To explore the personal and environmental contextual factors that influence use of affected arm for function among stroke survivors.
MethodsWe conducted a qualitative phenomenological study using an interpretivist paradigm among 23 stroke survivors in their late sub-acute and chronic stages and their relatives living in the rural regions of India using maximum variation sampling. Semi-structured interviews were conducted to identify personal and environmental contextual factors relevant to arm use. Their current level of arm use, motor and functional ability were evaluated using Motor Activity Log, AbilHand and Lawton Instrumental Activities of Daily Living scales and the scores were categorized in order to describe and compare the participant's characteristics before analyzing each interview. Differences among the contextual factors of participants with high and low levels of functional arm use and exercise using paretic limb were analyzed using qualitative content analysis.
ResultsStudy participants followed active exercises or passive interventions to improve their arm. Their immediate social environment influenced these decisions. Lack of awareness on how to self-engage or scale down their physical environment to match their abilities demoted active functional task performance. Ability to perceive small gains in arm function helped them sustain their efforts.
ConclusionContext influences arm use. Addressing contextual determinants influencing arm use such as facilitating understanding about the need for active functional task engagement; identifying and addressing factors moderating motivation to sustain functional task practice and enriching objects to match their movement abilities can increase arm use and promote upper limb recovery.
Stroke affects a large number of people. Every year 10,259,032 people are affected by stroke worldwide.1 Stroke survivors face a huge burden owing to the long term disability that ensues. The present years lived with disability after stroke in India alone is 12,083,416 years.2 Many stroke survivors remain partially or totally dependent on others.3 This burden not only compromises the quality of life but also pushes the rural households into medical poverty trap resulting in long term impoverishment.4
Stroke can cause cognitive, visual, speech and motor problems. Among these, motor impairment is a major source of functional dependence and results from deficits in mobility and dexterity.5,6 While internationally, 70–80% of survivors regain ability to walk; only 50% recover ability to move their affected arm.7 Notwithstanding this, only 5–20% exhibit complete functional recovery even in the chronic phases.8
Regaining a functioning arm augments the magnitude and quality of independence and consequently is perceived as essential by stroke survivors.9 Stroke rehabilitation guidelines recommend optimal quantities of task practice to promote motor ability of the affected arm.10 Nevertheless, improvement in motor ability alone does not translate to functional gains.11 In addition to performing exercises, engaging the affected arm in functional activities repeatedly for at least 2–3 months is vital to regain functional arm recovery.12,13 To facilitate this, the cause of discrepancy between motor ability and functional arm use should be elucidated.
Contemporary models of disability attribute activity levels to be influenced not solely by impairments but also by environmental and personal factors.14 Multiple contextual factors influence functional ability after stroke.15–20 However, the trajectory of upper limb recovery and factors that drive them are different from those that affect lower limb or stroke recovery where compensations can support.12,21 Moreover, contextual factors leading to disability and those influencing rehabilitation outcomes vary between cultures.22 Such divides also exist between rural and urban regions of a country.23 The rehabilitation needs of rural stroke survivors are high, yet accessibility to professional guidance is limited.24,25 In Southeast Asian culture, communication between the doctor and patient is predominantly one way with the patient being passive recipient.26 These factors compromise the guidance necessary to promote upper extremity recovery during the sub-acute and chronic phases after stroke.
Globally, there is limited data on degree of functional arm use and amount of active exercises performed by stroke survivors outside therapy sessions. Given the possibility of contextual influences on stroke care and paucity of studies exploring these factors on paretic upper extremity use, we are unaware of how best to promote recovery in survivors. Our knowledge on whether they perform exercises actively, do they try using their paretic arm for daily life activities, and how do they promote their upper extremity recovery are limited. Therefore, in this study, we aim to identify the arm utilization behaviours of persons with stroke, and principally, to understand how their personal and environmental contexts modify those behaviours. Understanding these contextual factors can provide us insights to better promote sustained arm use and augment recovery.
MethodsStudy designTo understand the influence of multiple contextual factors on idiosyncratic barriers and facilitators, we conducted a qualitative phenomenological inquiry using an interpretivist approach.27 We utilized phenomenology in order to identify factors that each survivor perceived as important in influencing their arm use and recovery and to gain a deeper understanding from their lived experiences on how these factors support or prevent them from using their arm.
