Alterations in glenohumeral and scapulothoracic kinematics have been theorized to contribute to rotator cuff pathology by impacting the magnitude of the subacromial space.
ObjectiveThe purpose of this review is to summarize what is currently known about the relationship between shoulder kinematics and subacromial proximities.
ConclusionsA variety of methods have been used to quantify subacromial proximities including photographs, MR imaging, ultrasonography, and single- and bi-plane radiographs. Changes in glenohumeral and scapulothoracic kinematics are associated with changes in subacromial proximities. However, the magnitude and direction of a particular motion's impact on subacromial proximities often vary between studies, which likely reflects different methodologies and subject populations. Glenohumeral elevation angle has been consistently found to impact subacromial proximities. Plane of humeral elevation also impacts subacromial proximities but to a lesser degree than the elevation angle. The impact of decreased scapulothoracic upward rotation on subacromial proximities is not absolute, but instead depends on the angle of humerothoracic elevation. The effects of scapular dyskinesis and humeral and scapular axial rotations on subacromial proximities are less clear. Future research is needed to further investigate the relationship between kinematics and subacromial proximities using more homogenous groups, determine the extent to which compression and other factors contribute to rotator cuff pathology, and develop accurate and reliable clinical measures of shoulder motion.
The development of rotator cuff pathology is likely a complex process involving multiple mechanisms including mechanical tissue deformation, intrinsic tendon degeneration, and exposure/overuse.1,2 In particular, mechanical subacromial impingement – compression and/or abrasion of the rotator cuff tendons beneath the coracoacromial arch – has long been considered a mechanism for the development of pathology. Consequently, numerous studies have compared measures of the subacromial space between asymptomatic controls and participants diagnosed with “impingement syndrome”3–6 or rotator cuff tears.7,8 However, these studies often report small or no group differences, which has called into question the presumption of subacromial compression as a mechanism for rotator cuff pathology.
A major limitation of previous studies that have investigated the subacromial space in clinical populations is that individuals with “impingement syndrome” have been shown to exhibit a variety of shoulder movement impairments.9–17 Because the geometry of the subacromial space is defined by both kinematic and anatomic factors, classifying participants using this broad diagnostic label may not result in a homogenous group from which to identify the kinematic factors that influence the subacromial space. Instead, understanding first the relationship between kinematics and the subacromial space will help identify movement impairments that may be important in the development – and possibly prevention – of rotator cuff pathology.
The purpose of this review is to summarize what is currently known about the relationship between shoulder kinematics and subacromial proximities. First, the methods for quantifying subacromial space will be reviewed (e.g. ultrasonography, single- and bi-plane x-ray systems), including a discussion on accuracy, interpretation, and potential clinical translation. Second, the effect of shoulder kinematics on subacromial proximities will be reviewed focusing on studies that utilized distance-based measures (e.g. acromiohumeral distance, minimum distance), collectively termed “subacromial proximities”. Other approaches such as contact pressures18–20 and coracoacromial ligament displacements/strains21 will not be included as they involve special methodological considerations that challenge direct comparison. Further, studies that investigated the effect of muscular contraction or fatigue22–26 will not be included to avoid potentially confounding the relationship between shoulder kinematics and subacromial proximities. Finally, opportunities for future research will be outlined in an effort to better understand the mechanisms of rotator cuff pathology.
Methodological considerations for quantifying the subacromial spaceQuantifying the subacromial space involves two primary methodological considerations: (1) the imaging technique used to visualize the subacromial space, and (2) the metric used to quantify the subacromial space from the images.
Imaging techniquesMethods for visualizing subacromial relationships vary widely. Two-dimensional (2D) approaches include photographs,27 radiographs,28,29 MR imaging,30,31 and ultrasonography.4,26,32–36 However, these 2D methods introduce various sources of error when used to quantify 3D relationships. For example, distances measured from 2D radiographs are affected by magnification and projection errors. Additionally, distances measured from 2D ultrasound and MR images are dependent upon the scan orientation and image slice from which the measurements are made. Despite these limitations, 2D methods are commonly employed because the required equipment is often clinically available and data processing time is generally minimal.
