Recovery of physical activity (PA) after telerehabilitation following knee and hip arthroplasty (TKA-THA) has rarely been studied. An improved understanding of PA recovery is needed, as it could be influenced by many factors such as age, gender or pre-operative physical function.
ObjectivesTo assess PA recovery weekly for 3 months after TKA-THA and to determine perioperative factors that could help predict PA recovery at 3 months.
MethodsFrom one week before until 3 months after surgery, 132 patients wore a fitness tracker continuously. Each patient received personalized and daily exercises and feedback through a tablet. Before and after surgery, patient-reported outcome measures of symptoms, pain, activities of daily living and quality of life were recorded. A one-way repeated-measure ANOVA was used to assess the time effect on step count for each post-operative week. To predict the absolute step count at 3 months post-surgery, a backward multiple linear regression was used.
ResultsPatients reached their pre-operative PA level at week 7, with no significant additional improvement by 3 months post-surgery. Pre-operative step count, the number of days using crutches and pre-operative symptoms explained 35% of the variability of step count at 3 months.
ConclusionThis patient population receiving telerehabilitation reached their pre-operative PA level at 7-week post-surgery with no further improvement over the subsequent 5 weeks. The PA level at 3 months could be predicted by pre-operative step count, duration of crutches use, and pre-operative symptoms.
Total hip arthroplasty (THA) or total knee arthroplasty (TKA) are surgical interventions for end-stage symptomatic osteoarthritis (OA). In Belgium, a total of 49,771 hip and knee arthroplasties were performed in 2016 (26736 THA, 23035 TKA1) and in the US the numbers are expected to increase significantly until 2030.2,3
Physical activity (PA) is defined as any movement produced by skeletal muscles that requires energy expenditure. PA is beneficial for physical, social and mental health,4 and is a major concern for public health policies.5 Recovery of PA in the early postoperative phase is still unclear as studies have showed conflicting results. Schotanus et al.6 observed that PA post TKA improves steeply during the first 4 postoperative days and continues to improve towards the 6-week assessment, however, it remained below preoperative levels. Conversely, Twiggs et al.7 recorded step counts similar to preoperative values at the 6 week post-operative time point. For later stages in the recovery, a systematic review by Arnold et al. (373 patients) found that compared to prior to surgery there are negligible changes in PA at 6 months after THA and TKA, but larger changes 1year postoperatively.8 Although THA and TKA improve pain and function,4,9 it is not clear if PA is also enhanced in comparison to pre-operative level.8 Moreover, PA post-surgery remains lower than in people without OA.10
PA assessment can be conducted through validated self-report questionnaires.11 Although such questionnaires are convenient, they are subject to patient recollection and therefore recall bias.12 In addition, change in PA after joint arthroplasty has mostly been assessed as a “snapshot”, at two or three time-points,8 failing to convey the complexity of the recovery. Paxton et al. recommended the use of fitness trackers, as accelerometry-based measurements at multiple post-surgical time points during rehabilitation.10 These fitness trackers enable objective PA quantification over long periods of time, calculating the number of steps per day.13 These devices can also gather detailed PA data that physical therapists cannot otherwise observe.14
Although the optimal approach for rehabilitation following TKA and THA is still unclear, telerehabilitation has demonstrated its potential to maximize patient recovery in a cost-effective way.15–17 Telerehabilitation appears to be effective and comparable to standard rehabilitation for the improvement of physical function and pain.18 Technological developments combining fitness tracker and tablet use are promising for providing telerehabilitation and for monitoring daily activity.19
To develop effective strategies to improve PA after hip and knee arthroplasties, it is necessary to thoroughly explore preoperative predictors of changes in PA after surgery.8 Some studies have already assessed the influence of predictors such as age and gender on PA in patients with knee or hip OA.20,21 Female gender,21 old age and a low level of functional performance20 were associated with lower levels of PA. However to our knowledge, studies assessing the influence of predictors on recovery after TKA and THA are scarce.22 Twiggs et al.7 recently observed a gender effect in PA in the pre-op period but not at 1 and 6 week after TKA. In their systematic review, Veenhof et al.20 observed conflicting evidence for the association between age, gender and the recovery level of PA in patients with knee OA. Twiggs et al.7 also showed that quality of life, body mass index (BMI) and preoperative step count predicted PA recovery in patients at 6 weeks post TKA.7 A better understanding of the association between age, gender, surgery type, PA level and PA recovery after surgery may help to tailor telerehabilitation programs to the patients’ needs.
The aim of our study was (1) to assess PA recovery each week after TKA or THA surgery, distinguishing between male and female populations, treated by telerehabilitation and, (2) to explore predictors of PA recovery every week up to 3 months after the surgery.
