The “6-clicks” is the reduced version of the Activity Measure for Post-Acute Care for inpatients that assesses limitations in basic mobility, daily activity, and applied cognitive, simply and quickly.
ObjectiveCross-culturally adapt the “6-clicks” into Brazilian-Portuguese and verify its measurement properties.
MethodsCross-cultural adaptation followed recommendations from international guidelines. Reliability indices, standard error of measurement and minimum detectable difference were calculated. Participants included 13 professionals, 13 patients and 13 companions. Test of measurement properties involved 101 patients’ of both sexes, hospitalized in the infirmary, under physical therapy care, able to understand and respond to commands and with no discharge expectation. Their 30 companions were also included.
ResultsMinor changes implemented to the original version. The three domains showed adequate internal consistency (α>0.65). Inter-rater reliability (n=50) and test–retest reliability, when administer to patients (n=51) and to companions (n=30), showed good for basic mobility domain (ICC2.1=0.81, 0.83 and 0.82, respectively), good to moderate for daily activity (ICC2.1=0.78 and ICC3.1=0.71 and 0.82, respectively) and moderate to poor for applied cognitive (ICC2.1=0.64, 0.36 and ICC3.1=0.63), respectively. The highest agreements among patients/companions were also in basic mobility. Standard error of measurement ranged from 2.03 to 2.64 while the minimum detectable difference ranged from 5.63 to 7.32.
ConclusionTranslated and adapted Brazilian version of the “6-clicks” showed acceptable measurement properties. The functional data provided by the instrument could be used to enhance care and help treatment follow-up.
Physical therapists play an essential role during the hospitalization period, since patients often present functional impairment limiting their activities.1 Functional deficits worsen clinical conditions and increase the length of hospitalization and rehabilitation after discharge.2 A good evaluation is imperative to monitor results, improve procedures and communication among professionals and services.3–5
In hospital settings, the use standardized assessments with items consistent with patients’ demands points to excellence in professional performance. However, quality practice can be challenged by excessive time required by available questionnaires, with complex interpretation, absence of relevant questions and lack of measurement properties.6,7 Ensure good measurement properties, such as test–retest and Inter-rater reliability is important to demonstrate consistency of scores by the same or by different raters.8 Standardized functional instruments grounded on the International Classification of Functioning, Disability and Health (ICF),9 are necessary to help improve the assistance and care of patients.
The “6-clicks” questionnaire, derived from the Activity Measure for Post-Acute Care (AM-PAC) CAT (Computer Adaptive Test) version, describes the functional profile of adult patients with any disease in the hospital environment.10 The AM-PAC CAT is composed of 269 items, based on the activity component of the ICF, and was developed according to Item Response Theory's (IRT) assumptions and CAT measurement technique.10 In the IRT, the calibrated items are sorted in a continuum, based on the level of difficulty of the activity; the CAT is a technique that optimize item response: based on answers from previous questions the following items to be presented are selected by algorithms.11 To administer a CAT-based instrument, access to a computer is required. Services lacking this technology should use the reduced and printed versions - outpatients, Medicare (USA) patients and inpatients - drawn from the bank of items of the AM-PAC CAT.10 The inpatient version “6-clicks” evaluates the domains of basic mobility, daily activity and applied cognitive. It is composed of simple items and of quick and easy administration.10 This instrument is for multidisciplinary team use and showed excellent reliability among physical therapists and nurses.12 It is an important tool to help health professionals identify patients’ limitations, make treatment decisions and support to other professionals.13,14 The “6-clicks” has also been used to predict referral of patients after hospital discharge,15,16 ensuring continuity of care. In addition, the “6-clicks” has various forms of application that include direct observation of the patient performing the activity, clinical judgment (professionals) or interview of the patients, companions and professionals from the health care team.10
Some of its features, including simplicity, agility of administration and interpretation, and multidisciplinary use attest to its advantage over other existing inpatient measures. However, this instrument needs to be translated and adapted into Brazilian-Portuguese language, like the Outpatient AM-PAC version,17 to ensure its equivalence to the original version. To date, only the basic mobility and daily activity domains had the measurements properties verified, which showed adequate.14,18 Therefore, the purpose of this study was to translate and cross-culturally adapt the “6-clicks” into Brazilian-Portuguese and verify its measurement properties.