Three-dimensional methods used to quantify subacromial proximities include kinematic tracking and modeling using either single-37 or bi-plane radiography,7,38,39 stereophotogrammetry,28 3D image reconstruction,40 or computational modeling.41,42 Although these 3D approaches provide higher accuracy, they often require custom equipment and data processing algorithms, and significant data processing time, which hinder broad use, clinical translation, and large sample sizes.
Metrics for quantifying the subacromial spaceIn addition to the imaging techniques, metrics for quantifying the subacromial space are also extremely varied. The most common metric has been the minimum distance, which quantifies the smallest distance between two structures. Generally speaking, the term “acromiohumeral distance” is used when the distance is measured between the acromion and the humerus,4,7,28,29,32–36,38–40,43,44 and the term “minimum distance” is used when the distance is measured between the acromion (with or without the coracoacromial ligament) and the humeral rotator cuff insertion37,38,45–47 or the tendon itself.31,41,42
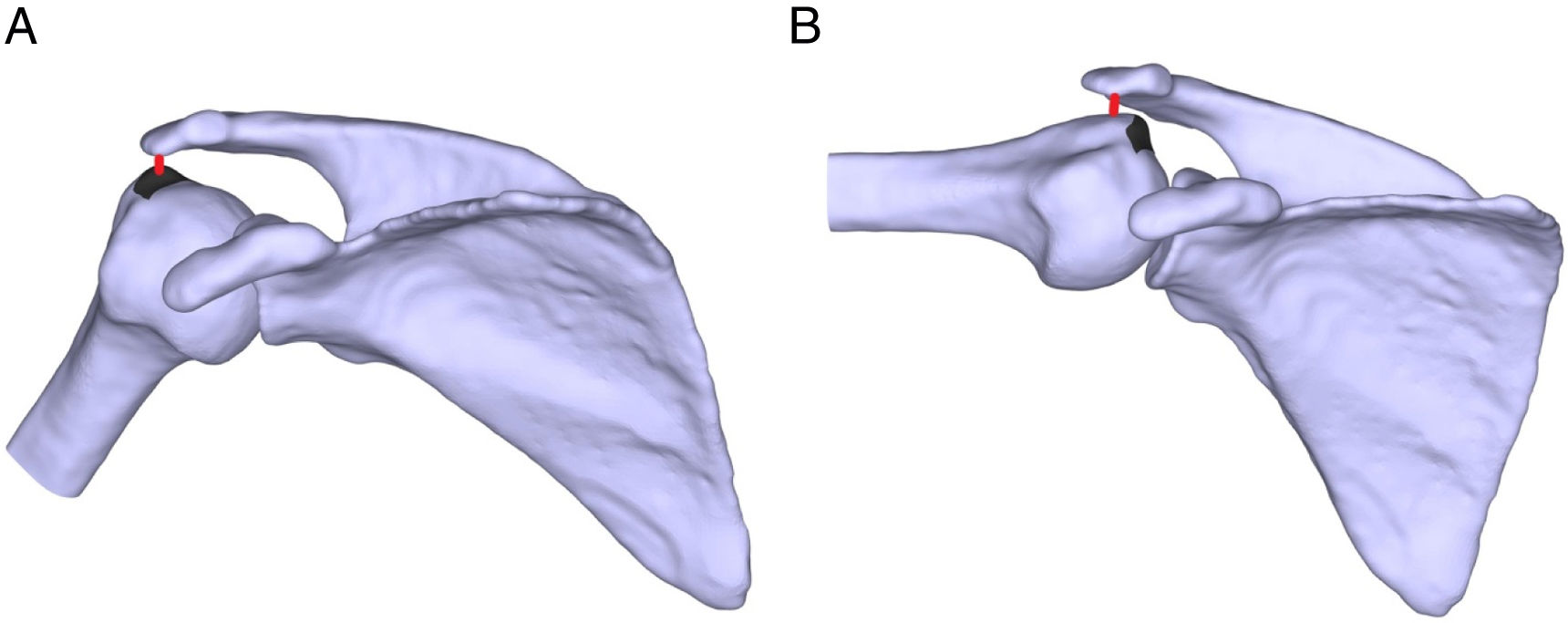
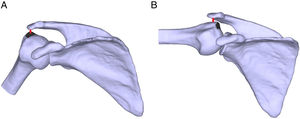
Although distance measures are by far the most common, they are limited in that they only describe the closest proximity between two surface points – a “worst case scenario” – and may therefore result in misleading conclusions. For example, some studies have shown that the acromiohumeral distance can continue to decrease even after the rotator cuff has already passed under the lateral acromion and is no longer in a position to be compressed (Fig. 1).28,38,40 Additionally, bone-to-bone distance measures can be challenging to interpret without information on the rotator cuff thickness, which averages approximately 5–7mm across individuals.37,48–50 However, high variability in tendon thickness exists between individuals and across portions of the tendon,50 making a single threshold difficult to generalize across a sample. As such, normalizing the minimum distance to a measure of the rotator cuff tendon thickness may aid data interpretation.37
The spatial relationship between the minimum distance vector (red) and the rotator cuff tendon insertion (black area on humeral surface). (A) At 30° of humerothoracic elevation, the minimum distance vector is located within the rotator cuff tendon insertion, which suggests the rotator cuff may be in a position to become compressed and/or abraded. (B) At 90° of humerothoracic elevation, the minimum distance vector is located lateral to the rotator cuff tendon insertion, which suggests the rotator cuff tendon has already cleared the lateral acromion and is no longer in a position to be compressed and/or abraded.
In addition to the limitations just described, distance measures alone may not provide a comprehensive assessment of subacromial space. Consequently, other geometric descriptions have been used. For example, the surface area of the rotator cuff tendons or humeral insertion site within immediate proximity to the acromion and/or coracoacromial ligament (i.e. subacromial proximity areas) has also been reported.28,37,41 Like minimum distance, however, subacromial proximity areas may be difficult to interpret without information on the rotator cuff thickness.
Ideally, subacromial proximities would be measured directly to the rotator cuff surface and also account for the incidence and amount of tissue deformation, if any. As such, some studies have used magnetic resonance (MR) imaging to visualize the rotator cuff in various shoulder positions.31,40 However, current MR technology limits investigation to static positions and within a limited range of motion. Other studies have reconstructed subject-specific three-dimensional (3D) models of the supraspinatus tendon from MR scans to perform computational modeling.41,42 However, this approach is extremely time consuming, making investigations with large samples impractical. A direct measure of soft tissue deformation requires a highly complex finite element model, which is challenging to develop and validate. However, some studies have estimated soft tissue deformation by quantifying the volume of the rotator cuff tendon that intersects with the coracoacromial arch during contact.41,42
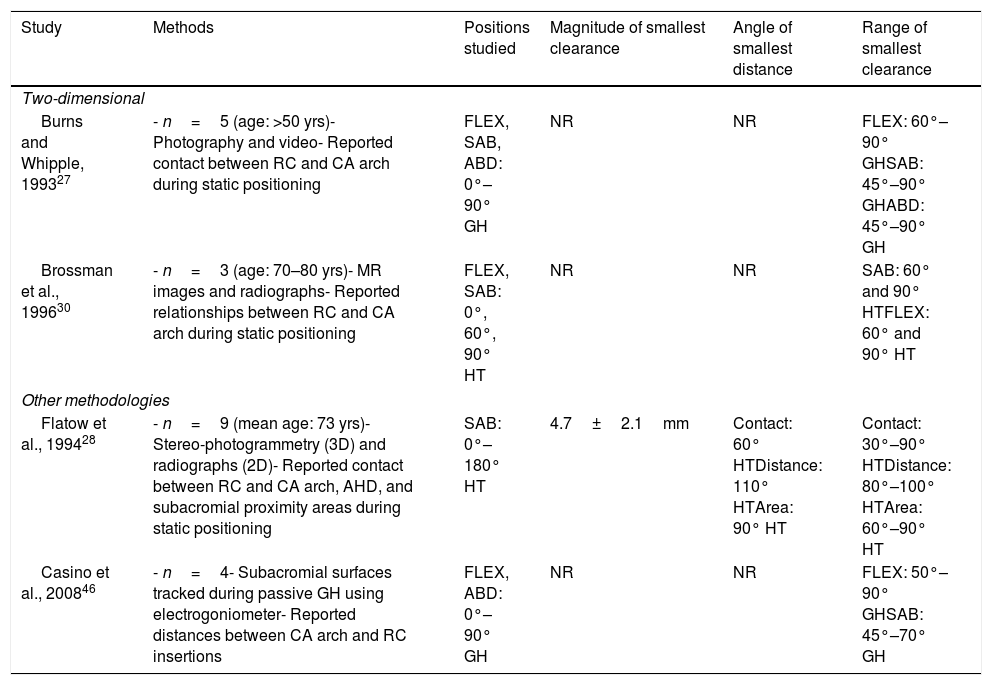
Effect of humeral elevation on subacromial proximitiesClinically, pain during arm raising is often presumed to be caused by subacromial rotator cuff compression. In particular, a “painful arc” of motion between 70° and 120° humerothoracic elevation is considered a hallmark sign of “impingement syndrome”.51 Therefore, numerous studies have investigated the impact of humeral elevation on subacromial proximities. For this review, these studies will be considered based on their in vitro (Table 1) or in vivo nature (Table 2).
