There has been many efforts and updates over the years to develop a consensus for English terminology related to the pelvic floor (PF). There is a similar need to standardize physical therapy related PF terminology in Brazil.
ObjectiveTo propose a guideline in Brazilian Portuguese language on the terminology related to the female PF function and assessment.
MethodsThe Brazilian Association of Physical Therapy in Women's Health (ABRAFISM) established a working group (Steering committee) responsible for conducting a systematic review on PF terminology, propose definitions in Portuguese, and manage the developmental stages. A systematic review of international consensus was conducted and the terms related to the PF were identified, listed, and defined in Portuguese. A Delphi method was used to reach a consensus on the definitions by querying a panel of expert professionals with clinical and research experience in the PF field. This panel included 19 physical therapists from all Brazilian regions and two physicians. The Delphi process included the following steps: evaluation of proposed terms by the panel of experts; review of suggestions made by the panel of experts, modification of terms based on those suggestions, and a new round of evaluation of the modified terms until reaching an 80% agreement.
ResultsTwo rounds were necessary for terms related to anatomy and signs/symptoms of the PF, while a 90% consensus for terms related to assessment of the PF muscles was achieved in the first round.
ConclusionA final Brazilian-Portuguese guideline with consensus terminology on anatomy, symptoms, signs, and terms related to assessment of PF muscles was developed.
The terminology used in Brazil regarding the assessment and diagnosis of pelvic floor (PF) function in females is diverse,1 depending on the physical therapist's training, region of the country where they work, and theoretical framework. The lack of standardization of terms used in clinical practice makes it difficult for physical therapists to understand and discuss clinical cases with other health professionals and for researchers to disseminate scientific findings. It should be a goal to standardize terminology used in healthcare.2
The International Urogynecological Association (IUGA) and the International Continence Society (ICS) have made joint efforts to develop terminology recommendations regarding the function and dysfunction of the PF muscles3–8 in English. Considering that a lack of consensus in Brazil on terminology related to the female PF impairs clinical and scientific communication, the objective of this study was to develop a consensus terminology in Brazilian-Portuguese that would include anatomical terms, description of signs and symptoms, and assessment of PF muscle function.
MethodsThis is a descriptive study of terminology based on a systematic search of the literature and consensus among Brazilian experts using a modified Delphi method. This project was approved by the Institutional Ethics Committee of the Universidade Federal de São Carlos (UFSCar), São Carlos, SP, Brazil (CAAE: 37684920.2.0000.5504). The preparation of this guideline was coordinated by the scientific board of the Brazilian Association of Women´s Health Physical Therapists (ABRAFISM), which appointed a working group (Steering committee) composed of five Brazilian researchers’ specialists in Women's Health Physical Therapy certified by the Federal Council of Physical Therapy and Occupational Therapy and ABRAFISM. The steering committee was responsible for undertaking the systematic review on PF terminology, proposing the initial definitions in Brazilian Portuguese language, inviting a group of experts (referred to as expert professionals) to evaluate the definitions of the terms, and managing the stages of the study until an 80% consensus was reached among experts on terminology terms. All stages of the research were conducted electronically.
Literature reviewInitially, a systematic review was conducted. Electronic searches in the MEDLINE (via PUBMED), PEDro, Embase, Lilacs, and Web of Science databases were conducted from January to February 2023 and updated in January 2024. Search strategies followed recommendations from Cochrane and PRISMA.9 Published articles on terminology and definition guides were included in this review. We did not restrict our search to language or publication date (Supplementary material 1).
Potential eligible records were inserted into the StArt software. Two independent reviewers screened the records, following three reading phases: titles, abstracts, and then full articles to identify the publications that met the pre-established inclusion criteria. Disagreements throughout the process were resolved by a third reviewer.
Selection of terms and elaboration of definitionsAfter reading all eligible records identified in the systematic review, the Steering committee extracted and listed all relevant terms. To complement the definitions of physical therapeutic action on PF function/dysfunction, the World Confederation for Physical Therapy10 website and the Brazilian legislation on physical therapy, which is available at the website of the Conselho Federal de Fisioterapia e Terapia Ocupacional (COFFITO - Federal Council of Physical Therapy and Occupational Therapy)11 were consulted, and additional terms found in these websites were added to the list. The final list of terms and definitions was sent to health professionals, who are experts in Women's Health/pelvic floor, for feedback.
Consensus on Terminology: Delphi MethodA group of professional experts was formed, which consisted of 19 physical therapists and two physicians, all board-certified, with five years or more of experience in teaching or research in the field of Women's Health/Pelvic Floor (i.e., publications in a peer-reviewed scientific journal related to the topic or published a national book in the last five years). All experts were required to accept the Informed Consent Form to participate in the research.
