Although lower limb muscle strength is associated with walking performance in people after stroke, even when there is good strength, walking speed may remain slower than normal, perhaps due to incoordination.
ObjectiveThe aim of this study was to examine the relationship between walking speed and lower limb coordination in people with good strength after stroke.
MethodsAn observational study was conducted with 30 people with stroke and 30 age-matched controls. Inclusion criteria for stroke were good lower limb strength (i.e., ≥Grade 4) and walking speed at >0.6m/s without aids in bare feet (with recruitment stratified so that walking speed was evenly represented across the range). Walking performance was measured as speed during the 10-m Walk Test and distance during the 6-min Walk Test. Coordination was measured using the Lower Extremity Motor Coordination Test and reported in taps/s.
ResultsStroke survivors walked at 1.00 (SD 0.26) m/s during the10-m Walk Test (64% of normal), walked 349 (SD 94) m during the 6-min Walk Test (68% of normal), and performed the Lower Extremity Motor Coordination Test at 1.20 (SD 0.34) taps/s with the affected side (64% of normal). Lower Extremity Motor Coordination Test scores for the affected side were statistically significantly correlated with walking performance in the 10-m Walk Test (r=0.42, p=0.02) and the 6-min Walk Test (r=0.50, p=0.01).
ConclusionCoordination was related to walking performance, suggesting that loss of coordination may contribute to slow walking in this group of stroke survivors with good strength.
Trial registration: ANZCTR12614000856617 (www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=366827).
The negative motor impairments of stroke include weakness and incoordination and these impairments lead to limitations in activities such as standing up, walking, reaching and manipulation.1 Several studies have investigated the contribution of weakness and incoordination along with other impairments to activity limitation after stroke. Muscle weakness has been shown to have a higher correlation with physical disability than any other motor impairment in upper limb activity,1–3 stair climbing,4 and walking.5–8 Therefore, strength is very important for regaining activity since it is a pre-requisite of movement. Furthermore, interventions focusing on addressing weakness after stroke are associated with improvement in strength, as well as improvement in activities such as walking.9,10
Nevertheless, once leg strength has reached a certain level, any additional strength does not appear to result in an increase in walking speed. The relationship beween leg strength and walking speed in older adults11 was found to be non-linear such that when leg strength is low, increases in strength result in increases in walking speed whereas when leg strength is high, there is little association beween strength and walking speed. Hence it is possible that where there is good strength, other impairments such as incoordination become important.
Incoordination after stroke has been less extensively researched than weakness, partially because coordination is confounded by weakness and most people after stroke present with weakness as well as incoordination. However, in a study where minimal strength was required to measure coordination, incoordination was found to make an independent contribution to upper limb activity.12 In contrast, the relationship between incoordination of the lower limb and long-term activity limitations in walking is not clear. Clinically, many stroke survivors who appear to have good strength of the lower limb muscles still walk slowly compared with their premorbid level. In this group, perhaps the slowness in walking speed is due to their inability to turn their muscles on at the right time during the gait cycle in order to coordinate both temporal and spatial parameters of movement, i.e., they have incoordination.
There are only three studies of the relationship between incoordination and walking after stroke. One study found that the duration of the stance phase was shorter on the affected side with increased co-activation of knee and ankle extensors in people with stroke compared with healthy controls, but there was no correlation between co-activation levels and walking speed.13 However, the other two studies found that reduced intralimb coordination of the lower limbs in community-dwelling people after stroke was associated with a slower walking speed.14,15
In summary, there is a significant association between lower limb muscle strength and walking performance in people after stroke especially when muscle strength remains low. When there is good lower limb strength yet walking speed remains slower than normal for that age group, the influence of other impairments (such as incoordination, spasticity, contracture, loss of sensation) may become more prominent. The aim of this study was to investigate the potential contribution of loss of coordination to walking disability after stroke. The specific research question was: “Is lower limb coordination related to walking speed in people who have good lower limb strength after stroke?”
MethodsDesignA quantitative observational study examining the relationship between walking speed and lower limb coordination after stroke was conducted. Measures were taken from stroke survivors and age-matched healthy controls over one session, 1–2h long. First, demographic information and physical measures to describe the sample were collected. Then, walking speed was measured, followed by coordination. Rests were taken in between measures to ensure that they were not confounded by fatigue. This study was approved by the Human Research Ethics Committee of the Sydney Local Health District, Sydney, NSW, Australia. This study was registered in a public registry (ANZCTR12614000856617). Informed consent was gained before data collection.
