Low back pain is the leading cause of years lived with disability in Brazil based upon Global Burden of Disease estimates. Since 1990, the number of years lived with disability has increased by 79.7%, and this number is expected to continue to rise due to population growth and ageing. Yet, similarly to other countries, little attention has been given to it in both the public and private health systems, arguably making it an overlooked epidemic in Brazil. There is evidence that Brazil has adopted unwarranted practices in the management of low back pain in a similar manner to what has been observed in high-income countries. To tackle the burden of low back pain in Brazil, we need highly coordinated efforts from government, the private sector, universities, health workers and civil society.
ObjectiveThis masterclass intends to provide an overview of the challenges faced by Brazil in relation to low back pain management and propose potential solutions that could potentially be implemented based on experiences reported in the literature.
The public health system in Brazil (the Unified Health System (SUS)), entitles every person living in Brazil to universal and free healthcare coverage across all levels of complexity (primary, secondary and tertiary care).1 Through the implementation of the Family Health Strategy programme, the proportion of the Brazilian population served by primary care facilities rose from 4% in 1998 to 62% (120 million people) in 2014.2 Nevertheless, despite the rapid scale-up of access to primary care, only about 35% of the Brazilian population report using primary care as their usual source of healthcare.2,3 People in Brazil can also access private healthcare either by paying healthcare providers at the time of service or by membership of a private health insurance plan. The most recent estimates indicate that 27.9% of the Brazilian population (approximately 56 million people), have private health insurance.4,5 In the Brazilian public health system, referral to medical specialists can only occur following a consultation in a primary care setting, usually with a general practitioner. Through this arrangement, the health provider acts as a gatekeeper, with the aims of promoting equity in access to healthcare, reducing unnecessary specialist referral and overutilisation of services, and providing best available care at a lower cost compared to other settings.6,7 In contrast, people willing to pay for a private consultation or many of those covered by private health insurance can choose to be seen first by a medical specialist.
Traditionally, Brazil's public health system has focused on tackling communicable diseases.1 However, the improvement of health status and increase in life expectancy has reduced the burden of these diseases over the last few decades.1,8 There has been a decrease in smoking rates (17%), and in the mortality attributed to ischaemic heart disease (26%) and chronic obstructive pulmonary disease (28%) in recent decades.8 In addition, Brazil excels in public health initiatives for immunisation and HIV/AIDS prevention and control.1 Despite many advances in health promotion, an increase in the burden of non-communicable diseases has been observed, which now represent the main source of disease burden in the country.1,8 Low back pain (LBP) is now the leading cause of years lived with disability in Brazil based upon Global Burden of Disease estimates.9 Since 1990, the number of years lived with disability has increased 79.7%,10 and this number is expected to continue to rise due to population growth and ageing. Yet, similarly to other countries, little attention has been given to it in both the public and private health systems,11–13 arguably making it an overlooked epidemic in Brazil.1,8
While only 28% of those with LBP experience severe or very severe levels of disability, the enormous worldwide disability burden associated with LBP is primarily a consequence of its high prevalence.13 Epidemiologic data on LBP in Brazil is scarce and derived mainly from studies with high risk of bias and imprecise estimates, according to a recent systematic review.14 Estimates for the one-year prevalence of LBP in adolescents range from 13.1% to 19.5%14 whereas prevalence estimates for persistent (≥12 weeks) LBP in adults range from 4.2% to 14.7%.14 Epidemiologic data on LBP can also be found in the National Health Survey,11 the most representative and comprehensive household-based survey conducted in the country (n=60,202 participants). The latest survey published in 2013 revealed a national point prevalence of severe or very severe chronic spinal pain of 16.4% (95% CI 15.2 to 17.2), representing