MethodsThis study was approved by the Ethics Review Committee of the Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, MG, Brazil, by the Learning and Research Department of the Clinical Hospital from Universidade Federal de Minas Gerais (HC-UFMG) and by the Nucleus of Education, Extension and Research of the Risoleta Tolentino Neves Hospital (RTNH), CAAE: 55602216.3.0000.5149. All participants signed the Informed Consent.
Measuring instrumentInpatient short form “6-clicks”The “6-clicks” has three domains: basic mobility (transferring in bed, sitting and getting up from the chair, walking, etc.), daily activity (changing clothes, feeding oneself, bathing, etc.) and applied cognitive (understanding conversations, remembering tasks, taking care of complicated tasks, etc.).10 Each domain has six items, scored on an ordinal scale from 1 to 4 according to the degree of difficulty or need for assistance that the patient presents to perform the activity (item). Lower scores indicate greater disability.10 The final score of each domain informs the functional profile of the patient and is obtained by summing the scores from the items. Raw score can be transformed into standardized score to allow comparison with other versions of the AM-PAC (outpatient, Medicare and “6-clicks”).10,15 Professionals score this instrument preferably by clinical judgment and/or observation of how the activity was performed.10 If the activity is difficult to observe, the professional may ask the patient or companion to answer the item.10
Translation and cross-cultural adaptationAfter permission for translation of the “6-clicks”, we followed the recommendations of the authors of the instrument19 and the ones in the literature.8,20 Initially, three professors from the Physical Therapy and Occupational Therapy departments of UFMG, evaluated the conceptual equivalence and relevance of the items. Using a questionnaire, they verified the concept of functionality addressed by the instrument and classified the relevance of the items to rehabilitation in Brazil.19 The professors also informed whether there were items difficult to understand or administer.19 The observations were taken into account by the team of translators.
The translation was carried out in pairs including three physical therapists and one occupational therapist, with different background and experiences in rehabilitation and fluent in Portuguese and English. The pairs of professionals conducted the translation independently. The result was the production of two versions of the “6-clicks” in Portuguese-Brazil, which were compared and synthesized into a single one.8,20 This version was then back-translated into English by two independent native speakers of English-speaking countries and fluent in Brazilian-Portuguese, with different professional backgrounds.20
Finally, a committee of experts reviewed the original version of the instrument, translations and back translations to ensure semantic, idiomatic and conceptual equivalence.20 This committee was composed by members of the equivalence and translation stages, along with other rehabilitation professionals.20 After this review, the pilot version was sent to the authors of the instrument for approval.
ParticipantsDifferent groups of participants composed the sample of the study, at its various stages. The assessment of the “6-clicks” translated version was conducted in two phases: cognitive interviews and pre-test. A group of three health care professionals, three inpatients and three inpatients’ companions participated in the cognitive interviews. Following sample size recommentations20 a total of 30 participants (i.e., ten health care professionals, ten inpatients and ten inpatients’ companions) were administered the translated version of the “6-clicks (pre-test)”. To assess the instrument's measurement properties, a group of 65 inpatients and their companions participated in the patient/companion agreement investigation and 51 out of this group participated in the test–retest examination. Finally, another group of 50 inpatients, from a different hospital, participated in the inter-rater reliability. No participant was included in more than one stage or phase described.
Assessment of the translated and adapted versionIn this phase, two methods were used: cognitive interviews and pre-tests. The interviews verified if the items and response options were clear to the target audience of the instrument,8,19 and the pre-test ensured the understanding of the items.20 Participants were recruited at the HC-UFMG and from RTNH, and those responsible for this stage were previously trained.
The interviews were conducted in three rounds. In each round a health care professional, patient and companion took part. Participants responded the “6-clicks” questions and then were requested to express their understanding of the question's content. They were also asked to explain previously selected terms that could cause confusion and clarify other questions.21,22 At the same time, the need for repetition or explanation of items and/or response options were annotated. The interviews were recorded and later transcribed. After each round, the need for adjustments were assessed.
The pre-test was then conducted using the version with the changes proposed after the interviews. The participants, after each item, answered the following question: “What did you understand about this question?”. From the answer, the interviewer annotated whether it was understood or not. Confusing items informed by more than 15% of respondents were reviewed.23
Evaluation of measurement propertiesThe evaluation of measurement properties followed the recommendations of the COnsensus-based Standards for the selection of health status Measurement INstruments (COSMIN).24 Two independent convenience samples of patients were selected for test–retest and inter-rater reliability. We included clinically stable patients, over 18 years of age, of both sexes, hospitalized in different wards. The patients were in therapeutic (physical therapy) care without expectation for discharge for the next three days. In addition, participants should be able to understand and respond to commands, as proposed by Andres et al.25 For the retest, in addition to these criteria, patients with companions were included. Participants who were discharged during the assessment period and those who refused to complete the evaluation were excluded.