Consensus on terminology definitions was obtained using the modified Delphi Method.12–14 To do so, the terms and definitions were sent to the 21 professional experts via a link, in which they had to answer blindly whether they agreed or disagreed with the definitions. If they disagreed, they had to suggest a revised definition. The Steering committee reviewed the experts' suggestions and made changes to terms that did not reach 80% agreement. Then, these terms were sent back to the professional experts for another round of evaluation. This process was repeated until reaching 80% consensus (defined agreement) among experts.12
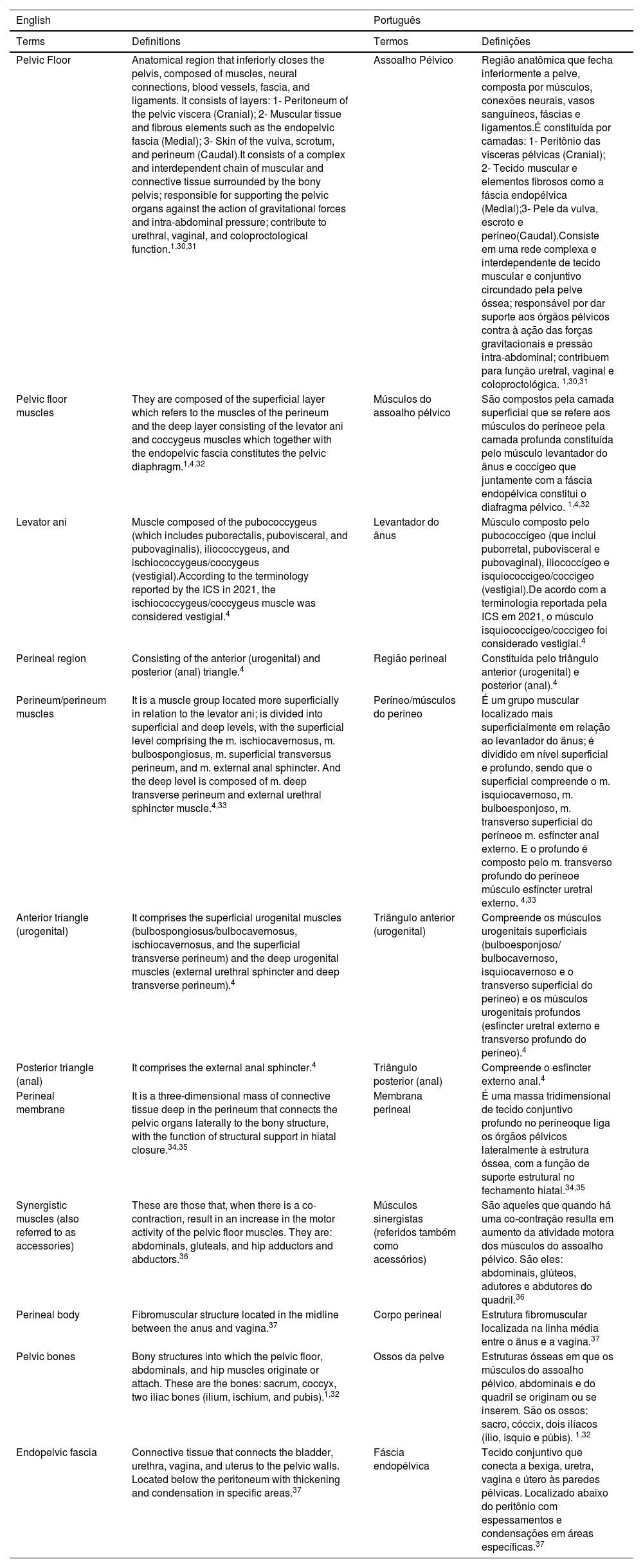
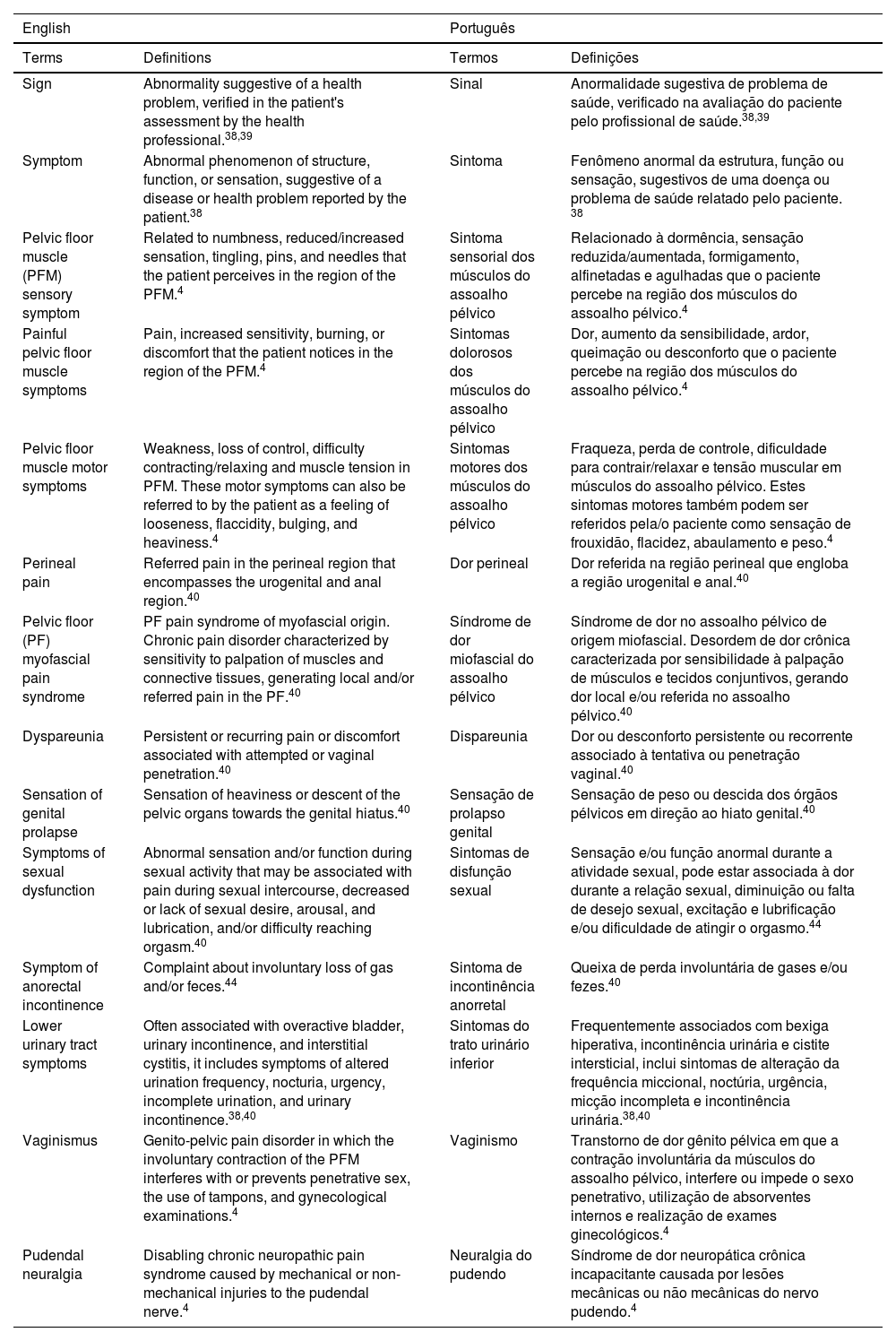
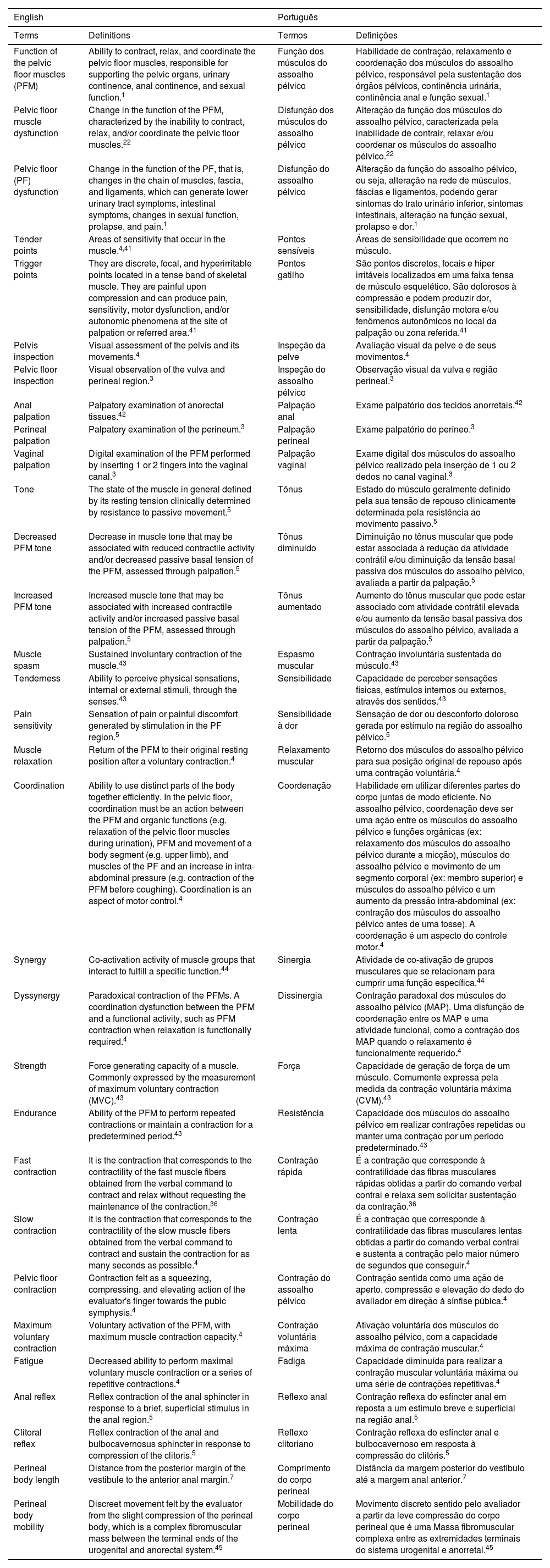
The list of definitions was divided into three tables: terms related to anatomy (Table 1), terms related to signs and symptoms (Table 2) and terms related to assessment (Table 3).
