To determine the effectiveness of mechanical diagnosis and therapy (MDT) in patients with chronic low back pain (CLBP) compared to other traditional physical therapy interventions.
MethodsRandomized controlled trials investigating the effect of MDT compared to other traditional physical therapy interventions in individuals with CLBP were considered eligible. For the purpose of this review, MDT was compared to active and passive physical therapy interventions. Independent reviewers assessed the eligibility of studies, extracted data, and assessed the risk of bias. The primary outcomes investigated were pain and disability.
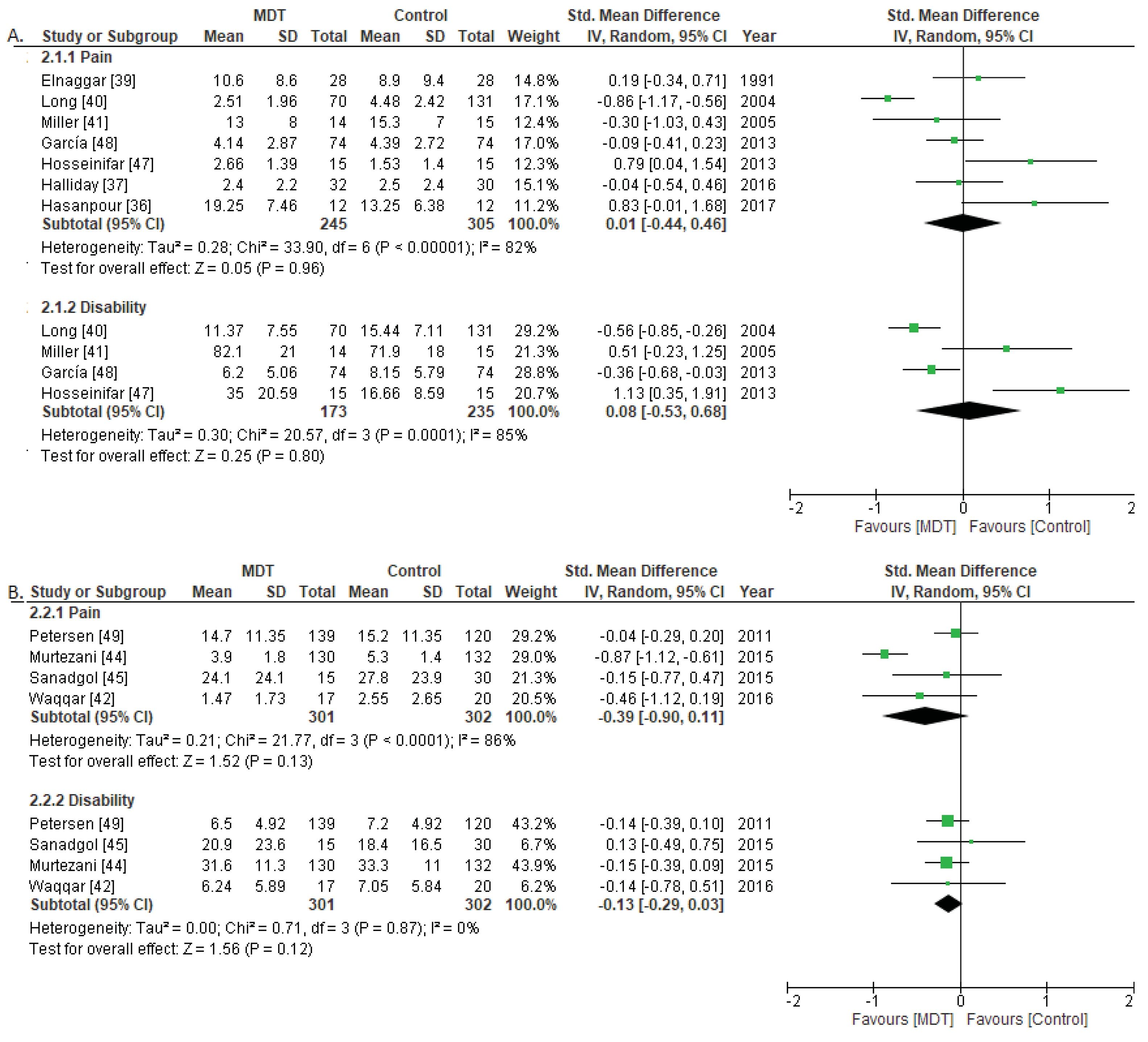
ResultsFourteen studies were included in the review. Of these, 11 provided data to be included in the meta-analyses. Our findings showed that MDT was no more effective in decreasing pain (standardized mean difference [SMD]=0.01, 95% confidence interval [CI]: −0.44, 0.46) and disability (SMD=0.08, 95% CI: −0.53, 0.68) than other active treatments. Similar results were found when comparing MDT to other passive treatments for pain (SMD=−0.39, 95% CI: −0.90, 0.11) and disability (SMD=−0.13, 95% CI: −0.29, 0.03).
ConclusionThere is low to moderate quality evidence that MDT is not superior than other traditional physical therapy interventions in improving pain and disability in people with CLBP.
