The aims of this study were to determine, in Australian pulmonary rehabilitation programs for people with COPD: (1) whether oxygen saturation (SpO2) was monitored during exercise testing; (2) whether supplemental oxygen was available during exercise testing and/or training; (3) whether oxygen was prescribed during exercise training; and the reason for providing oxygen; (4) whether a protocol was available for supplemental oxygen prescription during exercise training.
MethodsThis was a cross-sectional multi-center study using a purposed-designed survey. De-identified survey data were analyzed and the absolute number and percentage of responses were recorded for each question.
ResultsThe survey was sent to 261 pulmonary rehabilitation programs and 142 surveys (54%) were available for analysis. Oxygen saturation was monitored during exercise testing in 92% of programs. Supplemental oxygen was available in the majority of programs during exercise testing (82%) and training (84%). The rationale cited by 87 programs (73%) for prescribing oxygen during exercise training was maintaining SpO2 above a threshold ranging from SpO2 80–88%. Forty-five (32%) programs had a protocol for oxygen prescription during exercise training.
ConclusionWhile monitoring of SpO2 during exercise testing and using supplemental oxygen during testing and training is common in Australian pulmonary rehabilitation programs, few programs had a protocol in place for the prescription of supplemental oxygen for people with COPD who were not on long-term oxygen therapy. This may be due to lack of strong evidence to support the use of supplemental oxygen during exercise training.
Exercise-induced oxygen desaturation is common in people with chronic obstructive pulmonary disease (COPD).1–3 One Australian study reported that 47% of patients with COPD referred to pulmonary rehabilitation had a fall in oxygen saturation (SpO2) of more than 4% to a SpO2 of less than 90% during a six-minute walk test.1 Availability of supplemental oxygen is recommended for provision of a pulmonary rehabilitation program4,5 as it may be required during exercise testing or training in people with COPD who demonstrate oxygen desaturation or in case of an emergency. The rationale for use of oxygen is based on laboratory studies that have shown that oxygen administration during a single bout of exercise reduces minute ventilation at equivalent work rates and delays the onset of dynamic hyperinflation and the associated dyspnea in people with COPD who had severe disease.6,7
While there have been a number of national pulmonary rehabilitation surveys conducted in Australia,8 New Zealand,9 United States of America,10 United Kingdom11 and Canada,12 these surveys have focused on reporting current practice in terms of setting, access, structure, and the outcome measures from pulmonary rehabilitation programs. Information on how and why supplemental oxygen is utilized during programs for both exercise testing and exercise training is lacking. The National Canadian Survey reported that most pulmonary rehabilitation programs (90%) had supplemental oxygen available but no information was provided on whether SpO2 was monitored during exercise testing or how or why supplemental oxygen was prescribed during exercise training.12 The national pulmonary rehabilitation audit in the United Kingdom11 did not report supplemental oxygen availability but did report that 9% of pulmonary rehabilitation attendees used supplemental oxygen during exercise training.11 The report did not specify if these attendees were people on long-term oxygen therapy or were people who experienced exercise-induced oxygen desaturation and were provided with supplemental oxygen during exercise training.
The aims of this study were to determine, in Australian pulmonary rehabilitation programs for people with COPD: (1) whether oxygen saturation (SpO2) was monitored during exercise testing; (2) whether supplemental oxygen was available during exercise testing and/or training; (3) whether oxygen was prescribed during exercise training; and the reason for providing oxygen; (4) whether a protocol was available for supplemental oxygen prescription during exercise training.
MethodsStudy design and participantsThis was a cross-sectional multi-center study using a survey. The manager of the Lung Foundation Australia COPD national program sent an email on behalf of the researchers to the representatives of all pulmonary rehabilitation programs listed on the Lung Foundation Australia registry (n=261), inviting them to participate in the study via a link to the survey. The representatives were provided with an information sheet about the study and consent was implicit if the survey was returned. Emails were sent on three occasions between July 2015 and February 2016 to maximize the response rate. Approval was obtained from the University of Sydney Ethics Committee. The study was registered with the Australian New Zealand Clinical Trials Registry: ACTRN12616000813482.