MethodsStudy designThe data for this longitudinal cohort study are from the MORE Clinical Study (Clinical Trial Number : B117201732334), a pilot study part of a national program to create a framework for mobile health application in the Belgium healthcare system.23 During this study, patients were monitored after knee or hip arthroplasty by a commercially available mobile-health application (Move Up cvba, Belgium) for 3 months after surgery. This protocol was conducted, recorded and reported in compliance with ISO 14155:2011 Clinical investigation of medical devices for human subjects – Good Clinical Practice and ICH-GCP guidelines. In this report, we used data for one arm of study, all patients receiving the same treatment.
SettingPatients had TKA or THA performed between January 2017 and February 2018 in one of three Belgian hospitals. They were given a wearable fitness tracker and a computer tablet one week before surgery. They were instructed to continuously wear the tracker upon receipt, except during surgery and to synchronize it to the tablet by means of a Bluetooth connection every 7 days.
The ethics committee of Université Catholique de Louvain (Brussels, Belgium) approved the study protocol (agreement number: B403201523492) and each patient provided written informed consent to the use of their anonymized data for scientific use.
ParticipantsThe study population consisted of 146 adults aged 18 years and over, undergoing a hip or knee arthroplasty, discharged to home environment and able to independently perform daily life activities. Participants had to reside in Belgium during the rehabilitation period, to be able to give voluntary, written informed consent, and to receive no other physical therapy care other than the telerehabilitation program. Participants were identified and recruited by the clinical investigators and their research staff of each hospital.
Exclusion criteria were: pre- or post-operative procedures that might interfere with the rehabilitation, scheduled surgery in the 3 months following the reference surgery, significant neurological conditions that might interfere with the rehabilitation program, psychiatric disorders or active alcohol/drug abuse, incomplete medical record data either before the surgery or at 3 months post-operative period, a rehabilitation period of less than 6 weeks or an interruption in the data collection of the tracker.
VariablesThe primary, dependent outcome variable is PA, represented by the amount of steps recorded each day with the use of a fitness tracker. PA was measured during one week before surgery to the end of the rehabilitation. To have representative and reliable data, PA was averaged on a sample of 5–7 consecutive days for every analyzed period.24 The mean pre-operative step count was calculated over a 5–7 day period depending on the available recorded data. The mean post-operative step count was calculated for each post-operative week. The ratio between the step count at 3 months and the step count in the week before surgery was calculated and expressed as a percentage.
The following patient information was recorded pre-operatively as independent variables: age, gender, type of surgery (hip or knee arthroplasty) and patient-reported outcome measures (PROM) of symptoms, pain, activities of daily living and quality of life within the 2 weeks before surgery. In the post-operative phase we recorded: the number of days of anti-inflammatory drugs intake, the number of days using crutches and PROM 3 month after surgery. PROM were measured by adapted validated scales for the study population. Patients with knee surgery completed the Knee Injury and Osteoarthritis Score (KOOS) while those with hip surgery completed the Hip Injury and Osteoarthritis Score (HOOS) questionnaire using the tablet. These PROMs consist of 42 questions for the KOOS and 40 for the HOOS and investigate five different subscales: symptoms, pain, activities of daily living, sports and recreational activities and quality of life.25 Scores for each subscale range from 0 to 100 with higher scores representing better function. The sports and recreational activities subscale were not used for this study as improvement in these areas was not expected within 3 months of surgery.
Data sources/measurementPA was measured by a commercial fitness tracker (Nokia®Go, Nokia Europe, Issyles-Moulineaux, France). This device was selected for its low cost, long battery life, and waterproof properties.26 The validity of step count measurement has been previously assessed in comparison to reference devices for walking and free-living conditions.27 For walking, the bias was limited, while for the free-living condition, PA was underestimated in comparison to data from the ActiGraph device.27
The monitor was worn on the patient’s wrist (side based on patient’s personal preference). Compliance with monitor wear was assessed by self-reported take off time and post hoc examination of data. Patients were aware of their daily step count as displayed by the tracker.
The self-administered questionnaires (KOOS or HOOS) were completed electronically through the tablet as well as the recording of the number of days of anti-inflammatory drugs intake and the number of days using crutches.
Rehabilitation programThe rehabilitation was implemented through a mobile health solution via a tablet. The patient’s progress was monitored daily by physical therapists who offered daily personalized advices and adapted exercises. The daily step count, pain and stiffness reported by the patient, as well as the patient’s baseline characteristics were used to adapt advices and exercises. No specific behavior change principle was used at this stage, but physical therapists monitored for overloading.