Summary of studies investigating the effect of humeral elevation on subacromial proximities in cadaveric specimen.
| Study | Methods | Positions studied | Magnitude of smallest clearance | Angle of smallest distance | Range of smallest clearance |
|---|---|---|---|---|---|
| Two-dimensional | |||||
| Burns and Whipple, 199327 | - n=5 (age: >50 yrs)- Photography and video- Reported contact between RC and CA arch during static positioning | FLEX, SAB, ABD: 0°–90° GH | NR | NR | FLEX: 60°–90° GHSAB: 45°–90° GHABD: 45°–90° GH |
| Brossman et al., 199630 | - n=3 (age: 70–80 yrs)- MR images and radiographs- Reported relationships between RC and CA arch during static positioning | FLEX, SAB: 0°, 60°, 90° HT | NR | NR | SAB: 60° and 90° HTFLEX: 60° and 90° HT |
| Other methodologies | |||||
| Flatow et al., 199428 | - n=9 (mean age: 73 yrs)- Stereo-photogrammetry (3D) and radiographs (2D)- Reported contact between RC and CA arch, AHD, and subacromial proximity areas during static positioning | SAB: 0°–180° HT | 4.7±2.1mm | Contact: 60° HTDistance: 110° HTArea: 90° HT | Contact: 30°–90° HTDistance: 80°–100° HTArea: 60°–90° HT |
| Casino et al., 200846 | - n=4- Subacromial surfaces tracked during passive GH using electrogoniometer- Reported distances between CA arch and RC insertions | FLEX, ABD: 0°–90° GH | NR | NR | FLEX: 50°–90° GHSAB: 45°–70° GH |
Notes: Abbreviation: ABD, abduction; CA, coracoacromial; FLEX, flexion; GH, glenohumeral elevation; HT, humerothoracic elevation; NR, not reported; RC, rotator cuff; SAB, scapular plane abduction; yrs, years; 2D, two-dimensional, 3D, three-dimensional.
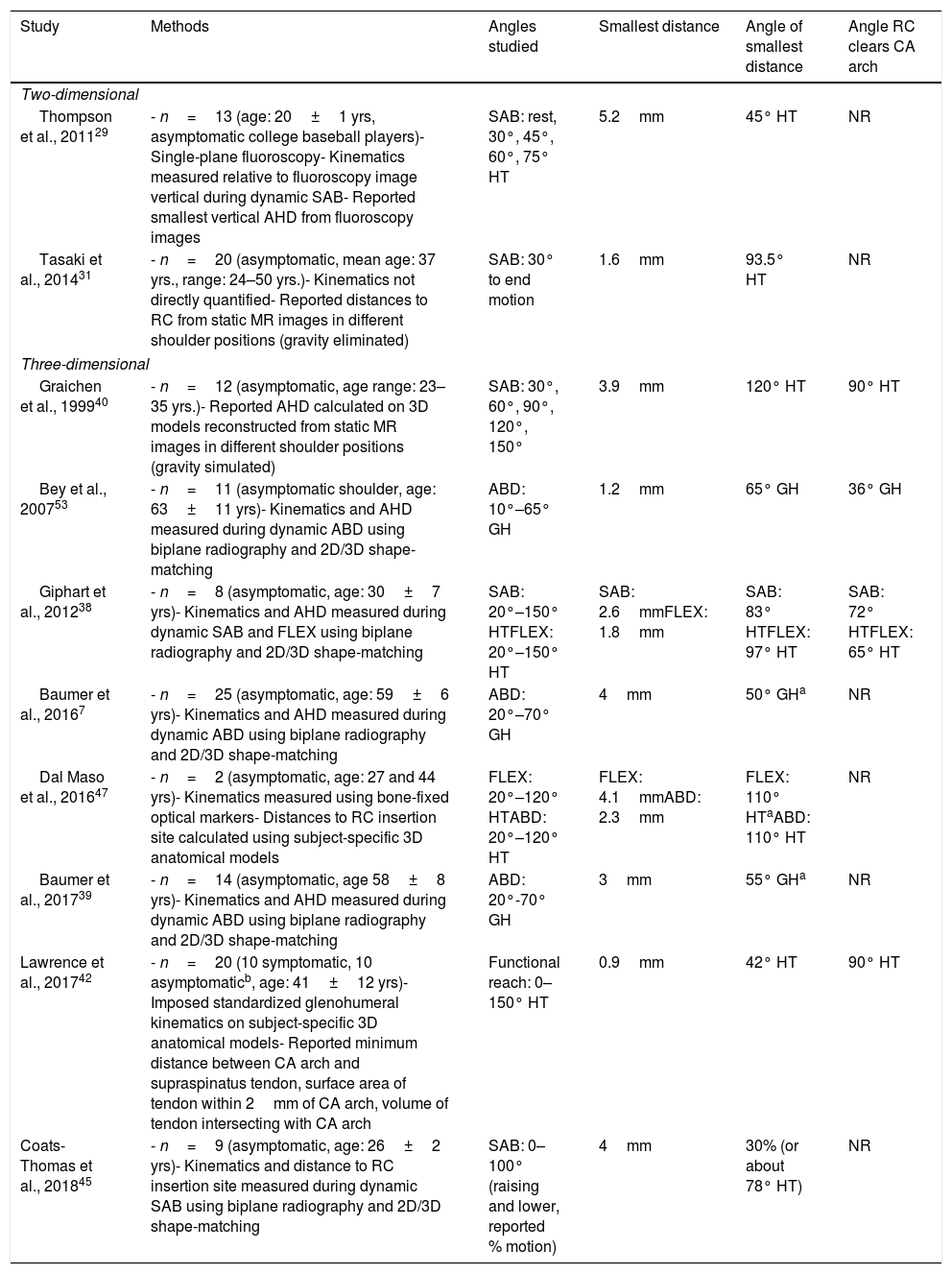
Summary of in vivo studies investigating the effect of humeral elevation on subacromial proximities.