SurveyA survey was developed by three experienced pulmonary rehabilitation clinicians. Eight pulmonary rehabilitation clinicians from six pulmonary rehabilitation programs in different Australian states tested the survey. Based on feedback, minor changes to the wording were made to enhance comprehension of the questions. The survey was divided into two sections. The first section collected the respondent's demographic information such as profession and years of experience in pulmonary rehabilitation plus information about the program setting and size (i.e. the number of participants who commenced rehabilitation each year at the site). The second section asked about whether SpO2 was monitored during exercise testing, the availability of supplemental oxygen during exercise testing and training, how supplemental oxygen was prescribed during exercise training, and whether a protocol was available for the prescription of supplemental oxygen during exercise training for people with COPD who were not on long-term oxygen therapy. A copy of the survey is in Supplementary Appendix 1 (online).
Survey data were collected and managed using Research Electronic Data Capture (REDcap) hosted at the University of Sydney.13 REDCap is a secure, web-based application designed to support data capture for research studies.
Data analysisDe-identified survey data were analyzed. The absolute number and percentage of responses were recorded for each question. Univariate cross-tabs were calculated with SPSS (version 22) to determine whether there were associations between years of experience of the health professionals or the size of the pulmonary rehabilitation program with responses to survey questions related to the management of patients during exercise testing or training.
ResultsData were collected between November 2015 and April 2016. Of 261 email invitations sent, 148 surveys (57%) were returned. Six surveys were discarded due to incomplete information and 142 surveys were included in the analysis.
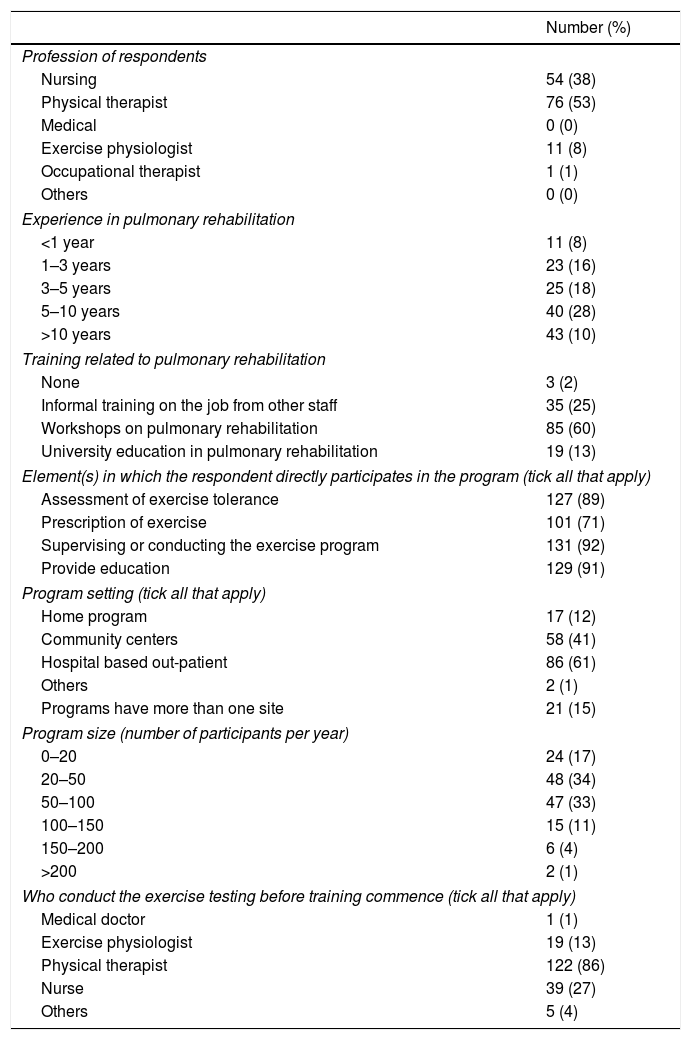
Characteristic information of respondents and pulmonary rehabilitation programsCharacteristics of the respondents and pulmonary rehabilitation programs are presented in Table 1. All programs included an exercise testing component, with the majority (99%, n=141) using the six-minute walk test (6MWT). The responder who did not choose 6MWT as the assessment tool also did not specify which tool was used during assessment.