ParticipantsTwenty three community dwelling adult stroke survivors with onset duration more than one month (late sub-acute: 3–6 months and chronic: >6 months) participated in the in-depth interview. People were excluded if they had co-morbidities that prevented using arm; unintelligible speech; cognitive deficit as identified by a score of <23/30 on MMSE; moderate to severe depression as identified by a score of >25/50 on major depression inventory or unwilling. Caregivers currently providing care to them and willing to participate were included. They provided complementary information to that provided by the stroke survivors.
We used maximum variation sampling to account for gender, urbanity, job status, social strata and ongoing rehabilitation status. Ethical clearance was obtained from Kasturba Hospital Institutional Ethics Committee, Manipal, Karnataka, India (IEC239/2015) and informed consent was obtained from each participants.
ProcedureParticipant examinationWe evaluated activity and participation levels in each participant using valid and reliable tools. Their functional ability was measured using AbilHand questionnaire and participation levels using Lawton Instrumental Activities of Daily Living scale.28,29
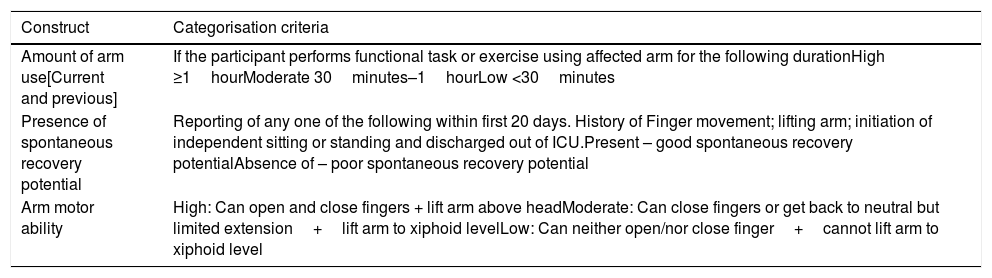
We measured the amount of arm use, using Motor Activity Log supplemented by their personal daily activity log. The scores were used to categorically identify participants with high and low functional arm use. Their current quantity of functional task practice was ascertained from the duration for which they attempted activities as shown in Table 1. This additional categorization as high, moderate and low amount of practice was used to identify those who were optimally exercising.30
Participant categorisation framework.
| Construct | Categorisation criteria |
|---|---|
| Amount of arm use[Current and previous] | If the participant performs functional task or exercise using affected arm for the following durationHigh ≥1hourModerate 30minutes–1hourLow <30minutes |
| Presence of spontaneous recovery potential | Reporting of any one of the following within first 20 days. History of Finger movement; lifting arm; initiation of independent sitting or standing and discharged out of ICU.Present – good spontaneous recovery potentialAbsence of – poor spontaneous recovery potential |
| Arm motor ability | High: Can open and close fingers + lift arm above headModerate: Can close fingers or get back to neutral but limited extension+lift arm to xiphoid levelLow: Can neither open/nor close finger+cannot lift arm to xiphoid level |
To compare amount of arm use between participants with different levels of motor ability and spontaneous recovery potential, we used a categorisation framework by operationally defining these constructs (Table 1).31 Their perceived magnitude recovery was documented using perceived recovery component of stroke impact scale. The functional scales and categorisation of the participants were utilized to clearly define each participant in terms of their ability, recovery potential and resultant amount of functional arm use.