| Study | Methods | Angles studied | Smallest distance | Angle of smallest distance | Angle RC clears CA arch |
|---|---|---|---|---|---|
| Two-dimensional | |||||
| Thompson et al., 201129 | - n=13 (age: 20±1 yrs, asymptomatic college baseball players)- Single-plane fluoroscopy- Kinematics measured relative to fluoroscopy image vertical during dynamic SAB- Reported smallest vertical AHD from fluoroscopy images | SAB: rest, 30°, 45°, 60°, 75° HT | 5.2mm | 45° HT | NR |
| Tasaki et al., 201431 | - n=20 (asymptomatic, mean age: 37 yrs., range: 24–50 yrs.)- Kinematics not directly quantified- Reported distances to RC from static MR images in different shoulder positions (gravity eliminated) | SAB: 30° to end motion | 1.6mm | 93.5° HT | NR |
| Three-dimensional | |||||
| Graichen et al., 199940 | - n=12 (asymptomatic, age range: 23–35 yrs.)- Reported AHD calculated on 3D models reconstructed from static MR images in different shoulder positions (gravity simulated) | SAB: 30°, 60°, 90°, 120°, 150° | 3.9mm | 120° HT | 90° HT |
| Bey et al., 200753 | - n=11 (asymptomatic shoulder, age: 63±11 yrs)- Kinematics and AHD measured during dynamic ABD using biplane radiography and 2D/3D shape-matching | ABD: 10°–65° GH | 1.2mm | 65° GH | 36° GH |
| Giphart et al., 201238 | - n=8 (asymptomatic, age: 30±7 yrs)- Kinematics and AHD measured during dynamic SAB and FLEX using biplane radiography and 2D/3D shape-matching | SAB: 20°–150° HTFLEX: 20°–150° HT | SAB: 2.6mmFLEX: 1.8mm | SAB: 83° HTFLEX: 97° HT | SAB: 72° HTFLEX: 65° HT |
| Baumer et al., 20167 | - n=25 (asymptomatic, age: 59±6 yrs)- Kinematics and AHD measured during dynamic ABD using biplane radiography and 2D/3D shape-matching | ABD: 20°–70° GH | 4mm | 50° GHa | NR |
| Dal Maso et al., 201647 | - n=2 (asymptomatic, age: 27 and 44 yrs)- Kinematics measured using bone-fixed optical markers- Distances to RC insertion site calculated using subject-specific 3D anatomical models | FLEX: 20°–120° HTABD: 20°–120° HT | FLEX: 4.1mmABD: 2.3mm | FLEX: 110° HTaABD: 110° HT | NR |
| Baumer et al., 201739 | - n=14 (asymptomatic, age 58±8 yrs)- Kinematics and AHD measured during dynamic ABD using biplane radiography and 2D/3D shape-matching | ABD: 20°-70° GH | 3mm | 55° GHa | NR |
| Lawrence et al., 201742 | - n=20 (10 symptomatic, 10 asymptomaticb, age: 41±12 yrs)- Imposed standardized glenohumeral kinematics on subject-specific 3D anatomical models- Reported minimum distance between CA arch and supraspinatus tendon, surface area of tendon within 2mm of CA arch, volume of tendon intersecting with CA arch | Functional reach: 0–150° HT | 0.9mm | 42° HT | 90° HT |
| Coats-Thomas et al., 201845 | - n=9 (asymptomatic, age: 26±2 yrs)- Kinematics and distance to RC insertion site measured during dynamic SAB using biplane radiography and 2D/3D shape-matching | SAB: 0–100° (raising and lower, reported % motion) | 4mm | 30% (or about 78° HT) | NR |
Notes: Abbreviation: ABD, abduction; AHD, acromiohumeral distance; CA, coracoacromial; FLEX, flexion; GH, glenohumeral elevation; HT, humerothoracic elevation; MR, magnetic resonance; NR, not reported; RC, rotator cuff; SAB, scapular plane abduction; yrs, years; 2D, two-dimensional; 3D, three-dimensional.
Before the advancement of imaging technologies, subacromial proximities during shoulder motion were primarily investigated using cadaveric shoulder specimens (Table 1). In general, early in vitro studies concluded that the rotator cuff was closest to the coracoacromial arch between approximately 45°–90° glenohumeral elevation.27,28,30,46 Assuming a 2:1 scapulohumeral rhythm,52 this range of glenohumeral elevation corresponds to approximately 68°–135° of humerothoracic elevation. Consequently, these early findings supported the clinical theory that pain during mid-range may be due to subacromial rotator cuff compression. However, the experimental nature of these studies hinders interpretation relative to in vivo conditions where muscle contraction and multi-axial motion occurs. Further, the studies generally used 2D methodologies, which are subject to errors as previously described.
Despite the limitations of early cadaveric studies, two critical advancements were made by Flatow et al.28 that have helped inform future studies. First, the researchers quantified both acromiohumeral distance and subacromial proximity area. The results of the distance measures suggested that subacromial contact occurred most frequently between 30° and 90° humeral elevation; however, proximity areas were greatest between 60° and 120° humeral elevation. These differences suggest a simple distance measure may not fully describe subacromial relationships. Second, the researchers observed that beyond 90° humeral elevation, the subacromial space “no longer accommodated” the rotator cuff tendons, which highlights the critical importance of considering tendon location when interpreting subacromial proximities.
In vivo studiesIn vivo studies investigating subacromial proximities during humeral elevation generally report the acromiohumeral distance progressively decreases with increasing humeral elevation until a minimum occurs between approximately 75°–120° of humerothoracic elevation before increasing again at higher angles (Table 2). However, most of these studies quantified acromiohumeral distances,7,29,38,39,45,47,53 which hinders clinical interpretation.
Not surprisingly, studies that accounted for the location of the humeral rotator cuff insertion found that the smallest minimum distance occurred at a lower angle of humeral elevation. For example, Giphart et al.38 reported the rotator cuff insertion cleared the acromion in asymptomatic participants by an average of 65°–72° humerothoracic elevation, depending on the plane of humeral elevation.38 Likewise, Coats-Thomas et al. reported the rotator cuff insertion cleared the acromion in asymptomatic participants by approximately 78° humerothoracic elevation (Fig. 1).45 Furthermore, when the minimum distance is measured three-dimensionally and directly to the supraspinatus, the tendon appears to remain in close proximity between 0° and 60° humerothoracic elevation (minimum distance <1.2mm), and is closest (average: 0.9mm) at an average of 42° humerothoracic elevation.42 Therefore, it appears the humeral rotator cuff insertion is closest to the coracoacromial arch at a much lower humeral elevation angle than what has been traditionally believed.
Interestingly, the two studies that quantified the minimum distance directly to the rotator cuff tendons observed the tendons came into contact (i.e. minimum distance=0mm) with the coracoacromial arch even in asymptomatic individuals. For example, Tasaki et al. reported contact in 25% of asymptomatic participants during static arm positions.31 Likewise, Lawrence et al. reported contact in 40% of asymptomatic participants during a simulated functional reaching task.42 However, given the cross-sectional nature of these studies, it remains unclear whether participants remained asymptomatic long-term. It is also important to consider that contact without substantive compression may not be problematic with a healthy subacromial bursa minimizing frictional forces.
Taken together, the results of in vitro and in vivo studies suggest humeral elevation impacts subacromial distances. Studies measuring distances directly to the rotator cuff tendon or its humeral insertion38,42,45 typically report the smallest proximities occur at a lower angle of humeral elevation than those reporting acromiohumeral distances.7,39,40,53 The smallest distance between the rotator cuff tendon insertion and coracoacromial arch occurs between 40° and 75° of humerothoracic elevation.31,38,42,45 In most individuals, the rotator cuff has passed medially under the acromion and is no longer in a position to be compressed by 90° of humerothoracic elevation.28,38,40,42 Furthermore, contact between the rotator cuff and coracoacromial arch may occur even in asymptomatic individuals.