approximately 33 million people. The prevalence of chronic spinal pain in Brazil varies according to education level, with illiterate people and those with incomplete elementary education displaying a higher prevalence (21.1%) compared to those with high school education incomplete (15.5%), higher education incomplete (10.9%) and higher education complete (7.0%).11 While the precise direct and indirect costs of LBP in Brazil is presently unknown, a 226% increase in the number of spinal surgeries and a 540% increase in the costs of spine surgery in the country has been observed from 1995 to 2014.15,16 Loss of productivity due to sick leave and early retirement are also a concern for the Brazilian economy and society. Spinal pain is the leading cause of compensation claims, representing 17.5% of all benefit claims in the last five years in Brazil.15 An important limitation of this survey is the use of a case definition of “chronic spinal pain”, a broader definition that might capture the prevalence of conditions other than LBP, such as chronic neck pain. The uncertainty around the time frame used to define what “chronic” pain means in this survey further limits the comparability of data from this survey with estimates from other countries.17
An overview of the recommendations for the management of low back pain from clinical practice guidelinesClinical practice guidelines currently recommend LBP to be managed in primary care, given that the vast majority of cases are not related to serious pathology.15,18–20 There is consensus among all recent guidelines to avoid routine imaging for LBP unless serious pathology is suspected.18–20 Routine spinal imaging for patients with non-serious LBP does not lead to better clinical outcomes, increases healthcare costs and may even be harmful to patients.21 Management should prioritise active treatments over passive interventions, with emphasis on non-pharmacologic interventions as first line of care.19 Advice to remain active and at work combined with education should be first line treatment for patients irrespective of whether they present with acute or more persistent low back pain.22 Some forms of passive therapies, such as spinal manipulative therapy and massage, may have a role in the treatment of both acute and persistent LBP, but are recommended mainly as adjunctive treatment options.15 Prescribed exercise therapy, regardless of the type, is considered first-line treatment for persistent LBP, but its use in patients with acute LBP is now recommended only for selected patients.15,18,19 Cognitive behavioural therapy, which relies on principles such as goal setting, activity pacing, graded activity, problem-solving and homework is endorsed by guidelines for the treatment of persistent LBP.18,19
The management of low back pain in Brazil is suboptimalThere is evidence that Brazil has adopted unwarranted practices in the management of LBP in a similar manner to what has been observed in high-income countries.15 Contrary to the recommendation of international guidelines to manage LBP in primary care,12,15 the 2011 Brazilian National Health Survey found that 36.5% of the survey participants had visited an emergency department, and 16.7% had been admitted to the hospital, in the past 6 months due to LBP.23 Musculoskeletal conditions were the most common reason for emergency department presentations, and LBP was the most prevalent of all musculoskeletal conditions.24 92% of Brazilian rheumatologists seeing patients with an uncomplicated episode of acute LBP would refer patients for a radiograph, 80% would prescribe rest, and 100% would prescribe at least one medication.25 A recent study also found that only a small percentage of Brazilian physical therapists fully adhered to the guidelines for the management of acute LBP with radiculopathy (5%) or acute LBP alone (11–14.5%).26
In addition, the Brazilian clinical practice guideline for the management of persistent LBP published in 2013 includes outdated recommendations.27 That guideline endorses the prescription of paracetamol and opioids, as well as treatments that have proven to be ineffective for treating LBP, such as ultrasound, short-wave diathermy and TENS. On the other hand, therapies that have been proven to be beneficial (e.g. cognitive behavioural therapy), have been omitted from the guideline.27 Even more outdated recommendations have been found on the official Brazilian Government website, which endorses absolute bed rest for acute LBP (http://www.brasil.gov.br/saude/2015/01/tire-suas-duvidas-sobre-a-lombalgia).28
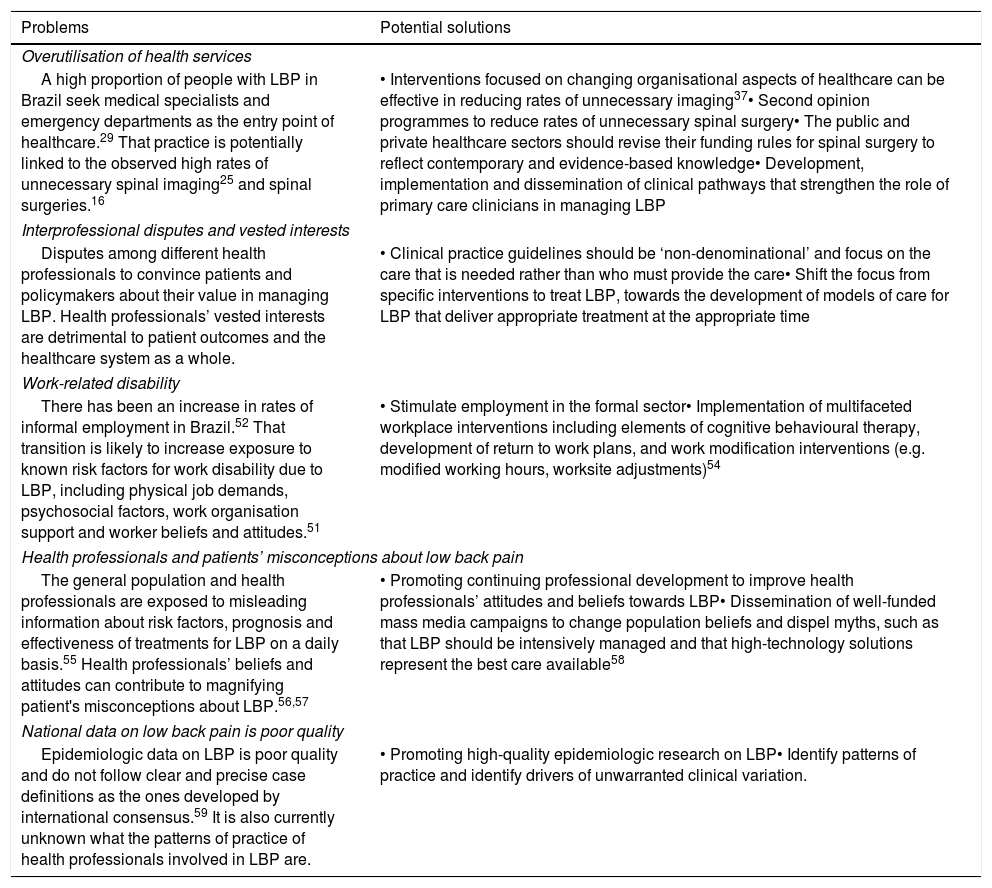