Three examiners administered the final translated version of the “6-clicks” in interview format. This mode of application was chosen since the examiners were not part of the clinical staff of the hospital. First, a pilot study (n=10) was conducted to test the methodology and train the examiners.
For test–retest reliability, one examiner administered the instrument in one day and repeated the application to patients and to their companions after three days. In case the patient had a different companion, there was an attempt five days later to meet with the same companion from the first evaluation. Patient–companion agreement analyses used data from the first test–retest evaluation. For inter-rater reliability, two other examiners administered the “6-clicks”; one did the first evaluation and the other repeated the evaluation after three days. The pair of examiners took turns in the order of the interviews throughout the applications and refrained from talking with each other about the results. All examiners, when possible, assessed the patients at the same time of the day, to avoid changes in the patients’ routine that could influence the results.
Statistical analysisThe test–retest and inter-rater reliability, as well as the patient–companion agreement were analyzed using intraclass correlation coefficient (ICC), types (2,1) and (3,1), with 95% confidence interval (CI). First, the F-test verified the presence of systematic error. In the presence of error, the ICC2.1 was used, and in the absence, ICC3.1 was performed.26 ICC values <0.40 were considered poor, 0.40–0.75 moderate and >0.75 good.27 Items agreement was examined using quadratic weighted kappa; values <0.00 were considered poor, 0.00–0.20 minimum, 0.21–0.40 reasonable, 0.41–0.60 moderate, 0.61–0.80 substantial and 0.81–1.00 excellent.28 The standard error of measure (SEM) was calculated using the squared root of the residual mean square from ANOVA results.26 The minimum detectable difference (MDD) was calculated from the SEM with the following formula: MDD=1.96×√2×SEM.29 To check the internal consistency of each domain of “6-clicks” we used Cronbach's alpha. Values between 0.70 and 0.90 were considered of good consistency.29 The Statistical Package for Social Sciences version 19.0 was used for all statistical analyzes, except for the kappa coefficient, calculated using the StatsDirect version 3.
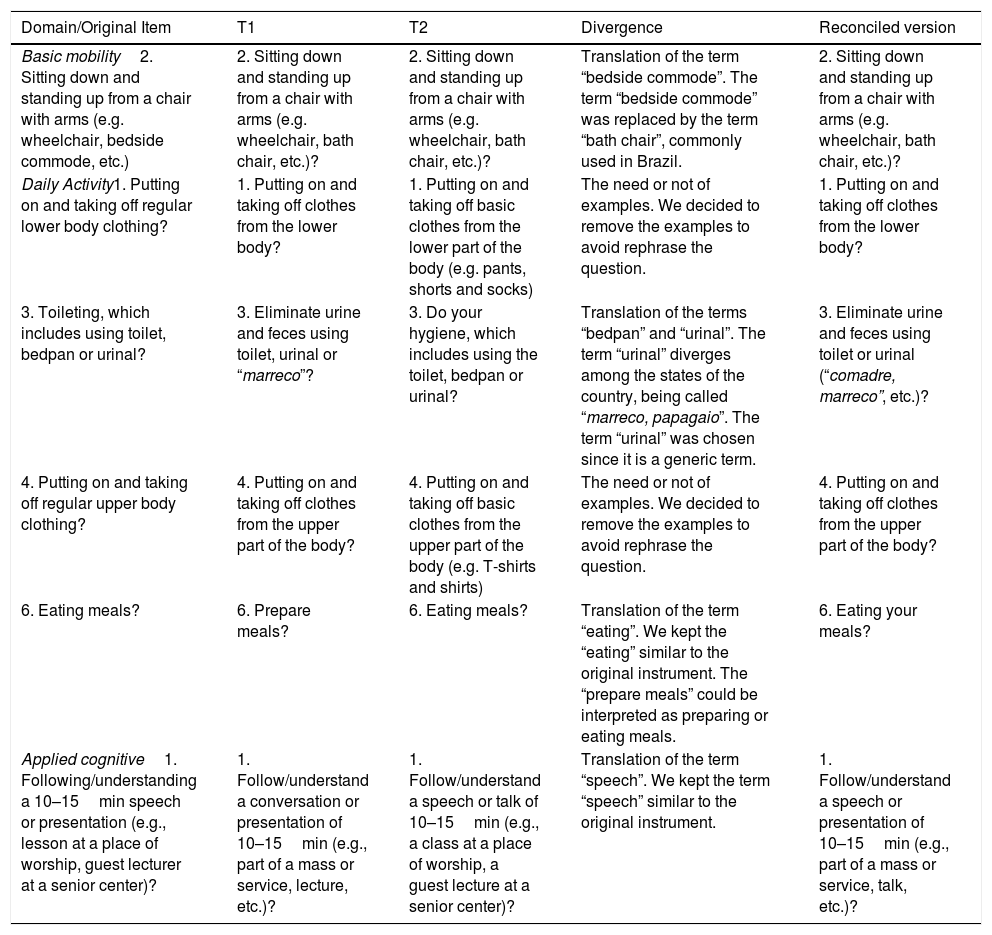
ResultsTranslation and cross-cultural adaptationDuring the consensus meeting, few items diverged between the pair of translators (Table 1). It was suggested that some items could be better explored with the cognitive interviews. These suggestions included understanding the terms from item 1 of daily activity domain: “talk or presentation of 10–15min”, “lower body” and “upper body”.
Divergences of translations observed during the translation phase of the study.
