The assessment of functional capacity in individuals with cardiovascular disease is closely related to lower limb function. The Glittre-ADL test is a global test to evaluate this patients.
ObjectiveWe aimed to verify whether the Glittre-ADL test discriminates functional status while evaluating individuals with cardiovascular disease.
MethodsA total of 42 participants were evaluated using the Glittre-ADL test Incremental Shuttle Walking Test (shuttle test), Human Activity Profile, and Duke Activity Status Index. Data from the shuttle test, Human Activity Profile, and DASI were divided into tertiles for statistical analysis. The time required to complete the Glittre-ADL test was compared among tertiles of the shuttle test, Duke Activity Status Index and Human Activity Profile using analysis of variance.
ResultsThere were significant differences between the tertiles of the shuttle test. Tertile 1 was different from tertiles 2 (mean difference, 47.63; 95% CI, 19.86–75.39) and 3 (mean difference, 67.15; 95% CI, 41.25–93.05). For the Duke Activity Status Index there were significant between-group differences. Tertile 1 was different from tertiles 2 (mean difference, 42.45; 95% CI, 8.82–76.09) and 3 (mean difference, 43.56; 95% CI, 13.68–73.44). For the Human Activity Profile there were significant between-group differences. Tertile 3 was different from tertiles 1 (mean difference, 51.46; 95% CI, 21.27–81.64) and 2 (mean difference, 33.01; 95% CI, 3.52–62.51).
ConclusionThe Glittre-ADL test is able to discriminate the functional status in individuals with cardiovascular disease, most of whom have hypertension. The Glittre-ADL test was sensitive to discriminate more functionally affected individuals.
Cardiovascular diseases (CVDs) are caused by the interaction of genetic and environmental factors.1 They are considered a public health issue2 and have a negative impact on quality of life and functional capacity. The most prevalent CVDs are hypertension, coronary artery disease, heart failure, cerebrovascular disease, and peripheral arterial disease.1
The assessment of functional capacity in CVD patients is important in clinical practice, as it helps understand the level of limitation in the individual's life.3 Functional capacity can be evaluated by maximal tests, which are considered the gold standard,4 followed by submaximal tests, scales, or questionnaires.3 The use of maximal tests in clinical practice could present some difficulties because of the need of high-cost equipment and a well-trained team. Therefore, other resources have been widely used for evaluating functional capacity, such as submaximal tests, questionnaires, and scales.4 These tools can be useful for evaluating functional capacity as well as responses to interventions.4 The 6-minute walk test and Incremental Shuttle Walk Test (ISWT) are usually used as submaximal tests.5,6 Since most daily activities are accomplished at a submaximal level, these tests can closely reflect the subject's level of functionality.5 The 6-minute walk test evaluates the longest distance an individual can walk, at the highest speed possible, on a 30-m flat surface for 6min.5 The ISWT involves walking down a 10-m aisle, at a progressive speed, marked by beeps.6 When compared to the 6-minute walk test, the ISWT presented higher reliability coefficients, better associations with hemodynamic variables,7 and better correlation with oxygen consumption.8 Furthermore, the ISWT evaluates the gradual cardiovascular response to progressive stress6 and is useful in individuals with distinct functional capacity. The ISWT is considered a reference test to measure functional capacity at a submaximal level. This test is often used in cardiovascular evaluation and involves exclusive lower limb function. This limits the capacity of the ISWT to evaluate daily activities, which require the frequent use of the upper limbs. The physiological response caused by upper limb activities differs from that caused by lower limb activities.9 For a certain oxygen consumption rate, both the heart rate (HR) and blood pressure (BP) are higher for activities involving the upper limbs in comparison to those involving the lower limbs,9 potentially causing higher cardiac overload. Thus, considering that the assessment of functional capacity of individuals with CVD should include both the upper and lower limbs, there is a need for global tests capable of achieving a broader evaluation, with diverse tasks that are more similar to those of the individual's daily activities.
The Glittre-ADL test (TGlittre) was initially developed to test the functional capacity of individuals with chronic obstructive pulmonary disease.10 The TGlittre covers different tasks performed with the lower and upper limbs such as sitting down and getting up, walking, going up and down the stairs, reaching, hand gripping, and moving weight.10 The TGlittre can be potentially used in clinical practice and can help in understanding the impact of health conditions in the daily life of individuals with CVD. The sensitivity of the TGlittre for discriminating individuals with CVD of different functional capacities and the safety of its use in this population have not been evaluated. The primary objective of this study was to verify whether the TGlittre is able to discriminate functional status in individuals with CVD. The secondary objective was to compare the hemodynamic responses between the TGlittre and ISWT.
MethodsStudy designThis was a cross-sectional study.
SampleThe sample consisted of individuals diagnosed as having CVD (by a cardiologist), aged between 18 and 80 years, with no underlying conditions that could interfere with the completion of the tests, such as orthopedic, rheumatologic, or neurological dysfunctions. Moreover, individuals with a recent episode of acute myocardial infarction (within a month), unstable angina, uncontrolled arrhythmia or heart failure, thrombophlebitis or intracardiac thrombus, recent pulmonary or systemic embolism, or pulmonary edema were excluded from the study. To perform the tests, the individuals had to be clinically stable for at least 2 months (no hospitalizations or emergency visits). Individuals with systolic BP higher than 160mmHg or diastolic BP higher than 105mmHg at rest,11 peripheral oxygen saturation lower than 85% at rest or during exercise, and HR higher than 90% of the maximum predicted for that individual (HRmax)12 were also excluded from the study. The Mini-Mental state examination was conducted in individuals 60 years of age or older, and a score lower than the cut-off point established by Bertolucci et al.13 was considered a criterion for exclusion. The present study was approved by the Research Ethics Committee of Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, MG, Brazil (approval number CAAE-23348813.7.0000.5149). All participants provided informed consent.
EvaluationsThe TGlittre, ISWT, Duke Activity Status Index (DASI), and Human Activity Profile (HAP) questionnaires were administered by well-trained evaluators. The TGlittre was conducted by a trained examiner. The DASI and HAP are questionnaires used to evaluate CVD patients and were chosen as instruments for the present study since they distinctly focus on evaluating the functional condition. Prior to data collection, the test–retest reliability of the TGlittre was evaluated in nine individuals with CVD (age, 57.22±15.43 years) and showed an intra-class correlation coefficient of 0.92 (95% confidence interval [CI], 0.69–0.98).
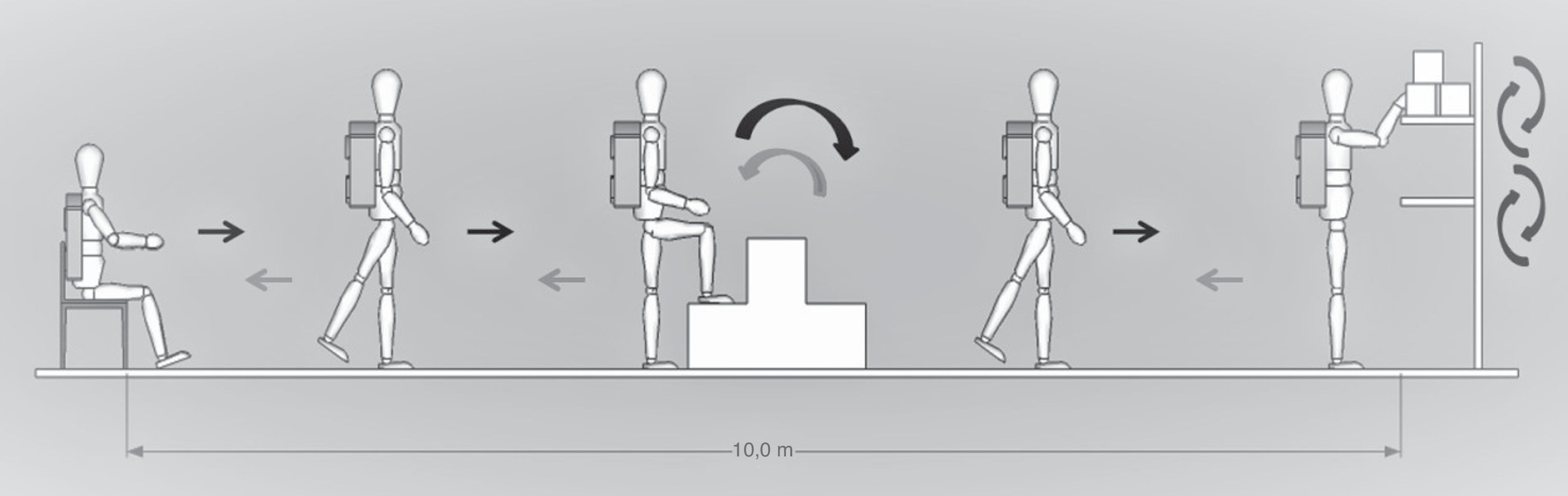
The TGlittre, which evaluates functional capacity, was administered as described previously by Skumlien et al.10 (Fig. 1). For this test, the subjects were first seated, carrying a backpack (weighing 2.5kg for women and 5kg for men). Then, the subjects had to walk down a 10-m aisle, with a stairway halfway through, to reach a shelf where they had to move 3 weights (1kg each) from the upper shelf (at the level of the shoulder girdle) to the lower shelf (at the level of the pelvis), and then to the ground. Next, they had to do the reverse order, placing the weights on the upper shelf and returning to the initial seating position. The test ended after five cycles were completed. The subjects were instructed to complete the test as quickly as possible. They were allowed to rest during the test, but were requested to resume the test as soon as possible. The subjects were not encouraged during the test, and the main parameter was the total time required for the completion of the test.10,14–16
The ISWT was selected in the present study as a direct measure of exercise capacity. This test was administered as previously described by Singh et al.6 The BP, HR, and peripheral oxygen saturation were measured during the ISWT and TGlittre. The modified Borg scale was used to evaluate the subjective perceived exertion before and after the tests.17 The tests were stopped if a subject presented dyspnea that would not allow the continuation of the exercise, paleness, dizziness, or chest pain or if the HR increased to more than 90% of the HRmax.11
The DASI is a valid questionnaire for evaluating the functional condition of individuals with CVD and it has been translated and culturally adapted to the Brazilian population.18 The DASI comprises 12 items that represent daily life activities (personal care, ambulation, household tasks, sexual function, and recreation).18,19 In the present study, the DASI was administered in the form of an interview.18 The final score varied between 0 and 58.2 points and was calculated according to the specific weight of each item based on the metabolic consumption. A higher score implied better functional capacity.18
The HAP, an instrument previously used to evaluate CVD patients,20 evaluates functional condition, considering the level of physical activity.20,21 This test comprises 94 items organized according to energy consumption. For each item, there are three possible responses: “still doing”, “stopped doing”, or “never done”. Based on the responses, the maximum activity score and adjusted activity score are calculated. The maximum activity score corresponds to the notation of the highest energy-demanding activity that the individual is “still doing”, with no mathematical calculation. The adjusted activity score is calculated by deducting the number of items the subject “stopped doing” from the maximum activity score, prior to the last activity the subject was “still doing”. The subjects were rated according to the adjusted activity score as inactive (score lower than 53), moderately active (score between 53 and 74), and active (score higher than 74).21 In the present study, the HAP was also administered by interview.
Data collecting procedureData collection began by randomizing the order of the administration of the ISWT and TGlittre through a blind drawing by the subject from a black sealed envelope. After the administration of the first test, a resting period of at least 20min or the necessary time for the stabilization of hemodynamic parameters was allowed.22 Meanwhile, the DASI or HAP questionnaires were administered in randomized order. After this step, the second test was carried out and the second questionnaire was administered.
Sample size calculationBased on a pilot study, the effect size (f) of the difference between the tertiles obtained from the ISWT (f=0.70), HAP (f=0.60), and DASI (f=0.50) was calculated. For a lower f (0.50) and power of 0.80, an alpha level of 5% corresponded to an n of 14 individuals per group (tertile), with a total of 42 individuals.
Statistical analysisData distribution was evaluated using the Shapiro–Wilk test. Data from the ISWT (distance in meters), HAP (adjusted activity score), and DASI (score) were divided into tertiles to verify if the TGlittre was able to discriminate functional classes. The tertiles were defined by dividing the sample into three different functional capacity levels: low, moderate, and high.23 The comparison of the TGlittre times between different groups divided by the ISWT, PAH, and DASI tertiles was performed by one-way analysis of variance with a post hoc least significant difference test. For the comparison of the hemodynamic responses between the TGlittre and ISWT, the t-test was used, paired for all variables except perceived exertion (Borg scale), for which the Wilcoxon test was used. For statistical significance, an alpha level of 5% was considered. For all analyses, the Statistical Package for Social Sciences® version 15.0 (SPSS Inc., Chicago, IL, USA) was used.
ResultsWe recruited 52 subjects, of whom 10 were excluded: seven showed more than 90% of HRmax, one reported pain around the breastbone area (myocardial restoration surgery), one stopped the test before completion because of claudication symptoms, and another subject did not start the test because of chest pain, resulting in 42 evaluated volunteers.
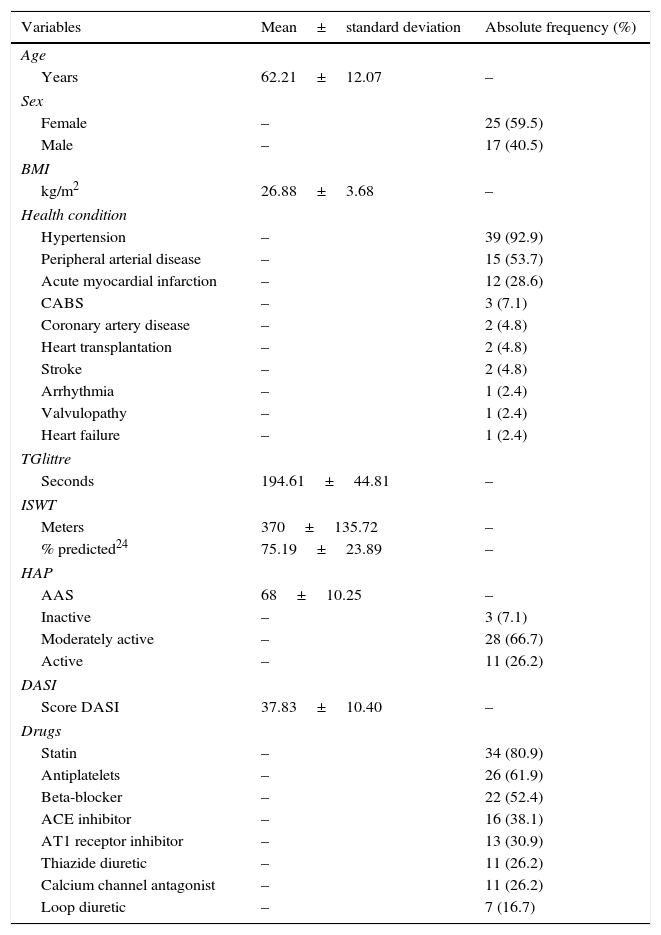
Table 1 shows the characteristics of the study subjects, as well as the test and questionnaire results.
Characteristics of the study population (n=42).
| Variables | Mean±standard deviation | Absolute frequency (%) |
|---|---|---|
| Age | ||
| Years | 62.21±12.07 | – |
| Sex | ||
| Female | – | 25 (59.5) |
| Male | – | 17 (40.5) |
| BMI | ||
| kg/m2 | 26.88±3.68 | – |
| Health condition | ||
| Hypertension | – | 39 (92.9) |
| Peripheral arterial disease | – | 15 (53.7) |
| Acute myocardial infarction | – | 12 (28.6) |
| CABS | – | 3 (7.1) |
| Coronary artery disease | – | 2 (4.8) |
| Heart transplantation | – | 2 (4.8) |
| Stroke | – | 2 (4.8) |
| Arrhythmia | – | 1 (2.4) |
| Valvulopathy | – | 1 (2.4) |
| Heart failure | – | 1 (2.4) |
| TGlittre | ||
| Seconds | 194.61±44.81 | – |
| ISWT | ||
| Meters | 370±135.72 | – |
| % predicted24 | 75.19±23.89 | – |
| HAP | ||
| AAS | 68±10.25 | – |
| Inactive | – | 3 (7.1) |
| Moderately active | – | 28 (66.7) |
| Active | – | 11 (26.2) |
| DASI | ||
| Score DASI | 37.83±10.40 | – |
| Drugs | ||
| Statin | – | 34 (80.9) |
| Antiplatelets | – | 26 (61.9) |
| Beta-blocker | – | 22 (52.4) |
| ACE inhibitor | – | 16 (38.1) |
| AT1 receptor inhibitor | – | 13 (30.9) |
| Thiazide diuretic | – | 11 (26.2) |
| Calcium channel antagonist | – | 11 (26.2) |
| Loop diuretic | – | 7 (16.7) |
AAS, adjusted activity score; BMI, body mass index; CABS, coronary artery bypass surgery; DASI, Duke Activity Status Index; HAP, Human Activity Profile; ISWT, Incremental Shuttle Walking Test; TGlittre, Glittre ADL test runtime.
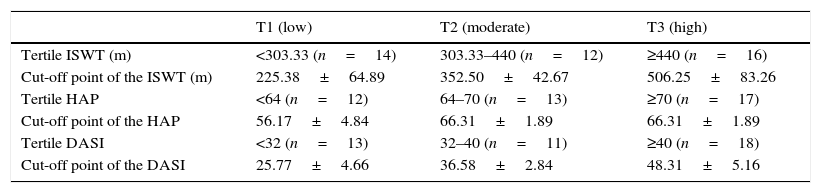
The division of tertiles of the ISWT, DASI, and HAP and the average of the results in each tertile are shown in Table 2.
Division of the ISWT, DASI, and HAP by tertiles and the mean of the results in the sample studied by tertiles (n=42).
| T1 (low) | T2 (moderate) | T3 (high) | |
|---|---|---|---|
| Tertile ISWT (m) | <303.33 (n=14) | 303.33–440 (n=12) | ≥440 (n=16) |
| Cut-off point of the ISWT (m) | 225.38±64.89 | 352.50±42.67 | 506.25±83.26 |
| Tertile HAP | <64 (n=12) | 64–70 (n=13) | ≥70 (n=17) |
| Cut-off point of the HAP | 56.17±4.84 | 66.31±1.89 | 66.31±1.89 |
| Tertile DASI | <32 (n=13) | 32–40 (n=11) | ≥40 (n=18) |
| Cut-off point of the DASI | 25.77±4.66 | 36.58±2.84 | 48.31±5.16 |
DASI, Duke Activity Status Index; HAP, Human Activity Profile; ISWT, Incremental Shuttle Walking Test; T1, tertile 1; T2, tertile 2; T3, tertile 3.
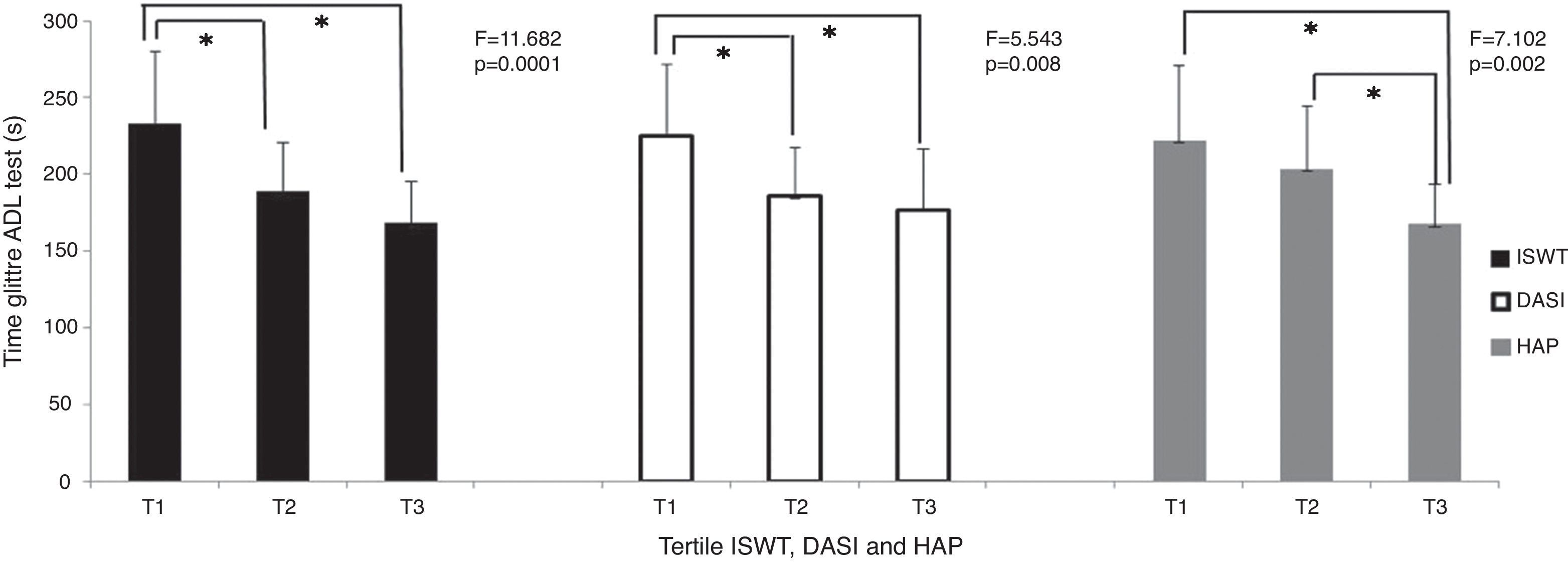
In relation to the time of execution of the TGlittre, there was a statistically significant difference between the ISWT, PAH, and DASI tertiles (Fig. 2). Dividing the sample by the ISWT scores, tertile 1 was different from tertiles 2 (average of the difference, 47.63; 95% CI, 19.86–75.39) and 3 (average of the difference, 67.15; 95% CI, 41.25–93.05). Dividing the sample by the DASI scores, tertile 1 was different from tertiles 2 (average of the difference, 42.45; 95% CI, 8.82–76.09) and 3 (average of difference, 43.56; 95% CI, 13.68–73.44). Dividing the sample by the HAP scores, tertile 3 was different from tertiles 1 (average of the difference, 51.56; 95% CI, 21.27–81.64) and 2 (average of the difference, 33.01; 95% CI, 3.52–62.51).
Comparison of the TGlittre runtime between tertiles of ISWT, HAP and DASI.
*Anova; post hoc LSD; p<0.05; Time Glittre ADL test in seconds; ISWT, Incremental Shuttle Walking Test; DASI, Duke Activity Status Index; HAP, Human Activity Profile. Tertile ISWT: T1=<303.33m, T2=between 303.33 and 440m, T3=≥440m; Tertile DASI: T1=<32, T2=between 32 and 40, T3=≥40; Tertile HAP: T1=<64, T2=between 64 and 70, T3=≥70.
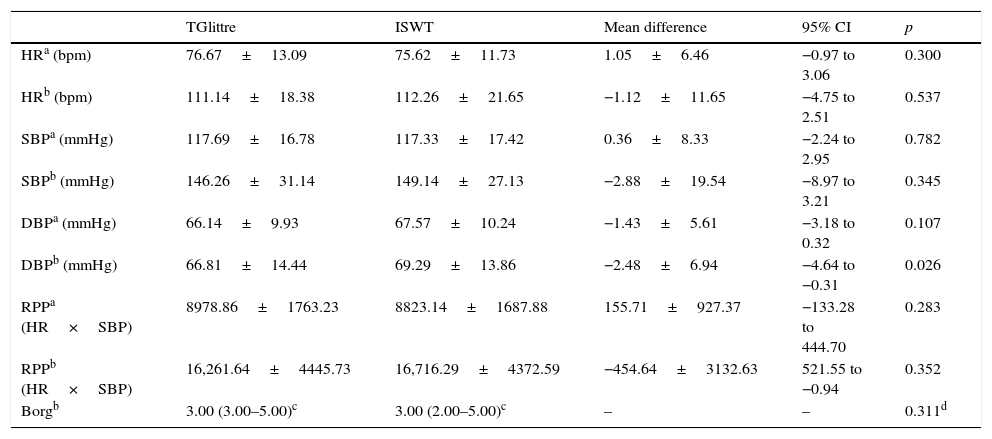
When comparing the hemodynamic responses between the TGlittre and ISWT, no significant difference was observed for most of the evaluated variables, except for the final diastolic BP (Table 3).
Comparison of hemodynamic responses generated by the TGlittre and ISWT (n=42).
| TGlittre | ISWT | Mean difference | 95% CI | p | |
|---|---|---|---|---|---|
| HRa (bpm) | 76.67±13.09 | 75.62±11.73 | 1.05±6.46 | −0.97 to 3.06 | 0.300 |
| HRb (bpm) | 111.14±18.38 | 112.26±21.65 | −1.12±11.65 | −4.75 to 2.51 | 0.537 |
| SBPa (mmHg) | 117.69±16.78 | 117.33±17.42 | 0.36±8.33 | −2.24 to 2.95 | 0.782 |
| SBPb (mmHg) | 146.26±31.14 | 149.14±27.13 | −2.88±19.54 | −8.97 to 3.21 | 0.345 |
| DBPa (mmHg) | 66.14±9.93 | 67.57±10.24 | −1.43±5.61 | −3.18 to 0.32 | 0.107 |
| DBPb (mmHg) | 66.81±14.44 | 69.29±13.86 | −2.48±6.94 | −4.64 to −0.31 | 0.026 |
| RPPa (HR×SBP) | 8978.86±1763.23 | 8823.14±1687.88 | 155.71±927.37 | −133.28 to 444.70 | 0.283 |
| RPPb (HR×SBP) | 16,261.64±4445.73 | 16,716.29±4372.59 | −454.64±3132.63 | 521.55 to −0.94 | 0.352 |
| Borgb | 3.00 (3.00–5.00)c | 3.00 (2.00–5.00)c | – | – | 0.311d |
This study showed that the TGlittre was able to discriminate the functional classes of individuals with CVD, especially in the more affected ones. In addition, the hemodynamic responses to the TGlittre and ISWT were similar. The TGlittre was able to discriminate subjects who walked less than 303.33m during the ISWT and presented scores lower than 32 in the DASI. Similar to the results of the present study, Skumlien et al.10 highlighted that the test offers additional information about daily life activities, especially in individuals with serious CVD. Correa et al.15 showed that the TGlittre was able to differentiate between the performance of healthy individuals and those with chronic obstructive pulmonary disease.
When comparing the TGlittre time of execution among HAP tertiles, a distinct behavior was noticed in relation to the ISWT and DASI. Concerning the HAP, the TGlittre was able to discriminate individuals with better functional capacity (score HAP≥70). For the HAP, individuals with a score lower than 53, between 53 and 74, and higher than 74 are considered inactive, moderately active, and active, respectively. In the present study groups, T1 and T2 presented an HAP average score of 56.17±4.84 and 66.31±1.89, respectively, and were classified as moderately active. In this study, T1 and T2 were similar groups because they fit the same classification according to the questionnaire interpretation. Furthermore, it should be considered that this difference between the DASI and HAP could also be a consequence of the questionnaires involving distinct constructs. The HAP measures the functional condition according to the level of physical activity, physical aptitude, and energetic consumption,21 while the DASI measures the functional condition with a focus on perceived functional capacity during daily life activities. In this regard, the DASI represents a construct closer to the TGlittre, and therefore, the TGlittre can discriminate the functional classes divided by the DASI more accurately. A systematic review of the HAP21 reported that, as the HAP is a measure of physical aptitude, stronger correlations are observed between its score and other measures of physical aptitude, and weaker correlations are observed with measures of distinct constructs.21 Another factor that should be considered is that the DASI is more applicable in individuals with moderate to low functional capacity.18,25 This is in accordance with the results of this present study in relation to the TGlittre, which was able to discriminate the group most affected by CVD.
Individuals of this study completed the TGlittre in 194.61±44.81s, which equals 3.24min. The time to complete the TGlittre in the present study was shorter than that reported in the literature. In a study by Valadares et al.,26 individuals with heart failure completed the test in 6.3±4.8min. In a study by Correa et al.,15 individuals with chronic obstructive pulmonary disease completed the test in 5.26±2.9min. The time to complete the TGlittre was 4.77±1.46min and around 4min according to studies by Karloh et al.27 and Tufanin et al.,28 respectively. In a study by Skumlien et al.,10 which also included individuals with chronic obstructive pulmonary disease, the time to complete the TGlittre was around 4min. In the same study, the authors suggested that 2min is the shortest time in which individuals can complete the test without violating the protocol.10 Therefore, although the individuals in the present study completed the test within a shorter time, it was considered adequate.10 This difference in the time to complete the TGlittre of approximately 1min between the present study and other studies is clinically important16 and can be explained by the fact that the studies evaluated different health conditions. Furthermore, only 7.1% of the sample in the present study was classified as inactive according to the HAP, which explains the superior performance among the subjects in the present study compared to that of subjects in the other studies.
When hemodynamic responses generated by the TGlittre and ISWT were compared, significant differences were not found for most variables analyzed, except for the final diastolic BP, which was significantly lower for the TGlittre; however, this difference is not considered clinically relevant. This result suggests that, from a hemodynamic perspective, both tests produce similar overload. Furthermore, individuals showed the same perceived exertion through the Borg scale. Although the TGlittre and ISWT hemodynamic responses were similar, as the average completion time for the TGlittre remained around 3min, this test could be classified as predominantly anaerobic. Daily life activities have different duration and intensity29,30 and are often not confined to stable conditions. Therefore, the ISWT and TGlittre are complementary, since the predominant anaerobic character and irregularity of activities performed in the TGlittre contribute relevant information in relation to walking.27
Of the 13.4% of subjects who had the TGlittre interrupted because of an HR over 90% of the HRmax, 85.7% interrupted the test during the second half of the third lap. The studies by Karloh et al.27 and Tufanin et al.28 found a plateau in the cardiac and respiratory variables, including the HR, during the third lap. A reduction in the number of laps for the most stricken individuals may be necessary adaptation for the test's protocol. The present study is one of the first to investigate the usefulness of the TGlittre in individuals with CVD; therefore, further studies are necessary to elucidate the assumptions raised.
Normal values for the TGlittre are still unknown, which can represent a limitation for the interpretation of the results obtained. Nevertheless, we observed that the completion time for the test (around 3min) is close to the completion time in studies with healthy subjects,15 which reveals a good performance of the studied sample. One of the limitations of the present study is that only one subject had heart failure, which is a disease associated with exercise intolerance.29 Furthermore, the target population of the present study was broad, which limits the clinical implication of the results. Thus, this research should be considered as a pilot study, and new studies on the use of the TGlittre for assessment of specific health conditions are needed for greater clinical applicability of the test in individuals with CVD.
In conclusion, the TGlittre can discriminate functional classes of individuals with CVD, most of whom are hypertensive and severely affected by the disease. This test should not be used indiscriminately to substitute tests currently used for evaluating functional capacity, such as the ISWT. The TGlittre may be considered an additional tool to evaluate individuals with CVD.
Conflicts of interestThe authors declare no conflicts of interest.
We wish to thank Pró-Reitoria de Pesquisa da Universidade Federal de Minas Gerais for their financial support.