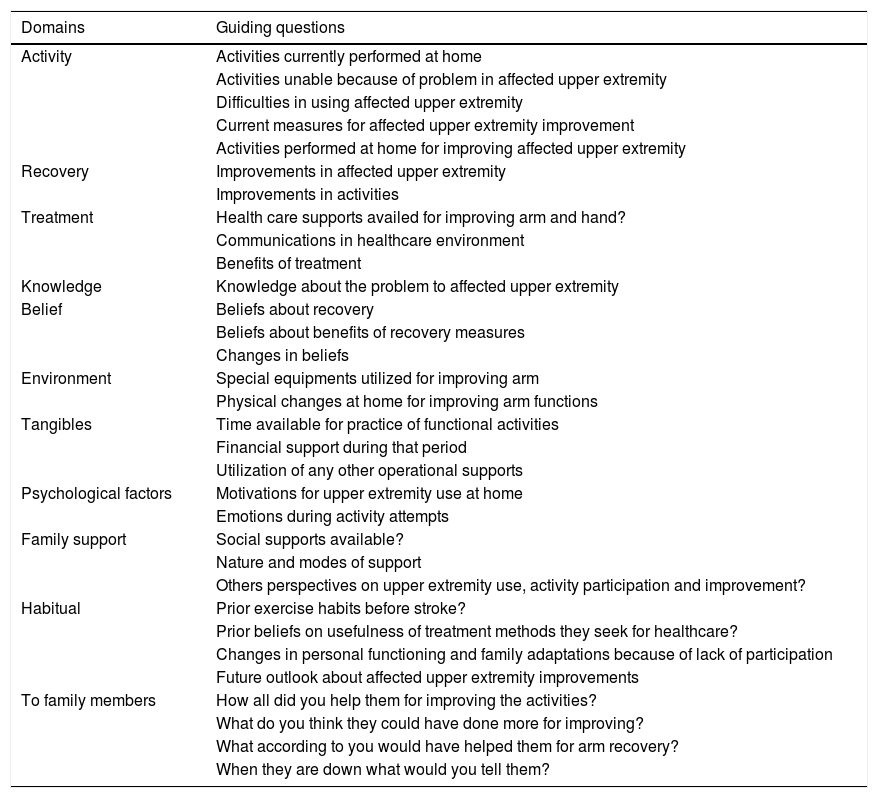
Semi standardized interviewWe conducted face to face semi-standardized interviews with the participants along with caregivers in their home using an interview guide addressing capacity, opportunity and motivation for arm use and perceived recovery (Table 2). List of factors influencing physical activity among general and stroke population were identified by reviewing existing literature by the team members. Two experienced stroke physical therapy clinicians and one psychologist not directly involved with the study validated the domains and sub domains for questioning. The caregivers were questioned about the nature of support such as physical, emotional, informational support that they provided. Their presence helped to complement and corroborate the information provided by the survivors.
Qualitative interview guide.
| Domains | Guiding questions |
|---|---|
| Activity | Activities currently performed at home |
| Activities unable because of problem in affected upper extremity | |
| Difficulties in using affected upper extremity | |
| Current measures for affected upper extremity improvement | |
| Activities performed at home for improving affected upper extremity | |
| Recovery | Improvements in affected upper extremity |
| Improvements in activities | |
| Treatment | Health care supports availed for improving arm and hand? |
| Communications in healthcare environment | |
| Benefits of treatment | |
| Knowledge | Knowledge about the problem to affected upper extremity |
| Belief | Beliefs about recovery |
| Beliefs about benefits of recovery measures | |
| Changes in beliefs | |
| Environment | Special equipments utilized for improving arm |
| Physical changes at home for improving arm functions | |
| Tangibles | Time available for practice of functional activities |
| Financial support during that period | |
| Utilization of any other operational supports | |
| Psychological factors | Motivations for upper extremity use at home |
| Emotions during activity attempts | |
| Family support | Social supports available? |
| Nature and modes of support | |
| Others perspectives on upper extremity use, activity participation and improvement? | |
| Habitual | Prior exercise habits before stroke? |
| Prior beliefs on usefulness of treatment methods they seek for healthcare? | |
| Changes in personal functioning and family adaptations because of lack of participation | |
| Future outlook about affected upper extremity improvements | |
| To family members | How all did you help them for improving the activities? |
| What do you think they could have done more for improving? | |
| What according to you would have helped them for arm recovery? | |
| When they are down what would you tell them? |
The semi-standardized interviews were conducted with participants, audio recorded and finally transcribed with the support of additional field notes. We refined the interview guide after analysing the initial interviews. The duration of interviews ranged from 30minutes to 2hours with an average of 45minutes/participant and was re-verified with participants.