| Domain/Original Item | T1 | T2 | Divergence | Reconciled version |
|---|---|---|---|---|
| Basic mobility2. Sitting down and standing up from a chair with arms (e.g. wheelchair, bedside commode, etc.) | 2. Sitting down and standing up from a chair with arms (e.g. wheelchair, bath chair, etc.)? | 2. Sitting down and standing up from a chair with arms (e.g. wheelchair, bath chair, etc.)? | Translation of the term “bedside commode”. The term “bedside commode” was replaced by the term “bath chair”, commonly used in Brazil. | 2. Sitting down and standing up from a chair with arms (e.g. wheelchair, bath chair, etc.)? |
| Daily Activity1. Putting on and taking off regular lower body clothing? | 1. Putting on and taking off clothes from the lower body? | 1. Putting on and taking off basic clothes from the lower part of the body (e.g. pants, shorts and socks) | The need or not of examples. We decided to remove the examples to avoid rephrase the question. | 1. Putting on and taking off clothes from the lower body? |
| 3. Toileting, which includes using toilet, bedpan or urinal? | 3. Eliminate urine and feces using toilet, urinal or “marreco”? | 3. Do your hygiene, which includes using the toilet, bedpan or urinal? | Translation of the terms “bedpan” and “urinal”. The term “urinal” diverges among the states of the country, being called “marreco, papagaio”. The term “urinal” was chosen since it is a generic term. | 3. Eliminate urine and feces using toilet or urinal (“comadre, marreco”, etc.)? |
| 4. Putting on and taking off regular upper body clothing? | 4. Putting on and taking off clothes from the upper part of the body? | 4. Putting on and taking off basic clothes from the upper part of the body (e.g. T-shirts and shirts) | The need or not of examples. We decided to remove the examples to avoid rephrase the question. | 4. Putting on and taking off clothes from the upper part of the body? |
| 6. Eating meals? | 6. Prepare meals? | 6. Eating meals? | Translation of the term “eating”. We kept the “eating” similar to the original instrument. The “prepare meals” could be interpreted as preparing or eating meals. | 6. Eating your meals? |
| Applied cognitive1. Following/understanding a 10–15min speech or presentation (e.g., lesson at a place of worship, guest lecturer at a senior center)? | 1. Follow/understand a conversation or presentation of 10–15min (e.g., part of a mass or service, lecture, etc.)? | 1. Follow/understand a speech or talk of 10–15min (e.g., a class at a place of worship, a guest lecture at a senior center)? | Translation of the term “speech”. We kept the term “speech” similar to the original instrument. | 1. Follow/understand a speech or presentation of 10–15min (e.g., part of a mass or service, talk, etc.)? |
Note: T1, translation conducted by pair 1; T2, translation conducted by pair 2.
