Sensorimotor control is commonly reported in neck pain research and rapidly gaining interest in clinical practice. Joint position error (conventional and torsion), postural balance, subjective visual vertical, head tilt response, The Fly®, smooth pursuit neck torsion and head steadiness are tests that have been reported to assess cervical sensorimotor control. However, it is unknown whether clinicians could use one test, or a test battery, to appropriately assess cervical sensorimotor control and improve efficiency. Our main research question is: Do seven cervical sensorimotor control tests measure unique or similar characteristics of sensorimotor control in individuals with chronic idiopathic neck pain?
MethodsPrinciple components factor analysis. Data from seven cervical sensorimotor control tests of 50 participants with chronic idiopathic neck pain were included. Individual factors, potentially related to sensorimotor control, were determined by Eigen values >1.00 and inspection of a loading plot. Items with loadings ≥0.40 were considered satisfactory for inclusion in a factor.
ResultsAll cervical sensorimotor control tests were found to measure unique skills. Four factors were isolated with two, postural balance and head steadiness, accounting for most of the variance across tests. The remaining two factors, continuous movement accuracy and perceived verticality, contributed less to the observed variance.
ConclusionPostural balance and head steadiness were the major underlying factors explaining cervical sensorimotor control in the current sample. However, our results imply that all seven tests are independent and measure different skills. It is not possible to recommend a test battery for clinical practice, as all tests measure unique skills which appear to be independent of each other.
Sensorimotor control (SMC) has been defined as the afferent and efferent information streams, as well as the central processing of these two, contributing to joint stability.1 Cervical sensorimotor control (CSMC), which comprises of head and neck movement control, eye movement control, and postural stability, is commonly considered important in neck pain research.2
Specifically, in individuals with idiopathic neck pain, it has been suggested that CSMC may be affected.3–5 To date, seven CSMC tests have been suggested useful in the assessment of individuals with idiopathic neck pain6: the joint position error (JPE),7 postural balance,7,8 subjective visual vertical,9 head tilt response,10 smooth pursuit neck torsion,11,12 head steadiness,13 and The Fly® test.14
The most commonly used test is the JPE test, which has been reported in a large number of studies and included in several reviews and meta-analyses.6,15,16 Despite its widespread use, the clinical significance of the JPE test remains unclear due to the lack of a gold standard for comparison. This also applies to the other suggested tests that have similarly not been validated, as the clinical meaningfulness of these tests is based on minimal research, conducted in varying populations.12,17–29
Despite the minimal understanding of their meaningfulness, the clinical use of CSMC tests in individuals with neck pain is rapidly gaining interest.30 However, the availability of multiple tests purportedly assessing CSMC may introduce a challenge for clinicians in trying to select an appropriate test. Furthermore, clinicians may believe they have a valid measurement of SMC by just using one test, or conversely believe they might need to use all available tests to properly assess SMC, as it is currently unclear how many and which tests provide a clinically meaningful understanding of SMC. This lack in understanding may possibly lead to invalid clinical assessments, and potentially unnecessary use of valuable resources.
SMC comprises multiple subsystems: proprioception and kinesthesis (both responsible for the sensation of head and neck orientation relative to the body), the visuomotor system (the processing of visual information for the purpose of movement) and the vestibular system (located in the inner ear, predominantly responsible for spatial orientation of the head and neck, and postural balance).1 It might be expected that different tests would measure the performance of one or more of these subsystems. However, available evidence does not allow for an easy comparison of reported SMC outcomes in order to determine whether a particular subsystem is being assessed by each of these tests.31 Individual studies report different outcomes in different neck pain populations21,28,32 and source populations.22,24,27
If groups of tests can be identified that address the different subsystems of CSMC,4 a test battery could potentially be developed for clinical practice. This may lead to a reduction in the amount of time and resources needed to assess CSMC in clinical practice.
Presently, based solely on face validity, it is proposed that different tests measure different subsystems of CSMC.1,33 The JPE and the head steadiness tests have been suggested to assess primarily cervical proprioceptive or kinaesthetic afferent input.7,13 The postural balance test is proposed to evaluate the vestibular and visual systems, but is thought to also incorporate cervical proprioceptive information.24 Both the subjective visual vertical test and the head tilt response test assess the visual perception of verticality linked to a motor output, potentially reflecting the visuomotor system.10,34 The Fly® test combines a visual input with a continuous movement control exercise, and is proposed to address the visuomotor system as well as proprioception/kinesthesis.35 Finally, the smooth pursuit neck torsion test is considered to assess oculomotor control.11,12
Even though similarities in the assessed subsystems are to be expected across these tests based on their face validity, to date, any overlap between different tests has not been investigated and it remains unclear whether tests can actually be grouped together to assess a particular characteristic of SMC.36 Tests are often used interchangeably as it is unclear which and how many tests are needed to get a clinically meaningful measurement. Until it is possible to validate cervical sensorimotor control tests using a gold standard, assessing whether tests measure the same or different subsystems of sensorimotor control is an important question in order to use time and resources efficiently. The present study aims to determine whether CSMC tests measure the same, or different, subsystems of SMC in individuals with chronic idiopathic neck pain. It is hypothesized that conditions of the same test, as well as different tests, should cluster together. This would identify clusters of tests that would assess different subsystems of CSMC. Subsequently, clustering of tests could be used clinically in determining what tests should be used in CSMC assessment.