Characteristics of respondents and pulmonary rehabilitation programs.
| Number (%) | |
|---|---|
| Profession of respondents | |
| Nursing | 54 (38) |
| Physical therapist | 76 (53) |
| Medical | 0 (0) |
| Exercise physiologist | 11 (8) |
| Occupational therapist | 1 (1) |
| Others | 0 (0) |
| Experience in pulmonary rehabilitation | |
| <1 year | 11 (8) |
| 1–3 years | 23 (16) |
| 3–5 years | 25 (18) |
| 5–10 years | 40 (28) |
| >10 years | 43 (10) |
| Training related to pulmonary rehabilitation | |
| None | 3 (2) |
| Informal training on the job from other staff | 35 (25) |
| Workshops on pulmonary rehabilitation | 85 (60) |
| University education in pulmonary rehabilitation | 19 (13) |
| Element(s) in which the respondent directly participates in the program (tick all that apply) | |
| Assessment of exercise tolerance | 127 (89) |
| Prescription of exercise | 101 (71) |
| Supervising or conducting the exercise program | 131 (92) |
| Provide education | 129 (91) |
| Program setting (tick all that apply) | |
| Home program | 17 (12) |
| Community centers | 58 (41) |
| Hospital based out-patient | 86 (61) |
| Others | 2 (1) |
| Programs have more than one site | 21 (15) |
| Program size (number of participants per year) | |
| 0–20 | 24 (17) |
| 20–50 | 48 (34) |
| 50–100 | 47 (33) |
| 100–150 | 15 (11) |
| 150–200 | 6 (4) |
| >200 | 2 (1) |
| Who conduct the exercise testing before training commence (tick all that apply) | |
| Medical doctor | 1 (1) |
| Exercise physiologist | 19 (13) |
| Physical therapist | 122 (86) |
| Nurse | 39 (27) |
| Others | 5 (4) |
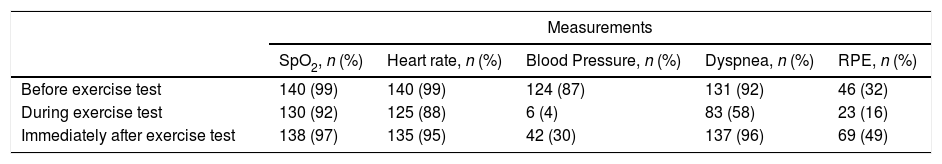
The number of programs using objective measurements during exercise testing can be found in Table 2. Respondents reported that SpO2 was monitored before (n=140, 99%), during (n=130, 92%), and after (n=138, 97%) exercise testing with 85% (n=121) indicating that SpO2 was recorded at least once per minute during an exercise test. One hundred and nineteen respondents (84%) reported that a finger probe was used for oxygen monitoring with the remainder using forehead probe (n=1, 0.5%), ear probe (n=1, 0.5%), and 21 respondents (15%) reported that the choice of probe depended on the clinical situation. Eighty-eight respondents (62%) indicated that a rest was imposed during exercise testing if SpO2 dropped below a certain threshold but the threshold varied widely. Of the 88 respondents who answered this section, the cut-off threshold to impose a rest during exercise testing was reported as SpO2 between 79% and 84% by 21 respondents (24%), SpO2 of 85% by 39 respondents (44%), and SpO2 between 86 to 92% by 28 respondents (32%). The respondents were not asked to justify the cut-off thresholds. In the univariate regression model, the odds of imposing a rest during 6MWT when SpO2 ≥85% was higher in responders who had less experience in pulmonary rehabilitation (less than 5 years of experience) (Odds Ratio (OR) 3.5, 95% CI 1.2, 10.6).
The number of programs using objective measurements during exercise testing.
| Measurements | |||||
|---|---|---|---|---|---|
| SpO2, n (%) | Heart rate, n (%) | Blood Pressure, n (%) | Dyspnea, n (%) | RPE, n (%) | |
| Before exercise test | 140 (99) | 140 (99) | 124 (87) | 131 (92) | 46 (32) |
| During exercise test | 130 (92) | 125 (88) | 6 (4) | 83 (58) | 23 (16) |
| Immediately after exercise test | 138 (97) | 135 (95) | 42 (30) | 137 (96) | 69 (49) |
SpO2, oxygen saturation; RPE, rate of perceived exertion; n, number of programs.
Of the 142 respondents, 82% (n=117) indicated that supplemental oxygen was available during exercise testing and 84% (n=119) indicated that supplemental oxygen was available during training. In the univariate regression model, the odds of oxygen availability during exercise testing was lower in small programs (less than 50 participants per year) compared to larger programs (≥50 participants per year) (OR 0.2, 95% CI 0.1, 0.6) and the odds of oxygen being available during exercise training was lower in small programs (less than 50 participants per year) (OR 0.2, 95% CI 0.1, 0.5) and in programs conducted by clinicians with less experience in pulmonary rehabilitation (less than 5 years of experience) (OR 0.3, 95% CI 0.3, 0.8).
For those who indicated that supplemental oxygen was available during training, 114 (96%) respondents reported that a portable cylinder was used as the source of oxygen and 86 (72%) respondents indicated that 2L/min of oxygen flow was used during training. In addition, 58 (49%) respondents indicated that supplemental oxygen would be used only during the exercises where a patient experienced exercise-induced desaturation compared to 44 (37%) respondents who indicated that supplemental oxygen would be used during all exercises in the training session. For the respondents who indicated no supplemental oxygen availability, five (4%) reported that supplemental oxygen was not available for use during exercise testing, three (2%) reported that supplemental oxygen was not available for use during exercise training, and 20 (14%) reported that supplemental oxygen was not available for use during either exercise testing or training. For the 20 programs without any availability of supplemental oxygen, seven were hospital out-patient programs and 13 were community programs.
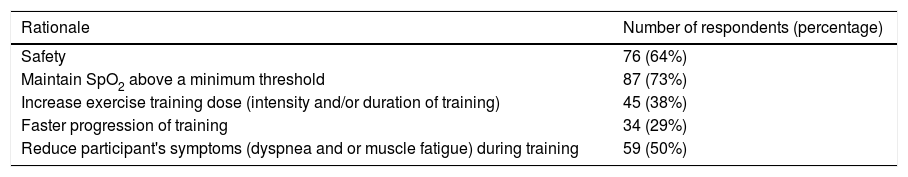
Rationale for supplemental oxygen prescription during exercise training in pulmonary rehabilitation programs for patients who were not on long-term oxygen therapyThe rationale for prescribing supplemental oxygen during exercise training varied between respondents and many selected more than one rationale (Table 3). Of the 87 respondents (73%) who prescribed supplemental oxygen to maintain SpO2 over a certain threshold during exercise training, 41 of these respondents (47%) indicated SpO2 between 80% and 87% as the threshold to provide supplemental oxygen, whereas 44 respondents (51%) reported SpO2 ≥88% as the threshold. Two of the 87 respondents (2%) reported that supplemental oxygen would be prescribed based on individual signs and symptoms but the SpO2 threshold was not specified.
Rationale for supplemental oxygen prescription during exercise training in pulmonary rehabilitation programs (n=119 programs).
| Rationale | Number of respondents (percentage) |
|---|---|
| Safety | 76 (64%) |
| Maintain SpO2 above a minimum threshold | 87 (73%) |
| Increase exercise training dose (intensity and/or duration of training) | 45 (38%) |
| Faster progression of training | 34 (29%) |
| Reduce participant's symptoms (dyspnea and or muscle fatigue) during training | 59 (50%) |
Note: respondents could select more than one rationale.
Of the 142 respondents, 45 (32%) indicated that a protocol was in place for supplemental oxygen prescription during exercise training. For this survey question, there was opportunity for respondents to provide details of the protocols. For the 34 (76%) respondents who provided details of protocols, the details included when supplemental oxygen would be administered during training and whom to consult in cases of exercise-induced oxygen desaturation before further intervention or provision of supplemental oxygen. Of the 45 programs where a protocol was in place for supplemental oxygen prescription, 20 respondents (44%) indicated that supplemental oxygen would be administered during exercise training if SpO2 fell below 88%. Seven of the 45 respondents (16%) reported that advice would be sought from a respiratory physician or nurse before training recommenced if SpO2 was less than 88% during exercise.
DiscussionThis is the first study to investigate the use of supplemental oxygen during exercise testing and training in Australian pulmonary rehabilitation programs. The main findings of the study indicate that SpO2 was commonly measured before, during, and after exercise testing and that supplemental oxygen was readily available in most pulmonary rehabilitation programs during exercise testing and training. The rationale for supplemental oxygen prescription during exercise training was wide-ranging with the most common reasons being to maintain SpO2 over a certain threshold, to ensure safety, and to reduce symptoms of dyspnea and fatigue during training. Only 32% of programs had a protocol in place for supplemental oxygen prescription during exercise training.
Oxygen saturation was commonly monitored during exercise testing, confirming that the majority of programs would be able to identify people who had exercise-induced oxygen desaturation during exercise testing. Monitoring oxygen saturation every minute during field walking tests is recommended.4 Based on the survey results, the majority (85%) of Australian pulmonary rehabilitation programs are meeting this recommendation.
Sixty-two percent of respondents indicated that a rest would be imposed if SpO2 fell below a certain threshold, however the threshold varied greatly between programs and the rationale for choosing such differing thresholds remains unknown. In addition, there were higher odds of inexperienced clinicians imposing a rest during the 6MWT when SpO2 ≥85%. Although no studies have examined appropriate SpO2 levels for test termination during field walking tests, a recent study indicated that desaturation to less than 80% during a 6MWT was not associated with adverse event in a large cohort of patients referred to pulmonary rehabilitation (n=549) including 384 participants with COPD.14 Such findings are consistent with other study that also found no adverse events associated with substantial exertional hypoxemia (SpO2 <85%) during a 6MWT in people with chronic lung diseases.15 This suggests that a clinician-imposed rest during a 6MWT may not be required when patients with COPD desaturate during the test. However, a clearer recommendation for test termination based on oxygen desaturation during exercise testing in people with COPD is necessary in any future guideline for field testing, especially for clinicians with less experience.
Although supplemental oxygen was readily available in most programs, 14% of programs did not have supplemental oxygen available during either exercise testing or training. This is higher than the 10% reported from the Canadian data12 and could be due to a higher percentage of programs being held in community centers in Australia compared to Canada (37% vs 8%). While the technical standards for field walking tests for people with chronic respiratory disease4 recommends that supplemental oxygen should be available in case of an emergency during a walk test, very few adverse events have been reported during a 6MWT in people with chronic lung disease,1,14 making the need for supplemental oxygen equivocal.
The rationale given by respondents for their prescription of supplemental oxygen during exercise training for people with COPD was wide-ranging. The differences in responses may relate to the different levels of workforce training for those providing pulmonary rehabilitation, which may have resulted in different degrees of understanding of the role supplemental oxygen may have during exercise training. Another reason for this variation may relate to conflicting recommendations for oxygen prescription making it difficult for those conducting pulmonary rehabilitation programs to formulate an oxygen protocol. A previous randomized controlled trial of cycle-based training in people with COPD without exercise-induced oxygen desaturation showed that supplemental oxygen allowed participants to achieve higher training intensities and obtain greater improvements in exercise capacity following training.16 In contrast, a few randomized controlled trials have demonstrated no difference in exercise capacity and symptoms when comparing the effect of supplemental oxygen versus air following training in people with COPD who experience exercise-induced oxygen desaturation.17–19 The quality of these trials was moderate due to lack of blinding and small sample size.17–19 A recent large, double blinded, multi-centered randomized controlled trial has confirmed that there was no added benefit from training with supplemental oxygen compared with medical air on exercise capacity and health-related quality of life for people with COPD who experience exercise-induced oxygen desaturation.20 Such findings demonstrate that exercise training for people with COPD who experience exercise-induced desaturation can be provided safely and with benefits in exercise capacity and health-related quality of life in venues where supplemental oxygen is not available.
A limitation of this study was that the response rate was only 57% despite three reminder emails being sent to the program representatives. The relatively low response rate could be due to the way the participants were recruited. All pulmonary rehabilitation programs were emailed by the Lung Foundation Australia based on their confidential list of programs, and surveys were submitted anonymously. Therefore, it was not possible to identify programs which had not responded to send follow-up emails directly. Despite this, the sample of programs that were included in this study represented programs of different sizes and settings across Australia, thereby providing a reasonable overview of current clinical practice with respect to supplemental oxygen use in pulmonary rehabilitation programs in this country.
ConclusionIn conclusion, SpO2 is commonly monitored during exercise testing and supplemental oxygen is available in most Australian pulmonary rehabilitation programs. However, protocols for the prescription of supplemental oxygen during exercise training have not been widely developed. As more robust evidence is emerging about the lack of value of supplemental oxygen during an exercise training program for people with COPD who experience exercise-induced oxygen desaturation but are not on long-term oxygen therapy, evidence-based protocols will be important.
Funding sourcesThis work was supported by National Health and Medical Research Council, Australia [grant number: APP1019989].
Conflicts of interestThe authors declare no conflicts of interest.
The authors wish to acknowledge Jennifer K. Peat (Australian Catholic University, Sydney, Australia) for statistical support.