The rehabilitation program was also adapted in function of the patient expectations and reported pain level during their daily activities and exercises.
Statistical methodsDescriptive statistics were used to describe the study population. PA recovery was first assessed by the slope of the linear regression between the weeks (X) and weekly mean step count (Y). Subsequently a one way Repeated ANOVA Measure (RM) was used to assess the time effect (comparing each postoperative week (1–11) data with pre-surgery data) in all patients (THA and TKA together). In addition, based on the potential influence of gender21 and type of surgery,22 the time effect (RM ANOVA) was also assessed for 4 subgroups: Women with knee surgery, Women with hip surgery, Men with knee surgery, Men with hip surgery, using a multiple comparison post hoc test with Holm-Sidak correction. To examine the association between dependent variables (PA recovery assessed by absolute step count at 3 weeks, 6 weeks; 3 months post-surgery) and independent variables, a multiple linear regression was used. The independent variables were the subgroups (Women with knee surgery, Women with hip surgery, Men with knee surgery, Men with hip surgery), age, PROM before-surgery (Symptoms, Pain, Activities of daily living and quality of life), mean PA before surgery (number of steps), the number of days of anti-inflammatory drugs intake, and the number of days using crutches. As described by Freke et al.,28 to limit over-fitting data, a backwards stepwise regression model was performed, using the Akaike Information Criterion; where variables were removed one by one to achieve the optimum fit for the model, while penalizing for complexity (more variables). This method was automated using SPSS software (IBM statistics SPSS 25). The adjusted regression coefficient of all independent variables entered into the multivariable model were displayed (with 95% confidence intervals) together with the adjusted R2 for each model, to indicate the strength of the model in explaining the variability in the dependent variable. A statistical significance of α≤ 0.05 was used for the overall model, and the association between independent variables within the model and the absolute step count.