What steps are required to reduce the burden of low back pain in Brazil?To tackle the burden of LBP in Brazil, we need highly coordinated efforts from government, the private sector, universities, health workers and civil society.1,15 One important consideration is that little LBP research has been performed in Brazil, which constitutes a barrier to the development of public health interventions tailored to the population's needs. A solution to overcome that is to adapt interventions that have proven effective in other countries. Those solutions have been recently highlighted in The Lancet series on low back pain.12,13,15 Hereafter, we present a list of problems faced by Brazil in relation to LBP management, and solutions that could potentially be implemented based on experiences reported in the literature. A summary is presented in Table 1.
Problems faced by Brazil in relation to LBP, and potential solutions to tackle each of those problems.
| Problems | Potential solutions |
|---|---|
| Overutilisation of health services | |
| A high proportion of people with LBP in Brazil seek medical specialists and emergency departments as the entry point of healthcare.29 That practice is potentially linked to the observed high rates of unnecessary spinal imaging25 and spinal surgeries.16 | • Interventions focused on changing organisational aspects of healthcare can be effective in reducing rates of unnecessary imaging37• Second opinion programmes to reduce rates of unnecessary spinal surgery• The public and private healthcare sectors should revise their funding rules for spinal surgery to reflect contemporary and evidence-based knowledge• Development, implementation and dissemination of clinical pathways that strengthen the role of primary care clinicians in managing LBP |
| Interprofessional disputes and vested interests | |
| Disputes among different health professionals to convince patients and policymakers about their value in managing LBP. Health professionals’ vested interests are detrimental to patient outcomes and the healthcare system as a whole. | • Clinical practice guidelines should be ‘non-denominational’ and focus on the care that is needed rather than who must provide the care• Shift the focus from specific interventions to treat LBP, towards the development of models of care for LBP that deliver appropriate treatment at the appropriate time |
| Work-related disability | |
| There has been an increase in rates of informal employment in Brazil.52 That transition is likely to increase exposure to known risk factors for work disability due to LBP, including physical job demands, psychosocial factors, work organisation support and worker beliefs and attitudes.51 | • Stimulate employment in the formal sector• Implementation of multifaceted workplace interventions including elements of cognitive behavioural therapy, development of return to work plans, and work modification interventions (e.g. modified working hours, worksite adjustments)54 |
| Health professionals and patients’ misconceptions about low back pain | |
| The general population and health professionals are exposed to misleading information about risk factors, prognosis and effectiveness of treatments for LBP on a daily basis.55 Health professionals’ beliefs and attitudes can contribute to magnifying patient's misconceptions about LBP.56,57 | • Promoting continuing professional development to improve health professionals’ attitudes and beliefs towards LBP• Dissemination of well-funded mass media campaigns to change population beliefs and dispel myths, such as that LBP should be intensively managed and that high-technology solutions represent the best care available58 |
| National data on low back pain is poor quality | |
| Epidemiologic data on LBP is poor quality and do not follow clear and precise case definitions as the ones developed by international consensus.59 It is also currently unknown what the patterns of practice of health professionals involved in LBP are. | • Promoting high-quality epidemiologic research on LBP• Identify patterns of practice and identify drivers of unwarranted clinical variation. |
There is evidence that Brazil, as like many other high-income countries, faces a significant challenge with overuse of medical services for LBP. High rates of consultation with medical specialists,29 imaging,25 and unnecessary surgeries16 are examples of such unwarranted practices. A high proportion of people with LBP seek medical specialists and emergency services rather than from general practitioners. A recent study showed that about 60% of Brazilian patients with chronic pain would seek orthopaedic surgeons (25%), pain specialists (14%), rheumatologists (12%) and neurologists (10%) as the entry point of healthcare.29 In contrast, only 8% of patients with chronic pain would first seek general practitioners.29 That phenomenon is particularly relevant in the private health sector and is potentially linked to the great number of unnecessary imaging and lumbar surgeries performed in Brazil.16