ParticipantsStroke survivors were recruited from individuals who were attending or who had attended a physiotherapy service at a tertiary metropolitan hospital in Australia. Age-matched healthy controls were also recruited from the community for comparison. Stroke survivors were eligible if they had a stroke at least 6 months previously; were between 18 and 85 years old; hip flexion and extension, knee flexion and extension and ankle dorsiflexion and plantarflexion strength on the affected side were all graded≥4/5 on Manual Muscle Testing16; were community ambulators (able to walk unaided≥0.6m/s); and were able to follow verbal instructions. Stratified sampling was used in order to represent a range of walking speeds. Speed on the 10-m Walk Test was divided into six categories (0.60–0.72m/s; 0.73–0.84m/s; 0.85–0.96m/s; 0.97–1.08m/s; 1.09–1.2m/s; and >1.2m/s) and five participants were recruited in each category. Healthy controls were eligible if they were between 18 and 85 years old; were able to walk independently unaided ≥1.2m/s; and had no weakness in the hip, knee or ankle muscles on manual muscle testing.
In order to describe the sample of stroke survivors, age, sex, type of stroke, side of hemiparesis, and time since stroke were collected. In addition, other motor impairments likely to affect walking such as spasticity, contracture and proprioceptive loss were collected. Spasticity of the ankle plantarflexors was measured using the Tardieu Scale and reported as a score from 0 to 4 where 0 represents no spasticity. Contracture was measured as the difference in magnitude of ankle dorsiflexion between the intact and the affected side and reported in degrees. Proprioception was measured using a lower limb matching task16 and reported as the difference between the intact and the affected side in degrees.
Measurement of walking and coordinationThe outcomes were walking performance and lower limb coordination. The measures of walking performance were the 10-m Walk Test17 (ICC2,1=0.94) and 6-min Walk Test17 (ICC2,1=0.99). The measure of lower limb coordination was the Lower Extremity Motor Coordination Test (LEMOCOT) (ICC2,1=0.95,18 ICC2,1=0.8419).
The 10-m Walk Test was conducted along a 14m straight walking track. Participants walked unaided in bare feet and were instructed to “walk as fast as you can but stay safe”. Familiarization trials were allowed to ensure participants understood the test before a single trial was undertaken where the time in seconds was recorded over the middle 10 metres. The time in seconds was converted to speed (m/s).
The 6-min Walk Test was conducted along a 26 or 32m walking track in bare feet. The instructions followed standard instructions according to Guidelines for the 6-min Walk Test20 and the distance walked was recorded and also converted to speed (m/s) in order to compare with walking performance during the 10-m Walk Test.
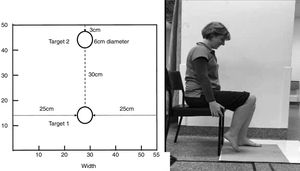
The Lower Extremity Motor Coordination Test (LEMOCOT)18,19 was conducted with the participant seated on a standard dining room height chair. Participants were instructed to touch and move between two targets 30cm apart with their big toe as accurately and as many times as they could in 20s (Fig. 1). Each participant was given familiarization trials with the unaffected side prior to testing to ensure that they understood the procedure of the test. The stroke group undertook a single trial of the affected side and the healthy controls undertook a single trial of each side which were then averaged. The number of accurate touches was recorded by the assessor and taps/s was calculated.
Data analysisCharacteristics of the participants are presented descriptively. Data were continuous, therefore independent t-tests were used to study between-group differences which are presented as mean differences (95% CI). Simple regression using Pearson product moment correlation analyses were used to determine the relationship between coordination and walking speed.
ResultsCharacteristics of participantsThirty-four community ambulating stroke survivors were invited to participate but four were excluded due to their walking speed being too slow. Therefore, 30 stroke survivors aged 65 years old (SD 15) and on average 25 months (SD 30) from the time of stroke participated (Table 1). They had little spasticity (mean 0.2/4.0, SD 0.8), contracture (1 deg, SD 6) or proprioceptive impairment (3 deg, SD 1). Thirty healthy controls who were aged 60 years old (SD 15) also participated.
Characteristics of participants.
| Characteristic | Stroke (n=30) | Healthy (n=30) |
|---|---|---|
| Age (yr), mean (SD) | 65 (15) | 60 (15) |
| Sex, n males (%) | 18 (60) | 8 (27) |
| Time since stroke (mth), mean (SD) | 25 (30) | n/a |
| Affected side, n right (%) | 10 (33) | n/a |
| Type of stroke, n ischaemic (%) | 28 (93) | n/a |
| Spasticity (Tardieu 0–4), mean (SD) | 0.2 (0.8) | n/a |
| Contracture (intact-affected, deg), mean (SD) | 1 (6) | n/a |
| Proprioception (intact-affected, deg), mean (SD) | 3 (1) | n/a |
Table 2 presents walking performance and coordination for both groups and the difference between groups. Walking in the 6-min Walk Test and 10-m Walk Test in the stroke group was 64–68% of the healthy control group. Similarly, the LEMOCOT score for the stroke group was 64% of the healthy control group.