MethodsDesignFor this factor analysis, that follows the STROBE guidelines,37 data were collected between July 2016 and June 2017. This study complies with the Declaration of Helsinki and was approved by the Human Research Ethics Committee of The University of Newcastle, Australia (H2016-0099). All participants included in this study provided written informed consent.
ParticipantsParticipants with chronic idiopathic neck pain were included, recruited from The University of Newcastle Callaghan campus, the Hunter Medical Research Institute Research Register, and physiotherapy practices in Newcastle, NSW, Australia. Local advertising and social media were also used to recruit participants. Adults with chronic idiopathic neck pain were eligible to participate if they rated their pain at least 4/10 on a numeric rating scale. Exclusion criteria were limited vision (after correction), current or past history of diabetes, current or past history of migraine headaches, history of neck trauma or surgery, and other neurological or musculoskeletal conditions that may be considered to affect SMC.
Sample sizeFor factor analyses, there is no definitive method for sample size calculation. A sample-to-variables ratio between 2:1 and 5:1 is most common for factor analyses according to a recent systematic review.38 With seven main outcome variables (the seven SMC tests), a sample size of 35 participants with idiopathic neck pain was considered sufficient.39 As this study was part of a larger study with follow-up measurements, a sample of 50 participants was recruited to allow for withdrawals.
ProcedureParticipant characteristics were recorded at the start of each session. Body mass index (BMI) was calculated from height and weight measures, using a stadiometer to the nearest cm (Surgical and Medical Supplies Pty. Ltd., Rose Park, SA, Australia) and a standard analogue scale to the nearest kg (model 762 1019009, seca gmbh & co., Hamburg, Germany) respectively. As subjective pain response varies with different recall periods in individuals with neck pain, the 100mm visual analogue scale (VAS), anchored by no pain on the left and worst pain imaginable on the right, was used to assess current pain, average pain over the last seven days, and average pain over the last four weeks.40 The neck disability index (NDI, scored 0–50) was used to assess perceived disability.41 Physical activity levels were assessed using the Godin-Shephard Leisure-Time Physical Activity Questionnaire.42 Cervical range of motion (ROM) was assessed with the cervical range of motion instrument (CROM, Performance Attainment Associates, Lindstrom, MN, U.S.) for rotation (left and right), flexion and extension.43 From three measurements for each direction, range of motion was recorded as the mean total range in the transverse (rotation) and sagittal (flexion/extension) plane.
Sensorimotor control testsSeven SMC tests, as identified by a recent systematic review,44 were included in this factor analysis: JPE, postural balance, subjective visual vertical, head tilt response, the Fly, smooth pursuit neck torsion, and head steadiness. Table 1 provides a detailed description of each of the tests.
Cervical sensorimotor control measures.
| Joint position error (JPE) |
| In the conventional JPE test, the participant was seated on a chair facing a target on the wall 90cm away. A standard laser pointer (Electus Distribution Pty. Ltd, Rydalmere, NSW, Australia) was placed on top of the head and the participant was blindfolded. While starting with the laser pointer exactly in the centre of the target, the participant was instructed to move the head away from the target. Upon returning to the centre, the difference between starting position and final position was assessed. This was repeated three times for right rotation, left rotation, flexion, and extension, and the mean error for each direction was calculated for analyses. The head was repositioned to the centre of the target after each attempt. To minimize sensory reference information, a foam cushion was placed under the feet.8For the JPE torsion test, a laser pointer (Electus Distribution Pty. Ltd, Rydalmere, NSW, Australia) was attached to the mid-sternum region using a strap around the chest. While the participant was seated in a neutral position, the laser pointer was aligned with the centre of the target on the wall 90cm away. While the examiner gently held the head stationary, the participant was instructed to rotate the trunk away from the target and return to the starting position. Similar to the conventional JPE, the difference between starting position and final position was measured. This was repeated three times for rotation to the right and to the left, and the mean value was used for each direction. For both tests, movements were performed through comfortable range of motion.8 |
| Postural balance |
| In the assessment of postural balance, a Kistler force platform (type 9260AA6, Kistler Instrumente AG, Switzerland) was used. While the participant was asked to take a comfortable stance on the platform, the centre of pressure was recorded for 30s. This was done with the eyes both open and closed in a neutral head position. This was then repeated with neck torsion to the left and to the right (both eyes open and eyes closed). In order to achieve the torsion stance, the examiner gently held the participant's head while they rotated their body 45 degrees, including their feet, to either the right or left. The reference position on the platform was marked with pieces of visible electrical tape. For the collection and analysis of postural sway data (total sway path in mm), MARS (S2P Ltd, Slovenia) software was used. |
| Subjective visual vertical |
| An Oculus Rift (SDK 2.0, Oculus VR, CA, U.S.) virtual reality device was used for the subjective visual vertical test. Custom made software as described by Treleaven and Takasaki9 was displayed in the virtual reality device. Two dots representing the end points of a 20 degree tilted imaginary line were presented within a square that was tilted 18 degrees. Both the tilted square and dots could be positioned either clockwise or anticlockwise, which was randomized by the software. The computer mouse could be used to rotate a button, allowing rotation of the dots by a minimum of 0.01 degree. The participant was instructed to reposition the dots so that the imaginary line was positioned vertically (i.e., dots directly over each other). The deviation from the true vertical was recorded as the average of the deviation of the two dots. This procedure was repeated 20 times and the mean deviation from these repetitions was used for analyses.34 |