Lumbar surgeries considered unnecessary are those indicated as first line treatment for patients who might have benefited from non-invasive approaches. For people who had been correctly referred to surgery, the type of surgery performed is also an issue. For example, while clinical outcomes between decompression alone versus decompression with lumbar fusion in people with spinal stenosis are similar,30 fusion is associated with higher costs and increased hospitalization.30 Data from observational studies suggest that referring patients to multidisciplinary clinics31 and implementing second opinion programs32–34 can reduce rates of spinal surgery.35 Conditioning the recommendation for surgery to the opinion of a second, independent, physician has shown promising results as well. Data from the “Second Opinion Program”33,35 for spinal surgery in Brazil revealed that a second opinion reduced the number of lumbar surgeries by 50%. It also reduced costs with surgical implants when surgery was the recommended treatment. Furthermore, outcomes of patients who had been recommended surgery and underwent non-surgical treatment were similar at 12 months.33 Another potential solution is revising funding rules for procedures whose effectiveness is not supported by current evidence. Recently, the Australian Government revised its funding rules for several spinal surgery procedures. From November 1st 2018, Australian Medicare will no longer fund spinal fusion surgery for uncomplicated LBP.36
Effective approaches to tackle overuse of unwarranted spinal imaging have recently been highlighted.37 The development of a clinical decision support for hospital-based physicians requesting imaging and the use of targeted reminders to primary care physicians reduced imaging requests by 36.8% and 22.5%, respectively. A more recent study showed that restricting reimbursement for imaging requests for non-serious LBP reduced lumbar spine radiograph and CT scans in primary care by 28.7%.38 In contrast to these findings, interventions aiming at educating clinicians and disseminating guideline recommendations were not effective in reducing overuse of imaging. These findings suggest that efforts to reduce overuse of imaging should focus on changing organisational aspects.
The current scenario indicates that clinical pathways for LBP in Brazil must be rethought. The time has come to promote rational use of health services, as well as to improve quality and access to health care.15 Promoting a stepped care approach, by increasing the role of primary care in managing LBP, is likely to be beneficial for patients and the Brazilian health system. In Canada, the creation of the Saskatchewan Spine Pathway39 aimed primarily at strengthening primary health care management of LBP. In addition, it also provided tools to improve coordination of care across levels of healthcare (e.g. unified medical record). That is particularly relevant for Brazil, where referral and counter referral across levels of healthcare is often poorly implemented.40 In the UK, the STarT Back model of care, which proposes different management strategies in primary care according to the patient's prognosis, has shown benefits in reducing disability, promoting early return to work and cost savings compared to usual care.41,42 Nevertheless, an attempt to implement the STarT Back model of care in the U.S43 has failed to replicate the findings from the UK trial,41 and had no effect on patient outcomes or healthcare utilisation. In Brazil, the STarT Back tool had poor prognostic ability when used in emergency departments44 and physical therapy clinics.45 Nevertheless, these studies found that stratifying patients after 6 weeks from baseline improved the prediction of clinical outcomes. The implications of these findings should inform future implementation studies.
Payment models are an important barrier preventing people with LBP to have access to appropriate care.15 Models of payment based on the quantity of services rather than the positive effect these services might have on patient outcomes are common in Brazil. Private health insurers in Brazil often pay for expensive and ineffective procedures (e.g. fusion for persistent non-specific LBP), but limit access to effective and cost-effective treatments (e.g. supervised exercise therapy46 and cognitive behavioural therapy47).
Problem 2: Interprofessional disputes and vested interestsDifferent health professions have long invested in aggressive professional advocacy strategies to convince patients and policymakers about their value in managing LBP. Nevertheless, effect sizes of interventions for LBP are often similar regardless of who delivers treatment,48 and findings from randomized controlled trials testing interventions delivered by different professions in people with LBP have mostly revealed comparable if not identical results (e.g. spinal manipulative therapy performed either by physical therapists, chiropractors or osteopaths).49,50 Professional disputes do not serve patients well and ideally guidelines should be ‘non-denominational’ but focus on the care that is needed rather than who must provide the care.12 LBP research must also shift its focus from specific interventions to treat LBP, towards the development of models of care for LBP that deliver the appropriate advice and/or care at the appropriate time. As well as re-evaluating the current models of care in both the public and private health system, this may also include consideration of strategies that promote healthy lifestyles and tackle social inequalities that contribute to the burden of LBP in Brazil.12
Problem 3: Work-related disabilityWork is an important determinant of health; unemployed people report poorer health and higher risk of early mortality.51 A number of risk factors for work disability due to LBP have been highlighted, including physical job demands, psychosocial factors, work organisation support and worker beliefs and attitudes.51 There has been an increase in rates of informal employment in Brazil,52 specially in people with lower socioeconomic status. Estimates from 2018 show that currently 10.7 million people in Brazil are working in the informal sector.52 That represents increased weekly working hours above of that regulated by the Consolidation of Labour Laws, absence of social security protection and poor employment conditions and increased work disability.53 Stimulating the employment in the formal sector is a necessary measure not only to benefit Brazil's economy but to improve the population's health.
Evidence to support some workplace interventions to reduce time lost off work, improve work functioning and costs have been recently summarized by a systematic review.54 For musculoskeletal conditions, there is evidence to recommend multi-component interventions that include at least two of the following components: health service-focused (e.g. cognitive behavioural therapy); service coordination (e.g. development of return to work plans and case management); and work modification interventions (e.g. modified working hours, worksite adjustments).54
Problem 4: Health professionals and patients’ misconceptions about low back painMisconceptions about LBP are a worldwide problem, and are common in Brazil as well. People are exposed to misleading information about risk factors, prognosis and effectiveness of treatments for LBP on a daily basis from advertisements and media. People with LBP usually have negative perceptions about the prognosis of pain and perceive their lumbar spine as vulnerable, a belief that triggers avoidance behaviours as a means to protect the spine.55 This in turn can further contribute to the cycle of increasing disability. Misconceptions are not exclusive to patients; they are often perpetuated by health care professionals who advise patients to rest, avoid movement and stay off work for prolonged periods.56 For example, compared with Australian physical therapy students, Brazilian students more strongly agree that having persistent LBP justifies disability and activity.57 Even if health professionals were always proficient in addressing LBP misconceptions during clinical encounters, this is unlikely to be enough to influence societal beliefs.
It may also be important to address misconceptions before the onset of LBP. One alternative is to tackle misinformation with extensive involvement of the mass media. Brazil has been successful in promoting mass media campaigns on several sensitive topics like tobacco cessation, family planning, control and prevention of HIV/AIDS and oral rehydration for diarrhoea in the past.1 Well-funded mass media campaigns, following successful models implemented in other countries,58 have the potential to shift population beliefs and dispel myths such as that LBP should be intensively managed and that high-technology solutions represent the best care available.58
Problem 5: National data on low back pain is poor qualityThere is an urgent need for high-quality data on LBP in Brazil. For example, epidemiologic data should be based upon clear and precise case definitions such as the standardized ones developed by international consensus.59 Furthermore, it is currently unknown what the patterns of practice of health professionals involved in LBP care are. Understanding patterns of practice are necessary to identify and address drivers of unwarranted clinical variation (i.e. variation that can only be explained by differences in health system performance). These studies could form the basis of clinical care standards that would need to be implemented across the country to optimise care and outcomes for people with LBP.
Final remarksThere is an urgent need to address the increasing burden of LBP in Brazil. This will require a systems approach that tackles different facets of the problem as outlined in this paper. We have provided suggestions that will require engagement of all relevant stakeholders. It is therefore paramount to follow a systematic process of adaptation and dissemination that takes into account that Brazil is a vast country with limited availability of health-related resources, great cultural, socio-economic and political diversity.1 We also acknowledge the additional challenges relating to recent cuts in the science budget made by the Brazilian government.60 Brazil cannot stay out of this worldwide wake-up to reduce the burden of LBP, and increasing awareness about the growing nature of this problem will be fundamental to encourage new initiatives to improve care and health outcomes.
Source of supportCoordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES).
Conflicts of interestThe authors declare no conflicts of interest.