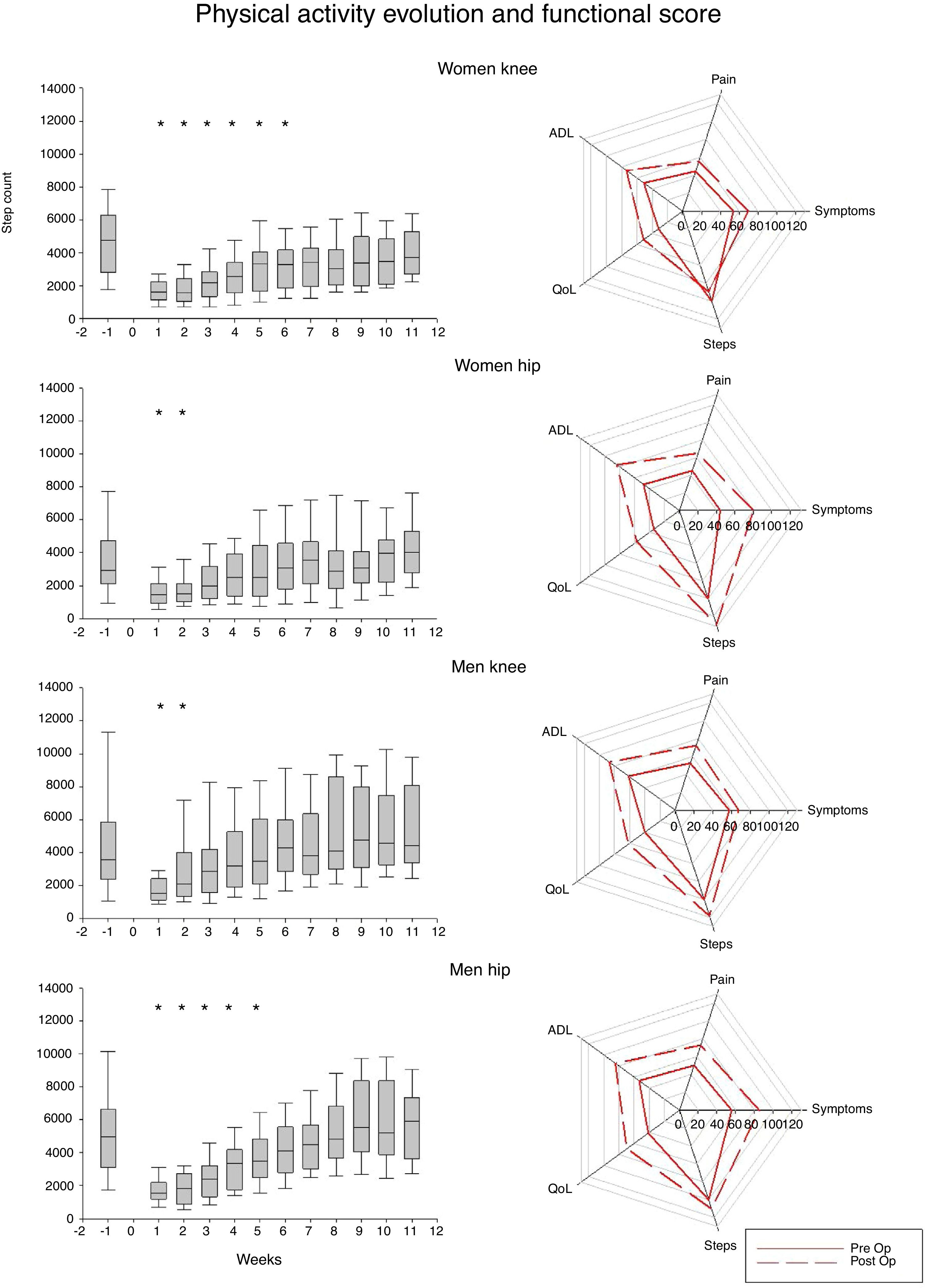
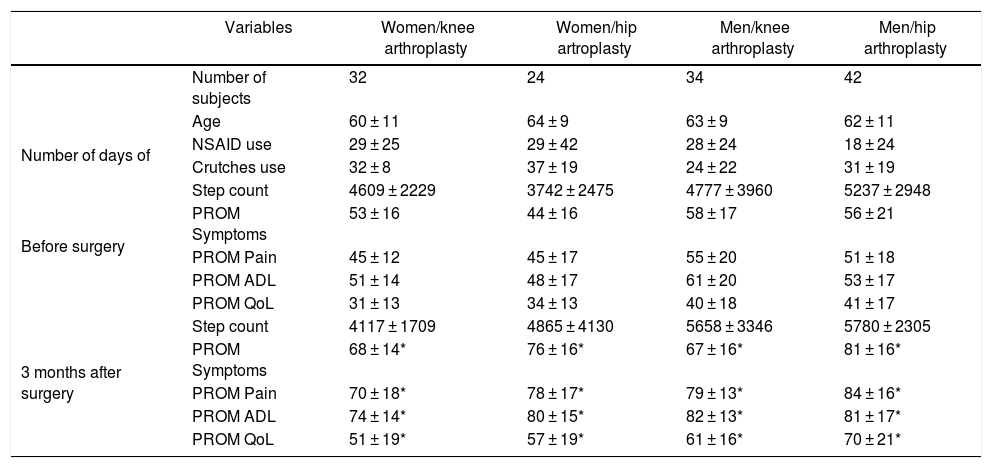
ResultsParticipantsFrom the 146 participants, 11 were excluded because of gaps in data collection (n=3) or a rehabilitation period of less than 6 weeks (n=8). Therefore 132 patients (42% females) were included in the data analysis. The mean age was 62 years (standard deviation: 10). The total proportion of knee and hip arthroplasty was equal (50% vs 50%). Patients took anti-inflammatory drugs on average for 25 days and required the use of crutches for 31 days. The 1 week preoperative and 3 month postoperative PROM data for each surgery and gender categories are presented in Table 1 and Fig. 1. Data for the PROM were significantly improved in each subgroup at 3 months post-surgery compared to pre-surgery (p<0.05).
Participants.
| Variables | Women/knee arthroplasty | Women/hip artroplasty | Men/knee arthroplasty | Men/hip arthroplasty | |
|---|---|---|---|---|---|
| Number of subjects | 32 | 24 | 34 | 42 | |
| Age | 60 ± 11 | 64 ± 9 | 63 ± 9 | 62 ± 11 | |
| Number of days of | NSAID use | 29 ± 25 | 29 ± 42 | 28 ± 24 | 18 ± 24 |
| Crutches use | 32 ± 8 | 37 ± 19 | 24 ± 22 | 31 ± 19 | |
| Before surgery | Step count | 4609 ± 2229 | 3742 ± 2475 | 4777 ± 3960 | 5237 ± 2948 |
| PROM Symptoms | 53 ± 16 | 44 ± 16 | 58 ± 17 | 56 ± 21 | |
| PROM Pain | 45 ± 12 | 45 ± 17 | 55 ± 20 | 51 ± 18 | |
| PROM ADL | 51 ± 14 | 48 ± 17 | 61 ± 20 | 53 ± 17 | |
| PROM QoL | 31 ± 13 | 34 ± 13 | 40 ± 18 | 41 ± 17 | |
| 3 months after surgery | Step count | 4117 ± 1709 | 4865 ± 4130 | 5658 ± 3346 | 5780 ± 2305 |
| PROM Symptoms | 68 ± 14* | 76 ± 16* | 67 ± 16* | 81 ± 16* | |
| PROM Pain | 70 ± 18* | 78 ± 17* | 79 ± 13* | 84 ± 16* | |
| PROM ADL | 74 ± 14* | 80 ± 15* | 82 ± 13* | 81 ± 17* | |
| PROM QoL | 51 ± 19* | 57 ± 19* | 61 ± 16* | 70 ± 21* |
Data are presented as mean±standard deviation, PROM: patient-reported outcome measures, for hip arthroplasty (KOOS), for knee arthroplasty (HOOS) (0–100 scale, higher scores indicating better function), ADL: activities of daily living, QoL: quality of life, SD: standard deviation, * : statistical difference between before and after surgery (p<0.05).