Chronic low back pain (CLBP) is a primary cause of pain, functional limitations, and disability worldwide.1,2 Prevalence estimates for CLBP vary considerably between studies, accounting for 11.9% as current prevalence, 38% as 1-year prevalence, and 38.9% as lifetime prevalence.3,4 Consequently, CLBP poses a substantial economic burden on healthcare, social, and welfare systems.5–7
The diagnosis and treatment of CLBP are well discussed topic in recent decades.8,9 A range of intervention strategies have been investigated, including active and passive strategies provided in isolation or in combination.10 A common reason for the lack of effectiveness for conventional treatments is that non-specific CLBP is broadly defined and rarely has a confirmed diagnosis.11 In addition, there is still no established classification system for patients with CLBP, because most classifications lack solid evidence of validity and reliability.12,13
In this context, some authors have suggested that the McKenzie method, also known as mechanical diagnosis and therapy (MDT) method, may be a suitable approach to treat CLBP.14,15 Although MDT has been commonly referred to as a treatment based on extension exercises, it actually consists of a treatment method based on a comprehensive diagnosis classification system, which includes three mechanical syndromes (Derangement, Dysfunction, and Postural) and an “Others” subgroup. Among those, derangement is by far the most common syndrome in patients with CLBP.16 This syndrome is characterized by quick mechanical and symptomatic changes secondary to performance of a directional-preference exercise. This directional preference is defined as the direction of a repeated movement and/or sustained position that induces mechanical and symptomatic improvement. Symptomatic improvements may include centralization,17–20 in which symptoms are progressively and permanently abolished in a distal-to-proximal direction, suggesting a good prognosis. Therefore, with the MDT approach, individuals with CLBP can be classified in one of the four groups, based on which specific treatment may be implemented.
Numerous authors have appraised the effects of MDT in individuals with CLBP.15,21–24 A previous systematic review, published in 2006, concluded that the effectiveness of MDT could not be estimated.25 More recently, another systematic review concluded that there is moderate-to-high-quality evidence that MDT is superior to other rehabilitation interventions in reducing pain and disability.26 However, the favorable results favoring MDT reported in this review, may have been due to the type of comparator used in the meta-analysis. To our knowledge, comparing the MDT approach to other active or passive physical therapy treatment approaches has not previously been done. Therefore, this systematic review with meta-analysis investigated the effectiveness of MDT compared to other active or passive physical therapy interventions in individuals with CLBP.
MethodsProtocol and registrationThis systematic review protocol was registered on PROSPERO (registration number: CRD42017080795) and adhered to the PRISMA recommendations and followed the recommendations from the Cochrane Collaboration.27,28
Search strategyElectronic searches were performed using the following databases: Medline (via PubMed), Embase, Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials (CENTRAL), Web of Science, Web of Knowledge, SCOPUS, CINAHL (via EBSCO), ProQuest, and PEDro. Additionally, manual searches on reference lists of previously published systematic reviews and relevant trials were conducted. The reference list from the McKenzie International Institute (www.mckenzieinstitute.org/clinicians/research-and-resources/references-list) was also screened. No time limit was set, and all studies that existed until March 2018 were considered for inclusion.
The search strategy for each database was developed by combining the relevant terms from each of the following three conceptual areas: MDT, non-specific CLBP, and clinical trial. The search strategy used in MEDLINE is available as supplemental online material.
Eligibility criteriaArticles were eligible for inclusion if they were randomized controlled trials; included participants with CLBP (i.e., defined as chronic pain in the lumbar spine lasting more than 12 weeks) with or without radiation to the lower extremities; the experimental group received MDT-based exercises only (trial specifies treatment according to the MDT principles) and the comparison group received a form of physical therapy intervention other than MDT-based exercises. Lastly, the studies had to be written in English, French, Spanish, Portuguese, Italian, Bulgarian, or Russian. Trials were excluded if the recruited participants had any specific spinal pathology (such as lumbar radiculopathy), if the participants’ symptoms were acute or subacute, or if it was not clearly indicated in the study that the participants’ symptoms were chronic.
Study selectionTwo reviewers (E.S.S and S.G.G) conducted the study selection process, defined prior to the beginning of the review, which included a checklist with the eligibility criteria. The results of the searches were transferred into an electronic reference manager (Mendeley Desktop, version 1.17.9), which eliminated duplicate entries. Two reviewers independently screened the titles, abstracts, and full-texts of potentially eligible studies for inclusion into this review. Disagreements or discrepancies were resolved by a third reviewer (J.M.B).
OutcomesPrior to the quantitative synthesis, the results were extracted and categorized based on the outcomes of interest. The primary outcomes were pain, as measured with the McGill Pain Questionnaire,29 disability, and lumbar range of motion (ROM). Secondary outcomes of interest included quality of life, recurrence, return to work/sick leave, medical visit, medication use, or global perceived effect.
Assessment of risk of biasThe PEDro scale was used to evaluate the methodological quality of the included studies. Studies were categorized into high (score 3/10 or lower), moderate (score 4/10 or 5/10), or low (score 6/10 or higher) risk of bias. Agreement between the two reviewers (E.S.S and S.G.G) was evaluated using Cohen's kappa coefficients and any disagreement or discrepancies were resolved through consensus by a third reviewer (J.M.B).
Data synthesis and strength of the evidenceFirst, a descriptive synthesis was performed. To summarize the characteristics of the included studies, we extracted the following data: study design, sample characteristics (i.e., number, mean age, and sex of participants), control and intervention groups, and scoring systems used to assess the predefined outcome measures. Subsequently, we performed a quantitative synthesis with meta-analysis.30 To do so, we summarized the evidence according to the type of experimental and control interventions used in the trials, and also to the time points used for outcome assessment (follow-up points). An intervention was classified as experimental when it included treatment based on MDT as the differentiating therapy. The control interventions were divided into two groups: active and passive treatment approaches. In the active treatment approach, participants played an active role as they performed some form of active exercise (e.g., Pilates), while in the passive treatment approach, participants received the treatment from the physical therapist (e.g., manual therapy). For trials testing more than two interventions, the control group included in the meta-analysis was the one that did not include MDT as part of the treatment or data from the control groups were combined. The Review Manager 5 software, from the Cochrane Collaboration, was used to conduct the meta-analysis. Time points of assessment were categorized as follows: short-term (less than three months after randomization), intermediate-term (at least three months but less than 12 months after randomization), and long-term (12 months or more after randomization). When there were multiple time points that fell within the same category we used the one that was closer to the end of the treatment, six months, and 12 months. Mean, standard deviation, and sample size from each group were extracted and used in the data analysis to estimate effect sizes. If these data were not available, estimations were based on t- and p-values. Because different scoring systems were used to assess the same outcome measures, effect sizes were estimated and presented using standardized mean difference (SMD). Cut-off points for interpreting the result are usually dependent on the type of intervention. However, the arbitrary thresholds established are generally accepted and allow interpretation of the magnitude of the pooled effects. Accordingly, the pooled effects were interpreted as small (SMD<0.2), moderate (0.2<SMD<0.8), or large (SMD>0.8).31 The meta-analysis was performed using the random effect model, assuming that the true effect may vary due to heterogeneity in the study design. Heterogeneity assessment was based on I2 statistics, and considered moderate to high when greater than 50%.32 The summary value for each study was represented in forest plots. Confidence intervals (CI) were set at 95%.