| Head tilt response |
| For the head tilt response test, the Oculus Rift virtual reality device was used with custom software (Libra@Home, Israel) as described by Geisinger, Ferreira, and Suarez.10 In the virtual reality device, a tilted white line was presented. The line was tilted either clockwise or anticlockwise, and the participant was instructed to tilt the head laterally so that the line would be positioned vertically. The Oculus Rift's head tracking sensors recorded the head tilt angle, which was compared to the line that was presented in the virtual reality device.10 |
| The Fly® |
| The original Fly test software was used as introduced by Kristjansson et al., 14 together with an electromagnetic tracking device (Polhemus Liberty, FasTrak, Colchester, VT, U.S.) to record head movement. On a computer screen, a representation of the head position was displayed with a crosshair, as well as a moving target (the “Fly”). By moving the head and neck, the target could be followed and movement accuracy (distance between crosshair and target) was measured. This was repeated for three different movement patterns – easy, medium, and difficult – which differed in length, time, and complexity. For the duration of each movement pattern, the mean distance between crosshair and target was used for analyses. A fourth movement pattern was used to familiarize participants with the test. |
| Smooth pursuit neck torsion |
| The smooth pursuit neck torsion test was adapted from Tjell and Rosenhall11 and Treleaven, Jull, and LowChoy.12 Testing was performed with the participant, seated facing a wall 100cm away. Custom made equipment which consisted of a laser pointer attached to a motor was positioned behind the participant with the laser pointer just above the head. The laser pointer, which projected a red dot (the target) on the wall, followed a sinusoidal pattern from left to right with a visual angle of 40 degrees. The target moved with a consistent speed of 20 degrees per second and a frequency of 0.2Hz. The participant was asked to follow the moving target with their eyes, while keeping their head still. The target moved from left to right and back ten times, and eye movements were recorded using surface electrooculography. This was done with the body straight ahead, and also in a torsion position in which the body was rotated 45 degrees on the chair but the head kept stationary. Eye movement was recorded using Ag/AgCl surface electrodes (Cleartrace, ConMed, Utica, NY, U.S.) positioned bilaterally just lateral to the eyes, and with one ground electrode on the forehead. This method has been previously utilized to record the corneo-retinal potential for the horizontal assessment of binocular electrooculography.45 The electrooculography signal was filtered through a 70Hz low pass filter and the data were de-identified prior to analysis. Data were analyzed by graphing the average velocity of eye movement and identifying the proportion of saccades for the sixth to ninth sequence. The difference between neutral and the average of the left and right torsion positions was calculated and used as outcome measure. |
| Head steadiness |
| For head steadiness testing, an electromagnetic motion tracking device (Polhemus Liberty, FasTrak, Colchester, VT, U.S.) was used to record head movement. Two conditions were investigated; low load with the participant seated on a treatment table with the back/head support at a 60 degree angle, and high load, with the participant lying supine on a horizontal treatment table. The participant was asked to lift their head approximately 1cm off the table and hold it still for 40s. Head movement (i.e., head angular velocity), was recorded continuously during the tasks.13 Participants that were not able to hold the lifted position for a minimum of 10s were excluded from the analysis. Raw data from sensor recordings were used to calculate average displacement and velocity over 40s.13 |
For some tests multiple test conditions were utilized: JPE was tested conventionally and with torsion, postural balance was tested in four conditions with eyes open and eyes closed, and neutral and torsion stance, the Fly test used three movement patterns differing in difficulty, and the head steadiness test was performed in a low load and high load condition. In total, seven tests were included, consisting of a total of 14 test conditions. A custom script written in MATLAB (MATLAB R2015a, The MathWorks, Inc., Natick, MA, U.S.) was used to randomize the order of range of motion tests and SMC test conditions.
Data analysisAll cervical sensorimotor test variables were measured on an ordinal scale and assumptions for performing the principal components factor analysis were checked prior to analysis including linearity, multicollinearity, and homoscedasticity. The correlation between test results was examined using Spearman's rho to assess the strength of any association between test results. A principle components factor analysis was then conducted to identify any relationships between the results of individual SMC tests and to expose the number of underlying factors present in the data. The optimum number of factors present was determined by the number of Eigen values greater than 1.00 and visual interpretation of the factor structure using a loading plot. In order to further clarify the factors, a Promax oblique rotation was performed. An oblique rotation was selected as we postulated that the factors identified as skills of SMC in people with chronic idiopathic neck pain would not necessarily be independent of each other and may influence other factors present in this population. Item loadings on each factor were greater than or equal to 0.40 for inclusion in that factor. Elements within each identified factor were subsequently analyzed and each factor was characterized. All statistical analyses were performed using Stata 13 (StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP).