Physical activity progression for the 12 weeks post-surgery and PROMs scores and step count for each subgroup before and 3 months after surgery. On the box plot, * represents statistically significant difference with pre-op step count. On the radar plot, actual PROM scores are presented for each time while step are presented in percentage from the preoperative step count (100%).
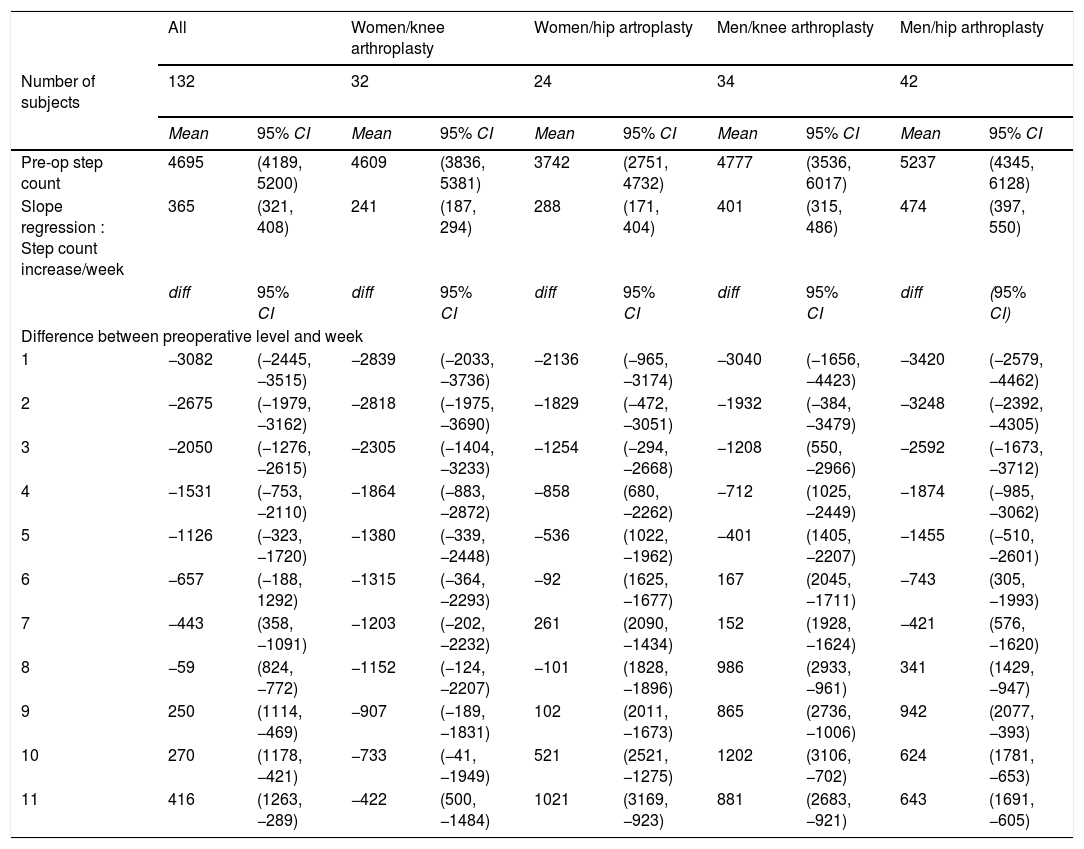
The time effect for PA, i.e. the mean step count per week, is presented in Table 2 and illustrated in Fig. 1. All patient groups presented a significant reduction in PA during the first weeks compared to the pre-operative value. Speed of PA recovery varied between groups, as illustrated by the step count increase per week (Fig. 1).