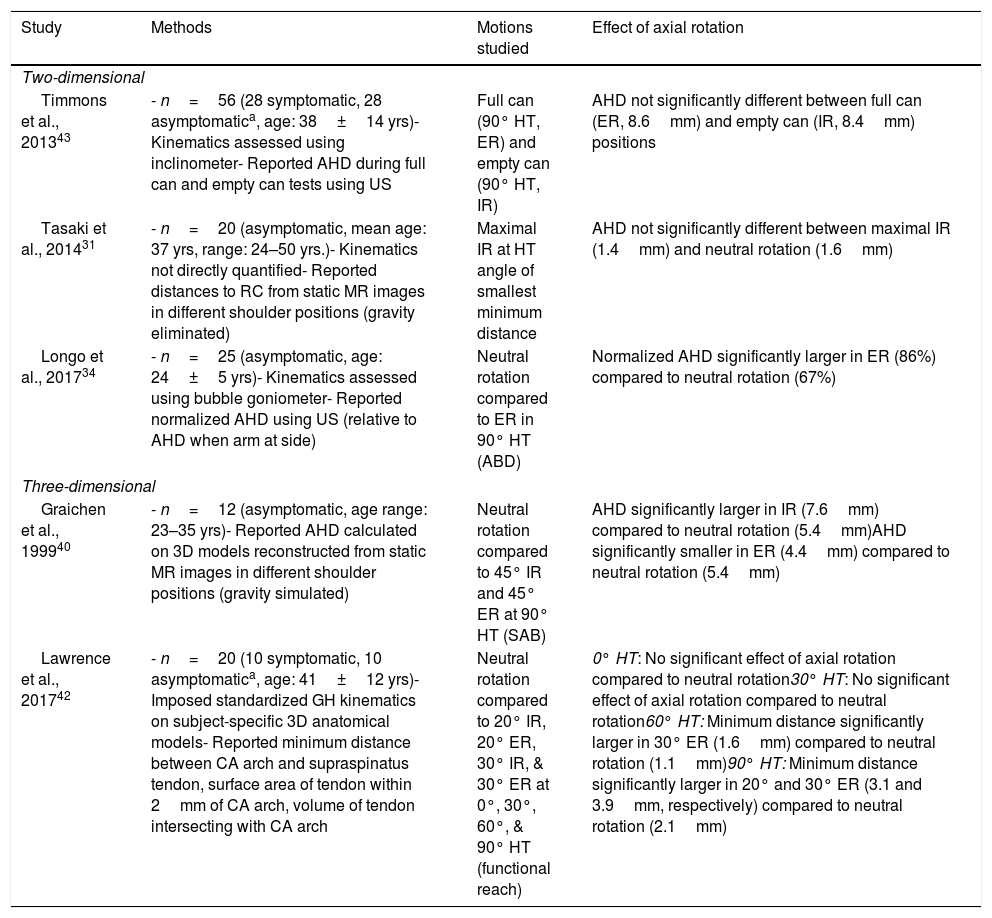
Effect of humeral axial rotation on subacromial proximitiesGlenohumeral external rotation is frequently hypothesized to increase the subacromial space by moving the humeral rotator cuff insertion away from the acromion.28,54,55 Conversely, internal rotation is thought to decrease the subacromial space. As such, several studies have investigated the effect of humeral axial rotation on subacromial proximities (Table 3). In general, the results of these studies are inconsistent. For example, despite quantifying acromiohumeral distances in the same position (axial rotation in 90° of humerothoracic elevation), Longo et al. reported humeral external rotation significantly increased the acromiohumeral distance,34 while Graichen et al.40 reported the distance significantly decreased,40 and Timmons et al. reported no significant change.43 Additionally, humeral internal rotation has been shown to increase40 and have no effect31,42 on acromiohumeral distances.
Summary of in vivo studies investigating the effect of humeral axial rotation on subacromial proximities.
| Study | Methods | Motions studied | Effect of axial rotation |
|---|---|---|---|
| Two-dimensional | |||
| Timmons et al., 201343 | - n=56 (28 symptomatic, 28 asymptomatica, age: 38±14 yrs)- Kinematics assessed using inclinometer- Reported AHD during full can and empty can tests using US | Full can (90° HT, ER) and empty can (90° HT, IR) | AHD not significantly different between full can (ER, 8.6mm) and empty can (IR, 8.4mm) positions |
| Tasaki et al., 201431 | - n=20 (asymptomatic, mean age: 37 yrs, range: 24–50 yrs.)- Kinematics not directly quantified- Reported distances to RC from static MR images in different shoulder positions (gravity eliminated) | Maximal IR at HT angle of smallest minimum distance | AHD not significantly different between maximal IR (1.4mm) and neutral rotation (1.6mm) |
| Longo et al., 201734 | - n=25 (asymptomatic, age: 24±5 yrs)- Kinematics assessed using bubble goniometer- Reported normalized AHD using US (relative to AHD when arm at side) | Neutral rotation compared to ER in 90° HT (ABD) | Normalized AHD significantly larger in ER (86%) compared to neutral rotation (67%) |
| Three-dimensional | |||
| Graichen et al., 199940 | - n=12 (asymptomatic, age range: 23–35 yrs)- Reported AHD calculated on 3D models reconstructed from static MR images in different shoulder positions (gravity simulated) | Neutral rotation compared to 45° IR and 45° ER at 90° HT (SAB) | AHD significantly larger in IR (7.6mm) compared to neutral rotation (5.4mm)AHD significantly smaller in ER (4.4mm) compared to neutral rotation (5.4mm) |
| Lawrence et al., 201742 | - n=20 (10 symptomatic, 10 asymptomatica, age: 41±12 yrs)- Imposed standardized GH kinematics on subject-specific 3D anatomical models- Reported minimum distance between CA arch and supraspinatus tendon, surface area of tendon within 2mm of CA arch, volume of tendon intersecting with CA arch | Neutral rotation compared to 20° IR, 20° ER, 30° IR, & 30° ER at 0°, 30°, 60°, & 90° HT (functional reach) | 0° HT: No significant effect of axial rotation compared to neutral rotation30° HT: No significant effect of axial rotation compared to neutral rotation60° HT: Minimum distance significantly larger in 30° ER (1.6mm) compared to neutral rotation (1.1mm)90° HT: Minimum distance significantly larger in 20° and 30° ER (3.1 and 3.9mm, respectively) compared to neutral rotation (2.1mm) |
Notes: Abbreviations: ABD, abduction; AHD, acromiohumeral distance; CA, coracoacromial; ER, external rotation; GH, glenohumeral; HT, humerothoracic elevation; IR, internal rotation; MR, magnetic resonance; RC, rotator cuff; SAB, scapular plane abduction; US, ultrasound; yrs, years; 3D, three-dimensional.
Several factors may help explain these conflicting results. First, quantifying the subacromial space with the arm positioned in 90° of humerothoracic elevation, particularly using ultrasound, is challenging given the rotator cuff insertion moves medially under the acromion by this angle and sound waves cannot penetrate bone to visualize the rotator cuff. Second, the ability to control both the magnitude of axial rotation and other concurrent shoulder motions (e.g. scapular orientation) is challenging, which may have confounded the comparison. Third, the results of Tasaki et al.,31 which found no impact of internal rotation on acromiohumeral distances, may be affected by a floor effect. Specifically, the effect of axial rotation was assessed in the position of humeral elevation at which the acromiohumeral distance was smallest. Therefore, the impact of axial rotation on acromiohumeral distances may be underestimated.