Mean (SD, range) of outcomes by group and mean difference (95%CI) between groups and stroke group as a proportion of the healthy group.
| Outcome | Groups | Between groups | ||
|---|---|---|---|---|
| Stroke (n=30) | Healthy (n=30) | Difference stroke-healthy | Proportion stroke/healthy | |
| Walking (10-m Walk Test) | ||||
| Speed (m/s) | 1.00 (0.26, 0.61–1.63) | 1.57 (0.31, 1.22–2.35) | −0.57 (−0.42 to −0.72) | 0.64 |
| Walking (6-min Walk Test) | ||||
| Speed (m/s) | 0.97 (0.26, 0.44–1.49) | 1.43 (0.30, 1.01–2.07) | −0.46 (−0.31 to −0.61) | 0.68 |
| Distance (m) | 349 (94, 158–536) | 515 (108, 364–745) | −166 (−218 to −114) | 0.68 |
| Coordination | ||||
| LEMOCOT (taps/s) | 1.20 (0.34, 0.70–2.30) | 1.88 (0.36, 1.25–2.95) | −0.68 (−0.86 to −0.50) | 0.64 |
LEMOCOT, Lower Extremity Motor Coordination Test.
LEMOCOT scores were moderately correlated with walking speed in the 10-m Walk Test (r=0.42, p=0.02) (Table 3). LEMOCOT scores were also moderately correlated with walking distance in the 6-min Walk Test (r=0.50, p=0.01) (Table 3).
Relationship between coordination and walking after stroke using Pearson's correlation coefficient r (95% CI, p value).
| Coordination | Relationship to walk tests | |
|---|---|---|
| 10-m Walk Test | 6-min Walk Test | |
| LEMOCOT | 0.42 (0.07–0.68, 0.02) | 0.50 (0.18–0.73, 0.01) |
LEMOCOT, Lower Extremity Motor Coordination Test.
This quantitative observational study has shown a moderate positive relationship between walking speed and lower limb coordination measured using the LEMOCOT in people with stroke who have good strength in their lower limb muscles. That is, people after stroke with good coordination walk faster and those with poor coordination walk slower. Overall, the results indicate that without other obvious motor impairments, coordination explains some of the slowness in walking after stroke.
The participants of this study were people with stroke who had good lower limb strength but still had some disability in walking. Their walking speed on the 10-m Walk Test, walking distance on the 6-min Walk Test and coordination in the LEMOCOT were all about two-thirds of their healthy counterparts. Similar to our findings, a study investigating coordination after stroke using the LEMOCOT score21 showed reduced coordination of the affected lower limb in well-recovered stroke survivors, with stroke survivors demonstrating 75% of healthy reference values. Recently, a study found that coordination using the LEMOCOT score, made the most consistent contribution to walking after stroke in community ambulators.15 These studies, combined with the results from our study, demonstrate that people who have good strength after stroke can continue to have lack of coordination affecting their lower limb.
Walking speed is an independent predictor of survival in older adults22 with people over 65 years with slower walking speeds having a higher mortality rate.23 Therefore, improvement in walking speed is important for community ambulation in people with stroke to maintain their ability to live independently and their participation in the community and to reduce the risk of death. Our research suggests that, clinically, in order to improve walking speed in community walkers with good lower limb strength; rehabilitation could include exercises that challenge coordination, i.e., both temporal and spatial parameters of movement. Means of achieving this could include using markers such as footprints to set the spatial parameters (i.e., step length) and providing auditory cues such as a metronome to set the temporal parameters (i.e., cadence). For example, a systematic review incorporating seven studies found that walking training incorporating cueing of cadence via a metronome or music demonstrated a greater effect than walking training alone at increasing cadence (by 19steps/min) and consequently walking speed (by 0.23m/s).24
A limitation of our study is that it involved a sample of convenience at a single site. However, our recruitment process involved stratifying for walking speed, thus increasing the representativeness of our sample of stroke survivors with good strength. According to the walking categories outlined by Perry et al.,25 the stratified walking speeds of 0.6–1.2m/s in our study represent a good range of community walkers from limited community ambulation to full community ambulation. Furthermore, the similarity between the walking speed measured in the 10-m and the 6-min Walk Tests suggests that fatigue did not influence the tests. A second limitation of our study is that we did not get an exact measurement of participants’ strength and as such, we therefore cannot definitively confirm that strength deficits did not have some effect on their walking speed. However, a study that measured the relationship of combined leg strength of four muscle groups (knee extensor, knee flexor, ankle plantar flexor, ankle dorsiflexor) and walking speed in 409 older adults showed a non-linear relationship between leg strength and gait speed. Once the summed lower limb strength reached 275Nm, any further increase in strength did not influence walking speed.11 Therefore it is unlikely that the strength deficits of the stroke survivors in our sample would influence walking speed since they had good lower limb strength, i.e., at least ≥Grade 4 in the 6 main lower limb flexors and extensors on Manual Muscle Testing.
In conclusion, this study has shown a moderate positive relationship between walking speed and lower limb coordination measured using the LEMOCOT in people with stroke who have good strength in their lower limb muscles. Incorporating coordination exercises focusing on temporal and spatial elements during walking rehabilitation for these individuals may promote improved walking speed and improved ability to participate in the community, but this remains to be tested.
Conflicts of interestThe author declares no conflicts of interest.