Terms related to anatomy.
| English | Português | ||
|---|---|---|---|
| Terms | Definitions | Termos | Definições |
| Pelvic Floor | Anatomical region that inferiorly closes the pelvis, composed of muscles, neural connections, blood vessels, fascia, and ligaments. It consists of layers: 1- Peritoneum of the pelvic viscera (Cranial); 2- Muscular tissue and fibrous elements such as the endopelvic fascia (Medial); 3- Skin of the vulva, scrotum, and perineum (Caudal).It consists of a complex and interdependent chain of muscular and connective tissue surrounded by the bony pelvis; responsible for supporting the pelvic organs against the action of gravitational forces and intra-abdominal pressure; contribute to urethral, vaginal, and coloproctological function.1,30,31 | Assoalho Pélvico | Região anatômica que fecha inferiormente a pelve, composta por músculos, conexões neurais, vasos sanguíneos, fáscias e ligamentos.É constituída por camadas: 1- Peritônio das vísceras pélvicas (Cranial); 2- Tecido muscular e elementos fibrosos como a fáscia endopélvica (Medial);3- Pele da vulva, escroto e períneo(Caudal).Consiste em uma rede complexa e interdependente de tecido muscular e conjuntivo circundado pela pelve óssea; responsável por dar suporte aos órgãos pélvicos contra à ação das forças gravitacionais e pressão intra-abdominal; contribuem para função uretral, vaginal e coloproctológica. 1,30,31 |
| Pelvic floor muscles | They are composed of the superficial layer which refers to the muscles of the perineum and the deep layer consisting of the levator ani and coccygeus muscles which together with the endopelvic fascia constitutes the pelvic diaphragm.1,4,32 | Músculos do assoalho pélvico | São compostos pela camada superficial que se refere aos músculos do períneoe pela camada profunda constituída pelo músculo levantador do ânus e coccígeo que juntamente com a fáscia endopélvica constitui o diafragma pélvico. 1,4,32 |
| Levator ani | Muscle composed of the pubococcygeus (which includes puborectalis, pubovisceral, and pubovaginalis), iliococcygeus, and ischiococcygeus/coccygeus (vestigial).According to the terminology reported by the ICS in 2021, the ischiococcygeus/coccygeus muscle was considered vestigial.4 | Levantador do ânus | Músculo composto pelo pubococcígeo (que inclui puborretal, pubovisceral e pubovaginal), iliococcígeo e isquiococcigeo/coccigeo (vestigial).De acordo com a terminologia reportada pela ICS em 2021, o músculo isquiococcigeo/coccigeo foi considerado vestigial.4 |
| Perineal region | Consisting of the anterior (urogenital) and posterior (anal) triangle.4 | Região perineal | Constituída pelo triângulo anterior (urogenital) e posterior (anal).4 |
| Perineum/perineum muscles | It is a muscle group located more superficially in relation to the levator ani; is divided into superficial and deep levels, with the superficial level comprising the m. ischiocavernosus, m. bulbospongiosus, m. superficial transversus perineum, and m. external anal sphincter. And the deep level is composed of m. deep transverse perineum and external urethral sphincter muscle.4,33 | Períneo/músculos do períneo | É um grupo muscular localizado mais superficialmente em relação ao levantador do ânus; é dividido em nível superficial e profundo, sendo que o superficial compreende o m. isquiocavernoso, m. bulboesponjoso, m. transverso superficial do períneoe m. esfíncter anal externo. E o profundo é composto pelo m. transverso profundo do períneoe músculo esfíncter uretral externo. 4,33 |
| Anterior triangle (urogenital) | It comprises the superficial urogenital muscles (bulbospongiosus/bulbocavernosus, ischiocavernosus, and the superficial transverse perineum) and the deep urogenital muscles (external urethral sphincter and deep transverse perineum).4 | Triângulo anterior (urogenital) | Compreende os músculos urogenitais superficiais (bulboesponjoso/ bulbocavernoso, isquiocavernoso e o transverso superficial do períneo) e os músculos urogenitais profundos (esfíncter uretral externo e transverso profundo do períneo).4 |
| Posterior triangle (anal) | It comprises the external anal sphincter.4 | Triângulo posterior (anal) | Compreende o esfíncter externo anal.4 |
| Perineal membrane | It is a three-dimensional mass of connective tissue deep in the perineum that connects the pelvic organs laterally to the bony structure, with the function of structural support in hiatal closure.34,35 | Membrana perineal | É uma massa tridimensional de tecido conjuntivo profundo no períneoque liga os órgãos pélvicos lateralmente à estrutura óssea, com a função de suporte estrutural no fechamento hiatal.34,35 |
| Synergistic muscles (also referred to as accessories) | These are those that, when there is a co-contraction, result in an increase in the motor activity of the pelvic floor muscles. They are: abdominals, gluteals, and hip adductors and abductors.36 | Músculos sinergistas (referidos também como acessórios) | São aqueles que quando há uma co-contração resulta em aumento da atividade motora dos músculos do assoalho pélvico. São eles: abdominais, glúteos, adutores e abdutores do quadril.36 |
| Perineal body | Fibromuscular structure located in the midline between the anus and vagina.37 | Corpo perineal | Estrutura fibromuscular localizada na linha média entre o ânus e a vagina.37 |
| Pelvic bones | Bony structures into which the pelvic floor, abdominals, and hip muscles originate or attach. These are the bones: sacrum, coccyx, two iliac bones (ilium, ischium, and pubis).1,32 | Ossos da pelve | Estruturas ósseas em que os músculos do assoalho pélvico, abdominais e do quadril se originam ou se inserem. São os ossos: sacro, cóccix, dois ilíacos (ílio, ísquio e púbis). 1,32 |
| Endopelvic fascia | Connective tissue that connects the bladder, urethra, vagina, and uterus to the pelvic walls. Located below the peritoneum with thickening and condensation in specific areas.37 | Fáscia endopélvica | Tecido conjuntivo que conecta a bexiga, uretra, vagina e útero às paredes pélvicas. Localizado abaixo do peritônio com espessamentos e condensações em áreas específicas.37 |
Terms related to signs and symptoms of pelvic floor.
| English | Português | ||
|---|---|---|---|
| Terms | Definitions | Termos | Definições |
| Sign | Abnormality suggestive of a health problem, verified in the patient's assessment by the health professional.38,39 | Sinal | Anormalidade sugestiva de problema de saúde, verificado na avaliação do paciente pelo profissional de saúde.38,39 |
| Symptom | Abnormal phenomenon of structure, function, or sensation, suggestive of a disease or health problem reported by the patient.38 | Sintoma | Fenômeno anormal da estrutura, função ou sensação, sugestivos de uma doença ou problema de saúde relatado pelo paciente. 38 |
| Pelvic floor muscle (PFM) sensory symptom | Related to numbness, reduced/increased sensation, tingling, pins, and needles that the patient perceives in the region of the PFM.4 | Sintoma sensorial dos músculos do assoalho pélvico | Relacionado à dormência, sensação reduzida/aumentada, formigamento, alfinetadas e agulhadas que o paciente percebe na região dos músculos do assoalho pélvico.4 |
| Painful pelvic floor muscle symptoms | Pain, increased sensitivity, burning, or discomfort that the patient notices in the region of the PFM.4 | Sintomas dolorosos dos músculos do assoalho pélvico | Dor, aumento da sensibilidade, ardor, queimação ou desconforto que o paciente percebe na região dos músculos do assoalho pélvico.4 |
| Pelvic floor muscle motor symptoms | Weakness, loss of control, difficulty contracting/relaxing and muscle tension in PFM. These motor symptoms can also be referred to by the patient as a feeling of looseness, flaccidity, bulging, and heaviness.4 | Sintomas motores dos músculos do assoalho pélvico | Fraqueza, perda de controle, dificuldade para contrair/relaxar e tensão muscular em músculos do assoalho pélvico. Estes sintomas motores também podem ser referidos pela/o paciente como sensação de frouxidão, flacidez, abaulamento e peso.4 |
| Perineal pain | Referred pain in the perineal region that encompasses the urogenital and anal region.40 | Dor perineal | Dor referida na região perineal que engloba a região urogenital e anal.40 |
| Pelvic floor (PF) myofascial pain syndrome | PF pain syndrome of myofascial origin. Chronic pain disorder characterized by sensitivity to palpation of muscles and connective tissues, generating local and/or referred pain in the PF.40 | Síndrome de dor miofascial do assoalho pélvico | Síndrome de dor no assoalho pélvico de origem miofascial. Desordem de dor crônica caracterizada por sensibilidade à palpação de músculos e tecidos conjuntivos, gerando dor local e/ou referida no assoalho pélvico.40 |
| Dyspareunia | Persistent or recurring pain or discomfort associated with attempted or vaginal penetration.40 | Dispareunia | Dor ou desconforto persistente ou recorrente associado à tentativa ou penetração vaginal.40 |
| Sensation of genital prolapse | Sensation of heaviness or descent of the pelvic organs towards the genital hiatus.40 | Sensação de prolapso genital | Sensação de peso ou descida dos órgãos pélvicos em direção ao hiato genital.40 |