Coding, categorization and analysisWe used qualitative content analysis software to perform analysis.32 We inductively coded physical capacity, environment and motivational contextual domains. Interview transcripts were read by the team members involved and parts of the transcript that were unclear were clarified with participants and they corrected informational discrepancies. Relevant inductive codes that were perceived contributory for arm use by proximity analysis formed subcategories. Prolonged engagement and member checks were used in the subsequent steps to understand and categorize the data. Next, the subcategories within each category were populated by content analysis and discriminated between those exhibiting positive versus negative arm use beliefs or behaviours. Eventually, the unique subcategories so identified were integral in framing final themes. Redundancy of major categories guided identification of data saturation. Data collection was stopped after interviewing 23 participants.
ReflexivityVR conducted all the interviews, coded and analyzed the transcripts. JMS, NM and JA verified the coding and interpreted the categories. All four framed the themes. VR, JMS and NM were physical therapists and JA was a clinical psychologist with all having more than 15 years of experience with stroke survivors. VR was research scholar and the other three were faculty with PhD degrees. Reflexivity was maintained against incorporating prior health behaviour theories during interpretation and theme formation.
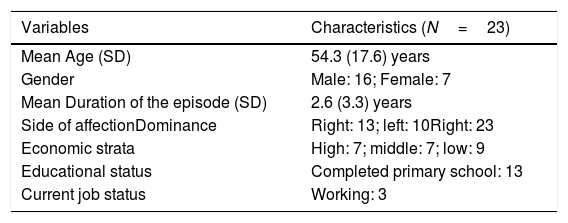
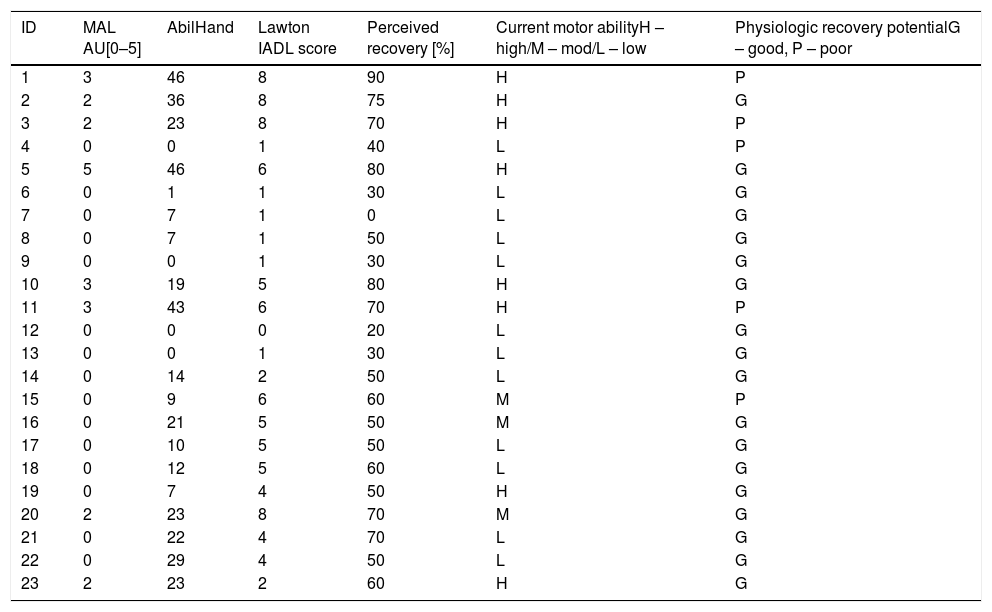
ResultThe characteristics of 23 participants are provided in Tables 3 and 4.
Demographic characters of participants.
| Variables | Characteristics (N=23) |
|---|---|
| Mean Age (SD) | 54.3 (17.6) years |
| Gender | Male: 16; Female: 7 |
| Mean Duration of the episode (SD) | 2.6 (3.3) years |
| Side of affectionDominance | Right: 13; left: 10Right: 23 |
| Economic strata | High: 7; middle: 7; low: 9 |
| Educational status | Completed primary school: 13 |
| Current job status | Working: 3 |
Participant physical ability and activity profiles.