To determine the quality of evidence, the Grade of Recommendation Assessment, Development, and Evaluation (GRADE) approach was applied, as recommended in the Cochrane Handbook for Systematic Reviews of Interventions32 and adapted in the updated Cochrane Back Review Group method guidelines.33 The GRADE scale shows the overall certainty of the evidence for the outcome being reviewed and following assessment of five domains: risk of bias (downgraded if more than 25% of the participants were from studies with low methodological quality), inconsistency of results (downgraded if significant heterogeneity was present by visual inspection or if the I2 value was greater than 50%), indirectness (generalizability of the findings, downgraded if more than 50% of the participants were outside the target group), imprecision (downgraded if fewer than 400 participants were included in the comparison), and other factors such as reporting bias or publication bias. The GRADE approach involves downgrading the evidence from high quality to moderate, to low, or to very low, based on the cumulative assessment of each of these criteria. The GRADE scale was applied to assess the evidence regarding the outcome measures “pain” and “disability”. Two authors independently reviewed and scored each study, with disagreements settled through discussion and consensus.
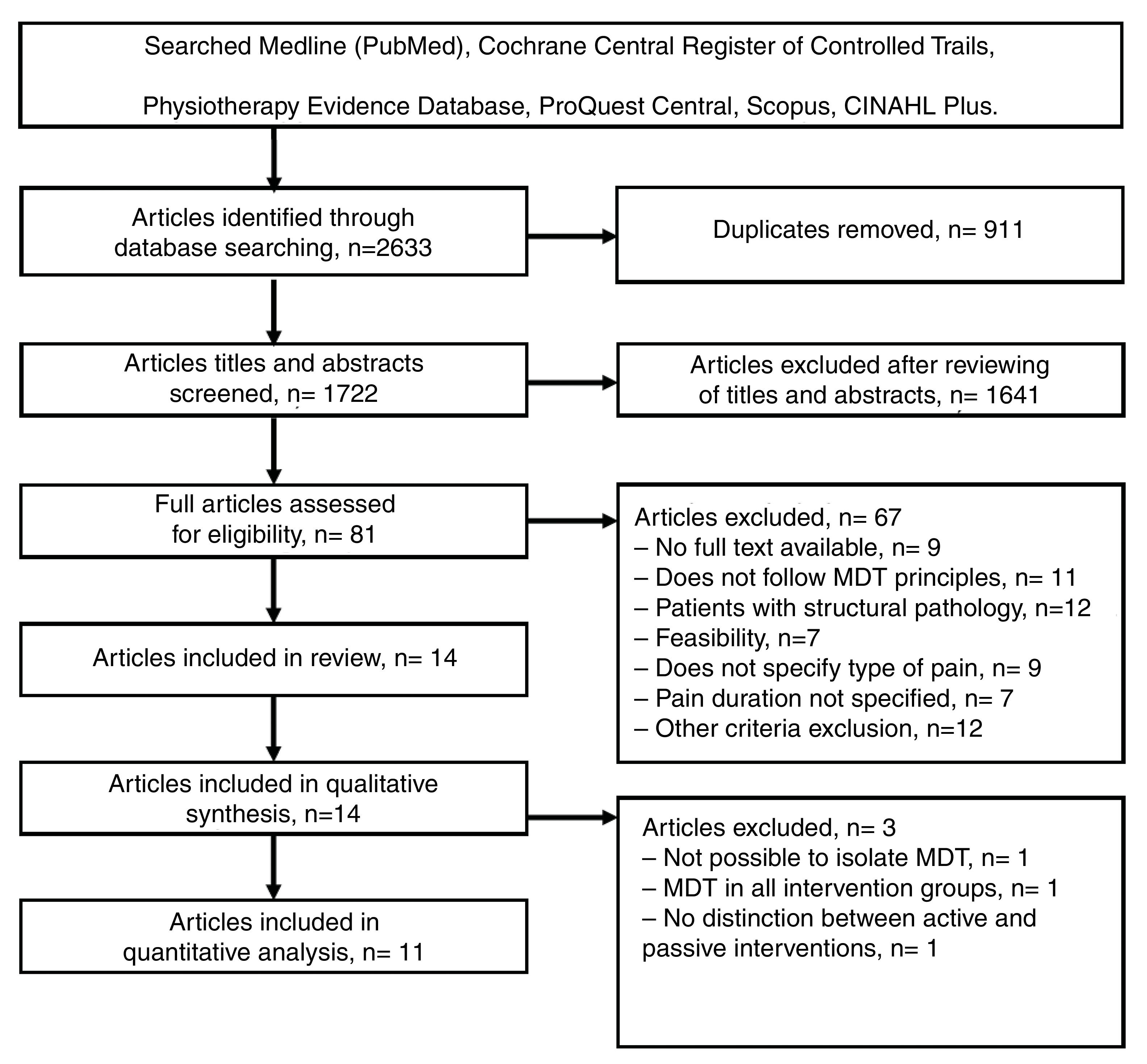
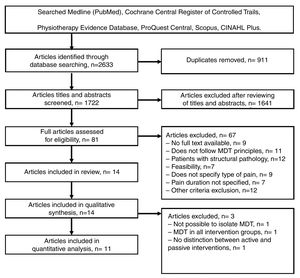
ResultsStudy selectionFig. 1 shows the flow diagram of the studies considered in the review. The initial database search resulted in a total of 2633 articles. After removing duplicates and screening titles and abstracts, 14 studies34–47 were included. Of these, 11 studies provided data to be included in the meta-analyses. Three studies36,41,44 were not included in the meta-analyses because MDT was used in all arms of the trial36,44 or the control group used a combination of active and passive treatments (Fig. 2).41
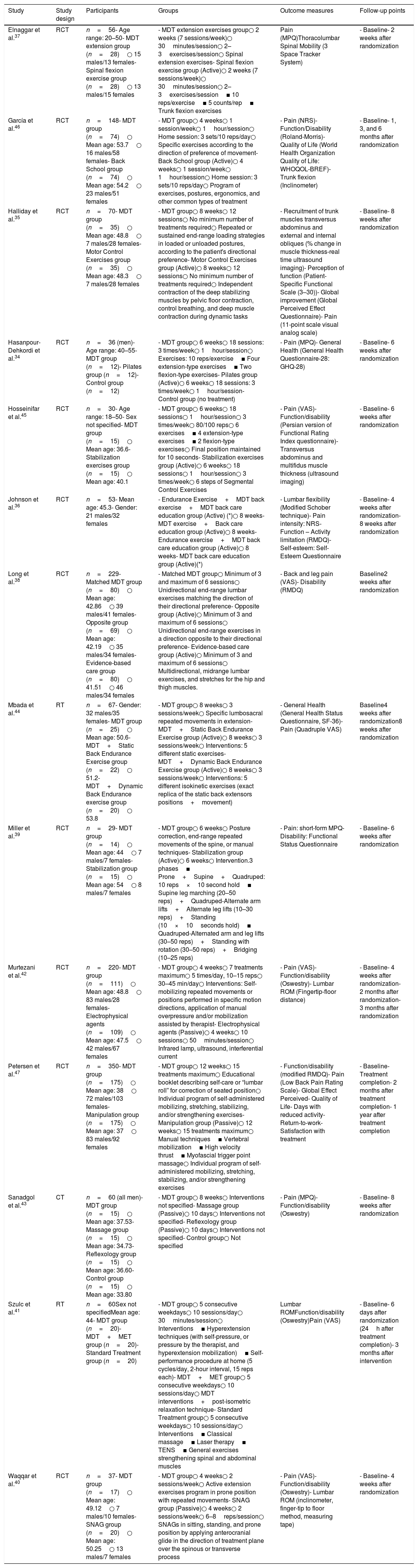
Study characteristicsThe studies characteristics are shown in Table 1. The following information was extracted from each study: study design, participants, groups, outcome measures, and follow-up points.
Characteristics of the included studies.
| Study | Study design | Participants | Groups | Outcome measures | Follow-up points |
|---|---|---|---|---|---|
| Elnaggar et al.37 | RCT | n=56- Age range: 20–50- MDT extension group (n=28)○ 15 males/13 females- Spinal flexion exercise group (n=28)○ 13 males/15 females | - MDT extension exercises group○ 2 weeks (7 sessions/week)○ 30minutes/session○ 2–3exercises/session○ Spinal extension exercises- Spinal flexion exercise group (Active)○ 2 weeks (7 sessions/week)○ 30minutes/session○ 2–3exercises/session ▪ 10 reps/exercise ▪ 5 counts/rep ▪ Trunk flexion exercises | Pain (MPQ)Thoracolumbar Spinal Mobility (3 Space Tracker System) | - Baseline- 2 weeks after randomization |
| García et al.46 | RCT | n=148- MDT group (n=74)○ Mean age: 53.7○ 16 males/58 females- Back School group (n=74)○ Mean age: 54.2○ 23 males/51 females | - MDT group○ 4 weeks○ 1 session/week○ 1hour/session○ Home session: 3 sets/10 reps/day○ Specific exercises according to the direction of preference of movement- Back School group (Active)○ 4 weeks○ 1 session/week○ 1hour/session○ Home session: 3 sets/10 reps/day○ Program of exercises, postures, ergonomics, and other common types of treatment | - Pain (NRS)- Function/Disability (Roland-Morris)- Quality of Life (World Health Organization Quality of Life: WHOQOL-BREF)- Trunk flexion (Inclinometer) | - Baseline- 1, 3, and 6 months after randomization |