Later work sought to understand the effect of humeral retroversion on subacromial proximities across a simulated functional reaching task.42 Because retroversion describes anatomic rotation about the humeral long axis, the results of this study can be used to infer the effect of axial rotation. Interestingly, the study found that the effect of humeral axial rotation on subacromial distances may depend on the humerothoracic elevation angle.42 Specifically, at 0° and 30° of humerothoracic elevation, humeral axial rotation did not significantly impact the minimum distance between the coracoacromial arch and supraspinatus tendon. Instead, axial rotation only appeared to shift which aspect of the tendon surface was in closest proximity to the coracoacromial arch. However, at 60° and 90° of humerothoracic elevation, external rotation significantly increased the minimum distance by rotating the supraspinatus tendon further away from the coracoacromial arch. Although statistically significant, the clinical meaningfulness of this finding is unclear because the supraspinatus tendon has already cleared the lateral acromion in most individuals (Fig. 1).28,38,40,42
As was the case for humeral elevation, interpreting minimum distances during axial rotation without accounting for the soft tissue may be misleading. For example, Graichen et al.40 reported that humeral external rotation significantly reduced the acromiohumeral distance.40 However, the minimum distance vector passed through the supraspinatus tendon in only 42% of participants compared to 100% of participants during internal rotation, which was found to significantly increase the acromiohumeral distance. This finding further suggests acromiohumeral distance measures may need to be interpreted with caution.
Taken together, the results of these studies suggest the impact of humeral axial rotation on subacromial distances remains unclear. Ultimately, axial rotation may impact which aspect of the rotator cuff tendons are in closer proximity more so than an overall change in proximity measures.
Effect of humeral plane of elevation on subacromial proximitiesOnly one study has directly compared the effect of humeral plane of elevation on subacromial proximities (Table 4).41 Glenohumeral elevation was imposed on subject-specific 3D anatomical models across three glenohumeral planes, which were chosen to represent flexion, scapular plane abduction, and abduction based on average data from symptomatic individuals.56 The researchers found differences between planes of elevation when the arm was at the side (i.e. 0° glenohumeral elevation relative an anterior/posterior axis). In this position, glenohumeral plane of elevation (i.e. rotation about a medial/lateral axis) moves the elbow anterior or posterior to the plane of the scapula. Specifically, flexion brings the elbow anterior to the scapular plane, while abduction brings the elbow posterior to the scapular plane. When the elbow was in line with (i.e. scapular plane) or posterior to (i.e. abduction) the scapular plane, the supraspinatus tendon was significantly closer to the coracoacromial arch compared to when the elbow was anterior to the scapular plane (i.e. flexion). Above approximately 70° of glenohumeral elevation, however, the supraspinatus tendon was significantly closer to the coracoacromial arch in the sagittal plane than in the coronal or scapular planes. Similar findings were also reported for subacromial proximity area and the volume of intersection between the supraspinatus tendon and coracoacromial arch. Compared to glenohumeral elevation, however, altering glenohumeral plane of elevation had a smaller impact on subacromial proximities.
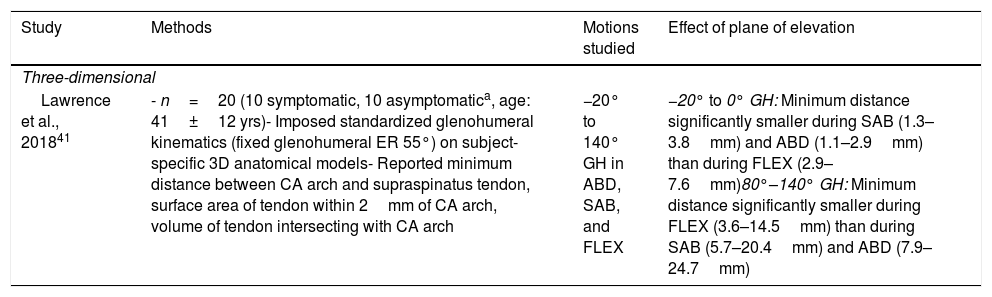
Summary of in vivo studies investigating effect of humeral plane of elevation on subacromial proximities.
| Study | Methods | Motions studied | Effect of plane of elevation |
|---|---|---|---|
| Three-dimensional | |||
| Lawrence et al., 201841 | - n=20 (10 symptomatic, 10 asymptomatica, age: 41±12 yrs)- Imposed standardized glenohumeral kinematics (fixed glenohumeral ER 55°) on subject-specific 3D anatomical models- Reported minimum distance between CA arch and supraspinatus tendon, surface area of tendon within 2mm of CA arch, volume of tendon intersecting with CA arch | −20° to 140° GH in ABD, SAB, and FLEX | −20° to 0° GH: Minimum distance significantly smaller during SAB (1.3–3.8mm) and ABD (1.1–2.9mm) than during FLEX (2.9–7.6mm)80°–140° GH: Minimum distance significantly smaller during FLEX (3.6–14.5mm) than during SAB (5.7–20.4mm) and ABD (7.9–24.7mm) |
Notes: Abbreviations: ABD, abduction; CA, coracoacromial; FLEX, flexion; GH, glenohumeral elevation; HT, humerothoracic elevation; MR, magnetic resonance; NR, not reported; RC, rotator cuff; SAB, scapular plane abduction; yrs, years; 3D, three-dimensional.
Clinicians have long postulated that scapular movement impairments – specifically decreased upward rotation, posterior tilt, and external rotation – reduce the subacromial space.1,2,11,12,57 However, relatively few studies have studied the impact scapular kinematics on the subacromial space (Table 5). In general, these studies can be classified as those that investigated dyskinesis and associated tests, which involve multi-axial alterations in scapular motion,4,32,33 or alterations in specific scapulothoracic kinematics.35–37,44
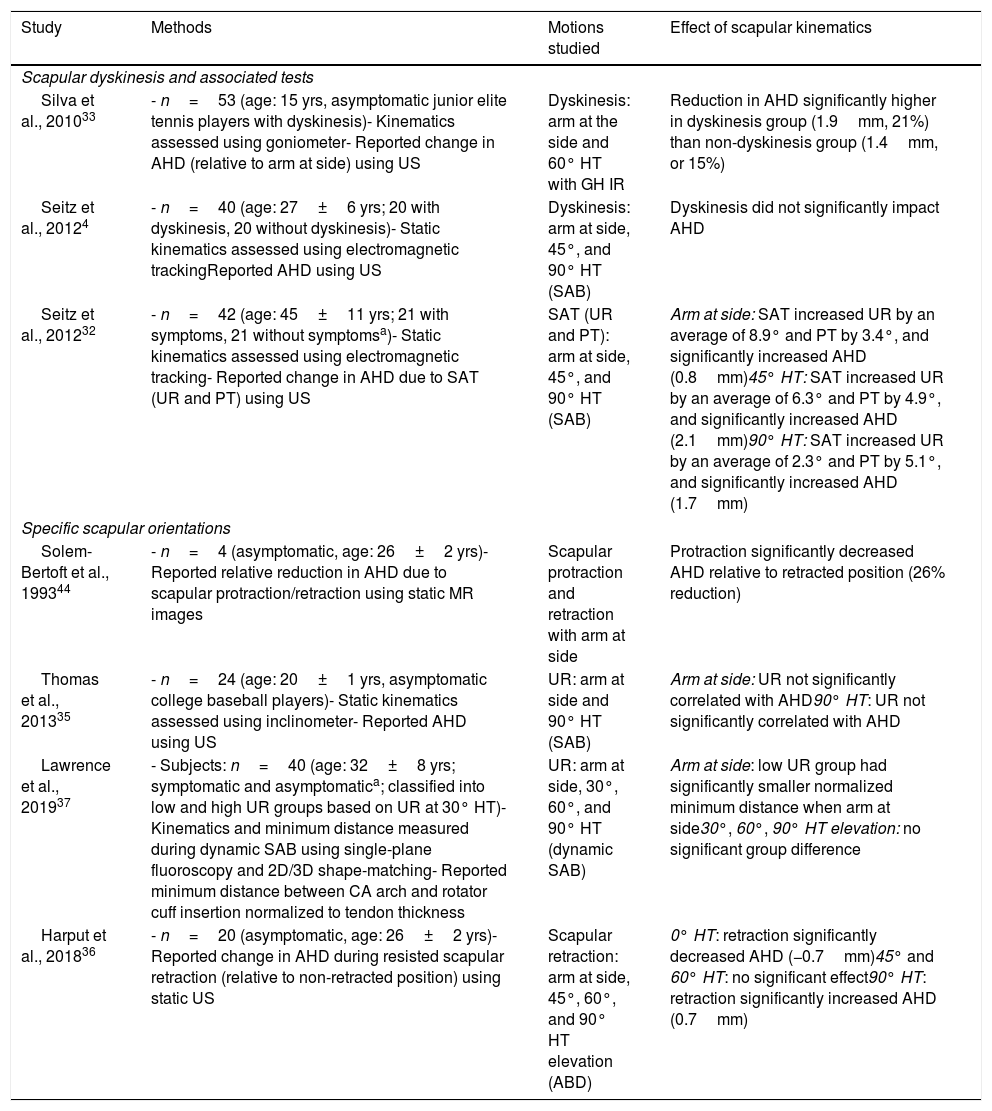
Summary of studies investigating effect of scapulothoracic kinematics on subacromial proximities.
| Study | Methods | Motions studied | Effect of scapular kinematics |
|---|---|---|---|
| Scapular dyskinesis and associated tests | |||
| Silva et al., 201033 | - n=53 (age: 15 yrs, asymptomatic junior elite tennis players with dyskinesis)- Kinematics assessed using goniometer- Reported change in AHD (relative to arm at side) using US | Dyskinesis: arm at the side and 60° HT with GH IR | Reduction in AHD significantly higher in dyskinesis group (1.9mm, 21%) than non-dyskinesis group (1.4mm, or 15%) |
| Seitz et al., 20124 | - n=40 (age: 27±6 yrs; 20 with dyskinesis, 20 without dyskinesis)- Static kinematics assessed using electromagnetic trackingReported AHD using US | Dyskinesis: arm at side, 45°, and 90° HT (SAB) | Dyskinesis did not significantly impact AHD |
| Seitz et al., 201232 | - n=42 (age: 45±11 yrs; 21 with symptoms, 21 without symptomsa)- Static kinematics assessed using electromagnetic tracking- Reported change in AHD due to SAT (UR and PT) using US | SAT (UR and PT): arm at side, 45°, and 90° HT (SAB) | Arm at side: SAT increased UR by an average of 8.9° and PT by 3.4°, and significantly increased AHD (0.8mm)45° HT: SAT increased UR by an average of 6.3° and PT by 4.9°, and significantly increased AHD (2.1mm)90° HT: SAT increased UR by an average of 2.3° and PT by 5.1°, and significantly increased AHD (1.7mm) |
| Specific scapular orientations | |||
| Solem-Bertoft et al., 199344 | - n=4 (asymptomatic, age: 26±2 yrs)- Reported relative reduction in AHD due to scapular protraction/retraction using static MR images | Scapular protraction and retraction with arm at side | Protraction significantly decreased AHD relative to retracted position (26% reduction) |
| Thomas et al., 201335 | - n=24 (age: 20±1 yrs, asymptomatic college baseball players)- Static kinematics assessed using inclinometer- Reported AHD using US | UR: arm at side and 90° HT (SAB) | Arm at side: UR not significantly correlated with AHD90° HT: UR not significantly correlated with AHD |
| Lawrence et al., 201937 | - Subjects: n=40 (age: 32±8 yrs; symptomatic and asymptomatica; classified into low and high UR groups based on UR at 30° HT)- Kinematics and minimum distance measured during dynamic SAB using single-plane fluoroscopy and 2D/3D shape-matching- Reported minimum distance between CA arch and rotator cuff insertion normalized to tendon thickness | UR: arm at side, 30°, 60°, and 90° HT (dynamic SAB) | Arm at side: low UR group had significantly smaller normalized minimum distance when arm at side30°, 60°, 90° HT elevation: no significant group difference |
| Harput et al., 201836 | - n=20 (asymptomatic, age: 26±2 yrs)- Reported change in AHD during resisted scapular retraction (relative to non-retracted position) using static US | Scapular retraction: arm at side, 45°, 60°, and 90° HT elevation (ABD) | 0° HT: retraction significantly decreased AHD (−0.7mm)45° and 60° HT: no significant effect90° HT: retraction significantly increased AHD (0.7mm) |
Notes: Abbreviations: ABD, abduction; AHD, acromiohumeral distance; CA, coracoacromial; ER, external rotation; GH, glenohumeral; HT, humerothoracic elevation; MR, magnetic resonance; RC, rotator cuff; SAB, scapular plane abduction; SAT, scapular assistance test; UR, upward rotation; US, ultrasound; yrs, years; 2D, two-dimensional; 3D, three-dimensional.
Multi-axial alterations in scapular orientations have been investigated in individuals with dyskinesis or during a scapular assistance test. Clinically, the term “dyskinesis” is used to describe many forms of altered scapular movement (e.g. increased internal rotation, decreased posterior tilt, rapid downward rotation), which may occur individually or in combination.58 To date, two studies have investigated the impact of scapular dyskinesis on subacromial proximities. Silva et al.33 used ultrasound to measure acromiohumeral distance in junior elite tennis players with and without scapular dyskinesis. Specifically, the researchers measured the change in acromiohumeral distance between two static positions: internal rotation at the side and with the arm elevated to 60° humerothoracic elevation. The researchers found that, on average, individuals with dyskinesis experienced a higher reduction in acromiohumeral distance than individuals without dyskinesis (dyskinesis: 1.9mm or 21%; without dyskinesis: 1.4mm or 16%).33 However, a similar study, by Seitz et al., reported the presence of dyskinesis in asymptomatic participants did not significantly impact the acromiohumeral distance at any angle of humerothoracic elevation tested.4
The seemingly disparate results between the studies by Silva et al.33 and Seitz et al.4 may be due to the use of “dyskinesis” as an inclusion criterion. Because the term describes many forms of altered scapular movement,58 it is likely the dyskinesis groups were heterogeneous in nature, which may have confounded the analyses. Classifying based on a specific scapular movement abnormality may help improve the precision with which the relationship between scapular kinematics and subacromial proximities can be identified. Furthermore, scapular dyskinesis is a movement impairment diagnosed during dynamic motion58 and ultrasound-based measures of acromiohumeral distances require static test conditions. Therefore, it is possible the dyskinetic movement impairments were not adequately reproduced and may have contributed to the inconsistent findings between studies.