| ID | MAL AU[0–5] | AbilHand | Lawton IADL score | Perceived recovery [%] | Current motor abilityH – high/M – mod/L – low | Physiologic recovery potentialG – good, P – poor |
|---|---|---|---|---|---|---|
| 1 | 3 | 46 | 8 | 90 | H | P |
| 2 | 2 | 36 | 8 | 75 | H | G |
| 3 | 2 | 23 | 8 | 70 | H | P |
| 4 | 0 | 0 | 1 | 40 | L | P |
| 5 | 5 | 46 | 6 | 80 | H | G |
| 6 | 0 | 1 | 1 | 30 | L | G |
| 7 | 0 | 7 | 1 | 0 | L | G |
| 8 | 0 | 7 | 1 | 50 | L | G |
| 9 | 0 | 0 | 1 | 30 | L | G |
| 10 | 3 | 19 | 5 | 80 | H | G |
| 11 | 3 | 43 | 6 | 70 | H | P |
| 12 | 0 | 0 | 0 | 20 | L | G |
| 13 | 0 | 0 | 1 | 30 | L | G |
| 14 | 0 | 14 | 2 | 50 | L | G |
| 15 | 0 | 9 | 6 | 60 | M | P |
| 16 | 0 | 21 | 5 | 50 | M | G |
| 17 | 0 | 10 | 5 | 50 | L | G |
| 18 | 0 | 12 | 5 | 60 | L | G |
| 19 | 0 | 7 | 4 | 50 | H | G |
| 20 | 2 | 23 | 8 | 70 | M | G |
| 21 | 0 | 22 | 4 | 70 | L | G |
| 22 | 0 | 29 | 4 | 50 | L | G |
| 23 | 2 | 23 | 2 | 60 | H | G |
IADL, Instrumental Activities of Daily Living.
We enquired the extent to which stroke survivors were using their affected arm for either performing daily activities or exercises. We found that ten of the twenty three participants performed exercise with the affected arm while rest of them did not perform any arm activity. Those who exercised predominantly performed passive exercises. One participant explained how she used to spend her time exercising her arm. [Participant 6] “I come and sit outside the house. People will be walking on the road. I watch them and keep exercising all through the day [demonstrates passive movements of the wrist and fingers]”. Only six of the twenty participants reported engaging the affected arm in functional activities. For example, [Participant 21] reported “At home I perform chores like dusting the furniture, sweeping floor and feeding animals in our farm. I try using my affected arm to feed my goat.”
We additionally inquired about the actions they undertook to promote arm recovery. Many participants underwent Ayurvedic treatment [a complementary and alternative medical treatment that includes massage with herbal oil and food restrictions]. A number of participants did not seek health care for improving their arm. Few visited rehabilitation centres to perform exercises. Others, as noted above performed passive or functional exercises, at home. Thus, our participants selected different means, some that could promote and others that could mitigate recovery. We identified four major contextual factors that influenced these diverse choices and subsequently, whether they engaged in requisite level of activities necessary to promote functional recovery.
Factors influencing uptake of exercisesAwareness and knowledgeMany participants were unaware that they have to exercise their arm to augment the natural recovery process. They believed that arm will automatically improve after stroke. [Participant 08], a chronic stroke survivor, expressed “I keep thinking when this arm and leg will start moving? When will it get alright? And when will I be able to perform my activities? I pray daily to God for improvement”. [Participant 12] another chronic survivor expressed, “We asked our doctor why am I not able to move my arm? He said it will be alright in due course. So we are waiting for improvement”. Some survivors, despite attaining negligible improvements were prospectively awaiting recovery even beyond two years without initiating any remedial measures. Certain others felt that the problem in arm was not due to the stroke. [Participant 6] described “When we came to hospital [acute hospitalization] problem in brain was treated. Now only the arm has to get alright”. A number of participants did not actively seek information on what measures to initiate for regaining arm function.
Very few participants [Participants 1, 2, 19, 20] could explain how to perform functional task practice to facilitate relearning of lost abilities. All the remaining participants were unclear on how to engage arm during activities or perform functional task practice. [Participant 7] informed that his doctor advised him to try doing activities using arm, yet did not describe how to perform. Those who practiced active movements felt practicing functional activities as superfluous and believed improvement of arm movements will directly translate into functional gains. Hence they did not engage their arm in performing functional activities. Nevertheless, none of them expressed how much they should practice in a day for achieving nominal gains, despite the fact that some of them were regular attendants to rehabilitation sessions.