| Halliday et al.35 | RCT | n=70- MDT group (n=35)○ Mean age: 48.8○ 7 males/28 females- Motor Control Exercises group (n=35)○ Mean age: 48.3○ 7 males/28 females | - MDT group○ 8 weeks○ 12 sessions○ No minimum number of treatments required○ Repeated or sustained end-range loading strategies in loaded or unloaded postures, according to the patient's directional preference- Motor Control Exercises group (Active)○ 8 weeks○ 12 sessions○ No minimum number of treatments required○ Independent contraction of the deep stabilizing muscles by pelvic floor contraction, control breathing, and deep muscle contraction during dynamic tasks | - Recruitment of trunk muscles transversus abdominus and external and internal obliques (% change in muscle thickness-real time ultrasound imaging)- Perception of function (Patient-Specific Functional Scale (3–30))- Global improvement (Global Perceived Effect Questionnaire)- Pain (11-point scale visual analog scale) | - Baseline- 8 weeks after randomization |
| Hasanpour-Dehkordi et al.34 | RCT | n=36 (men)- Age range: 40–55- MDT group (n=12)- Pilates group (n=12)- Control group (n=12) | - MDT group○ 6 weeks○ 18 sessions: 3 times/week○ 1hour/session○ Exercises: 10 reps/exercise ▪ Four extension-type exercises ▪ Two flexion-type exercises- Pilates group (Active)○ 6 weeks○ 18 sessions: 3 times/week○ 1hour/session- Control group (no treatment) | - Pain (MPQ)- General Health (General Health Questionnaire-28: GHQ-28) | - Baseline- 6 weeks after randomization |
| Hosseinifar et al.45 | RCT | n=30- Age range: 18–50- Sex not specified- MDT group (n=15)○ Mean age: 36.6- Stabilization exercises group (n=15)○ Mean age: 40.1 | - MDT group○ 6 weeks○ 18 sessions○ 1hour/session○ 3 times/week○ 80/100 reps○ 6 exercises ▪ 4 extension-type exercises ▪ 2 flexion-type exercises○ Final position maintained for 10 seconds- Stabilization exercises group (Active)○ 6 weeks○ 18 sessions○ 1hour/session○ 3 times/week○ 6 steps of Segmental Control Exercises | - Pain (VAS)- Function/disability (Persian version of Functional Rating Index questionnaire)- Transversus abdominus and multifidus muscle thickness (ultrasound imaging) | - Baseline- 6 weeks after randomization |
| Johnson et al.36 | RCT | n=53- Mean age: 45.3- Gender: 21 males/32 females | - Endurance Exercise+MDT back exercise+MDT back care education group (Active) (*)○ 8 weeks- MDT exercise+Back care education group (Active)○ 8 weeks- Endurance exercise+MDT back care education group (Active)○ 8 weeks- MDT back care education group (Active)(*) | - Lumbar flexibility (Modified Schober technique)- Pain intensity: NRS- Function – Activity limitation (RMDQ)- Self-esteem: Self-Esteem Questionnaire | - Baseline- 4 weeks after randomization- 8 weeks after randomization |
| Long et al.38 | RCT | n=229- Matched MDT group (n=80)○ Mean age: 42.86○ 39 males/41 females- Opposite group (n=69)○ Mean age: 42.19○ 35 males/34 females- Evidence-based care group (n=80)○ 41.51○ 46 males/34 females | - Matched MDT group○ Minimum of 3 and maximum of 6 sessions○ Unidirectional end-range lumbar exercises matching the direction of their directional preference- Opposite group (Active)○ Minimum of 3 and maximum of 6 sessions○ Unidirectional end-range exercises in a direction opposite to their directional preference- Evidence-based care group (Active)○ Minimum of 3 and maximum of 6 sessions○ Multidirectional, midrange lumbar exercises, and stretches for the hip and thigh muscles. | - Back and leg pain (VAS)- Disability (RMDQ) | Baseline2 weeks after randomization |