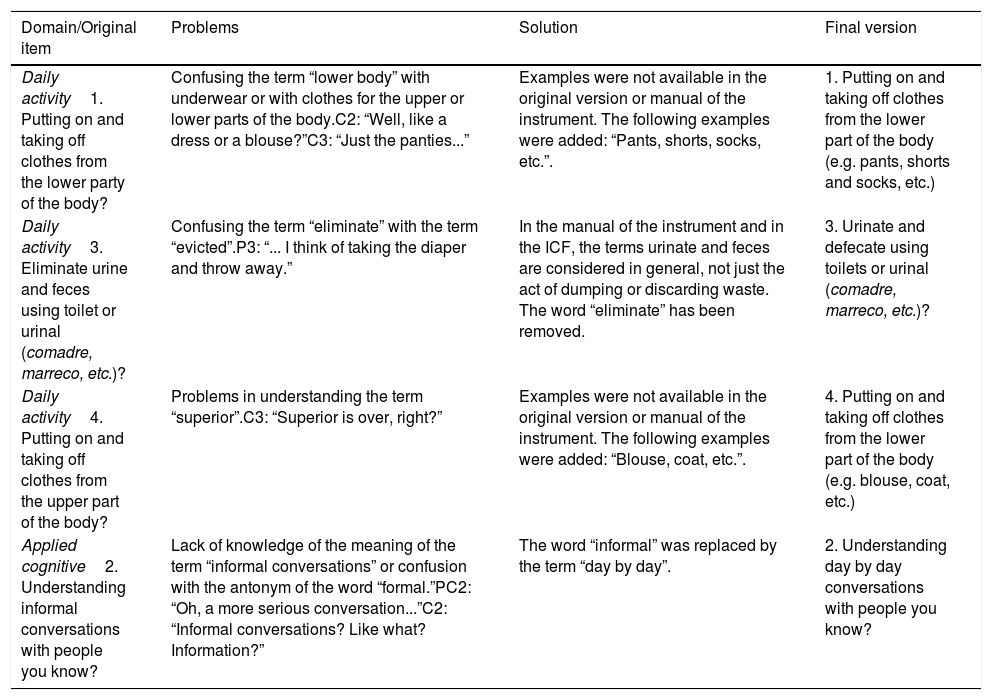
Seven women and two men ages 32–57 years, participated in the cognitive interviews. Patients had complete secondary education, were hospitalized from 10 to 30 days for pulmonary, oncological and renal diseases. Companions had education levels ranging from elementary to secondary school. Professionals (physical therapist, occupational therapist and a nurse) had postgraduate degree (specialization) with seven to 17 years of experience with inpatients. From the cognitive interviews, four items were changed to improve the participants’ understanding (Table 2). For the other items, no major changes were needed. In next stage, pre-test, participants were patients from both sexes, 25–77 years old, education ranging from elementary school to undergraduate degree and hospitalized from 4–29 days for oncological, orthopedic, cardiological or neurological diseases. Companions had similar education and were 20–73 years. Professionals were 24–51 years and had one to 22 years of experience with inpatients. None of the items were identified as confusing for more than 15% of the sample.
Problems and solutions detected during the cognitive interviews.
| Domain/Original item | Problems | Solution | Final version |
|---|---|---|---|
| Daily activity1. Putting on and taking off clothes from the lower party of the body? | Confusing the term “lower body” with underwear or with clothes for the upper or lower parts of the body.C2: “Well, like a dress or a blouse?”C3: “Just the panties...” | Examples were not available in the original version or manual of the instrument. The following examples were added: “Pants, shorts, socks, etc.”. | 1. Putting on and taking off clothes from the lower part of the body (e.g. pants, shorts and socks, etc.) |
| Daily activity3. Eliminate urine and feces using toilet or urinal (comadre, marreco, etc.)? | Confusing the term “eliminate” with the term “evicted”.P3: “... I think of taking the diaper and throw away.” | In the manual of the instrument and in the ICF, the terms urinate and feces are considered in general, not just the act of dumping or discarding waste. The word “eliminate” has been removed. | 3. Urinate and defecate using toilets or urinal (comadre, marreco, etc.)? |
| Daily activity4. Putting on and taking off clothes from the upper part of the body? | Problems in understanding the term “superior”.C3: “Superior is over, right?” | Examples were not available in the original version or manual of the instrument. The following examples were added: “Blouse, coat, etc.”. | 4. Putting on and taking off clothes from the lower part of the body (e.g. blouse, coat, etc.) |
| Applied cognitive2. Understanding informal conversations with people you know? | Lack of knowledge of the meaning of the term “informal conversations” or confusion with the antonym of the word “formal.”PC2: “Oh, a more serious conversation...”C2: “Informal conversations? Like what? Information?” | The word “informal” was replaced by the term “day by day”. | 2. Understanding day by day conversations with people you know? |
Note: C, companion; P, professional; PC, patient.
