The accurate diagnosis of pelvic floor muscle impairments is essential. The plethora of terms and the lack of evidence to support widely used pelvic floor muscle function (PFMF) measurements hinder diagnostic labels.
ObjectiveTo structure an examination of PFMF using visual observation and digital palpation and terms consistent with the ICF terminology, and to test its intra and interrater reliability/agreement.
MethodsA panel of 9 physical therapists applied Delphi method to structure the PFMF exam under ICF terminology and to verify its measurements reproducibility. For reliability and agreement, a convenience sample of women aged 51.2 ± 14.7 years had the sensitivity to pressure, pain, muscle tone, involuntary movement reaction, control of voluntary movement (contraction/relaxation), coordination, strength, and endurance examined by two raters, in the same day for interrater (n = 40), and one week apart, for intrarater reliability (n = 25). Percent agreement, linear weighted kappa, intraclass correlation coefficient, and Bland-Altman's limits of agreement were calculated (alpha = 0.05).
ResultsFour round Delphi discussion structured the PFMF exam, named EFSMAP (Exame das Funções Sensoriais e Motoras do Assoalho Pélvico/Examination of Pelvic Floor Sensory and Motor Functions), set a list of concepts and instructions targeted at reproducibility and established PFMF diagnostic labels. Reliability, except for pain and tone, were moderate to excellent (Kw= 0.67–1.0 and ICC=0.48–0.82). Agreement was substantial for most PFMF features (0.64–1.00), except pain.
ConclusionsThe EFSMAP was successfully developed as a valid and reliable exam to be used in research and clinical practice; it provides labels for the diagnosis of pelvic floor muscle impairments. It might be easily adopted worldwide as it uses ICF terminology.
The importance of physical therapy diagnosis has been promoted by the physical therapists (PT) scientific community, which advocates the need for diagnostic labels that reflect the body of knowledge of the physical therapy profession.1 As movement is a fundamental aspect of the role and identity of physical therapists, diagnostic labels should reflect movement analysis.1,2 A first attempt of a pelvic floor muscle (PFM) diagnosis system based on movement systems was made by Siptznagle et al.3 Also, albeit its flaws, the International Classification of Functioning, Disability and Health (ICF) of the World Health Organization (WHO) 4 provides a universal language and terminology based on human functionality including movement domain, that fosters communication and classification across the health care professions.2
Saltiel et al.5 have proposed the use of ICF terminology to organize 61 different terms referring to pelvic floor muscle function (PFMF) from a systematic review of PFMF tests of women with pelvic floor disorders (PFD) reported in literature.6 Through a valid linking process7 they reduced the number of terms to six muscle and movement related terms,5 described in ICF/Chapter :74 muscle tone, involuntary movement reaction, control of voluntary movement (contraction and relaxation), coordination, strength, and endurance. This terminology is grounded in neuromuscular physiology, motor control literature,8–10 and in a bio-psycho-social model that provides a comprehensive approach to human functionality.11 It aims to facilitate communication across disciplines and cultures and to gather data for clinical and research purposes among WHO-enrolled countries.
The International Continence Society (ICS) has been working on consensual terminology for "pelvic floor muscle function and dysfunction."12 In their recent report on PFM assessment,13 they noted a surplus of terms for similar functions6 and a lack of evidence supporting widely used assessments, particularly those relying on visual observation and digital palpation.13 The ICS recommended methodological studies to assess the accuracy of common PFM clinical methods, aiming to establish normative values and guide clinical practice and research.13 Women, at higher risk due to factors like parity, labor, and aging, may develop PFD such as urinary and anal incontinence and pelvic organ prolapses.14 Given the vital role of pelvic floor muscles (PFM) in urinary, anal, and sexual functions, and organ support, prompt PFM diagnosis in women is essential.
Therefore, given the need for diagnostic labels in the physical therapy profession1,2 and in Women’s Health physical therapy,3 the potential use of the ICF as a consensual terminology for these labels,2 and the need to provide evidence to support or abandon some PFMF assessments widely used in clinical practice and research,13 this study was designed to: structure a valid exam of all PFMF investigated in the literature using the ICF terminology,5 test reliability and agreement of those PFMF examined by visual observation and vaginal palpation by physical therapist in women with and without PFD.
MethodsStudy designThis is a methodological study approved by the Universidade Federal de Minas Gerais Ethics' Committee’ Committee (CAAE 44534615.5.0000.5149), and conducted according to the Declaration of Helsinki. All subjects gave written informed consent. The study was written according to Guidelines for Reporting Reliability and Agreement Studies (GRRAS).15 Methods of examination, definitions, and units also complies with standards jointly recommended by the International Urogynecology Association (IUGA) and the International Continence Society (ICS).12,14
ParticipantsTo structure the PFMF exam, a panel of experts, comprised of experienced and novice physical therapists in pelvic floor (PF) examination, was selected from working contact.
For reliability and agreement tests, a convenience sample of women from community older than 18 years, with and without urinary incontinence (UI) and other PFD were included. Women virgo, pregnant, who had an abortion or had given birth, either vaginally or via caesarean section, in the last 12 months, were in their monthly period, had symptoms and signs of vaginal and/or urinary infection, had undergone pelvic surgery (except caesarean section), in the last five years, those who did not understand the instructions during the pelvic floor assessment, or who refused to sign the informed consent were excluded.
The sample size necessary to reach a reliability index of 0.80 for continuous variables with 80% statistical power and 0.05 alpha value was calculated and concluded that at least 23 subjects were necessary.16 For categorial data, a reliability index of 0.7017,18 was considered to calculate sample size with 80 % statistical power and 0.05 two-tailed alpha value yielding a sample of 21 subjects.