| Mbada et al.44 | RT | n=67- Gender: 32 males/35 females- MDT group (n=25)○ Mean age: 50.6- MDT+Static Back Endurance Exercise group (n=22)○ 51.2- MDT+Dynamic Back Endurance exercise group (n=20)○ 53.8 | - MDT group○ 8 weeks○ 3 sessions/week○ Specific lumbosacral repeated movements in extension- MDT+Static Back Endurance Exercise group (Active)○ 8 weeks○ 3 sessions/week○ Interventions: 5 different static exercises- MDT+Dynamic Back Endurance Exercise group (Active)○ 8 weeks○ 3 sessions/week○ Interventions: 5 different isokinetic exercises (exact replica of the static back extensors positions+movement) | - General Health (General Health Status Questionnaire, SF-36)- Pain (Quadruple VAS) | Baseline4 weeks after randomization8 weeks after randomization |
| Miller et al.39 | RCT | n=29- MDT group (n=14)○ Mean age: 44○ 7 males/7 females- Stabilization group (n=15)○ Mean age: 54○ 8 males/7 females | - MDT group○ 6 weeks○ Posture correction, end-range repeated movements of the spine, or manual techniques- Stabilization group (Active)○ 6 weeks○ Intervention.3 phases ▪ Prone+Supine+Quadruped: 10 reps×10 second hold ▪ Supine leg marching (20–50 reps)+Quadruped-Alternate arm lifts+Alternate leg lifts (10–30 reps)+Standing (10×10seconds hold) ▪ Quadruped-Alternated arm and leg lifts (30–50 reps)+Standing with rotation (30–50 reps)+Bridging (10–25 reps) | - Pain: short-form MPQ- Disability: Functional Status Questionnaire | - Baseline- 6 weeks after randomization |
| Murtezani et al.42 | RCT | n=220- MDT group (n=111)○ Mean age: 48.8○ 83 males/28 females- Electrophysical agents (n=109)○ Mean age: 47.5○ 42 males/67 females | - MDT group○ 4 weeks○ 7 treatments maximum○ 5 times/day, 10–15 reps○ 30–45 min/day○ Interventions: Self-mobilizing repeated movements or positions performed in specific motion directions, application of manual overpressure and/or mobilization assisted by therapist- Electrophysical agents (Passive)○ 4 weeks○ 10 sessions○ 50minutes/session○ Infrared lamp, ultrasound, interferential current | - Pain (VAS)- Function/disability (Oswestry)- Lumbar ROM (Fingertip-floor distance) | - Baseline- 4 weeks after randomization- 2 months after randomization- 3 months after randomization |
| Petersen et al.47 | RCT | n=350- MDT group (n=175)○ Mean age: 38○ 72 males/103 females- Manipulation group (n=175)○ Mean age: 37○ 83 males/92 females | - MDT group○ 12 weeks○ 15 treatments maximum○ Educational booklet describing self-care or “lumbar roll” for correction of seated position○ Individual program of self-administered mobilizing, stretching, stabilizing, and/or strengthening exercises- Manipulation group (Passive)○ 12 weeks○ 15 treatments maximum○ Manual techniques ▪ Vertebral mobilization ▪ High velocity thrust ▪ Myofascial trigger point massage○ Individual program of self-administered mobilizing, stretching, stabilizing, and/or strengthening exercises | - Function/disability (modified RMDQ)- Pain (Low Back Pain Rating Scale)- Global Effect Perceived- Quality of Life- Days with reduced activity- Return-to-work- Satisfaction with treatment | - Baseline- Treatment completion- 2 months after treatment completion- 1 year after treatment completion |
| Sanadgol et al.43 | CT | n=60 (all men)- MDT group (n=15)○ Mean age: 37.53- Massage group (n=15)○ Mean age: 34.73- Reflexology group (n=15)○ Mean age: 36.60- Control group (n=15)○ Mean age: 33.80 | - MDT group○ 8 weeks○ Interventions not specified- Massage group (Passive)○ 10 days○ Interventions not specified- Reflexology group (Passive)○ 10 days○ Interventions not specified- Control group○ Not specified | - Pain (MPQ)- Function/disability (Oswestry) | - Baseline- 8 weeks after randomization |
| Szulc et al.41 | RT | n=60Sex not specifiedMean age: 44- MDT group (n=20)- MDT+MET group (n=20)- Standard Treatment group (n=20) | - MDT group○ 5 consecutive weekdays○ 10 sessions/day○ 30minutes/session○ Interventions ▪ Hyperextension techniques (with self-pressure, or pressure by the therapist, and hyperextension mobilization) ▪ Self-performance procedure at home (5 cycles/day, 2-hour interval, 15 reps each)- MDT+MET group○ 5 consecutive weekdays○ 10 sessions/day○ MDT interventions+post-isometric relaxation technique- Standard Treatment group○ 5 consecutive weekdays○ 10 sessions/day○ Interventions ▪ Classical massage ▪ Laser therapy ▪ TENS ▪ General exercises strengthening spinal and abdominal muscles | Lumbar ROMFunction/disability (Oswestry)Pain (VAS) | - Baseline- 6 days after randomization (24h after treatment completion)- 3 months after intervention |
| Waqqar et al.40 | RCT | n=37- MDT group (n=17)○ Mean age: 49.12○ 7 males/10 females- SNAG group (n=20)○ Mean age: 50.25○ 13 males/7 females | - MDT group○ 4 weeks○ 2 sessions/week○ Active extension exercises program in prone position with repeated movements- SNAG group (Passive)○ 4 weeks○ 2 sessions/week○ 6–8reps/session○ SNAGs in sitting, standing, and prone position by applying anterocranial glide in the direction of treatment plane over the spinous or transverse process | - Pain (VAS)- Function/disability (Oswestry)- Lumbar ROM (inclinometer, finger-tip to floor method, measuring tape) | - Baseline- 4 weeks after randomization |
Abbreviations: MDT, mechanical diagnosis and treatment; rep(s), repetition(s); MPQ, McGill Pain Questionnaire; NRS, numerical rating scale; RMDQ, Roland Morris Disability Questionnaire; VAS, visual analog scale; ROM, range of motion; MET, muscle energy technique; TENS, transcutaneous electrical nerve stimulation; SNAG, Sustained Natural Apophyseal Glide.
Notes: (*) Endurance exercise: six types of exercises such as pelvic tilt, hamstring stretch, abdominals, spinal extensor muscles, cycling, and brisk walking-exercise for the general body; MDT exercise: series of either extension or flexion exercises; Back care education: education for standing, sitting, lifting, and other activities of daily living.
All studies included in this review compared MDT with different intervention strategies. Four studies40,42,43,47 compared MDT with passive treatments, such as massage and reflexology43 (data from both groups were combined in the meta-analysis), mobilization,40 manipulation,47 or electrophysical agents.42 Another seven studies34,35,37–39,45,46 compared MDT with active interventions such as back school education,46 stabilization exercises,39,45 motor control exercises,35 repeated lumbar flexion movements,37,38 or Pilates.34 In the study by Long et al.,38 the effects of MDT were compared with two different active interventions, so data from both controls were pooled for analysis. Finally, the remaining three studies,36,41,44 not included in the meta-analysis, combined MDT with other interventions such as endurance exercises, passive traditional interventions, and dynamic back exercises. In all included studies,34–47 the MDT directional preference was lumbar extension and participants were instructed on how to perform the exercises independently.
All studies34–47 assessed pain intensity over time. Eleven studies35,36,38–43,45–47 evaluated disability, six36,37,40–42,46 evaluated lumbar ROM, and four34,44,46,47 evaluated general health and quality of life. Treatment lasted from 10 days to 12 weeks, and all participants were adults, with an age ranging from 40 to 60 years. Regarding the time point of assessment, 11 studies34–40,42–45 assessed short-term, two studies41–46 intermediate, and one study47 long-term effect.
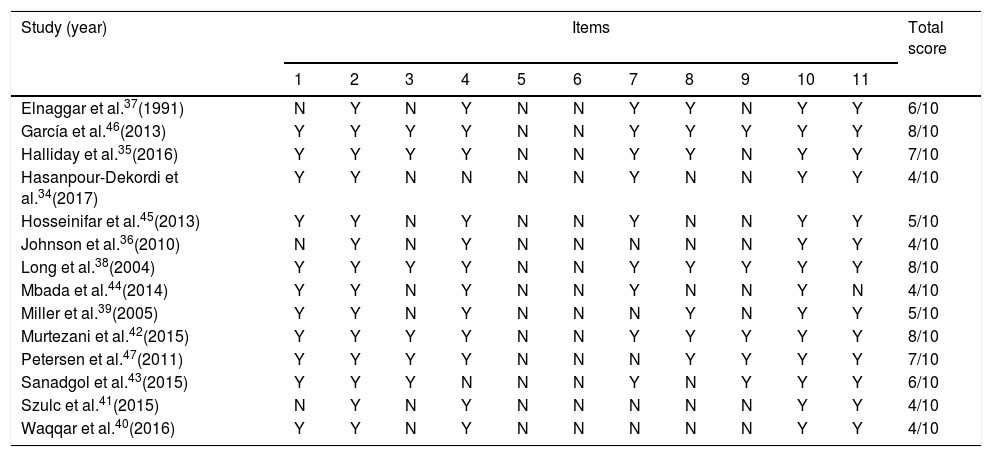
Quality assessment and risk of biasThe quality assessment and risk of bias is shown in Table 2. The kappa index for reliability between the two reviewers was high (k=0.76; 95% CI: 0.70, 0.82), indicating good reliability. The main disagreements between the two reviewers were related to the selection of the participants, the blinding of participants and assessors, the concealment of allocation, and the statistical analyses.
Summary of methodological quality of trials using the PEDro scale.
| Study (year) | Items | Total score | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | ||
| Elnaggar et al.37(1991) | N | Y | N | Y | N | N | Y | Y | N | Y | Y | 6/10 |
| García et al.46(2013) | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8/10 |
| Halliday et al.35(2016) | Y | Y | Y | Y | N | N | Y | Y | N | Y | Y | 7/10 |
| Hasanpour-Dekordi et al.34(2017) | Y | Y | N | N | N | N | Y | N | N | Y | Y | 4/10 |
| Hosseinifar et al.45(2013) | Y | Y | N | Y | N | N | Y | N | N | Y | Y | 5/10 |
| Johnson et al.36(2010) | N | Y | N | Y | N | N | N | N | N | Y | Y | 4/10 |
| Long et al.38(2004) | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8/10 |
| Mbada et al.44(2014) | Y | Y | N | Y | N | N | Y | N | N | Y | N | 4/10 |
| Miller et al.39(2005) | Y | Y | N | Y | N | N | N | Y | N | Y | Y | 5/10 |
| Murtezani et al.42(2015) | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8/10 |
| Petersen et al.47(2011) | Y | Y | Y | Y | N | N | N | Y | Y | Y | Y | 7/10 |
| Sanadgol et al.43(2015) | Y | Y | Y | N | N | N | Y | N | Y | Y | Y | 6/10 |
| Szulc et al.41(2015) | N | Y | N | Y | N | N | N | N | N | Y | Y | 4/10 |
| Waqqar et al.40(2016) | Y | Y | N | Y | N | N | N | N | N | Y | Y | 4/10 |
Abbreviations: Y, yes; N, no.
1, Eligibility criteria; 2, Random allocation; 3, Concealed allocation; 4, Baseline comparability; 5, Blind subjects; 6, Blind therapists; 7, Blind assessors; 8, Adequate follow-up; 9, Intention-to-treat analysis; 10, Between group comparisons; 11, Point estimates and variability.
Note: Eligibility criteria item does not contribute to total score.
From the 14 studies,34–47 six of them35,37,42,43,46,47 had a low risk of bias, and the remaining eight 34,36,38–41,44,45 had a moderate risk of bias. Incomplete outcome data or a non-specific description of the type of pain, as well as lack of blinding of participants due to the nature of clinical trials, were commonly reported.
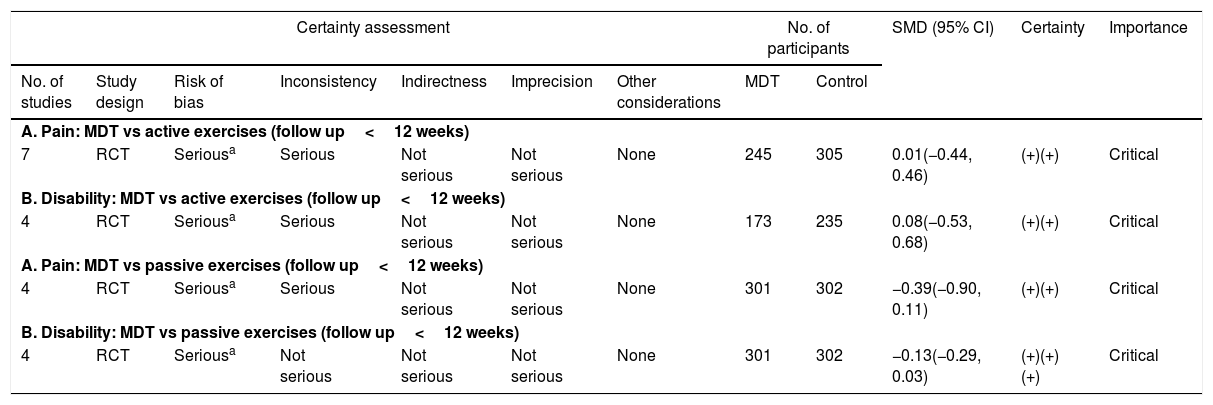
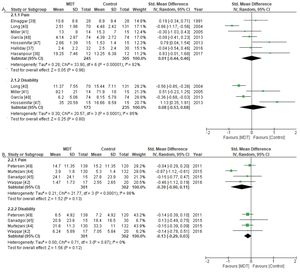
Meta-analysis and quality of evidenceA total of seven trials34,35,37–39,45,46 compared MDT with active treatments with follow-up assessment up to three months. The MDT approach was no more effective than active treatments for reducing pain (SMD=0.01; 95% CI: −0.44, 0.46) and disability (SMD=0.08; 95% CI: −0.53, 0.68). For pain intensity, based on seven trials,34,35,37–39,45,46 and for disability, based on four trials,38,39,45,46 the quality of evidence was downgraded due to inconsistency and risk of bias (Table 3). Therefore, the overall quality of evidence for both outcomes was considered to be low.
Summary of findings and quality of evidence (GRADE) for MDT versus active and passive treatments.
| Certainty assessment | No. of participants | SMD (95% CI) | Certainty | Importance | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | MDT | Control | |||
| A. Pain: MDT vs active exercises (follow up<12 weeks) | |||||||||||
| 7 | RCT | Seriousa | Serious | Not serious | Not serious | None | 245 | 305 | 0.01(−0.44, 0.46) | (+)(+) | Critical |
| B. Disability: MDT vs active exercises (follow up<12 weeks) | |||||||||||
| 4 | RCT | Seriousa | Serious | Not serious | Not serious | None | 173 | 235 | 0.08(−0.53, 0.68) | (+)(+) | Critical |
| A. Pain: MDT vs passive exercises (follow up<12 weeks) | |||||||||||
| 4 | RCT | Seriousa | Serious | Not serious | Not serious | None | 301 | 302 | −0.39(−0.90, 0.11) | (+)(+) | Critical |
| B. Disability: MDT vs passive exercises (follow up<12 weeks) | |||||||||||
| 4 | RCT | Seriousa | Not serious | Not serious | Not serious | None | 301 | 302 | −0.13(−0.29, 0.03) | (+)(+)(+) | Critical |
Abbreviations: CI, confidence interval; SMD, standardized mean difference; MDT, mechanical diagnosis and therapy; RCT, randomized controlled trial.