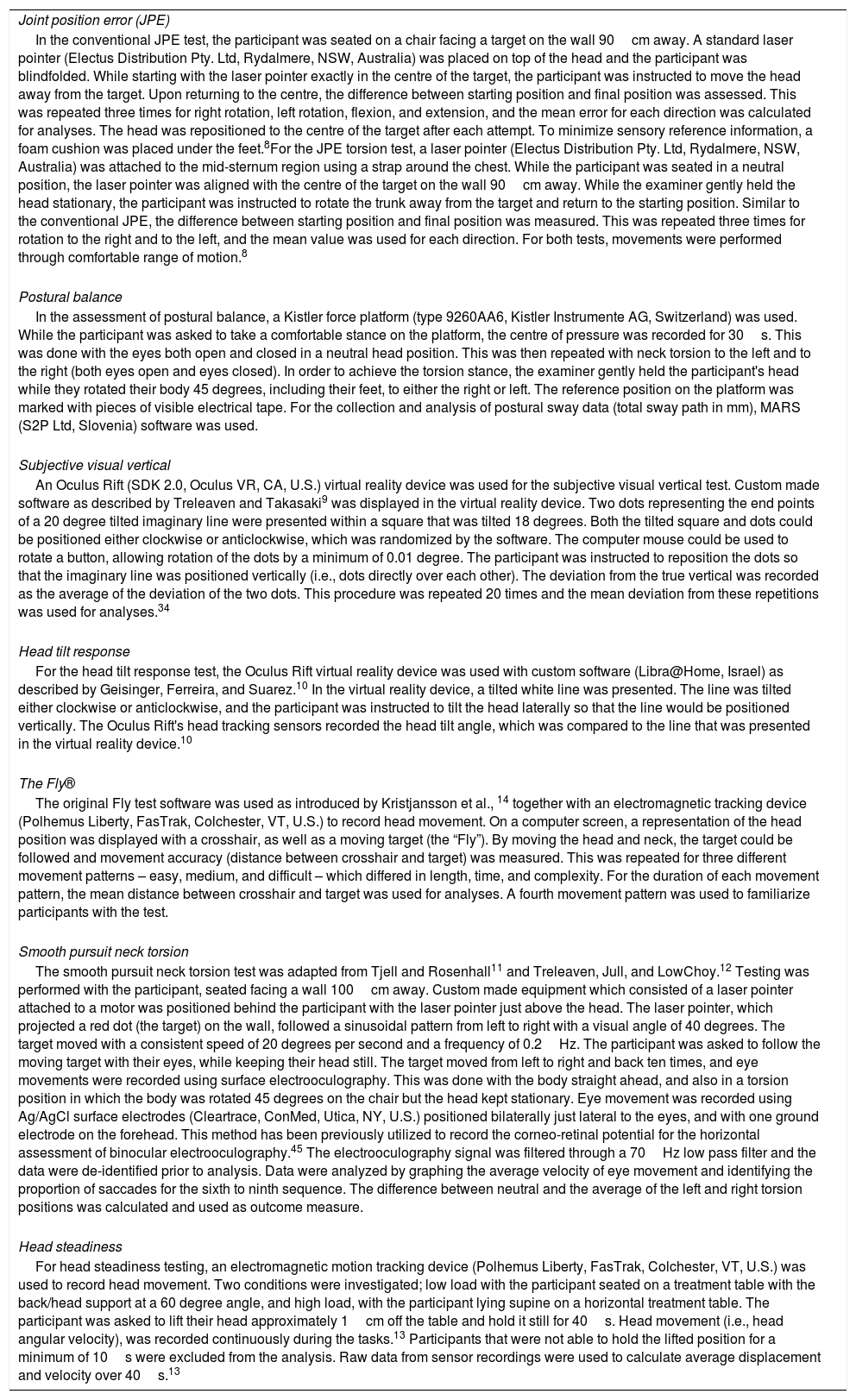
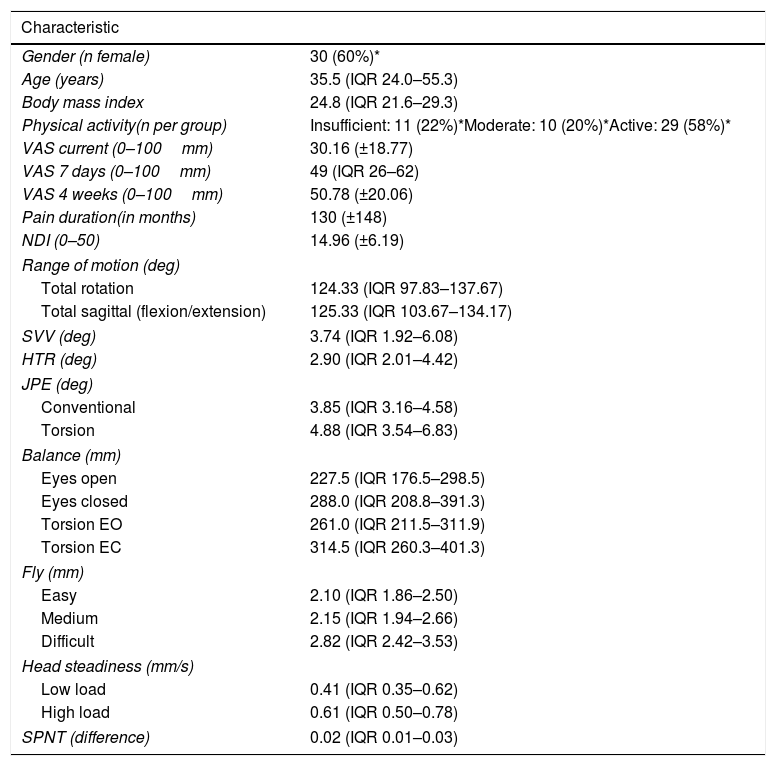
ResultsThe sample of individuals with chronic idiopathic neck pain consisted of 30 females and 20 males with a mean age of 41.61 (SD: 17.52) years. Participant demographics are presented in Table 2. Strong correlations (Spearman's rho higher than 0.60) were found between similar conditions of the same test, but not between different tests (Table 3).