Multiple comparison post hoc test with Holm-Sidak - time effect across category based on gender and surgery type.
| All | Women/knee arthroplasty | Women/hip artroplasty | Men/knee arthroplasty | Men/hip arthroplasty | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Number of subjects | 132 | 32 | 24 | 34 | 42 | |||||
| Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | |
| Pre-op step count | 4695 | (4189, 5200) | 4609 | (3836, 5381) | 3742 | (2751, 4732) | 4777 | (3536, 6017) | 5237 | (4345, 6128) |
| Slope regression : Step count increase/week | 365 | (321, 408) | 241 | (187, 294) | 288 | (171, 404) | 401 | (315, 486) | 474 | (397, 550) |
| diff | 95% CI | diff | 95% CI | diff | 95% CI | diff | 95% CI | diff | (95% CI) | |
| Difference between preoperative level and week | ||||||||||
| 1 | −3082 | (−2445, −3515) | −2839 | (−2033, −3736) | −2136 | (−965, −3174) | −3040 | (−1656, −4423) | −3420 | (−2579, −4462) |
| 2 | −2675 | (−1979, −3162) | −2818 | (−1975, −3690) | −1829 | (−472, −3051) | −1932 | (−384, −3479) | −3248 | (−2392, −4305) |
| 3 | −2050 | (−1276, −2615) | −2305 | (−1404, −3233) | −1254 | (−294, −2668) | −1208 | (550, −2966) | −2592 | (−1673, −3712) |
| 4 | −1531 | (−753, −2110) | −1864 | (−883, −2872) | −858 | (680, −2262) | −712 | (1025, −2449) | −1874 | (−985, −3062) |
| 5 | −1126 | (−323, −1720) | −1380 | (−339, −2448) | −536 | (1022, −1962) | −401 | (1405, −2207) | −1455 | (−510, −2601) |
| 6 | −657 | (−188, 1292) | −1315 | (−364, −2293) | −92 | (1625, −1677) | 167 | (2045, −1711) | −743 | (305, −1993) |
| 7 | −443 | (358, −1091) | −1203 | (−202, −2232) | 261 | (2090, −1434) | 152 | (1928, −1624) | −421 | (576, −1620) |
| 8 | −59 | (824, −772) | −1152 | (−124, −2207) | −101 | (1828, −1896) | 986 | (2933, −961) | 341 | (1429, −947) |
| 9 | 250 | (1114, −469) | −907 | (−189, −1831) | 102 | (2011, −1673) | 865 | (2736, −1006) | 942 | (2077, −393) |
| 10 | 270 | (1178, −421) | −733 | (−41, −1949) | 521 | (2521, −1275) | 1202 | (3106, −702) | 624 | (1781, −653) |
| 11 | 416 | (1263, −289) | −422 | (500, −1484) | 1021 | (3169, −923) | 881 | (2683, −921) | 643 | (1691, −605) |
Differences highlighted in bold are the statistical significant difference with pre-op step count level. Negative difference means lower step count value than pre-op, positive difference means higher step count value than pre-op. diff : mean difference with pre-op step count, 95% CI : confidence interval for difference.
Starting from 7 weeks after surgery, PA values were similar to pre-operative PA values. However, considering the wide 95% CI in the subgroups (Table 2), not every patient recovered to their pre-operative activity level. Finally, none of the subgroups showed significant additional improvement between 7 weeks and 3 months post-surgery.
Women with hip arthroplasty were the most sedentary group pre-operatively (mean [95% confidence interval] step count of 3742 [2751, 4732]). They presented no significant difference with pre-operative step count at week 3 post-surgery, with no additional improvement beyond that point. Women with knee arthroplasty had the slowest recovery (241 step increase/week), while men with knee and hip arthroplasty respectively reached their pre-operative PA level at weeks 4 and 5 before reaching a plateau.
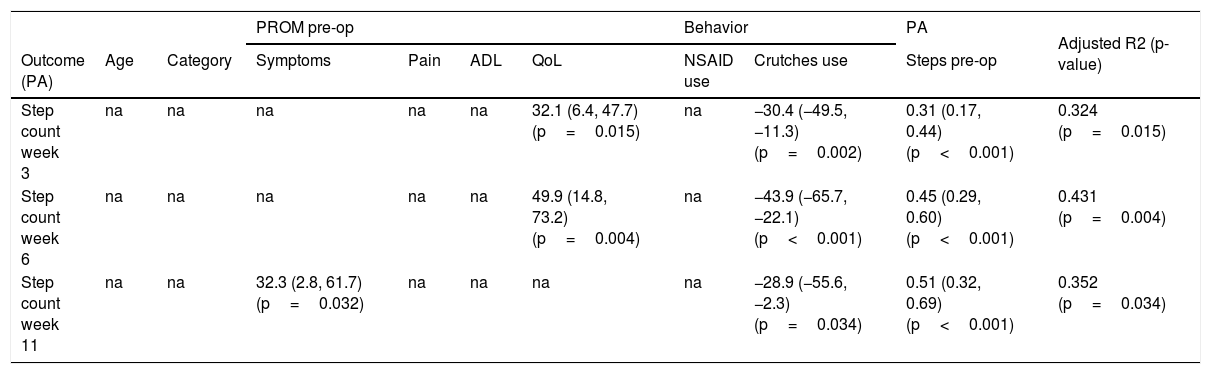
Predictors of PA recoveryResults of the stepwise backward regression are presented in Table 3. For the step count at 3 and 6 weeks, pre-operative step count, the number of days using crutches and the score on the pre-operative quality of life subscale on the PROM explained respectively 32 and 43% of the variability. For the step count at week 11, pre-operative step count, the number of days using crutches and the score on the pre-operative symptoms subscale of the PROM explained 35% of the variability.
Stepwise backward regression: adjusted estimates (95% CI) of the association between dependent variables and physical activity level post arthroplasty.
| PROM pre-op | Behavior | PA | Adjusted R2 (p-value) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome (PA) | Age | Category | Symptoms | Pain | ADL | QoL | NSAID use | Crutches use | Steps pre-op | |
| Step count week 3 | na | na | na | na | na | 32.1 (6.4, 47.7) (p=0.015) | na | −30.4 (−49.5, −11.3) (p=0.002) | 0.31 (0.17, 0.44) (p<0.001) | 0.324 (p=0.015) |
| Step count week 6 | na | na | na | na | na | 49.9 (14.8, 73.2) (p=0.004) | na | −43.9 (−65.7, −22.1) (p<0.001) | 0.45 (0.29, 0.60) (p<0.001) | 0.431 (p=0.004) |
| Step count week 11 | na | na | 32.3 (2.8, 61.7) (p=0.032) | na | na | na | na | −28.9 (−55.6, −2.3) (p=0.034) | 0.51 (0.32, 0.69) (p<0.001) | 0.352 (p=0.034) |
pre-op : pre operative, ADL : activities of daily living (PROMS), QoL : Quality of life (PROMS), NSAID : non-steroidal anti-inflammatory drug, PA : physical activity (stepcount), na : no association.
The pre-operative step count variable was the strongest predictor at week 11 (26.6%) while the pre-operative symptoms (change in R2: 5.2%) and crutches use (change in R2: 3.4%) had less weight in the model.
Age, sub group (1–4), symptoms, pain, activities of daily living (PROM) and number of days using anti-inflammatory drugs were not significant and therefore not included in the regression model (p>0.05).
DiscussionThe main results of this study were that individuals post TKA and THA recover rapidly to their pre-operative PA levels over the first six weeks after surgery, which was followed by a plateau until the end of the follow-up period at 3 months post-surgery. The level of PA at 3 months post-surgery was mostly predicted by the preoperative PA level, the number of days of using crutches and the pre-operative symptoms as measured with a PROM.
PA recoveryWe observed a fast recovery of PA in the first weeks, followed by a steady state at the pre-operative level until the end of the follow-up period. Function and pain improved over time from the preoperative levels but were not associated to PA increase. Post-operative PA recovery varied depending on gender and type of surgery. Women with hip surgery recovered faster but were also the most sedentary group at baseline. Although women with knee surgery didn’t fully recover to their pre-operative PA level, there was no significant difference between step count at 3 months and the preoperative step count. They recovered at a slower pace and exhibited the lowest functional score (PROMS) after 3 months. Those results suggest that this patient subpopulation could benefit from better guidance in the recovery process.
In our sample, the 7 week time point appears to be a milestone in the patient’s recovery process, followed by a steady state. Crizer et al.22 also observed a gradual PA recovery for patients with THA and TKA, with a slower recovery for TKA. Those patients regained their baseline PA after 9 weeks22 while patients post-THA recovered to their baseline at week 5. The faster recovery in our sample could be partly attributed to the tele-rehabilitation program and the PA awareness developed by the patients.29 But in the current study, a control group with standard of care is lacking. Our sample also had higher baseline PA than in the study by Crizer et al.22 with a PA baseline for all of our patients at 4695 steps while their PA baseline was 2682 steps for THA and 1988 steps for TKA.