Physical and social environmental influences on task practiceWe quizzed them on availability, accessibility and utilization of objects they interacted with while performing ADL's. One participant complained about his inability to lift a drinking glass. [Participant 19] “I cannot lift drinking glass. I feel afraid that it might fall when I lift.” However, another participant with similar motor ability elaborated how he managed to perform the activity. [Participant 1] explained; “I used to fill water in big glass and try to drink. It was difficult. Then I started using thinner light weight glasses with little water.” Another participant [3] expressed “I found it hard to lift a bucket filled with water, and so I fill little amount of water and carry more times. He also said, morning, I take three milk packets two in this hand and one in this hand”. Participants modified the manner in which they used objects to decrease task difficulty during functional task practice. Four participants, performing home exercises had created exercise facilities such as pulley systems, custom made arm exercise equipment and hand railing to support when walking as in a physical therapy department. [Participant 3] had a hand railing inside a narrow pathway in his home enriching the immediate physical environment to support practice.
Caregivers were immediate family members. They reported providing physical assistance for performing activities and guided exercise sessions. Although the survivors acknowledged their contribution, they highly appreciated the emotional support extended during their most difficult times. Family members and care providers motivated them to attempt activities using affected arm. [Participant 5] explained “My wife asked me to eat using only the affected hand and not with a spoon”. She says, “even if it falls, it is ok, eat with this hand only.” Participant 20, wanted to open bottles. She expressed “My physio has told that I have to open bottle and show before Diwali [festival date]. She said, “If you really like me you will have to do this.” “I also feel that I will have to do it because she is the only person who talks nicely with me. I took it as a challenge, and I did it”. In contrast, few participants reasoned lack of emotional support from family members as a major deterrent to active life participation. Additionally, some perceived that family members were not competent to advise them. [Participant 7] explained “My family members support me a lot but I don’t rely on them for improving arm. How do they know about this?”
Reliance on complementary and alternative treatmentsAfter being discharged from acute hospital care, most of our participants moved to centres offering complementary and alternative medicine [CAM] treatments. In the rural regions, these treatments were perceived as cheaper and to result in fewer side effects than rehabilitation treatments and hence the first choice not only for stroke but also for certain other diseases. In CAM therapy, medicinal oil and pastes are applied over the affected arm and patients are made to lie down for long hours. Advice to use arm actively were rare from CAM centres. Only three participants reported getting such an advice alongside the traditional treatments. Such advice was more common from practitioners of modern medicine. [Participant 1] described: “At CAM centre, doctor said it is good if you use the arm more. Even the other physician [neurologist who initially treated] also said, the more you use the arm it will be more beneficial”. Since participants underwent this treatment during sub-acute stage, a period of maximum natural recovery, whatever improvement ensued was attributed to these passive means and not to their active attempts.
Factors facilitating sustenance of effortsPerceived success invigorates sustenance of practiceSustaining active task practice is indispensable to materialize the initial gains of practice. We inquired why they continued to practice. [Participant 1] explained; “I noticed that I was able to lift my hand and do activities more than before. Then I understood that I am getting alright. Initially, when I tried lifting tumbler to drink water, it used to fall. As I kept on doing, it improved. Later, I was also able to eat with this hand.” Another participant [Participant 2] reported; “After practicing daily activities it started improving. As I used more it improved more.”
However, other participants did not perceive such gradual increments. [Participant 7]: “Initially I was trying but it was slightly difficult. I tried till a certain point. I could not see improvement in any activities. Even now I want to do all daily activities but I don’t have confidence”. [Participant 6] PH: “Initially we were exercising more; we used to do exercise two times a day, more in the morning. Now it has reduced, only once”. Perceived improvements matching their expected recovery potential gradually shaped their beliefs over a period of time guiding them to ultimately sustain or stop their efforts.
Participants’ personal and environmental contexts did guide their choice to pursue active or passive means to regain the affected arm functions. Together, these factors modulated the degree to which they actively engaged their arm and sustained their efforts.