Demographics of participants (n=50) with descriptive data for each test and test condition (mean, SD or median, IQR).
| Characteristic | |
|---|---|
| Gender (n female) | 30 (60%)* |
| Age (years) | 35.5 (IQR 24.0–55.3) |
| Body mass index | 24.8 (IQR 21.6–29.3) |
| Physical activity(n per group) | Insufficient: 11 (22%)*Moderate: 10 (20%)*Active: 29 (58%)* |
| VAS current (0–100mm) | 30.16 (±18.77) |
| VAS 7 days (0–100mm) | 49 (IQR 26–62) |
| VAS 4 weeks (0–100mm) | 50.78 (±20.06) |
| Pain duration(in months) | 130 (±148) |
| NDI (0–50) | 14.96 (±6.19) |
| Range of motion (deg) | |
| Total rotation | 124.33 (IQR 97.83–137.67) |
| Total sagittal (flexion/extension) | 125.33 (IQR 103.67–134.17) |
| SVV (deg) | 3.74 (IQR 1.92–6.08) |
| HTR (deg) | 2.90 (IQR 2.01–4.42) |
| JPE (deg) | |
| Conventional | 3.85 (IQR 3.16–4.58) |
| Torsion | 4.88 (IQR 3.54–6.83) |
| Balance (mm) | |
| Eyes open | 227.5 (IQR 176.5–298.5) |
| Eyes closed | 288.0 (IQR 208.8–391.3) |
| Torsion EO | 261.0 (IQR 211.5–311.9) |
| Torsion EC | 314.5 (IQR 260.3–401.3) |
| Fly (mm) | |
| Easy | 2.10 (IQR 1.86–2.50) |
| Medium | 2.15 (IQR 1.94–2.66) |
| Difficult | 2.82 (IQR 2.42–3.53) |
| Head steadiness (mm/s) | |
| Low load | 0.41 (IQR 0.35–0.62) |
| High load | 0.61 (IQR 0.50–0.78) |
| SPNT (difference) | 0.02 (IQR 0.01–0.03) |
Physical activity measured by The Godin-Shephard Leisure-Time Physical Activity Questionnaire. EC, eyes closed; EO, eyes open; HTR, head tilt response; JPE, joint position error; NDI, neck disability index; SPNT, smooth pursuit neck torsion; SVV, subjective visual vertical; VAS, visual analogue scale.
Correlations between cervical sensorimotor control tests and test conditions in individuals with chronic idiopathic neck pain.
| SVV | HTR | JPE conventional | JPE torsion | Balance EO | Balance EC | Balance torsion EO | Balance torsion EC | Fly Easy | Fly Medium | Fly Difficult | Head steadiness Low | Head steadiness High | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HTR | 0.370* | ||||||||||||
| JPE Conventional | 0.311 | 0.038 | |||||||||||
| JPE torsion | 0.160 | −0.087 | 0.372 | ||||||||||
| Balance EO | −0.250 | 0.181 | 0.010 | −0.102 | |||||||||
| Balance EC | −0.396* | 0.051 | −0.185 | −0.007 | 0.727* | ||||||||
| Balance torsion EO | −0.361* | 0.167 | −0.097 | −0.101 | 0.750* | 0.781* | |||||||
| Balance torsion EC | −0.439* | 0.064 | −0.156 | −0.092 | 0.715* | 0.805* | 0.903* | ||||||
| Fly Easy | 0.261 | 0.107 | 0.235 | 0.233 | −0.213 | −0.188 | −0.106 | −0.192 | |||||
| Fly Medium | 0.332* | 0.174 | 0.074 | 0.099 | −0.227 | −0.181 | 0.011 | −0.069 | 0.544* | ||||
| Fly Difficult | 0.366* | 0.175 | 0.083 | 0.295* | −0.106 | −0.136 | −0.097 | −0.135 | 0.624* | 0.665* | |||
| Head steadiness Low | −0.034 | −0.028 | −0.125 | 0.097 | 0.183 | 0.258 | 0.087 | 0.091 | 0.127 | −0.055 | 0.208 | ||
| Head steadiness High | −0.039 | −0.017 | 0.034 | 0.057 | 0.210 | 0.120 | 0.043 | −0.056 | 0.212 | −0.074 | 0.265 | 0.702* | |
| SPNT | 0.144 | −0.006 | 0.003 | −0.095 | 0.000 | −0.046 | 0.035 | −0.067 | −0.144 | −0.102 | −0.031 | 0.020 | 0.103 |
EC, eyes closed; EO, eyes open; HTR, head tilt response; JPE, joint position error; SPNT, smooth pursuit neck torsion; SVV, subjective visual vertical. Correlations provided are Spearman's rho, p-value between brackets, bold and * denotes statistically significant (α=0.05).
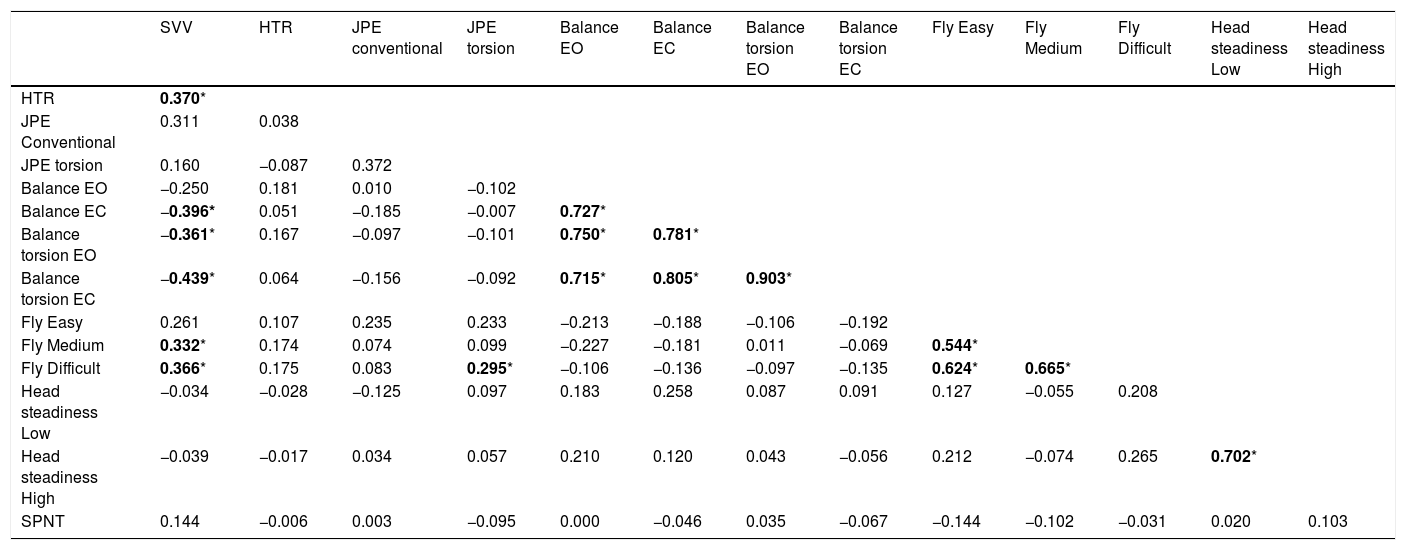
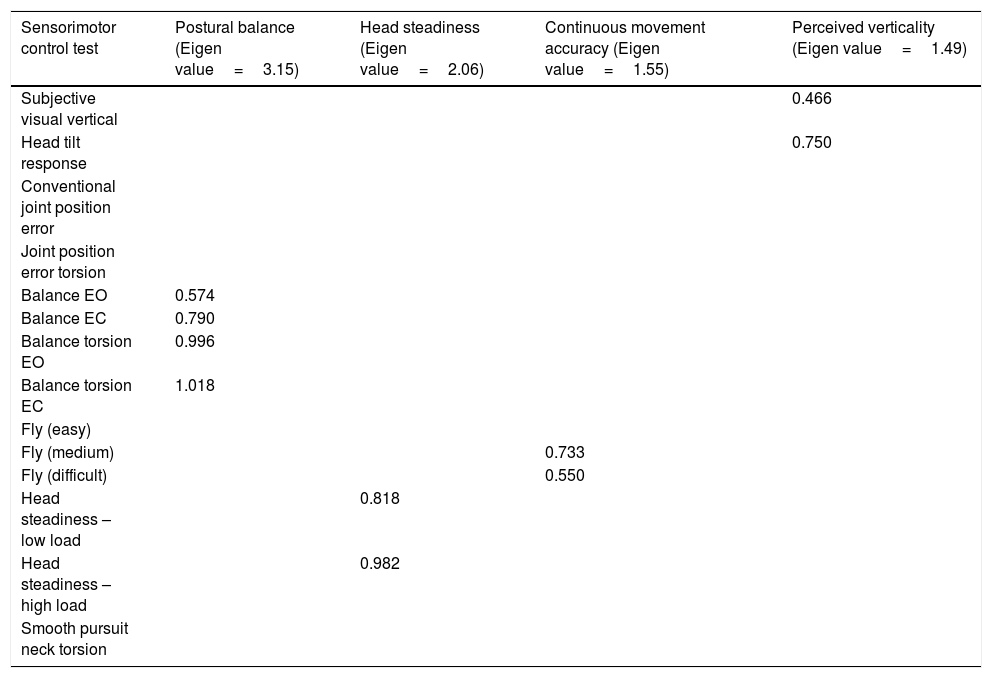
From the principle components factor analysis, four factors with Eigen values over 1.00 emerged. Table 4 presents these factors, as well as the constituent items that were included in factors 1–4.
Cervical sensorimotor control test item loadings for each of the four factors.
| Sensorimotor control test | Postural balance (Eigen value=3.15) | Head steadiness (Eigen value=2.06) | Continuous movement accuracy (Eigen value=1.55) | Perceived verticality (Eigen value=1.49) |
|---|---|---|---|---|
| Subjective visual vertical | 0.466 | |||
| Head tilt response | 0.750 | |||
| Conventional joint position error | ||||
| Joint position error torsion | ||||
| Balance EO | 0.574 | |||
| Balance EC | 0.790 | |||
| Balance torsion EO | 0.996 | |||
| Balance torsion EC | 1.018 | |||
| Fly (easy) | ||||
| Fly (medium) | 0.733 | |||
| Fly (difficult) | 0.550 | |||
| Head steadiness – low load | 0.818 | |||
| Head steadiness – high load | 0.982 | |||
| Smooth pursuit neck torsion |
Item loadings <0.40 are omitted from this table, as these did not account for a large proportion of the variance within each factor. EC, eyes closed; EO, eyes open.
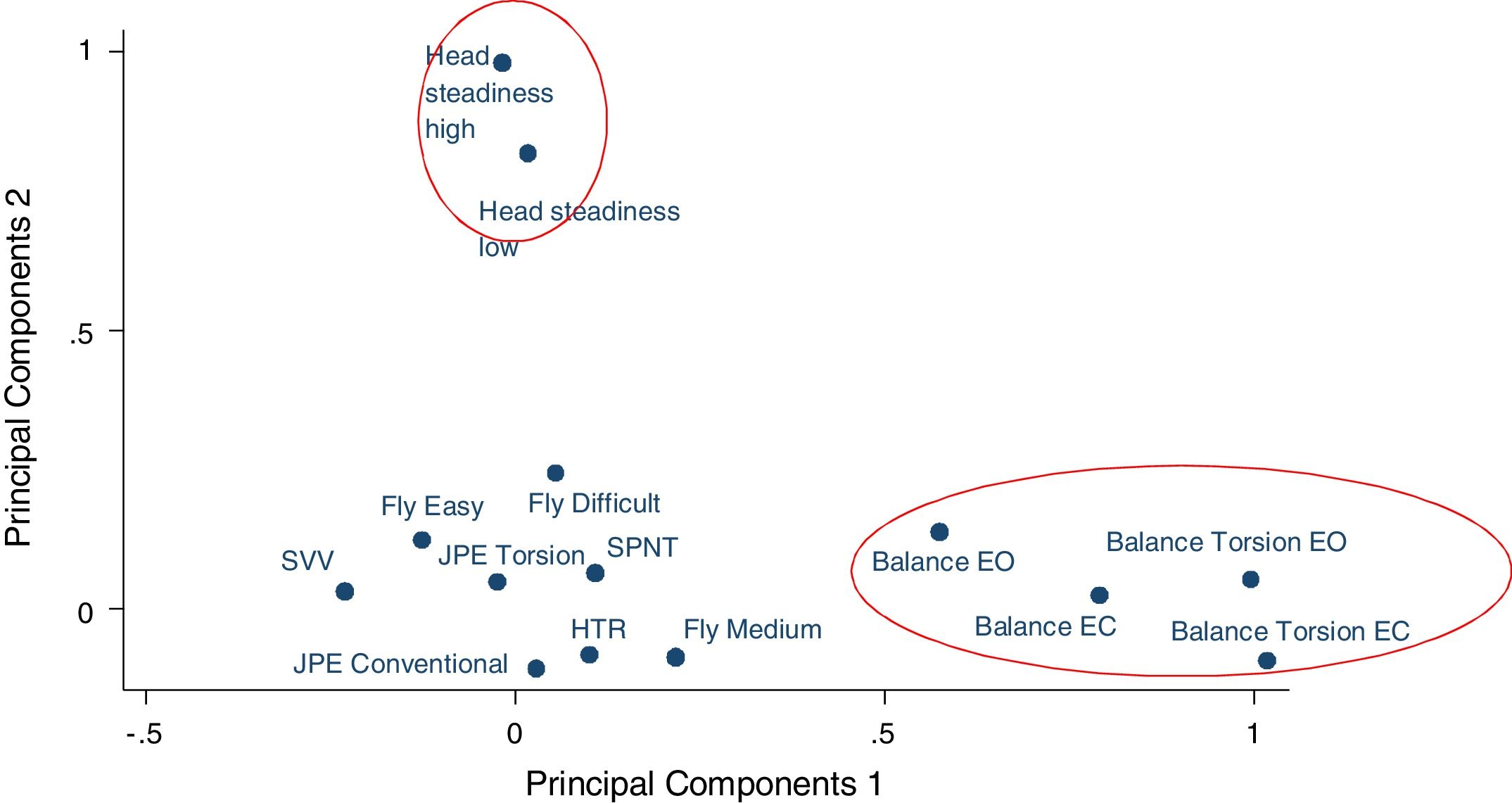
Factor one consisted of all four postural balance test conditions; eyes open, eyes closed, torsion eyes open, torsion eyes closed, and was thus labelled as ‘postural balance’. Factor two consisted of both low and high load conditions of the head steadiness test and was labelled ‘head steadiness’. Factor three consisted of the medium and difficult movement patterns of the Fly test and was labelled ‘continuous movement accuracy’. Factor four consisted of the subjective visual vertical and head tilt response tests and was labelled ‘perception of verticality’. Through observation of the factor loadings plot (Fig. 1) it was determined that factor one (postural balance) and factor two (head steadiness) formed clusters visually distinct from the other SMC tests.
Factor loading plot of all cervical sensorimotor control tests. Postural balance and head steadiness account for most of the variance across tests.
EC, eyes closed; EO, eyes open; HTR, head tilt response; JPE, joint position error; SPNT, smooth pursuit neck torsion; SVV, subjective visual vertical.
The present study used factor analysis to investigate whether existing CSMC tests measure the same, or different, subsystems of SMC. Two factors, postural balance and head steadiness, explained the majority of the variance in measured SMC. However, the results of this study demonstrate that most CSMC tests measure unique skills, and it is not possible to group them according to the different subsystems of SMC. For clinical practice, this means that different tests measure unique skills, thus a clinician cannot simply select one test. It is also not possible to recommend a specific battery of tests which would suffice in the assessment of CSMC, as all tests are unique.
Two factors, postural balance (factor one) and head steadiness (factor two), had relatively high Eigen values of 3.15 and 2.06 respectively, demonstrating that they are responsible for a large proportion of the variance across the tests. Factors three and four were less distinct clusters and accounted for less of the overall variance observed. From inspection of the factor loading plot, it is clear that postural balance and head steadiness groupings are distinct from the other tests, which implies that these two factors measure different characteristics of SMC, which do not appear to be captured by other SMC tests.
It has been suggested that postural balance is an important measure of SMC in individuals with neck pain.3,46 Cervical proprioceptors, the vestibular system and the visuomotor system are important in providing relevant afferent information for postural balance, and this may be affected in individuals with neck pain.33 Even though little consistency exists in the reported discriminating abilities of postural balance testing between individuals with idiopathic neck pain and healthy individuals,3,6,24,46 postural balance may be a unique characteristic of SMC, not captured by the other tests that are all performed seated. Alternatively, balance tests may rely on other systems outside of CSMC and thus may be testing a different construct to the other tests.
Factor two consisted of the two test conditions of the head steadiness test (i.e., low load and high load), and did not include other tests. The head steadiness test has been used in the sensorimotor assessment of individuals with neck pain in only one identified study that found differences between individuals with idiopathic neck pain and healthy controls.13 However, based on the test's characteristics, it might be argued that the head steadiness test is predominantly a muscle endurance test and not a true SMC test. Rather than being the result of differences in SMC skills, the discriminating capabilities of this test may illustrate a difference in neck muscle endurance and activation which has been reported in other literature.47,48 Other tests examined in this study do not require high levels of muscle strength, which is probably why the head steadiness test was found to be distinct from the other tests.
Factor three was labelled continuous movement accuracy and consisted of two conditions of the Fly test; the medium and difficult movement pattern. The Fly test is a continuous movement accuracy test suggested to involve sensory (visual) information processing and a motor output specific for the cervical spine (head movement).35,49 These results suggest the medium and difficult Fly test conditions measure unique skills that are not being assessed in the other tests. However, limited evidence14,35 is available for the Fly test and outcomes have only been examined cross-sectionally.
In the present factor analysis, not all Fly test conditions cluster together in one factor: the easy movement pattern failed to contribute to factor three. This was unexpected as the different test conditions appear to be very similar and the three conditions are together considered as one test. The only notable differences between the three conditions are the test duration and the number of changes in movement direction. The easy pattern takes 25s, the medium takes 40s and the difficult pattern takes 50s, and the number of direction changes increases with each level of difficulty. A potential reason for the easy condition not clustering with the two more demanding conditions (and also with none of the other tests) is its difficulty: it may simply be too easy to test continuous movement accuracy. However, previous studies did not find a difference in the discriminative ability of the three conditions of the Fly test in both whiplash and idiopathic neck pain populations.14,35
The subjective visual vertical test and the head tilt response test clustered in factor four. The two tests are both spatial orientation tests in which perceived verticality is assessed.9,10 The head tilt response test has been introduced as supplementary to the subjective visual vertical test10 as it introduces a motor output more specific to the cervical spine (i.e., head tilt, compared to arm/hand movement to control a computer mouse in the subjective visual vertical test). However, as the two tests cluster together in factor four, it can be argued that they both measure spatial orientation.
Based on the assumption that all tests measure SMC, stronger associations between different tests were expected. From the current findings, it can be concluded that each of these CSMC tests measure different skills that have been suggested relevant in SMC assessment. If multiple CSMC tests were found to cluster together and contribute to one factor, this would have supported the assumption that SMC is a single entity that might be measured using a single test or a small number of different tests. However, the present outcomes lead to the more likely explanation that each of these tests measure their own individual skill, which may potentially all be different characteristics of SMC.
A noteworthy observation is the fact that the most commonly used cervical SMC test, the JPE test, failed to contribute to any of the factors in this study. This suggests that this test must assess a unique skill, different to all of the other tests we investigated. Although the two test conditions of JPE (conventional and torsion) might have been expected to strongly correlate based on their face validity, Table 3 demonstrates they do not (rho=.37). Possibly, the subsystems of CSMC assessed by the two test conditions may be different. The conventional test condition appears to assess both the proprioceptive and vestibular subsystems, whereas the torsion condition, in which the head is kept still, the vestibular system may not contribute as much. The findings from the current study cannot determine whether the skill assessed by JPE relates to a specific characteristic of SMC, only that it must be unique to the other tests evaluated in the current study.
Limitations and strengthsRequired sample size in factor analysis remains contentious. Despite the lack of clear sample size requirements for factor analyses, a participant:variable ratio of 5:1 was considered sufficient.39 Based on available literature, however, it was assumed that all test conditions that are part of the same test, for example the three conditions of The Fly® test, could be considered as one factor. As outlined above, the results show that the three conditions of the Fly test do not cluster together in one factor, which results in the creation of an extra factor and thus a reduction in statistical power.
A strength of the current study is the use of factor analysis to explore commonalities between the available tests. Unlike related literature to date which solely reports the group-comparison findings of cross-sectional studies, this study has allowed us to address whether available CSMC tests measure similar skills. As this issue has not been addressed before, the present findings contribute to our understanding of available CSMC tests in both clinical and research settings.
A methodological strength of the current study is that test methods similar to the original test descriptions were used for all tests. By closely collaborating with other research groups, we were able to replicate test methods and even use the original test equipment and software for most of the tests. This results in the methods of the present study being highly comparable to earlier studies and strengthens its external validity. Furthermore, as most tests used computerized recordings, the likelihood that the examiner influenced the recording of test outcomes is negligible, which reduces assessor bias.
ConclusionsAll CSMC tests measure unique skills and cannot be grouped together under SMC subsystems such as proprioception, visuomotor control and the vestibular system. Only very similar tests, or test conditions that are part of the same test, were found to cluster together. This indicates that the available CSMC tests do not measure similar skills. Clinicians assessing CSMC therefore arguably have to perform each test, as each provides unique information. The clinical relevance of this information, in terms of the concept known as CSMC, remains unknown.
The researchers wish to acknowledge the support of the HMRI Research Volunteer Register for their assistance in participant recruitment.