ProceduresThe Delphi method was used to guide the work of the panel of experts.19,20 Nine physical therapists were invited and accepted to participate in the study. They were selected from working contact according to their expertise in PFM evaluation. All of them were specialists in women's health physical therapy, including novice and experts in pelvic floor examination. All the EFSMAP (Exame das Funções Sensoriais e Motoras do Assoalho Pélvico)’ contents were presented to the experts, either to be “included, modified, or excluded”, until perfect agreement (a 100 % agreement among experts for each item of the EFSMAP) among experts was reached. The panel of experts discussed and refined concepts, measurements, and verbatim instructions targeting at EFSMAP reproducibility and diagnostic labelling. It took four rounds discussion among experts until perfect agreement on all EFSMAP content was reached. All the experts participated to the following discussion rounds: 1st) structuring the PFMF exam’ sheet including the PFMF terms, conceptual and operational definitions5 and design; 2nd) structuring a list of concepts and instructions to perform the PFMF exam; 3rd) discussion to clear doubts and barriers to measurement along with clinical testing of the PFMF exam; 4th) refinement and approval of the final version of the PFMF exam sheet and list of concepts and instructions.
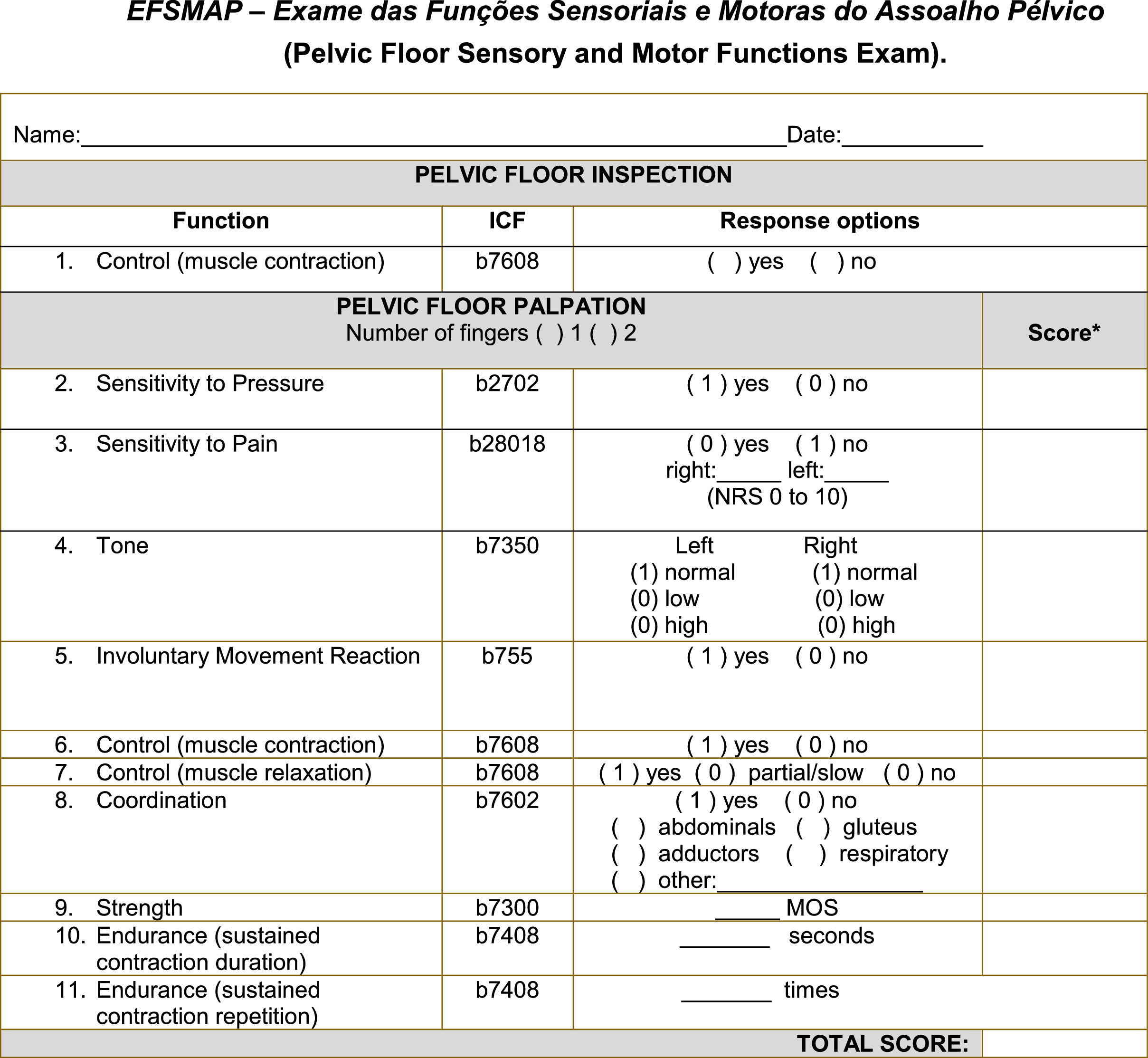
The final version of the PFMF exam’ sheet and the list of instructions (Fig. 1 and Table 1) were then used for intra- and inter-rater reliability and agreement testing.
EFSMAP – Exame das Funções Sensoriais e Motoras do Assoalho Pélvico. Legend: NRS - numeric rating scale; MOS - Modified Oxford Scale. *Scores for items 9 and 10 are respectively the MOS value and the value, in seconds of the sustained contraction; Total score is the linear sum of items 2 to 10.