DiscussionWe aimed to understand how contextual factors influence paretic arm use among stroke survivors residing in rural regions of India. Current upper extremity rehabilitation guidelines recommend high amount of functional task practice during sub-acute and chronic stages after stroke.10,33 Our participants demonstrated suboptimal quantities of non-task specific practices. Such low quantities were prevalent among those with low as well as high physical abilities. Yet, few participants with low physical abilities did attempt performing many functional activities, thus pointing towards the presence of factors other than physical ability as moderators of functional arm use.
In this study we found that personal and environmental factors promote or limit arm use of rural stroke survivors. We also identified that indirect social influences of competing health care systems could adversely affect proactive use of affected arm by stroke survivors. Although, a few previous studies have identified factors like informational needs, self-efficacy and environmental barriers to participation after stroke these pertain to promotion of general physical activity.34–36 In contrast, in this study we identified additional contextual factors unique to upper extremity activity promotion.
Early stage after stroke is crucial to recovery of upper extremity and hence lost time is irrevocable. During, this period, participants were unaware of the benefits of active exercises and many were either waiting for recovery or utilizing prevalent passive treatment modes such as CAM therapies.37 While, effectiveness of such therapies may be debatable, undertaking such treatments during spontaneous recovery period promoted staunch beliefs that passive means of engaging arm is sufficient to promote recovery. This belief prevents those who aspire to recover from engaging in optimal amounts of functional task practice. Hence, along with training participants to perform active exercises, educating about the importance of active arm use in the early stages is necessary to reinvigorate positive beliefs and increase arm use behaviours.
Not only initiation but sustained effort is necessary to realize success. Modifying objects used for daily life activities to fit their current ability can supplement achieving optimal amounts of self-driven task practice in their homes. As in acute stages, involving family members on how to provide behavioural support could reinforce individual efforts.38 In people with low motor abilities or lower self-efficacy, enriching the environment by modifying objects they use alongside raising awareness about the importance of active training in their family members might motivate the participants and help sustaining their pursuits long enough to recover, since difficulties extend for a long time after stroke.39
Dwindling recovery curves alongside perpetual failures in perceiving improvements devitalized many of our participant's sustenance efforts. Participants could dichotomize either their arm had functional ability or not, but they could not appreciate smaller improvements relatively easily. This prevents them from rapidly discerning the outcome of both their appropriate and inappropriate efforts and progress the exercises accordingly. Such information deficiencies dis-empower individuals from taking an active role in their rehabilitation.40 Promoting graded functional activity practice, educating about smaller improvements, vigilant long-term monitoring and time contingent feedback illustrative of potential functional improvements may continue to motivate them during those incapacitating periods.
Unlike prior studies, we could not identify specific psychological barriers to functional activity practice with paretic arm.41 A majority of our participants were not actively exercising for longer periods. A minority of those who were in the sub-acute stage, either showed general apathy due to lack of perceptible improvements or enthusiasm owing to their incremental success. The above context limited us from gleaning the psychological constructs. This might be an area for further study in those who have started engaging their arm in activities.
Regaining paretic arm for performing functional activity is an uphill task. To this end, achieving an optimal practice quantity is a necessary first step. Empowering participants to engage in active task practice using paretic arm is influenced by each person's unique personal contexts and their physical and psychosocial environment. Hence, future programmes to retrain paretic upper extremity and promote self-management should not only halt with educating or training stroke survivors and their family members but also guard their beliefs and behaviours against the enervating contextual influences to promote sustained functional arm use.
In our study, these factors biased their beliefs towards adopting passive means to recover and limited proactive utilization of arm in physical activities. Improving stroke survivors, understanding about the nature of exercise that would benefit them, changing their beliefs about their current suboptimal practices, enrichment of objects they handle with their paretic arm and keeping their motivation up for sustained periods may all go a long way in optimizing paretic arm engagement. Nevertheless, future programmes that focus on upper extremity functional activity promotion should comprehensively identify an individual's perceived and actual contextual barriers and address them to optimize recovery.
Conflicts of interestThe authors declare no conflicts of interest.
The authors wish to thank Mr. K. Hariohm and V. Prakash for their significant inputs in writing an earlier version of this manuscript.