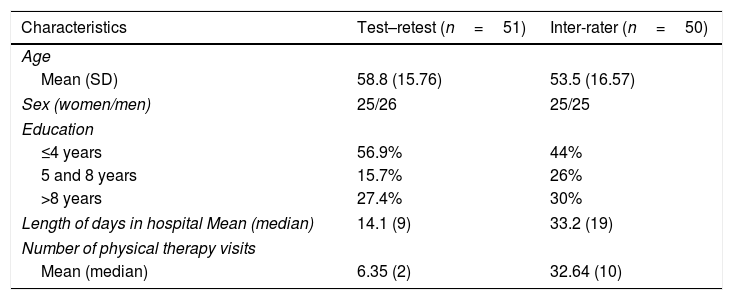
Of the 65 participants, 14 were discharged before the second evaluation. Participants were from the neurology (35.3%), cardiovascular surgery (35.3%), orthopedics and traumatology (23.5%) and other (5.9%) wards, such as nephrology. Additional information is presented in Table 3.
Characteristics of the sample for the reliability study.
| Characteristics | Test–retest (n=51) | Inter-rater (n=50) |
|---|---|---|
| Age | ||
| Mean (SD) | 58.8 (15.76) | 53.5 (16.57) |
| Sex (women/men) | 25/26 | 25/25 |
| Education | ||
| ≤4 years | 56.9% | 44% |
| 5 and 8 years | 15.7% | 26% |
| >8 years | 27.4% | 30% |
| Length of days in hospital Mean (median) | 14.1 (9) | 33.2 (19) |
| Number of physical therapy visits | ||
| Mean (median) | 6.35 (2) | 32.64 (10) |
Note: SD, standard deviation.
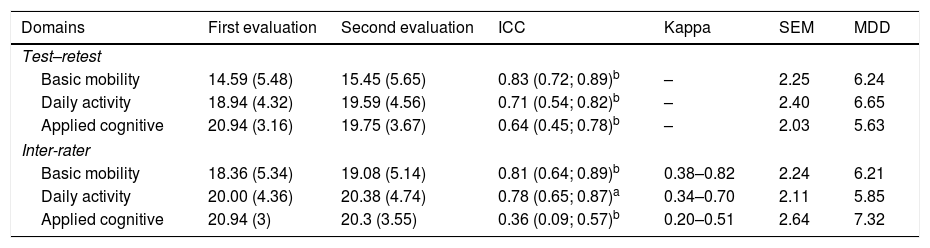
Basic mobility domain had the highest reliability with ICC2.1=0.83 (95% CI: 0.72, 0.89),followed by daily activity (ICC2.1=0.71, 95% CI: 0.54, 0.82) and applied cognitive (ICC2.1=0.64, 95% CI: 0.45, 0.78). The SEM ranged from 2.03 to 2.25 and the MDD from 5.63 to 6.55 (Table 4).
Test–retest (n=51) and inter-rater (n=50) reliability of the “6-clicks”.
| Domains | First evaluation | Second evaluation | ICC | Kappa | SEM | MDD |
|---|---|---|---|---|---|---|
| Test–retest | ||||||
| Basic mobility | 14.59 (5.48) | 15.45 (5.65) | 0.83 (0.72; 0.89)b | – | 2.25 | 6.24 |
| Daily activity | 18.94 (4.32) | 19.59 (4.56) | 0.71 (0.54; 0.82)b | – | 2.40 | 6.65 |
| Applied cognitive | 20.94 (3.16) | 19.75 (3.67) | 0.64 (0.45; 0.78)b | – | 2.03 | 5.63 |
| Inter-rater | ||||||
| Basic mobility | 18.36 (5.34) | 19.08 (5.14) | 0.81 (0.64; 0.89)b | 0.38–0.82 | 2.24 | 6.21 |
| Daily activity | 20.00 (4.36) | 20.38 (4.74) | 0.78 (0.65; 0.87)a | 0.34–0.70 | 2.11 | 5.85 |
| Applied cognitive | 20.94 (3) | 20.3 (3.55) | 0.36 (0.09; 0.57)b | 0.20–0.51 | 2.64 | 7.32 |
Note: Variables are presented in mean (standard deviation); kappa values show the lowest and highest values in each domain; ICC, intraclass correlation coefficient; SEM, standard error of measurement; MDD, minimum detectable difference.