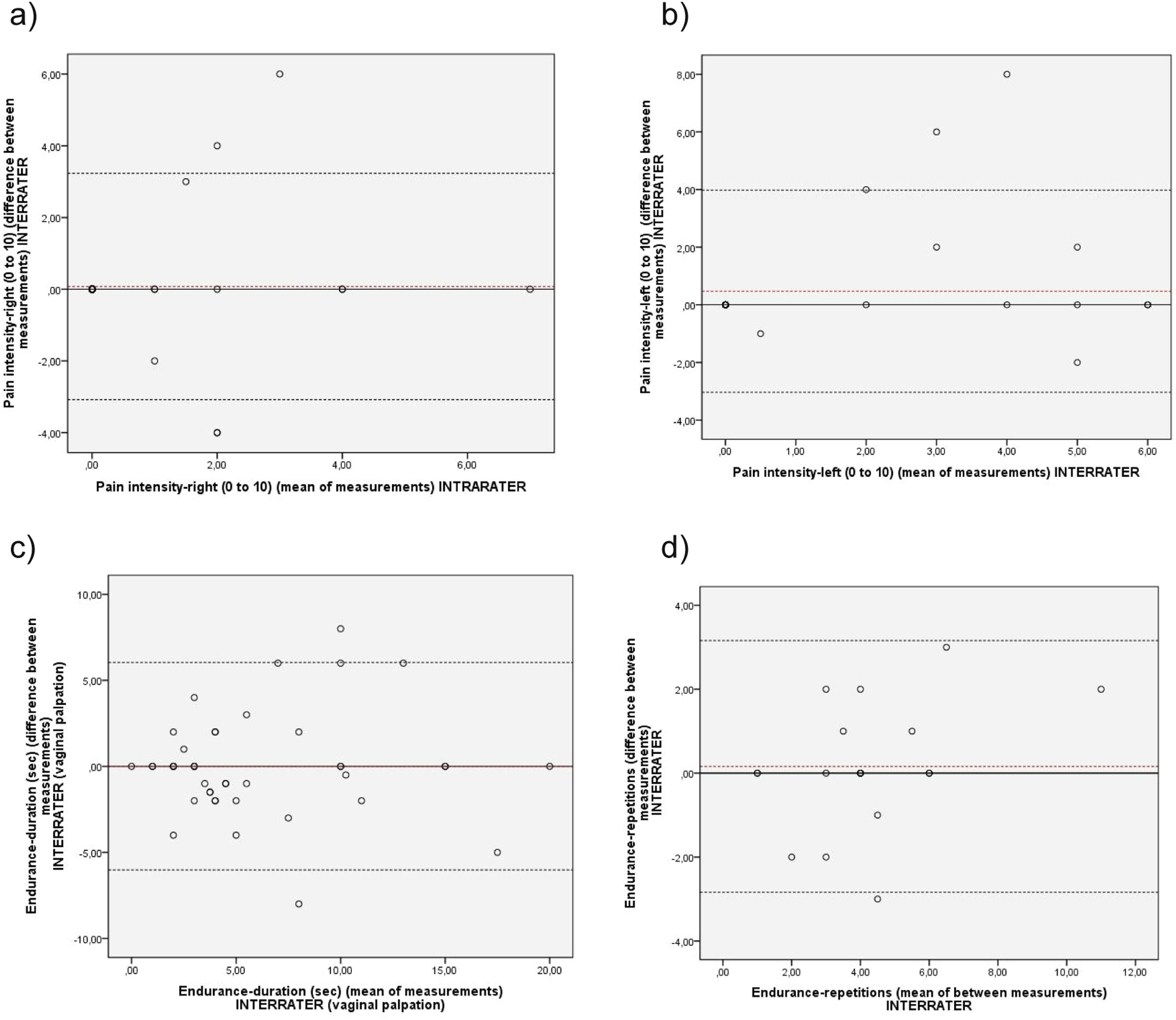
Menu of terms, concepts, standardized instructions to perform the EFSMAP and diagnostic label to PFMF impairments.
| PFM function (ICF code) | Conceptual definition | Operational definition | Participants instructions*all instructions can be given up to three times | Scale (scores)§Diagnostic label |
|---|---|---|---|---|
| Sensitivity to pressure (b2702) | Sensory functions of sensing pressure against or on the skin/mucosa.4 | Digital vaginal palpation: Examiner inserts one finger in vaginal canal and contacts the medial aspect of the vagina corresponding to the level of the deep PFM and presses on anterior, posterior, right, and left lateral vaginal walls and asks woman to inform the direction of pressure felt. | Keep your muscles relaxed and tell me the direction in which I am pressing: if down, up, left, or right (show the directions to the patient using the non-palpating hand). | Yes (1): pressure directions identified. State directions felt.No (0): pressure directions not identifiable. Impaired sensitivity to pressure |
| Pain sensation (b28018) | Sensation of unpleasant feeling indicating potential or actual damage to some body structure.4 | Digital vaginal palpation: Finger position as described above, examiner presses on right and left lateral vaginal walls, covering tendons and muscle belly, and asks woman to inform the presence of pain from 0 (no pain) to 10 (the worst pain felt). | Keep your muscles relaxed, as I will press it. Please, inform the presence of pain. In case of affirmative answer, the woman was asked to grade its intensity in a zero to 10 numerical scale as follows:Please, rate your pain in a 0 to 10 scale, meaning that 0 is no pain and 10 is the worst pain felt. | No (1): No pain is felt.Yes (0): There is pain or discomfort.impaired pain sensationNumeric Classification Scale (0 to 10); not used for total score. |
| Muscle tone (b7350) | Tension felt over PFM during palpation in the most relaxation state in which women can voluntarily reach.10 | Digital vaginal palpation: Examiner inserts one finger in vaginal canal and contacts the medial aspect of deep pelvic floor muscles anterior to anorectal junction (separately on the left and then on the right sides of vaginal canal) and performs a slow compression over PFM. This maneuver was repeated three times after 3 pelvic floor voluntary muscle contractions to locate muscle and to refrain muscle from tixotropy.39 | Keep your muscles as relaxed as possible as I press the vaginal walls. | Normal (1): tissue offers some resistance to stretch, but it is easily deformable. Low (0): no or minimum resistance to pressure offered by muscle (very deformable; or no palpable muscle due to muscular atrophy as in hypoestrogenism). Impaired muscle toneHigh (0): muscle offers high resistance to deformation or cannot be deformed.Impaired muscle tone |
| Involuntary movement reaction (cough) (b755) | Muscular contraction in response to a perturbation.10 | Vaginal (bi) digital palpation: Examiner feels muscle response to a strong cough on demand. | Give me a strong cough. | Yes (1): a contraction is clearly felt under examining finger, either on left or right sides of vaginal canal. No (0): No contraction is felt when a strong cough is performed. Impaired involuntary movement reaction |
| Control of simple voluntary movement (contraction) (b7608) | Ability to contract the PFM on demand.54 | Vaginal (bi) digital palpation: Examiner inserts one or two fingers in vaginal canal (depending on its natural aperture) and contacts the medial aspect of deep PFM (simultaneously on the left and right sides)* and feels muscle response to contraction on demand.37 | Please, contract your pelvic muscles as if you were to stop the flow of urine or gases. | Visual observation (not used for final score): Yes: Inward movement of perineum (in cranial direction) is observedNo: no inward movement of perineumImpaired control-contractionPalpation:Yes (1): Unequivocal increase in muscle tension during contraction is felt. No (0): No contraction of pelvic floor muscles is palpable.Impaired control-contraction |
| Control of simple voluntary movement (relaxation) ‡ (b7608) | Ability to relax pelvic floor muscles on demand after a contraction has been performed.54 | Vaginal (bi) digital palpation: † Examiner feels muscle response to relaxation on demand.12 | Please, stop contracting your pelvic muscle. | Yes (1): Relaxation is felt as a termination of the contraction. The pelvic floor muscles should return fast and completely to their resting state.No (0): No relaxation is felt. Contraction persists even after the command “stop contracting”Partial/Slow (0): Pelvic floor muscles do not return to their resting state or do it in a slow manner. Impaired control-relaxationObs: whenever Control (contraction) (b7608) is classified as absent, this function should not be examined and rated as “No”. |
| Coordination of voluntary movement (b7602) ‡ | Activation of correct muscles in adequate time and intensity to perform a specific action.9 | Vaginal (bi) digital palpation + visual observation of abdomen, breathing pattern, tight and buttocks: Examiner feels contraction and the use of other muscles. | Please, contract your pelvic floor muscles as if you were to stop the flow of urine or gases. Try to focus the contraction only on your PFM. We expect a PFM contraction without visible contraction of synergistic muscles; i.e., we expect that women can activate the target (correct) muscles. | Yes (1): No muscles other than PFM contracted on demandNo (0): Contraction of PFM together with other muscles. We have targeted at the frequently observed synergies: abdominal (other than transversus abdominis muscle), gluteal, tight adductors, respiratory, or Valsalva maneuver. Register the muscles that contracted along with PFM. A flicker contraction of transversus abdominis is expected and it is not considered coordination impairment.55Impaired coordinationObs: women were previously instructed on how to perform the correct PFM contraction. If even after being instructed women contract PFM using visual contraction of synergistic muscles, coordination is rated as “No”. |