| Symptoms of sexual dysfunction | Abnormal sensation and/or function during sexual activity that may be associated with pain during sexual intercourse, decreased or lack of sexual desire, arousal, and lubrication, and/or difficulty reaching orgasm.40 | Sintomas de disfunção sexual | Sensação e/ou função anormal durante a atividade sexual, pode estar associada à dor durante a relação sexual, diminuição ou falta de desejo sexual, excitação e lubrificação e/ou dificuldade de atingir o orgasmo.44 |
| Symptom of anorectal incontinence | Complaint about involuntary loss of gas and/or feces.44 | Sintoma de incontinência anorretal | Queixa de perda involuntária de gases e/ou fezes.40 |
| Lower urinary tract symptoms | Often associated with overactive bladder, urinary incontinence, and interstitial cystitis, it includes symptoms of altered urination frequency, nocturia, urgency, incomplete urination, and urinary incontinence.38,40 | Sintomas do trato urinário inferior | Frequentemente associados com bexiga hiperativa, incontinência urinária e cistite intersticial, inclui sintomas de alteração da frequência miccional, noctúria, urgência, micção incompleta e incontinência urinária.38,40 |
| Vaginismus | Genito-pelvic pain disorder in which the involuntary contraction of the PFM interferes with or prevents penetrative sex, the use of tampons, and gynecological examinations.4 | Vaginismo | Transtorno de dor gênito pélvica em que a contração involuntária da músculos do assoalho pélvico, interfere ou impede o sexo penetrativo, utilização de absorventes internos e realização de exames ginecológicos.4 |
| Pudendal neuralgia | Disabling chronic neuropathic pain syndrome caused by mechanical or non-mechanical injuries to the pudendal nerve.4 | Neuralgia do pudendo | Síndrome de dor neuropática crônica incapacitante causada por lesões mecânicas ou não mecânicas do nervo pudendo.4 |
Terms related to evaluation.
| English | Português | ||
|---|---|---|---|
| Terms | Definitions | Termos | Definições |
| Function of the pelvic floor muscles (PFM) | Ability to contract, relax, and coordinate the pelvic floor muscles, responsible for supporting the pelvic organs, urinary continence, anal continence, and sexual function.1 | Função dos músculos do assoalho pélvico | Habilidade de contração, relaxamento e coordenação dos músculos do assoalho pélvico, responsável pela sustentação dos órgãos pélvicos, continência urinária, continência anal e função sexual.1 |
| Pelvic floor muscle dysfunction | Change in the function of the PFM, characterized by the inability to contract, relax, and/or coordinate the pelvic floor muscles.22 | Disfunção dos músculos do assoalho pélvico | Alteração da função dos músculos do assoalho pélvico, caracterizada pela inabilidade de contrair, relaxar e/ou coordenar os músculos do assoalho pélvico.22 |
| Pelvic floor (PF) dysfunction | Change in the function of the PF, that is, changes in the chain of muscles, fascia, and ligaments, which can generate lower urinary tract symptoms, intestinal symptoms, changes in sexual function, prolapse, and pain.1 | Disfunção do assoalho pélvico | Alteração da função do assoalho pélvico, ou seja, alteração na rede de músculos, fáscias e ligamentos, podendo gerar sintomas do trato urinário inferior, sintomas intestinais, alteração na função sexual, prolapso e dor.1 |
| Tender points | Areas of sensitivity that occur in the muscle.4,41 | Pontos sensíveis | Áreas de sensibilidade que ocorrem no músculo. |
| Trigger points | They are discrete, focal, and hyperirritable points located in a tense band of skeletal muscle. They are painful upon compression and can produce pain, sensitivity, motor dysfunction, and/or autonomic phenomena at the site of palpation or referred area.41 | Pontos gatilho | São pontos discretos, focais e hiper irritáveis localizados em uma faixa tensa de músculo esquelético. São dolorosos à compressão e podem produzir dor, sensibilidade, disfunção motora e/ou fenômenos autonômicos no local da palpação ou zona referida.41 |
| Pelvis inspection | Visual assessment of the pelvis and its movements.4 | Inspeção da pelve | Avaliação visual da pelve e de seus movimentos.4 |
| Pelvic floor inspection | Visual observation of the vulva and perineal region.3 | Inspeção do assoalho pélvico | Observação visual da vulva e região perineal.3 |
| Anal palpation | Palpatory examination of anorectal tissues.42 | Palpação anal | Exame palpatório dos tecidos anorretais.42 |
| Perineal palpation | Palpatory examination of the perineum.3 | Palpação perineal | Exame palpatório do períneo.3 |
| Vaginal palpation | Digital examination of the PFM performed by inserting 1 or 2 fingers into the vaginal canal.3 | Palpação vaginal | Exame digital dos músculos do assoalho pélvico realizado pela inserção de 1 ou 2 dedos no canal vaginal.3 |
| Tone | The state of the muscle in general defined by its resting tension clinically determined by resistance to passive movement.5 | Tônus | Estado do músculo geralmente definido pela sua tensão de repouso clinicamente determinada pela resistência ao movimento passivo.5 |
| Decreased PFM tone | Decrease in muscle tone that may be associated with reduced contractile activity and/or decreased passive basal tension of the PFM, assessed through palpation.5 | Tônus diminuido | Diminuição no tônus muscular que pode estar associada à redução da atividade contrátil e/ou diminuição da tensão basal passiva dos músculos do assoalho pélvico, avaliada a partir da palpação.5 |
| Increased PFM tone | Increased muscle tone that may be associated with increased contractile activity and/or increased passive basal tension of the PFM, assessed through palpation.5 | Tônus aumentado | Aumento do tônus muscular que pode estar associado com atividade contrátil elevada e/ou aumento da tensão basal passiva dos músculos do assoalho pélvico, avaliada a partir da palpação.5 |
| Muscle spasm | Sustained involuntary contraction of the muscle.43 | Espasmo muscular | Contração involuntária sustentada do músculo.43 |
| Tenderness | Ability to perceive physical sensations, internal or external stimuli, through the senses.43 | Sensibilidade | Capacidade de perceber sensações físicas, estímulos internos ou externos, através dos sentidos.43 |
| Pain sensitivity | Sensation of pain or painful discomfort generated by stimulation in the PF region.5 | Sensibilidade à dor | Sensação de dor ou desconforto doloroso gerada por estímulo na região do assoalho pélvico.5 |
| Muscle relaxation | Return of the PFM to their original resting position after a voluntary contraction.4 | Relaxamento muscular | Retorno dos músculos do assoalho pélvico para sua posição original de repouso após uma contração voluntária.4 |
| Coordination | Ability to use distinct parts of the body together efficiently. In the pelvic floor, coordination must be an action between the PFM and organic functions (e.g. relaxation of the pelvic floor muscles during urination), PFM and movement of a body segment (e.g. upper limb), and muscles of the PF and an increase in intra-abdominal pressure (e.g. contraction of the PFM before coughing). Coordination is an aspect of motor control.4 | Coordenação | Habilidade em utilizar diferentes partes do corpo juntas de modo eficiente. No assoalho pélvico, coordenação deve ser uma ação entre os músculos do assoalho pélvico e funções orgânicas (ex: relaxamento dos músculos do assoalho pélvico durante a micção), músculos do assoalho pélvico e movimento de um segmento corporal (ex: membro superior) e músculos do assoalho pélvico e um aumento da pressão intra-abdominal (ex: contração dos músculos do assoalho pélvico antes de uma tosse). A coordenação é um aspecto do controle motor.4 |
| Synergy | Co-activation activity of muscle groups that interact to fulfill a specific function.44 | Sinergia | Atividade de co-ativação de grupos musculares que se relacionam para cumprir uma função específica.44 |
| Dyssynergy | Paradoxical contraction of the PFMs. A coordination dysfunction between the PFM and a functional activity, such as PFM contraction when relaxation is functionally required.4 | Dissinergia | Contração paradoxal dos músculos do assoalho pélvico (MAP). Uma disfunção de coordenação entre os MAP e uma atividade funcional, como a contração dos MAP quando o relaxamento é funcionalmente requerido.4 |
| Strength | Force generating capacity of a muscle. Commonly expressed by the measurement of maximum voluntary contraction (MVC).43 | Força | Capacidade de geração de força de um músculo. Comumente expressa pela medida da contração voluntária máxima (CVM).43 |
| Endurance | Ability of the PFM to perform repeated contractions or maintain a contraction for a predetermined period.43 | Resistência | Capacidade dos músculos do assoalho pélvico em realizar contrações repetidas ou manter uma contração por um período predeterminado.43 |
| Fast contraction | It is the contraction that corresponds to the contractility of the fast muscle fibers obtained from the verbal command to contract and relax without requesting the maintenance of the contraction.36 | Contração rápida | É a contração que corresponde à contratilidade das fibras musculares rápidas obtidas a partir do comando verbal contrai e relaxa sem solicitar sustentação da contração.36 |
| Slow contraction | It is the contraction that corresponds to the contractility of the slow muscle fibers obtained from the verbal command to contract and sustain the contraction for as many seconds as possible.4 | Contração lenta | É a contração que corresponde à contratilidade das fibras musculares lentas obtidas a partir do comando verbal contrai e sustenta a contração pelo maior número de segundos que conseguir.4 |
| Pelvic floor contraction | Contraction felt as a squeezing, compressing, and elevating action of the evaluator's finger towards the pubic symphysis.4 | Contração do assoalho pélvico | Contração sentida como uma ação de aperto, compressão e elevação do dedo do avaliador em direção à sínfise púbica.4 |
| Maximum voluntary contraction | Voluntary activation of the PFM, with maximum muscle contraction capacity.4 | Contração voluntária máxima | Ativação voluntária dos músculos do assoalho pélvico, com a capacidade máxima de contração muscular.4 |
| Fatigue | Decreased ability to perform maximal voluntary muscle contraction or a series of repetitive contractions.4 | Fadiga | Capacidade diminuída para realizar a contração muscular voluntária máxima ou uma série de contrações repetitivas.4 |
| Anal reflex | Reflex contraction of the anal sphincter in response to a brief, superficial stimulus in the anal region.5 | Reflexo anal | Contração reflexa do esfíncter anal em reposta a um estímulo breve e superficial na região anal.5 |
| Clitoral reflex | Reflex contraction of the anal and bulbocavernosus sphincter in response to compression of the clitoris.5 | Reflexo clitoriano | Contração reflexa do esfíncter anal e bulbocavernoso em resposta à compressão do clitóris.5 |
| Perineal body length | Distance from the posterior margin of the vestibule to the anterior anal margin.7 | Comprimento do corpo perineal | Distância da margem posterior do vestíbulo até a margem anal anterior.7 |
| Perineal body mobility | Discreet movement felt by the evaluator from the slight compression of the perineal body, which is a complex fibromuscular mass between the terminal ends of the urogenital and anorectal system.45 | Mobilidade do corpo perineal | Movimento discreto sentido pelo avaliador a partir da leve compressão do corpo perineal que é uma Massa fibromuscular complexa entre as extremidades terminais do sistema urogenital e anorretal.45 |
The data obtained from the initial systematic review are presented in Supplementary material 2. The steering group delved into the 22 retained terminology guides related to the female PF1,3–8,15–29 and listed 57 terms and their definitions that were incorporated into a guideline for the Delphi process.
The expert professional group consisted of 19 physical therapists and 2 physicians representing the five regions of Brazil. The mean (SD) age of the participants was 42.8 (6.3) years, with an average of 20.6 (6.5) years of academic experience.
Of the 57 terms included in this guideline for the Delphi process, 52 (90%) achieved an 80% consensus in the first round, and 5 (10%) terms (PF, perineum, motor symptoms of the PFM, PF myofascial pain syndrome, and vaginismus) required more than one round to reach consensus.
Table 1 presents 12 terms related to PF anatomy, considering the components of muscular, connective, and bone tissues and the definition of synergistic muscles of the PF.
Table 2 presents 14 terms related to signs and symptoms of PF. It includes sensory and motor symptoms.
Table 3 presents 31 terms related to evaluation of PF function and dysfunction, from inspection to quality of muscle contraction.
ConclusionThis guideline proposes a consensus of Brazilian-Portuguese terminology related to anatomy, signs/symptoms, and assessment of the PF muscles in the female population, based on a systematic and updated review of the scientific literature. This consensus involved 21 professional experts in teaching and/or research in the field of Women's Health/Pelvic Floor. The clear definition of PF terminology in Brazilian Portuguese language represents an important advance in clinical communication and scientific research. The terminology allows for an objective description of clinical practice and scientific discussion without ambiguity of terminology, making understanding difficult. The expectation is that this terminology guideline will be widely used, from undergraduate teaching to the description and conduct of research and clinical practice to evaluate the function and treatment of PF dysfunctions.
Aline Teixeira Alves, Ana Beatriz Gomes de Souza Pegorare, Angélica Mércia Pascon Barbosa, Cristiane Carboni, Elyonara Mello de Figueiredo, Janeisa Frank Virtuoso, João Simão de Melo Neto, Juliana Falcão Padilha, Lilian Rose Mascarenhas, Luciana Mamede Gomes, Mariana Tirolli Rett Bergamasco, Marianne Lucena da Silva, Melissa Medeiros Braz, Rubneide Barreto Silva Gallo, Simony Lira do Nascimento, Tatiana de Bem Fretta e Thaiana Bezerra Duarte.
Professional Perspectives