Of the 65 companions assessed on the first day, only 30 were present for the second evaluation. Basic mobility domain showed an ICC2.1=0.82 (95% CI: 0.61, 0.91), daily activity ICC3.1=0.82 (95% CI: 0.65, 0.91) and applied cognitive ICC3.1=0.63 (95% CI; 0.35, 0.80).
Inter-rater reliabilityOf the 57 participants, three were discharged prior to the second evaluation, three refused to respond and one was absent from the infirmary on the second evaluation day. Participants were from cardiovascular (40%), oncology (20%), orthopedics and traumatology (8%), neurology (4%) and others (28%) wards. Additional information is shown in Table 3. The highest reliability was observed in the basic mobility domain ICC2.1=0.81 (95% CI; 0.64, 0.89), followed by daily activity ICC3.1=0.78 (95% CI; 0.64, 0.87) and applied cognitive ICC2.1=0.36 (95% CI; 0.09, 0.57). Basic mobility domain showed the highest kappa and the SEM ranged from 2.11 to 2.64, while the MDD ranged from 5.85 to 7.32 (Table 4).
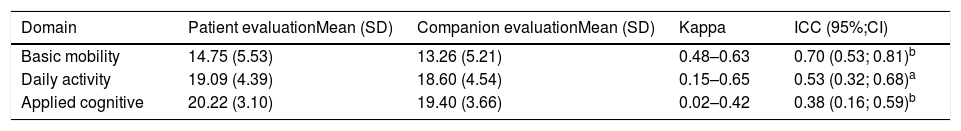
Patient/Companion agreementAll 65 patients and their respective companions answered the questions of the “6-clicks”. Most of the companions were women (73.8%) and other patients’ family members (86.1%); their mean age was 43.37 years (SD=15.13) and 43.1% had up to eight years of education. The highest agreements measured by kappa and ICC were from the domains of basic mobility, followed by daily activity and applied cognitive. These results are detailed in Table 5. The application of the questionnaires lasted on average 5min for each participant.
Results of the agreement tests conducted with the patients and/or companions.
| Domain | Patient evaluationMean (SD) | Companion evaluationMean (SD) | Kappa | ICC (95%;CI) |
|---|---|---|---|---|
| Basic mobility | 14.75 (5.53) | 13.26 (5.21) | 0.48–0.63 | 0.70 (0.53; 0.81)b |
| Daily activity | 19.09 (4.39) | 18.60 (4.54) | 0.15–0.65 | 0.53 (0.32; 0.68)a |
| Applied cognitive | 20.22 (3.10) | 19.40 (3.66) | 0.02–0.42 | 0.38 (0.16; 0.59)b |
Note: SD, standard deviation; kappa values show the lowest and highest values in each domain; ICC, intraclass correlation coefficient; CI, confidence interval.
For these calculations we considered the scores of the first evaluation day of all participants (n=181). The basic mobility domain showed the highest consistency (α=0.89). For the daily activity domain, the internal consistency was 0.81 and for the applied cognitive, 0.65. Despite the latest domain had internal consistency <0.70, deleting any of the items would not increase α.
DiscussionThe objective of this study was to translate, examine the cross-cultural adaptation of the “6-clicks” into Brazilian-Portuguese language and verify its measurement properties. The methodology followed recommendations from the authors of the instrument and other guidelines.8,19,20,29 During the process of translation and adaptation, none of the items were considered inappropriate for Brazilian culture and few items changed in relation to the original version. For example, the word “urinol” has different names across Brazilian regions, but we opted to use this term, since it is a more generic term and probably understood in every part of the country.20 In addition, the cognitive interviews and pre-tests helped verify the understanding of the questions by the participants with low level of education. The instrument was easily understood by professionals from the health care professionals, patients and their companions.
As for the measurement properties of the translated version, the test–retest reliability when the “6-clicks” was applied to the patients showed good magnitude for basic mobility and moderate magnitude for daily activity and applied cognitive. Although test–retest reliability was omitted in the original version, similar results were found in studies that evaluated this property for the complete bank of items of the AM-PAC,25 and for its Brazilian-Portuguese outpatient version.17 When the instrument was administered to the companions the test–retest reliability presented similar ICCs as to test–retest of the patients. This property is important for the Brazilian health care system since many patients remain hospitalized for long periods and are often assisted by the same professional.