| Strength** ‡ (b7300) | Capacity of a muscle to generate force.56 | Vaginal (bi) digital palpation:† Examiner feels intensity of the muscle tension during contraction under the examining finger and movement of the finger.37 | Please, contract your pelvic muscles as if you were to stop the flow of urine or gases as hard as you can, focusing on your PFM. | Modified Oxford Scale (MOS)37: 0 No discernible muscle contraction.1 A flicker or pulsation is felt under the examiner's finger.2 An increase in tension is detected, without any discernible lift.3 Muscle tension is further enhanced and characterised by lifting of the muscle belly and also elevation of the posterior vaginal wall.4 Increased tension and a good contraction are present which are capable of elevating the posterior vaginal wall against resistance (digital pressure applied to the posterior vaginal wall).5 Strong resistance can be applied to the elevation of the posterior vaginal wall; the examining finger is squeezed and drawn into the vagina (like a hungry baby sucking a finger)37§ Use the MOS score to compute total score.Impaired strength |
| Endurance (duration of sustained contraction) ‡ (b7408) | Ability to sustain muscle contraction of isolated muscle groups for the required period of time.56 | Vaginal (bi) digital palpation: Examiner feels the time (in seconds) the subject sustains the maximum or near maximum contraction. The consistent and marked drop in muscle contraction intensity and/or intermittent contractions and/or use of synergistic muscles were the cutt-off point to terminate this evaluation.37 | Contract your pelvic muscles as if you were to stop the flow of urine or gases and hold contraction for as long as you can without using other muscles, such as buttocks, abdomen, thigh or holding your breath. | Seconds§ use the number of seconds to compute total score)Impaired endurance-duration |
| Endurance (repetitions of sustained contraction)(b7408) | Ability to perform a set of sustained contractions until fatigue occurs.56 | Vaginal (bi) digital palpation: Examiner feels the number of sustained contraction that the woman was able to perform. Interval between contractions corresponds to a breathing cycle (approximately 4–5 s). Repetitions cut-off point is any fatigue sign, such as explicit reduction in contraction intensity, irregular contraction or slow relaxation after contraction.37 | Same command as above for endurance (duration). Obs: When contraction loses intensity or explicit use of synergistic muscle(s) is observed. The woman is instructed to relax, and take a deep breath in and out. Another sustained contraction is then requested. This procedure is repeated until intensity/duration is reduced in comparison to the first one, or until woman can only contract PFM using synergistic muscles (the quality of sustained contraction is lost). | Number of repetitions§ Use the number of repetitions to compute total scoreImpaired endurance-repetition |
Notes: *In order to help patient to keep her mind at the present moment and help keep muscles relaxed, we recommend to ask the patient to take a deep breath between each pelvic floor muscle function examined. : †This finger position was used in all vaginal palpation tests, unless otherwise specified. ‡ Whenever the function Control (contraction) is rated as “no”, the functions in which this symbol is presented cannot be examined and are to be rated as “no” as well. ** The term used in ICF4 is “Power”, nevertheless, power is the product of force and velocity.56 The term strength is more appropriate as it is defined as the maximal force a muscle or muscle group can generate at a specified angle56 and it is what effectively is intended to be measured during the PFMF digital assessment. So, we recommend the term strength instead of Power, as set in ICF in the Portuguese version.57 §Numbers in parenthesis correspond to scoring of EFSMAP concerning each PFMF. Thus, the EFSMAP total score is the linear sum of the results from each PFMF examined. The lower the score, the worse the muscle disability. The higher the score, less muscle disability the patient presents.
The PFMF examination was conducted independently by two physical therapists, in a private room. The participants: were educated about structure and function of the PFM, using anatomic figures of the pelvis and pelvic organs as well as information about the PFMF exam procedures12,21; answered a sociodemographic and clinical ad hoc interview based on questionnaires on urinary,22 sexual, and defecation functions,21,23,24 and anthropometric measurements (height and weight) were taken; were oriented to lay in lithotomy position to perform the Pelvic Organ Prolapse Quantification system (POP-Q)25 for sample characterization; and were instructed to rest their legs over a foam roll measuring 30 cm in diameter, and 70 cm in length, allowing a relaxed posture to examine the PFMF, via visual inspection and (bi)digital vaginal palpation of the PF.
Before collecting data, the two raters (one with 15 years of experience in PFM exam and one a novice) were systematically trained by a physical therapist with 20 years of experience on PFM examination. Training consisted of discussing conceptual and operational definitions on PFMF and of clinical testing. A sample of 20 women was examined during training until self-perception of confidence with the examination procedures was reached by the two examiners.
For interrater reliability and agreement, the two raters, independently examined participants within a 10 to 20 min interval between assessments in a random order and on the same day.
For intrarater assessment, only one rater (more experienced) examined women one week apart from the first examination, at the same period of the day as in the previous exam. Participants who had impaired PFM control – contraction (EFSMAP item # 6 – Fig. 1) were not tested to the subsequent EFSMAP items (items # 7 to 11), as that impairment makes impossible to measure those other functions.
Statistical analysisDescriptive statistics were used as appropriate. Intraclass Correlation Coefficient (ICC) was used to test interrater (ICC 2,1) and intrarater (ICC 3,1) reliability,26 and Bland Altman analysis, to test agreement coefficients for continuous variables.27 Percent agreement, Kappa statistics, and linear weighted Kappa computed measurement error and reliability of categorical and ordinal variables, respectively.26 Reliability and agreement coefficients were interpreted as follows: ICC values above 0.75 indicate good reliability and below 0.75, moderate to poor reliability.26 For agreement and Kappa, values above 80 % represent excellent agreement; above 60 % substantial agreement; from 40 % to 60 % moderate agreement; and below 40 % fair to poor agreement.28 A paired t-test or a McNemar test were used as appropriate to test differences between measurements.29
Statistical significance was set at 5 %. Analyses were done using SPSS-19 and VassarStats © available at http://vassarstats.net/kappa.html.
ResultsThe panel of experts comprised nine physical therapists with between 35 years to less than a year of experience in PFM examination. Six were specialist in Women's Health physical therapy certified by the Physical Therapy Federal Council (COFFITO) in association with the Brazilian Women's Health Physical Therapy Association (ABRAFISM). From the 1st round discussion, the following decisions were taken. i) To initiate the exam by visual inspection of the perineum while the woman contracts and relaxes the PFM; this allows the examination of control that involves contraction and relaxation ability.5 Visual inspection also offers information about those women who might not tolerate digital vaginal palpation. ii) To perform vaginal palpation either uni or bi-digital,12,30 according to the examiners’ experience, and should be indicated in the exam sheet12; the women's position during examination must allow relaxation of the PF and adjacent muscles; the examiner should refrain from touching the patient's legs avoiding torque generation. Also, vaginal palpation is to be performed mainly at posterior vaginal wall where most of the PFM are located, going through all PFM (see Table 1 for detailed information on measurement procedures). iii) To include the ICF codes in the second column of the exam's sheet corresponding to the function to be examined to allow diagnostic labels for clinic and scientific data, and the identification of ICF terms in different languages, as the codes are interchangeable throughout ICF translated versions.11iv) To add two PFM sensorial functions: sensitivity to pressure and pain sensation (ICF codes b2702 and b28018, respectively) together with the muscle/movement functions proposed,5 as those can be impaired during vaginal delivery.31–33v) To include two measures of endurance (contraction duration and repetition) targeting a specific PFM training dose (example: to perform eight repetitions of PFM contraction sustained for 5 s each-duration). vi) To define the measurement scales for each PFMF based on the literature.5 The Brink Scale,34 Ortiz Scale,35 Modified Oxford Scale (MOS),36,37 PERFECT scheme,37 Slieker ten-Hove's scheme,38 and Dietz39 tone scale were consulted. vii) To include a final EFSMAP score, built by the linear sum of the individual PFMF scores as follows: for strength, the score is the result of the MOS (from 0 to 5 points)36,37; for endurance-duration, the score is the contraction’ holding time in seconds; and for endurance-repetition, the score is how many times that contraction’ holding time is repeated until fatigue is reached. For the other functions, no impairment adds 1 point to the score. The EFSMAP lower score limit is zero, but there is no upper limit, as it varies according to endurance (contraction duration - EFSMAP item 10). Item 11-endurance (repetition of contraction) is not computed in sum, as it would inflate the weight of endurance in the total EFSMAP score. The higher the total score, the better the PFMF (Table 1). The sequence of the pelvic floor sensorial and muscle functions (from 1 to 11) proposed in EFSMAP was carefully designed according to motor control concepts allowing clinical reasoning during the assessment. For example, the diagnosis of pelvic floor pain (item 3) and high tonus (item 4) could lead the physical therapist to hypothesize further impairment in control/relaxation (item 7), coordination (item 8), strength (item 9), and endurance (items 10 and 11). viii) To develop a list of conceptual and operational definitions, along with detailed instructions to perform the EFSMAP, so as to overcome the plethora of terms, definitions, and operationalization of PFMF in the literature,3,6,13 targeting reproducibility of measures (Table 1). The table contains patient positioning, raters’ hand and fingers locations, verbatim instructions to patients, the rating scale of each function and the impairments’ diagnostic label (also available in Brazilian Portuguese in the online Supplementary Material 1 and 2).
The final scales and scoring methods were refined and finalized during the 2nd, 3rd, and 4th discussion rounds. Also, in the 4th round discussion, a name to the PFMF exam was defined: EFSMAP, an acronym of Exame das Funções Sensoriais e Motoras do Assoalho Pélvico in Brazilian Portuguese, meaning Exam of Sensorial and Muscular Functions of the Pelvic Floor (Fig. 1).
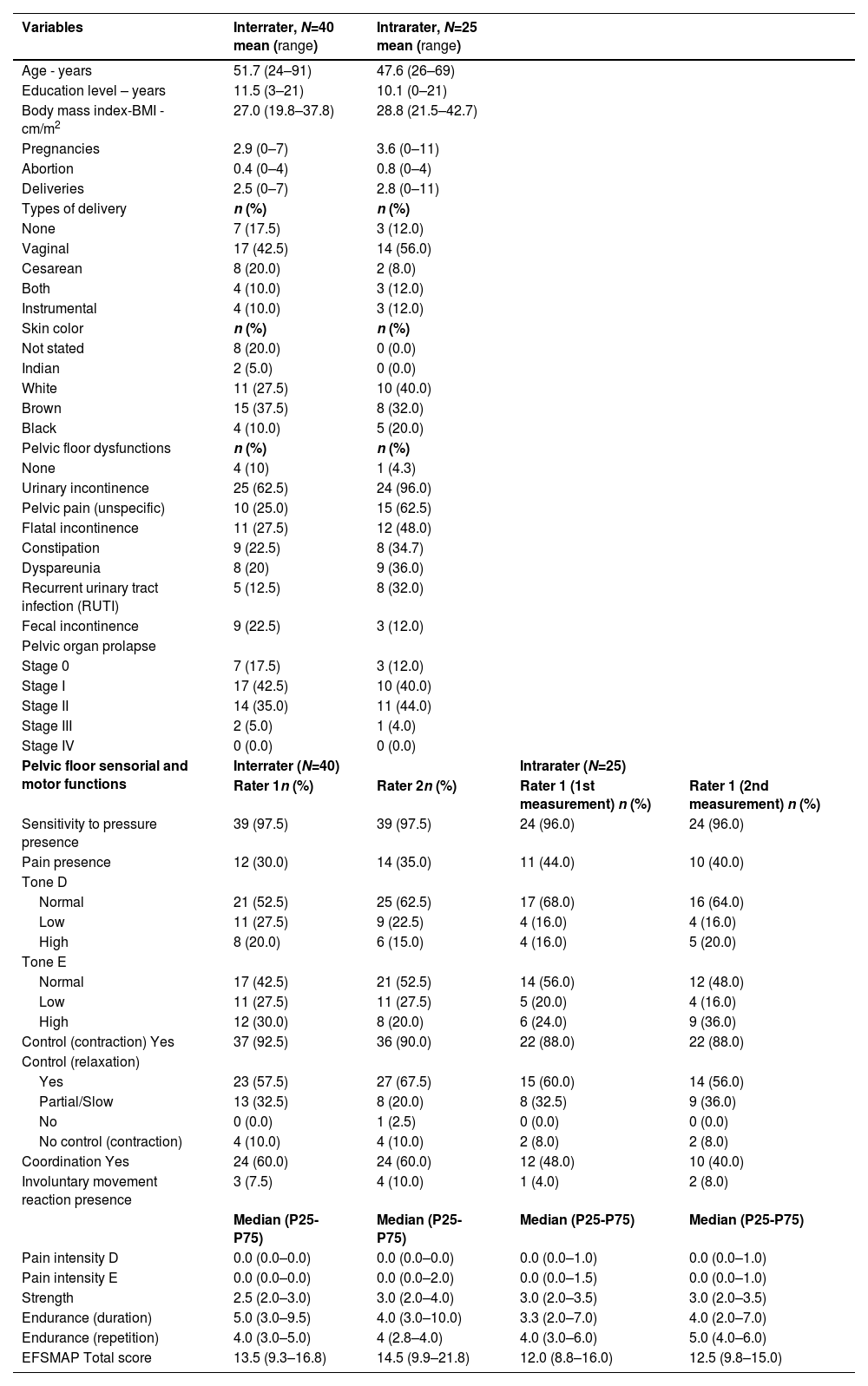
Reliability and agreementFor interrater analysis, 40 participants were examined by two raters (rater 1 – most experienced and rater 2 – novice). For intrarater analysis, the rater 1 examined 25 participants. Sample characteristics are displayed in Table 2.
Study participants socio-demographic and clinical characteristics.
*Note: Participants could have reported more than one pelvic floor dysfunction.
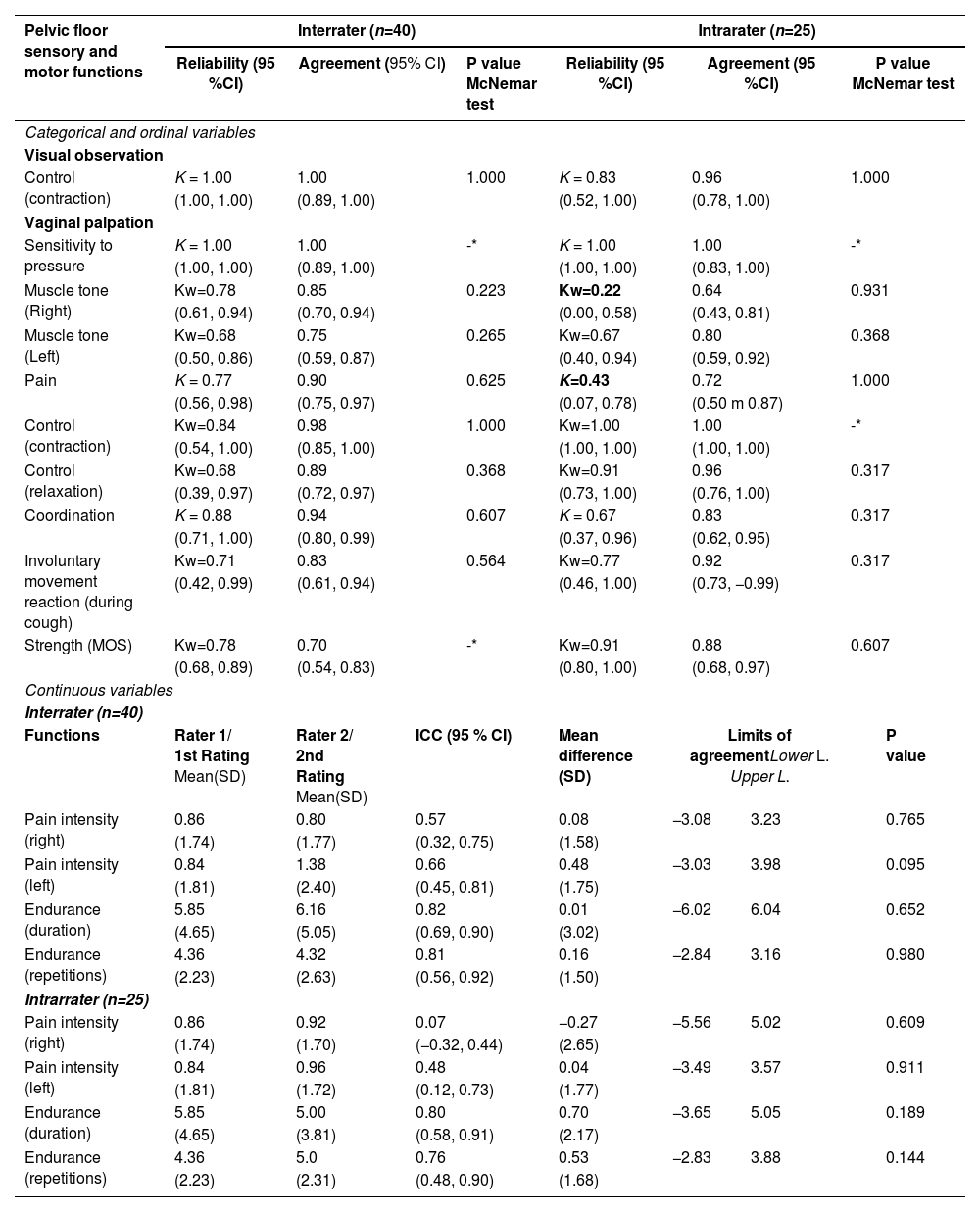
Results of intra- and inter-rater reliability and agreement are presented in Table 3.
Reliability and agreement for interrater and intrarater measurements of pelvic floor sensory and motor functions.
Legend: CI, confidence interval; K, Kappa coefficient; Kw, Weighted Kappa coefficient; MOS, Modified Oxford Scale. ICC, intraclass correlation, CI, confidence interval; SD, standard deviation.
For most functions, reliability and agreement analysis both in interrater and intrarater testing coefficients were considered good to excellent (Table 3) and no statistical differences was observed between measurements.
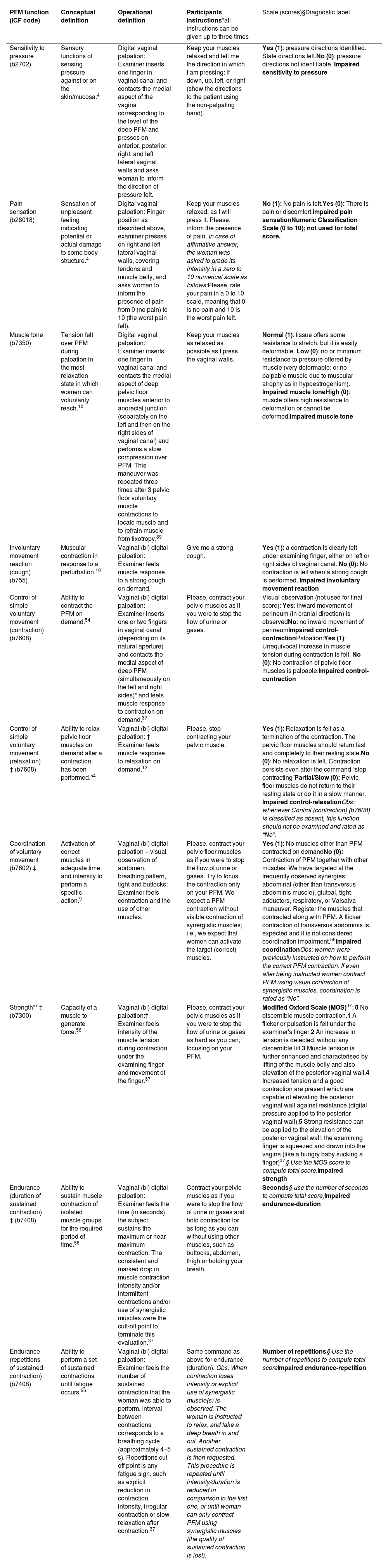
Pain intensity (ICC=0.07, 95 %CI= −0.32, 0.44) and tone (Kw=0.22; 95 %CI 0.00, 0.58) both measured on the right side of vaginal wall presented no intrarater reliability (Table 3). In Bland Altman's agreement analysis for pain intensity-right side, the mean differences increased as measurement values increased (Fig. 2a and e). No statistical significance between measurements were observed.
Bland–Altman plots showing interrater (2a, 2b, 2c and 2d) (n = 40) and intrarater (2e, 2f, 2g and 2h) agreement analysis (n = 23) for pain intensity and endurance. 2a) Interrater Bland Altman agreement analysis of pain intensity (right side of vaginal wall); 2b) Interrater Bland Altman agreement analysis of pain intensity (left side of vaginal wall); 2c) Interrater Bland Altman agreement analysis of endurance – duration; 2d) Interrater Bland Altman agreement analysis of endurance – repetitions; 2e) Intrarater Bland Altman agreement analysis of pain intensity (right side of vaginal wall); 2f) Intrarater Bland Altman agreement analysis of pain intensity (left side of vaginal wall); 2g) Intra Bland Altman agreement analysis of endurance – duration; 2h) Intrarater Bland Altman agreement analysis of endurance – repetitions.
The present study aimed to contribute to the discussion on PFMF physical therapeutic diagnosis. It structured an examination of all PFMF investigated in the literature, categorized and labeled under the ICF,5,6 and tested the reproducibility of visual observation and digital palpation for these PFMF, as recommended by the ICS.13 The exam, named EFSMAP, was successfully structured by full agreement among a panel of physical therapists experts. It includes an exam sheet, a list of concepts, standardized instructions, and diagnostic labels targeted at reproducibility of visual observation and digital palpation of the pelvic floor. Most of the PFMF tested presented adequate intra/interrater reliability and agreement, indicating that the EFSMAP can be reliably used in clinical practice and research.