A total of four trials40,42,43,47 compared MDT with passive treatments with follow-up assessment up to three months. The MDT approach was no more effective than passive treatments for reducing pain (SMD=−0.39; 95% CI: −0.90, 0.11) or disability (SMD=−0.13; 95% CI: −0.29, 0.03). For pain intensity, the quality of evidence (downgraded due to risk of bias and inconsistency) was low. However, for disability, the overall quality of evidence (downgraded due to risk of bias) was considered to be moderate (Table 3).
Six studies36,37,40–42,46 assessed improvements in lumbar ROM. However, the characteristics of the included studies precluded meta-analysis. For two studies36,41 the interventions were not comparable, while for the remaining four studies,37,40,42,46 the authors used different approaches for assessing lumbar mobility. Two studies37,46 compared MDT with an active intervention by assessing sagittal, coronal, and transverse lumbar mobility versus overall trunk flexion; the other two40,42 compared MDT with a passive intervention, by assessing lumbar flexion versus fingertip to floor distance test. Therefore, a meta-analysis was not performed for this outcome.
Among the studies included in the meta-analysis, two46,47 assessed the outcomes three months or longer after randomization. But, one46 compared MDT versus an active intervention and the other one47 compared MDT versus a passive intervention; hence, it was not possible to perform meta-analysis for the immediate and long-term follow-up time points of assessment.
DiscussionThis systematic review appraised the available evidence on MDT for the treatment of CLBP and compared the effects of MDT with other active or passive treatment approaches. The meta-analysis, which included 11 studies, indicated that there is low to moderate evidence that the MDT method is no more effective than other active or passive physical therapy treatment approaches to reduce pain and improve disability in individuals with CLBP.
A previously published systematic review by Machado et al.25 found limited evidence for the use of MDT for CLBP. However, the studies included in that review indicate that MDT was applied using a “one size fits all” approach in heterogeneous samples with CLBP. Based on this conclusion, the authors highlighted the need to properly classify patients with CLBP before assigning them to treatment. Despite Machado et al.’s recommendations, subsequent studies included in our systematic review did not subgroup participants with CLBP following the principles of MDT classification system. Thus, the effectiveness of MDT for this population still remains unclear.
Within the principles of the MDT classification system, assessment is a key feature. It consists of a thorough history intake followed by a physical examination, where symptomatic, mechanical, and functional baselines are assessed and response to repeated end-range movements or postures are determined. The therapist then establishes whether a characteristic pattern can be recognized. Consequently, treatment with MDT is only possible when the correct syndrome (Derangement, Dysfunction, Postural) is correctly determined.16 In addition, in both Machado et al.’s and our systematic review, the prescribed MDT was mostly based on lumbar extension exercises, not systematically considering the patients’ directional preference. Equating lumbar extension movements to directional preference might lead to an inappropriate application of MDT principles.
Unlike our systematic review focused on people with CLBP, a recent systematic review by Lam et al.26 analyzed the effectiveness of MDT on people with both acute and CLBP. The authors concluded that there is moderate-to-high quality evidence that MDT is superior to other rehabilitation interventions for reducing pain and disability in patients with CLBP. In contrast, based on our results, we would argue that the effectiveness of MDT may depend on type of comparator used.26 In addition, the definitions of acute and CLBP are not well established in the literature, as reflected by the varied definitions used in studies that assess the effectiveness of MDT. This may account for the discrepancy in results. For instance, the Quebec Task Force defined chronic pain as pain lasting over 7 weeks,48 whereas the International Association for the Study of Pain (IASP) determined pain lasting more than 3 months as chronic. Furthermore, how the comparison group was defined in the study by Lam et al.26 may also explain the difference in the results regarding the effectiveness of MDT for CLBP. Another difference is that Lam et al.26 only included trials in which the therapist was previously trained in MDT, whereas we included all published trials that investigated the effectiveness of MDT regardless of the therapist qualification. We believe that the inclusion of all trials might ensure a better representation of the available MDT literature and prevent possible overestimation of MDT effects due to study selection bias.
The low number of included studies, the methodological differences among them, as well as their unexplained heterogeneity mean that the results obtained in this systematic review should be interpreted with caution. The differences reported in our systematic review may have occurred due to an inadequate study design as a consequence of the sampling method, the interventions applied, the duration of the interventions, and the time points of assessment across the included studies. Moreover, patient motivation is an external factor that may influence a patient's collaboration, and thus, outcomes when applying MDT. However, this factor was not considered among the included studies.
LimitationsThe language limits used as selection criteria may have led to potential selection bias, but considering the combined coverage of the various databases consulted and the inclusion of the most often used languages for scientific research dissemination, it has been minimized to a great extent. Despite the fact that the Cochrane Collaboration27,28 does not recommend the systematic use of outcome measures as part of the search strategy filters, we decided to use them as a consequence of the wide range of results that proved to be of interest in relation to the aims of the review. Cut-off thresholds used to interpret the effect size of interventions were those arbitrarily set by Cohen31; even when these are generally accepted, we recommend looking into the resultant SMD figures, while the statements about small, moderate, or high effects have been only provided to assist reading and allow comparability.
ConclusionsThe MDT approach is no more effective than other traditional physical therapy approaches in improving pain and disability in people with CLBP. Further research including more homogeneous samples that consider MDT classification subgroups is needed.
Conflict of interestPepe Guillart-Castells was an official instructor of the McKenzie Institute between 2015 and 2018.