The traditional overflow method for measuring limb volume remains the gold standard, but many disadvantages still inhibit its routine use in clinical practice.
ObjectiveTo assess the intra-rater and inter-rater reliability and criterion validity of the ‘communicating vessels volumeter’ (CVV) for volume measurement of lymphedematous upper extremities (LUE) by using the overflow volumeter (OV) as the reference standard.
MethodsTwelve LUE of 12 women undergoing mastectomy for breast cancer were measured three times each by three raters using both methods, totaling 216 volume measurements. Criterion validity was estimated by 33 volume measurements of one cylinder of known volume by three raters using both methods, totaling 198 measurements.
ResultsMeasurement time was short with both CVV and OV. The intraclass correlation coefficient3,1 was high for both CVV and OV in intra-rater (0.99 vs 0.99) and inter-rater (0.99 vs 0.99) analyses. The bias between methods was low (7.50mL; 0.40%) and the limits of agreement were narrow (−5.80 to 6.50%). The volumes were statistically equal with a strong correlation (R2=0.98) between methods. CVV was more accurate than OV (0.00 vs 0.02%) in cylinder measurements.
ConclusionThe high intra-rater and inter-rater reliability rates of CVV were comparable to those of OV, and the volumes resulting from LUE measurements were statistically equal in the two methods. Criterion validity rates indicated that CVV measurements were closer to the actual value of the cylinder than those obtained with the OV.
The role of measurement in physical therapy cannot be overstated. However, it is not sufficient that measurements in physical therapy be reproducible, accurate, and close to reality. Above all, they need to be practical, easy to implement, and affordable, thus stimulating their standardized use on a routine basis in clinical practice.
A common and relatively understudied complication of breast cancer therapy is upper extremity lymphedema. Because upper extremity lymphedema can have a detrimental impact on the quality of life of patients who have had breast cancer, the role of limb volume measurement in the practice of physical therapy is currently of great relevance to proper monitoring of this complication. In this setting, the precise determination of upper extremity volume serves three important purposes: (a) making an early diagnosis of lymphedema; (b) following the volumetric evolution of the lymphedema; and (c) comparing the effects of different treatments.1
The traditional overflow method for measuring limb volume, based on Archimedes’ principle, remains the gold standard,2–7 but its routine use has been challenged by several difficulties associated with the objective measurement of upper extremity volume.1,8–12 Several studies have focused on providing an alternative to the gold-standard overflow method while overcoming classical drawbacks, such as volumetric losses due to its open system and contraindication in the presence of ulcers.1,2,4–6,8,11–18 However, the options available have not adequately overcome these drawbacks, since some devices maintain some of the original disadvantages associated with overflowing, while others are expensive and/or provide inaccurate measurements for irregular surfaces or acral segments, such as hands and fingers.1,2,5,8,10–12,16,17
A device called the ‘communicating vessels volumeter’ (CVV) has been used to measure the volume of non-swollen wrist-hand segments, with reliable results in both intra-rater and inter-rater analyses presented in a previous publication.19 As a new contribution to this continuing effort, the hypothesis tested in this study was that the CVV would produce reliable intra-rater and inter-rater measurements of the volumes of edematous upper extremities in patients undergoing physical therapy for postmastectomy lymphedema.
The present study was therefore designed to determine the intra-rater and inter-rater reliability and criterion validity of the CVV for volume measurement of lymphedematous upper extremities (LUE) by using the traditional overflow method as the reference standard.
MethodsParticipantsThis measurement study was conducted to test the reliability and criterion validity of clinical measurement procedures performed with the CVV in patients undergoing physical therapy after breast cancer surgery. Volunteers recruited from the Physical Therapy Clinic of our institution underwent a screening interview and physical examination for enrollment in the study. Eligible participants were all adults aged ≥18 years with a diagnosis of upper extremity lymphedema after breast cancer who had a body mass index (BMI)≥18.50 and ≤39.90kg/m2 and agreed to participate in the study. Exclusion criteria were corticosteroid use, heart failure, renal failure or any other disorder that can affect blood flow or pressure (not controlled with medication), rheumatic or chronic inflammatory disease that can affect the acral joints, infection, or allergy to glove materials.
Three raters and two note takers were selected among fourth-year physical therapy students. All raters were previously trained to become familiar with the measurement procedures.
Overflow volumeter (OV)A polyvinyl chloride (PVC) upper-extremity OV for home use was manufactured to order (Q2 Tec Produtos Médicos e Odontológicos Ltda., Barretos, SP, Brazil) as previously described.13 The amount of water displaced by the OV was weighed on an electronic scale (UDC 20/2 POP; Urano Indústria de Balanças e Equipamentos Eletrônicos Ltda., Canoas, RS, Brazil) with maximum capacity of 20.00kg and accuracy of ±2.00g to ensure optimal precision for the method.
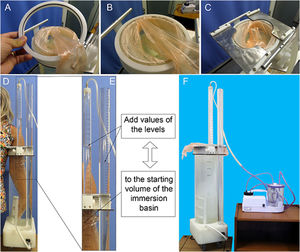
Communicating vessels volumeter (CVV)An acrylic prototype of the CVV was manufactured to order (Q2 Tec Produtos Médicos e Odontológicos Ltda.) and consists of three communicating vessels: (a) an immersion basin for the upper extremity; (b) a volumetric column; (c) and a suction column to extract residual air. The upper extremity, when introduced into the immersion basin, is protected by an upper-extremity-length glove that attaches to the edge of the basin, thereby closing its open end. Two accessories are used in this process, one PVC ring for the fixation of the border of the glove and a pair of metal sheets to restrict the upper expansion of the glove; both are coupled to the upper edge of the immersion basin. A veterinary surgical glove (95.00cm long; Guantes Simil Latex, SuperFlex®, Argentina) was used in this study and served as the interface between the upper extremity and the water in the immersion basin. The vacuum source was a 70.00W portable tracheal suction system for home use (Aspiramax; NS Indústria de Aparelhos Médicos Ltda., São Paulo, SP, Brazil).
Cylinder of known volume (“phantom”)Each of the three raters made 33 measurements of a polyamide cylinder of known volume (πr2h=999.68mL; where r is radius and h is height) by each of the two methods, as performed in previous studies.4,10–13,20 A total of 198 measurements of the cylinder were made.
Measurement proceduresA non-contact infrared digital thermometer (model GM-300; Benetech®, Guangdong, Mainland, China) was used to monitor water temperature in the devices during both OV and CVV trials. The water inside the immersion basin of both devices was maintained within the temperature range defined by Boland and Adams21 using a portable electric heater. A small PVC stepladder, with four steps spaced 2.00in. apart, was fixed to the bottom of the immersion basin of both devices to serve as a baseline reference to limit the immersion of the LUE. To further standardize the volume measurements made by both methods, an immersion threshold was established at 15.00cm from the acromion and was marked on the skin to guide the immersion process. That is, all LUE were advanced into the water until they reached this predetermined threshold.
OV measurementsThe participant was asked to gently immerse the LUE into the immersion basin. The displaced water was collected into a pitcher, which was weighed on the electronic scale (previously corrected for the mass of the empty pitcher). The water mass was converted from grams to milliliters, considering that 1.00g of water is equivalent to 1.00mL of water. This amount equals the volume of the LUE. The LUE volumes of the three consecutive OV measurements were recorded for further analysis. A 10% sodium hypochlorite solution was added to the water in the immersion basin (1.00mL per 10.00L of water), and the water was changed every day during the experiment.
CVV measurementsThe participant was asked to put the glove on the LUE, and then to submerge the LUE partially until the edge of the glove was tied to the fixation ring connected to the upper edge of the immersion basin. The LUE was then slowly submerged into the full immersion basin, and the metal sheets intended to restrict glove expansion were coupled to the upper edge of the basin just above the fixation ring. The air remaining between the glove and the basin water was removed by activating the vacuum system connected to the top of the suction column by a latex tube. The volume of the LUE is the sum of the volumes measured in the immersion basin, in the suction tube, and in the volumetric column (Fig. 1). The LUE volumes of the three consecutive CVV measurements were recorded for further analysis.
The communicating vessels volumeter (CVV). (A) and (B) glove tied to the fixation ring; (C) metal sheets to restrict glove expansion; (D) introduction of the upper extremity in the immersion basin; (E) reading procedure for volume measurement; and (F) the CVV connected to a suction system for home use.
Sample size was calculated for the reliability analysis of the measurements obtained in this study using Student's t-test for paired data. At least 102 readings per method were required to give 80.00% power to detect a significant difference between OV and CVV measurements, with a two-sided type 1 error of 5.00%.
Data analysisDemographic data and descriptive measures were expressed as mean (SD). All analyses were performed using SAS®, version 9.0 (SAS Institute Inc., Cary, NC, USA). A p-value <0.05 was considered significant for all analyses.
Criterion validityCriterion validity22 of the CVV, considering both LUE and cylinder measurements, was assessed by calculating the bias (CVV volume−OV volume), limits of agreement (LOA=mean difference±1.96*SD), and a specific calculation of the difference between the measurements by the two methods, called accuracy (Ac), given by the following formula23: Ac=100*(CVV−OV)22n/0.5CCV¯+OV¯, where CVV−OV is the difference between the volume measurements made by the two methods, CVV¯ is the mean of the CVV measurements, and OV¯ is the mean of the OV measurements.
With regards to the LUE measurements, a regression analysis of volume differences CVV−OVvs OV values was performed to evaluate whether CVV criterion validity was influenced by the volume magnitude.
Construct validityIn relation to the cylinder measurements, hypothesis testing was used to determine whether the difference between the cylinder volumes calculated by the two methods and the known cylinder volume was statistically different from zero.
Intra-rater and inter-rater reliabilityThe intraclass correlation coefficient (ICC 3.1, two-way mixed model) and the standard error of measurement (SEM), given by, where SD is the standard deviation, were used to assess the reliability of the two volume measurement methods (OV and CVV) by calculating intra-rater and inter-rater variance, with 95% confidence interval (CI). The sign test was used to determine any differences in LUE volume estimated by the two methods and any differences in time records and water temperatures between the two methods.
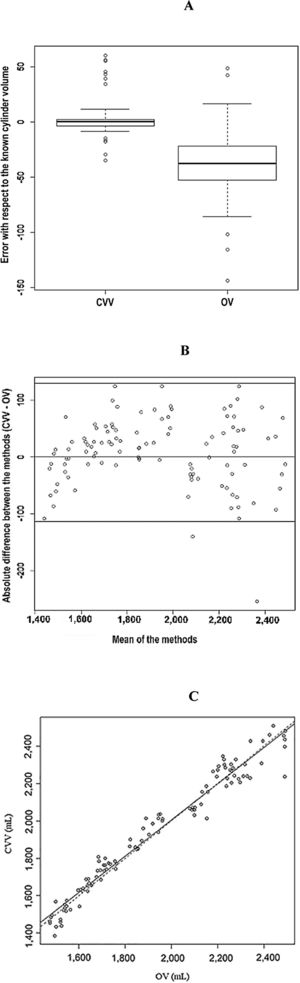
Graphic techniquesBland–Altman bias and LOA plots and concurrent validity plots were used to compare the LUE volume measurements made by the two methods (OV and CVV). To better visualize the measured volumes in relation to the known volume, boxplots of the differences in the measurements by the two methods in relation to the cylinder of known volume are displayed.
EthicsThe study was approved by the Research Ethics Committees of the participating institutions (approval no. 569854, Universidade Federal de São Paulo, São Paulo, SP, Brazil; and approval no. 1198169, Universidade Federal de Uberlândia, Uberlândia, MG, Brazil). All procedures were in accordance with the ethical standards of the institutional research committees and with CNS Resolution 466/2012 (main guideline for ethics in research in Brazil). Written informed consent was obtained from all participants before inclusion in the study.
ResultsTwelve women with unilateral postmastectomy lymphedema were ultimately included in the study and their 12 LUE were evaluated 18 times each by the three raters, who alternately measured each LUE three times using the CVV (108 readings) and three times using the OV (108 readings), resulting in 216 volume measurements for analysis in this study.
Mean (SD) patient age was 53.70 (9.80) years (range, 37–69 years). Mean (SD) height was 1.57 (0.07) m (range, 1.45–1.67m), mean (SD) weight was 69.40 (8.80) kg (range, 52.50–86.60kg), and mean (SD) BMI was 28.21 (3.84) kg/m2 (range, 20.51–32.08kg/m2). Eleven participants were right-handed, and one was left-handed.
CylinderThe SEM was lower in CVV than in OV measurements, both in inter-rater (CVV, 14.75mL vs OV, 29.47mL) and intra-rater (CVV, 14.75mL vs OV, 29.36mL) analyses. The total SD of cylinder measurements (paired t test) was statistically lower for CVV (SD=16.00mL) than for OV (SD=30.00mL) (Table 1A).
(A) Mean, median and SD of cylinder volume measured by OV and CVV, per rater and total; (B) Mean, median and SD of OV and CVV measurements, per rater and total, followed by inter-rater and intra-rater intraclass correlation coefficients, in lymphedematous upper extremities.
| Rater | n assessments | OV (mL) | CVV (mL) | ||||
|---|---|---|---|---|---|---|---|
| Mean | Median | SD | Mean | Median | SD | ||
| A. Cylinder | |||||||
| I | 33 | 955 | 950 | 27 | 1001 | 999 | 15 |
| II | 33 | 971 | 968 | 26 | 1004 | 1001 | 14 |
| III | 33 | 961 | 962 | 36 | 1001 | 1000 | 18 |
| Total | 99 | 962 | 962 | 30 | 1002 | 1000 | 16 |
| Inter-rater SEM (mL) | 29.47 | 14.75 | |||||
| Intra-rater SEM (mL) | 29.36 | 14.75 | |||||
| B. Lymphedematous upper extremities | |||||||
| I | 36 | 1937 | 1890 | 323 | 1942 | 1944 | 308 |
| II | 36 | 1919 | 1867 | 305 | 1935 | 1956.5 | 312 |
| III | 36 | 1936 | 1895 | 319 | 1938 | 1917 | 315 |
| Total | 108 | 1931 | 1884 | 313 | 1938 | 1933 | 309 |
| Inter-rater ICC (95%CI) | 0.99 (0.98–0.99) | 0.99 (0.98–0.99) | |||||
| Inter-rater SEM (mL) | 32.80 | 36.56 | |||||
| Intra-rater ICC (95%CI) | 0.99 (0.98–0.99) | 0.99 (0.98–0.99) | |||||
| Intra-rater SEM (mL) | 31.28 | 36.56 | |||||
OV, overflow volumeter; CVV, communicating vessels volumeter; SD, standard deviation; SEM, standard error of measurement; ICC, intraclass correlation coefficient; CI, confidence interval. p-Value (paired t test): <0.001 (comparison between standard deviations).
The CVV bias was 2.40mL (0.20%), while the OV bias was −37.50mL (−3.80%). The LOA ranged from −28.40 to 33.20mL in CVV and from −97.20 to 22.10mL in OV measurements. By applying the accuracy formula to the cylinder measurements in relation to its known volume, we obtained an Ac=1.00×10−3% for CVV and an Ac=19.00×10−3% for OV (Table 2A).
(A) Construct validity of CVV and OV for cylinder measurement (999.68mL); (B) criterion validity of CVV in relation to OV for volume measurement of lymphedematous upper extremities (n=12).
| Method | Rater 1 | Rater 2 | Rater 3 | Overall | |||||
|---|---|---|---|---|---|---|---|---|---|
| Absolute (mL) | Relative (%) | Absolute (mL) | Relative (%) | Absolute (mL) | Relative (%) | Absolute (mL) | Relative (%) | ||
| A. Cylinder | |||||||||
| CVV | Biasa | 1.30 | 0.10 | 4.20 | 0.40 | 1.70 | 0.20 | 2.40 | 0.20 |
| LOA | −28.90 to 31.50 | −2.90 to 3.20 | −23.40 to 31.70 | −2.30 to 3.20 | −33.20 to 36.60 | −3.30 to 3.70 | −28.40 to 33.20 | −2.80 to 3.30 | |
| OV | Biasb | −45.00 | −4.50 | −28.70 | −2.90 | −38.90 | −3.90 | −37.50 | −3.80 |
| LOA | −97.70 to 7.60 | −9.80 to 0.80 | −80.00 to 22.60 | −8.00 to 2.30 | −109.40 to 31.60 | −10.90 to 3.20 | −97.20 to 22.10 | −9.70 to 2.20 | |
| B. Lymphedematous upper extremities | |||||||||
| CVV-OV | Biasc | 5.20 | 0.30 | 15.60 | 0.80 | 1.80 | 0.10 | 7.50 | 0.40 |
| LOA | −125.30 to 135.60 | −6.50 to 7.00 | −99.90 to 131.20 | −5.20 to 6.80 | −88.40 to 91.90 | −4.60 to 4.70 | −111.30 to 126.30 | −5.80 to 6.50 | |
OV, overflow volumeter; CVV, communicating vessels volumeter; LOA, limits of agreement.
Hypothesis testing showed that the mean volume measured by the OV was statistically lower than the known cylinder volume (p<0.001). The CVV, however, gave statistically the same mean cylinder volume (p=0.75) (Table 3 and Fig. 2A).
Mean, median and SD of OV and CVV measurements and the respective differences in relation to the cylinder.
| Variable | Mean (mL) | Median (mL) | SD (mL) |
|---|---|---|---|
| OV | 962.14 | 962.00 | 30.45 |
| OV−Cylinder | −37.54 | −37.68 | 30.45 |
| CVV | 1002.06 | 1000.00 | 15.72 |
| CVV−Cylinder | 2.38 | 0.32 | 15.72 |
OV, overflow volumeter; CVV, communicating vessels volumeter; SD, standard deviation. p-Value OV (sign test): <0.001. p-Value CVV (sign test)=0.747. p-Value OV×CVV (sign test): <0.001.
(A) Boxplot showing the behavior of CVV and OV measurements (mL) in relation to the known cylinder volume (criterion validity) and the distance between the measurements made by each method (reliability). (B) Bias and limits of agreement between CVV and OV (Bland–Altman plot) for volume measurement (mL) of lymphedematous upper extremities. CVV, communicating vessels volumeter; OV, overflow volumeter. (C) Concurrent validity between CVV and OV for volume measurement of lymphedematous upper extremities, obtained by the adjusted regression model. CVV, communicating vessels volumeter; OV, overflow volumeter.
Both the OV and CVV methods showed high reliability (i.e., consistent performance) for LUE volume measurements, with intra-rater and inter-rater ICC greater than 0.90 (Table 1B). The SEM and SD of LUE volumes did not differ significantly between OV and CVV in both intra-rater and inter-rater analyses.
The sign test showed that the measured volumes were statistically equal in the two methods (Appendix 1). Water temperature was also statistically equal in the two methods. There was a statistical difference of less than 1min in time records between the two methods.
When calculating the CVV bias in relation to OV, there was agreement between the two methods (Table 2B and Fig. 2B). The accuracy formula applied to LUE volume differences (CVV – OV) yielded a low value (Ac=2.00×10−3%), indicating that, on average, there was almost no difference for this type of assessment between the two methods. On average, the volumes obtained with the CVV were slightly higher than those obtained with the OV. The same was true when the three raters were evaluated separately.
The linear regression analysis of measurement differences (CVV−OV) vs OV values (y=12.80−0.00272x; R2=0.0003) showed no significant relationship between the volumes measured by the OV (x) and volume differences (y: CVV volume−OV volume). The adjusted regression model showed a statistically significant association between OV and CVV values (p<0.001), and that LUE volumes measured by the CVV explain 98% of the variance in the volumes measured by the OV (y=−12.80+1.000272x, R2=0.98) (Fig. 2C).
DiscussionMain findingsThe comparison of intra-rater and inter-rater reliability showed that both CVV and OV measurements had high ICC for LUE volume measurements, according to the Currier criteria,24 and were compatible with the values obtained with the gold standard in previous studies.1,3,5,6,11,15,17,25 Intra-rater and inter-rater SEM values were also sufficiently low, considering the volumetric magnitude of the upper extremity measured in the present study, since other studies measured only the volume of the arm-forearm segment, excluding wrist and hand, due to the limitations of the three-dimensional scanning or circumference measurement of irregular surfaces.3,5,6,11 There was no statistically significant difference in intra-rater and inter-rater ICC and SEM between CVV and OV, which also had similar relatively low SD5,6 for their LUE volume measurements. The lack of difference between reliability measures for both devices was supported by the results of the sign test, showing statistical equality between LUE volume measurements made by CVV and OV. The excellent reliability of the overflow method, used as the reference standard, confirmed previously published OV-related findings.13,26 However, the sources of disadvantages associated with the OV were present as well.1,2,12,27 The CVV, in turn, eliminated the disadvantages due to its design and operation in a closed system. Unlike the CVV, open volumeters require that the immersion basin be replenished1,4,6,7,10–15,17,18,20,21,23,25,27–30 for measurement of the same LUE by different raters.
General findingsMeasurements with the OV were statistically faster than with the CVV. This is probably due to the simplicity and effectiveness of the OV designed by Lette13 for home use and patient self-management.26 As for the CVV, the gloves used, although attachable, were not custom-made for the device. Due to budget limitations, commercially available extra-large veterinary surgical gloves made of ethylene-vinyl acetate were used. However, manufacturing disposable gloves in variable sizes may further reduce CVV measurement time. Nevertheless, the mean CVV volume measurement time was approximately 1min40s, shorter than that previously reported using overflow methods,13,23,31 perometry,32 laser scanning,2,4 and circumference measurements,1 or even when compared to the mean measurement time of its first prototype for volume measurement of the wrist-hand segment.19 Also noteworthy is that, during all OV and CVV trials, the water temperature in both devices was strictly maintained at a temperature range within which vascular response does not change the volume of the measured segment.6,15,21
The bias observed in the mean difference between LUE measurements made by CVV and OV, considering the latter as the reference standard, was lower than that reported in studies using scanning methods and circumference measurements compared to the gold standard.5 The present study also showed narrower LOA with the CVV (vs OV) than those reported with the use of laser scanning4 and circumference measurements.10,11,25 Our LOA were larger than those reported for Kinect33 and SkanLab,5 but it should be noted that these are three-dimensional scanning methods whose measurements, in the respective studies, excluded the wrist-hand segment, an important part of the upper extremity frequently affected by postmastectomy lymphedema.28 As shown in the Bland–Altman plot (Fig. 2A), there was a statistically strong agreement between CVV and OV, and the adjusted regression model, represented by the concurrent validity plot (Fig. 2B), makes it clear that both methods are interchangeable for LUE volume measurement. The criterion validity of CVV measurements, expressed as a low bias of 0.40% and LOA ranging from −5.80 to 6.50%, indicates a variance below the threshold of 10% difference between upper extremities for the diagnosis of lymphedema, which further supports the interchangeability of the two methods compared here.11,34 The criterion validity of CVV measurements, calculated as the difference in relation to OV measurements, was low, indicating close proximity of LUE measurements made by the two methods. The linear regression analysis of the difference between LUE measurements by the two methods (CVV−OV) confirmed the criterion validity of the CVV by demonstrating that the result for volume differences was not significantly associated with the magnitude of the volumes measured using the OV.
Clinical applicabilityThere were practical advantages of the CVV over the OV, including a more hygienic, precise and rapid measurement of the volume of severely edematous segments without removing the limb from the water. These features support the clinical feasibility of CVV for comprehensive assessment of upper extremity volume, including wrist and hand, with high reproducibility of the gold standard and coexistence of characteristics widely reported as desired for a potential surrogate method for measuring limb volume.2,9 Also, the use of a glove to protect the limb under analysis prevents direct contact of the limb with water, which favors the indication of CVV in the presence of ulcers and open or dressed wounds.
Study limitations and strengthsA limitation involves the use of only one phantom. As in the study by Man et al.,12 we used a single inanimate object of known volume. Other studies with similar methods have used several objects of different known volumes.4,5,13 The intra-rater and inter-rater SEM values, as well as the total SD of CVV measurements, were approximately half the same values obtained with the OV, indicating greater reliability for cylinder volumes measured by the CVV. The CVV bias was lower than the OV bias for cylinder measurements, and the lowest among the aforementioned studies. McKinnon et al.,4 in their study using laser scanning as a new method of volume measurement and the coefficient of reproducibility, showed a difference of 19.00mL in relation to the volume of the measured objects. This observation of a tendency of the OV to underestimate the actual volume is supported by the present findings. Also, it must be noted that the number of included patients was limited to the ethically based minimum necessary to ensure the statistical robustness of the results from reliability and criterion validity analyses (12 patients; 12 LUE). However, this number of volunteers allowed us to collect a large number of measurements with the two devices by adopting the standard of triplicate measurements and raters, as recommended by the International Society for Advancement in Kinanthropometry (ISAK).35 In this respect, the number of measurements performed was sufficiently large to give statistically significant findings.
Implications for future researchThe high correlation indicating a positive relationship between CVV and OV implies that the CVV could be used as a simple and safe alternative to the traditional overflow method in clinical practice. This should contribute to the development of a clear protocol that is based on current practice and experience and that can be tested and adapted over time to improve practice. Conducting a measurement study of the CVV with measurements performed by graduated physical therapists, similar to the study conducted by Farrel et al.,29 may allow a comparison of the consistency of the measurements obtained in the present study by physical therapy students with regard to the effectiveness of using the device in clinical practice, a setting with poorly controlled protocol and environment. Further investigations of the CVV are warranted to assess potential ergonomic adjustments, different sizes of gloves and boots, and the use of a waterproof infrared sensor, which could make the process of volume measurement faster and obviate the need to read the volume level on the volumetric column of the CVV. This would also allow measurement of lymphedema or other volumetric disorders of the lower extremities.
ConclusionsThe high intra-rater and inter-rater reliability rates of the CVV were comparable to those of the OV, and the volumes resulting from LUE measurements were statistically equal in the two methods. Criterion validity rates indicated that, considering the LUE volumes obtained with the OV as the actual volumes, the CVV was statistically equal to the OV. However, when the cylinder of known volume was considered the actual reference, the CVV was more accurate, with a statistically significant difference in relation to the OV.
Financial disclosureA research grant was received from the São Paulo Research Foundation (Fundação de Apoio à Pesquisa do Estado de São Paulo, FAPESP) (grant number 2010/11552-6). This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES) – Finance Code 001.
Conflicts of interestThe authors declare that they have a patent pending (number PI 0502899-0 A, deposit under review).
We thank our volunteers who made this study possible. We are also grateful to the statistician Lorene Guirado, for her expert statistical advice, to Aline Candiota for her assistance in editing the manuscript, and to the engineer Cristiano Campozana de Queiroz for his valuable technical assistance.
Mean, median and SD of volume, temperature and time records for OV and CVV, followed by the p-value of the sign test, in lymphedematous upper extremities.
| Comparison | Method | n assessments | Mean | Median | SD | p-Value (sign test) |
|---|---|---|---|---|---|---|
| Volume (mL) | OV | 108 | 1930.74 | 1884 | 312.78 | 0.068 |
| CVV | 108 | 1938.27 | 1933 | 308.95 | ||
| Temperature (̊C) | OV | 108 | 29.01 | 28.9 | 1.62 | 0.062 |
| CVV | 108 | 28.73 | 28.5 | 1.23 | ||
| Time (s) | OV | 108 | 46.97 | 47 | 9.45 | <0.001 |
| CVV | 108 | 100.64 | 98 | 25.34 | ||
OV, overflow volumeter; CVV, communicating vessels volumeter; SD, standard deviation.