The PFMF included in the EFSMAP are not new, they were retrieved from the literature through a systematic review on PFMF of women with PFD6 and from a subsequent study that used ICF terminology to narrow down the 61 terms referring to PFMF5 into ICF terms described in chapter 7 on neuromusculoskeletal and movement-related functions.4,6,13 The ICF is endorsed and readily available for all 191 WHO member countries in their native languages11 offering universal terminology that spares additional efforts to worldwide translation. ICF terms and coding4 may improve communication among health care professionals concerning PFMF impairment label diagnosis.2 Impairments are problems in the structure and function of human body's physiological systems.4 Thus, applying ICF terminology (and further its bio-psycho-social model), although complex, might facilitate the discussion on labelling physical therapy diagnosis.2,3,40
The many assessment scales/schemes available to measure the PFMF30,34–38 lack consensual theoretic foundations and terminology,13 hampering data-gathering and communication.6,41 In contrast, the list of concepts and instructions developed in the EFSMAP was based on the literature on human movement8–10 and on the recognized ICF terminology.4 The panel of experts discussed and refined concepts and verbatim instructions targeting at EFSMAP reproducibility and diagnostic labelling. Conceptual must precede operational definition, the reverse leads to operationism41 which precludes professionals from clearly understanding what is actually being measured. Operationism leads to a proliferation of terms and definitions, impeding data gathering, diminishing the feasibility of generalization beyond a specific investigation, and ultimately constraining communication and scientific progress.5,41 In PFMF terminology, this phenomenon is evident,6 and it could potentially be mitigated through the utilization of the EFSMAP.
The literature reveals inconsistent reproducibility for PFMF examination through visual observation and vaginal palpation.13 EFSMAP reproducibility was good to excellent for most PFMF examined, except for pain and tone, which were reliable in interrater analysis but not in intrarater testing. A few authors have previously investigated pain and tonus using similar operational definitions as we did and also found inconsistent results.17,38 We used a numeric rating scale (0–10) for pain measure and found good to excellent reliability and agreement indices, except for intrarater reliability that was moderate. Previous studies also found variability in pain measures using an 11 point numeric rating scale.17 Similar to ours, they reported low indices of pain intensity (<3/10), which may have weakened the ability of a pain scale to discriminate mild symptoms. Moreover, pain is an intricate sensorial response influenced by both biological and personal factors, including affective components,42 which might have fluctuated during the week and contributed to the moderate intrarater reliability observed for pain.
The literature shows conflicting results on tone reproducibility, ranging from moderate to good reliability in intra and interrater analyses,18,43 to fair or no reliability.17,43 Kavvadias et al.,17 found no intra or interrater reliability using an 11 point scale. Authors were not clear on how tone was conceptually defined nor how measurement was scored. Oppositely, Loving et al.,18 found good reliability in a six point tone scale. Thus, clear conceptual and operational definitions for tone as well as a scale with fewer categories may improve tone reliability measure. Still, we have found poor intrarater reliability for tone-right side. The left/right asymmetry observed seems to reflect the adaptive and complex nature of muscle tone, as it is influenced by many factors such as myofascial force transmission,44–48 stress, fear, anxiety, injury, hormonal, lifestyle, and occupational factors.49 On the other hand, the persistence of high tone is observed in emptying disorders such as constipation, recurrent urinary tract infection, and sexual disorders.50–52 However, women with these PFD were infrequent in our sample, which may have contributed to the low intrarater reliability observed.
The EFSMAP total score provided by interval/numeric scale might captures changes over time in the PFMF, for example, before and after physical therapeutic intervention. The clinically relevant changes should be investigated in future studies. Although a total score is provided, the observation of the specific impairments identified in the EFSMAP are crucial to the diagnosis of PFM impairments and to the prescription of patient-oriented physical therapeutic approach. For instance, a woman with pain, high tone and impairment in control/relaxation might need myofascial interventions before assigning her to pelvic floor muscle training (PFMF), which targets strength and endurance. Another woman, diagnosed with impaired coordination will need to learn to adequately activate PFM before conducting PFMT. Finally, a woman diagnosed with impairments in strength and endurance, but not in pain, tone, control, and coordination might be directly assigned to PFMT. Therefore, the EFSMAP diagnosis reveals specific combinations of pelvic floor sensorial and motor impairments.
Raters had the freedom to choose their preferred palpation approach, either unidigital or bidigital. Recently, Silva et al.,30 found that bidigital palpation yielded better reproducibility indices than unidigital palpation for strength and endurance. Bidigital palpation seems reasonable for testing these functions, as the rater primarily relies on gross motor skills to feel perineum movement. Conversely, fine sensitivity is needed to test more delicate functions,10 such as tone and involuntary movement reaction. Thus, we advocate leaving the decision of whether to palpate PF with one or two fingers to the rater's ability, as this may result in a more precise response.
Physical therapists, using their hands as the primary examination tool, must be trained in manual techniques, including PFMF measurement. High reproducibility indices indicate that practicing a minimum of 20 examinations refines skills for consistent performance in EFSMAP. While learning curves are studied in medical and nursing fields,53 this aspect is overlooked in physical therapy, as no studies address it. Encouraging future research on this topic is essential.
The present study has limitations. The low level of pain observed in the investigated sample might have limited the reproducibility outcomes of the numeric rating scale for PFM pain. Also, our inferences for the left/right tone asymmetries observed in intrarater reliability are one possible rationale but it might lack external validity for all women with UI and other PFD. We advocate that changes in tone over time reflect the adaptive nature of the musculoskeletal system therefore changes in tone are expected.
ConclusionEFSMAP was successfully developed as a valid and reliable exam of the PFMF of women whether they have pelvic floor disorders. EFSMAP, grounded on movement systems physiology and ICF/WHO terminology, consolidates 61 previously identified PFMF terms into six: tone, involuntary movement reaction, control of voluntary movement (contraction and relaxation), coordination, strength, and endurance. Additionally, the expert panel incorporated two sensorial functions (pressure and pain) and established clear definitions and diagnostic labels for PFM impairments. As a result, EFSMAP emerges as a valid and reliable method to exam and diagnose women's PFMF, using visual observation and vaginal palpation. It can be utilized in both clinical practice and research. The integration of ICF terminology into EFSMAP enables the provision of valid labels for diagnosing PFM impairments, fostering evidence-based practice and communication across disciplines and cultures.
Special thanks to the panel of experts, to Juliana Machado Magalhães Barbosa for kindly and thoroughly reviewing the manuscript; and to Elza Baracho for keeping inspiring Women's Health physical therapists. This study is dedicated to the memory of Vera Lúcia Batista Barbosa da Silva.