The scapular assistance test has also been used to investigate the effects of scapulothoracic kinematics on subacromial distances. The test assesses the effect of altering scapulothoracic kinematics on patient symptoms by manually facilitating upward rotation, posterior tilt, and/or external rotation.59 A positive scapular assistance test occurs when the patient's symptoms are reduced with manual facilitation, presumably from increasing subacromial space. Seitz et al.32 used ultrasound to determine the extent to which the scapular assistance test impacted scapulothoracic kinematics and subacromial proximities in symptomatic and asymptomatic individuals at three static arm positions (arm at side, and 45° and 90° humerothoracic elevation). The researchers reported the maneuver increased posterior tilt at all angles (mean: 4.5°) and upward rotation with the arm at the side and at 45° humerothoracic elevation (mean: 8.9° and 6.3°, respectively). These changes corresponded with a significant increase in acromiohumeral distance at 45° and at 90° humerothoracic elevation (2.1mm and 1.7mm, respectively). Ultimately, the results of this study suggest acromiohumeral distance can be increased by facilitating scapulothoracic upward rotation and posterior tilt in combination. However, the relationship between specific scapulothoracic rotations and subacromial proximities remains unclear. Although isolated scapulothoracic rotations do not occur physiologically, they often form the basis of movement-based diagnostic classifications (e.g. insufficient scapular upward rotation).60–62 Therefore, understanding the impact of specific scapulothoracic rotations on subacromial space is important to understand the relationship between motion and potential mechanisms of pathology.
Scapulothoracic kinematicsFew studies have investigated the relationship between specific scapulothoracic motions and subacromial proximities. Initial work by Thomas et al.35 suggested acromiohumeral distance (measured via ultrasound) was not significantly correlated with scapular upward rotation angular position when the arm was at the side or at 90° humerothoracic elevation in asymptomatic college baseball players. Recent work,37 however, suggests the relationship between scapulothoracic upward rotation and subacromial proximities is not absolute, but depends on the angle of humerothoracic elevation. The study quantified shoulder kinematics and minimum distance (normalized to the rotator cuff tendon thickness) in 40 symptomatic and asymptomatic individuals during dynamic scapular plane abduction. Instead of identifying groups based on symptom status, participants were classified into the “low” or “high” scapular upward rotation groups based on their kinematics at 30° humerothoracic elevation. Using this approach, the average normalized minimum distance was significantly smaller in the low upward rotation group (210%) compared the high upward rotation group (245%) when the arm was at the side. However, at 90° humerothoracic elevation, the average normalized minimum distance tended to be larger (but not statistically significant) for the low upward rotation group compared to the high upward rotation group. Ultimately, these findings suggest that decreased upward rotation shifts the range of smallest proximities to lower angles of humerothoracic elevation.
Alterations in shoulder girdle protraction/retraction have also been theorized to impact subacromial proximities. The results of an early study by Solem-Bertoff et al.44 using 2D MR images lend initial support to this theory. Specifically, protracting the shoulder with the arm at the side resulted in an average reduction in acromiohumeral distance of 26% in asymptomatic participants. However, the results of a more recent ultrasound study by Harput et al.36 challenge these findings. Although significant changes in acromiohumeral distance were found (0.7mm), the authors concluded that active scapular retraction had minimal to no meaningful influence on acromiohumeral distance during shoulder abduction in young asymptomatic individuals.
Subacromial proximities appear to be mostly affected by alterations in scapulothoracic upward rotation with or without concurrent alterations in posterior tilt.4,37 However, the effect of scapulothoracic kinematics on subacromial proximities may depend on the angle of humerothoracic elevation. Specifically, decreased scapulothoracic upward rotation shifts the range of closest proximities to lower angles of humerothoracic elevation.37 The effect of scapular dyskinesis and shoulder girdle protraction/retraction remains unclear. Future research is needed to more rigorously determine the impact of altered scapular kinematics on subacromial proximities and their relationship with tissue pathology.
Opportunities for future researchAlthough the studies examined herein have contributed much to our understanding of the relationship between shoulder kinematics and subacromial proximities, many questions remain. First, it remains unclear the extent to which simple minimum distance measures effectively describe subacromial relationships. Future research would benefit from comparing these simple metrics to more complex, multi-dimensional measures of the subacromial space using highly accurate 3D motion tracking and anatomical modeling.
Second, despite the nearly universal acceptance of the mechanical compression theory as a mechanism for rotator cuff pathology, the extent to which compression actually results in pathology remains unclear. Experimental animal studies provide initial support for the role of compression in the development of tendinopathy63,64; however, the results of these findings have not been confirmed in humans. Without evidence to support compression as a mechanism, the implications of abnormal shoulder kinematics on the potential to create subacromial compression remain theoretical. Furthermore, it is likely the pathogenesis of rotator cuff pathology involves many factors other than compression (e.g. variations in anatomical morphology, intrinsic tendon degradation, overuse). Indeed, animal models suggest the combined effect of tendon compression and experimentally-induced degeneration or overuse is greater than any individual factor.63,65,66 Therefore, future research should determine the role of each factor and combinations of factors in the development of rotator cuff pathology.
Third, future work aiming to understand the relationship between kinematics and subacromial proximities would benefit from homogenous groups defined based on motion, or sufficiently large sample sizes from which to classify movement-based subgroups. This will allow for a more direct (i.e. less confounded) assessment of the relationship between kinematics and subacromial proximities.
Finally, more research is needed to develop accurate and reliable clinical measures of shoulder motion. This research direction may seem dependent upon future research establishing a link between abnormal shoulder motion and rotator cuff pathology. However, other mechanism of rotator cuff pathology (e.g. posterior/internal impingement) or types of pathology (e.g. labral tear, biceps tendinosis) may be impacted by abnormal motion. Furthermore, the ability of clinicians to accurately assess human motion is fundamental to providing best care for patients as it informs the basis for exercise, manual therapy, and activity modification recommendations.
ConclusionChanges in glenohumeral and scapular kinematics are associated with changes in subacromial proximities. The common metric of bone-to-bone acromiohumeral distance consistently results in minimal distances occurring in the range of 70°–120° of humerothoracic elevation; however, this metric does not reflect proximity to the rotator cuff tendons. When proximity to the humeral insertion site is considered specifically, the minimal distance occurs between 45° and 90° of humerothoracic elevation. The magnitude and direction of a particular motion's impact on subacromial proximities (i.e. increase/decrease) often vary between studies, which likely reflects different methodologies and subject populations. Future research is needed to further investigate the relationship between kinematics and subacromial proximities using more homogenous groups, determine the extent to which compression and other factors contribute to rotator cuff pathology, and develop accurate and reliable clinical measures of shoulder motion.
Conflicts of interestThe authors declare no conflicts of interest.