The inter-rater reliability ICCs for the basic mobility and daily activity domains showed good results with ICC>0.75, similar to the test–retest indices found in this study and in its original version.18 However, the applied cognitive ICC was poor. The calculation of this ICC takes into account the variability among sample's subjects and, therefore, low variability reduces the coefficient value;26 in our study, this domain showed the lowest variability. This might explain the lower ICC for applied cognitive. Regarding the items, the kappa results varied from minimum to substantial for basic mobility and daily activity, showing similar results compared to the original version.18 This type of reliability was satisfactory for the domains basic mobility and daily activity, and less satisfactory for the applied cognitive domain.
In relation to the agreement between patients and companions, the basic mobility domain obtained the best results, followed by daily activity and applied cognitive. This type of agreement has been investigated in previous studies using the complete bank of AM-PAC,25,30,31 however, comparison of results is restricted due to the fact that these studies were conducted in a combination of inpatient and outpatient settings. During our study, some companions reported that they never observed certain activities because they were present only part of the day, and some items from the daily activity and applied cognitive domains, could be better observed during a specific moment such as bathing. The literature supports that subjective domains, as in the case of applied cognitive, tends to show lower agreement compared to those that are less subjective.25 The moderate magnitude of agreement in indices for basic mobility and daily activity suggests that patients and companions share information but not in such a way as to substitute one informant for the other.
The standard error of the measure and the minimum detectable difference are important indices for longitudinal follow-up, since the first indicates how much error in measurement are due to the scores,26,29 and the second, how much of the scores reflect a real difference or change, beyond the measurement error.26,29 The values found were close to those of the original “6-clicks” for the basic mobility and daily activity domains.18 Brazilian professionals and researchers should consider change in functionality with values above the minimum detectable difference, >6.24, between two consecutive measurements made by the same evaluator.
The internal consistency of the three domains was adequate. Our indices corroborate with the results of the original version of the “6-clicks” for basic mobility and daily activity.14 As both studies showed that the items in each domain are highly correlated, there is evidence to attest for the content validity of the “6-clicks” domains.29 To our knowledge, this is the first study to report the internal consistency of the “6-clicks” domain of applied cognitive. Considering the lower index obtained in this domain, further investigation of its content is suggested.
The “6-clicks” is a simple and fast measure, suitable to evaluate patients with various health conditions, unlike other disease-specific instruments10; its domains are independent and can be used according to the demands of the service. These characteristics should encourage the use of this standardized tool among professionals in hospital settings. It may also be a useful tool to help the development of rehabilitation databases, hospitalization strategies and continuity of care. In conjunction with the outpatient version of the AM-PAC, the “6-clicks” assists in defining treatment goals and evaluate functional outcomes of patients transferred to other services, since the scores from each version can be standardized and compared.10 As the Portuguese-Brazil version of the “6-clicks” becomes available, studies should use this instrument to evaluate its predictive value in patient discharge from hospital.
Limitations of the study include low variability of scores from the applied cognitive domain, which affected its reliability indices. Future studies should include participants of various cognitive levels in an attempt to investigate the consistency of information provided by items from the applied cognitive domain. Furthermore, monitoring of this domain in inpatients as well as its predictive value for hospital discharge will add relevant information. In addition, this study did not analyze the construct validity of the translated version of “6-clicks”, although this measurement property of the instrument has been examined by other studies.14,32
ConclusionThe instrument “6-clicks” for inpatients was translated and adapted to the Brazilian culture with satisfactory measurement properties. This instrument is useful to evaluate inpatients functionality, based on the patients’ own report and on their companions. Information on functionality evaluated by the “6-clicks” improves the use of inpatient rehabilitation data to enhance care and ensure the progress of patients’ treatment in the hospital setting and after discharge.
Conflicts of interestThe authors declare no conflicts of interest.
Thanks to the translation team: Fabiane Ribeiro Ferreira and Marina de Brito Brandão; to the professors that participated in the conceptual equivalence/items: Ciomara Maria Perez Nunes, Danielle Aparecida Gomes Pereira, Gisele de Cássia Gomes and Ligia de Loiola Cisneros; the students Déborah Ébert Fontes and Danielle Latini Gaudêncio who participated in the data collection; to Wendy Jane Coster for reviewing the translated version; to the support of RTNH and HC-UFMG; and the financial support from Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES).