Theresa Mae Maliksi for their help for the redaction of the manuscript in English. Matthieu Guémann received a post-doctoral grant from the French Direction Générale de l'Armement (DGA) to conduct this work.