Self-reported measurements of pain and function improved significantly post-surgery. This result is in agreement with studies on the effectiveness of arthroplasty for reducing symptoms.15 But PA did not increase relative to pre-operative level. Similar findings demonstrating this disassociation have been demonstrated in several studies.30,31 PROM are central to orthopedic research, clinical practice and quality control,32 But they provide only one aspect of functional recovery. Other objective markers of successful rehabilitation are therefore needed. While pre-operative PA level could be a good indicator of returning to normal physical habitus after surgery, the association of PA with the return to professional and recreational activities, patient specific goals33 and participation according the International classification of Functioning, Disability and Health need to be addressed in future research.34,35
Predictors of PA recoveryOur second aim was to explore predictors of PA recovery every week up to 3 months after TKA and THA. The PA recovery at 3 and 6 weeks could be predicted by preoperative PA level, the number of days using crutches and the pre-operative score on the quality of life subscale of the PROM. While the PA at 3-months could be predicted mostly by the preoperative PA level, the number of days using crutches and the pre-operative score on the symptoms subscale of the PROM. At week 11, preoperative PA level is the most important predictor. It means that a higher preoperative PA level, less days using crutches and less preoperative symptoms predict a better PA outcome.
Twiggs et al.7 also observed a relationship between the physical component of the SF12 (SF12 PCS) and 6 week post-operative step count and explained 75% of the PA level at 6 weeks with preoperative step count, gender and score on the SF12 PCS.7 It means that such PROM results could be useful in the step count target in rehabilitation. However, Crizer et al.22 observed in 589 patients that lower extremity functional scale (LEFS) scores were only weakly correlated with step count and that the correlation became increasingly weak with time after surgery, with no clear correlation at 12 weeks postoperatively.22 This lack of correlation between preoperative symptoms and PA level observed in our study could be surprising. Past experiences with illness, personality, coping styles, family and cultural norms, and current interpersonal interactions are examples of factors that interact to influence PA level.36 Surprisingly, age was not retained in our model while Toogood et al. observed an age effect by a categorical comparison (<70 years versus > 70 years).37 This discrepancy could be explained by the statistical method as well as by differences in our patient sample.
The number of days using crutches seems to be associated with PA and could represent an objective quantitative measure of disability. While this assistive technology may be beneficial for individuals with OA, their impact on mobility and community participation depend on the user’s ability.38 Caution is needed in the understanding of the relation between PA and crutches use, because of its potential impact on the accuracy of the activity tracker, which may be reduced when using crutches.39 However, a recent study on step recording validity in subjects walking with crutches reported a small bias, unlikely to affect our study results.40
PerspectivesPrevious research observed few changes in PA evolution at two or three time points after arthroplasty.8 In contrast, a few recent research investigated recovery speed and found different results regarding pre-surgery PA level.6,7,22 Our study adds more information in the emerging field of continuous activity monitoring. Moreover, it is the first study to provide activity data from patients, which performed their rehabilitation through a telerehabilitation application. However, as we did not have a control group, have no data on co-morbidities and functional recovery, it is not possible to conclude on its effectiveness on PA change.
Our results provide information allowing the development of personalized step count goals for patients, based on their pre-operative activity status and characteristics. Step count is not a new marker, but its accessibility to healthcare providers is increasing. The relevance of this measure in the 3 month acute phase could contribute to adapt treatment frequency and intensity in the recovery of pre-operative PA level. The use of relevant and objective, continuous or high-frequency digital measures of clinical efficacy and disability (pain severity, PA, sleep quality, activity pattern, etc.) could have a positive influence on the rehabilitation protocols and lead to more personalized care. Their potential for clinical decision making in personalized rehab should be evaluated in future research.
Measurement of PA level at further time points may prove informative. Indeed, in our sample, the PA level was low in comparison to healthy individuals and PA guidelines.41 The main goal of surgery is pain relief, but expectations in a public health perspective could be to increase PA level in the long term. Attention to social and community participation, in the context of a multidisciplinary approach to post-operative care, could be paramount in improving PA.34
Furthermore, the device used in our study provides the patient feedback on their activity level and allow a comparison with their pre-operative PA level. This technology will allow to define patient-specific step goals to reach in the post-operative period and assess their clinical utility in PA improvement in future studies.29
LimitationsOur study has some limitations. First, we did not control for comorbidities, BMI or social support which could influence PA21 and we lacked information such as the pre-operative use of crutches or working status. Secondly, we reach the conclusion that PA is unchanged from the pre-operative situation at 3 months, but changes to PA are difficult to detect42 and depend on the outcome measure. An increase in PA would require 6–12 months to be clearly highlighted.42 Moreover, the variability of the step count estimates in our sample limit the interpretation. Considering that a whole subgroup recovered their pre-operative PA level at week 11 could be a mistake as the confidence intervals are wide. We also compared our results with other studies but comparison with other studies is difficult as the step tracking method differ. Indeed, our fitness tracker (Nokia®Go) has an excellent agreement with the reference device in a walking task but systematically underestimates step count in comparison to the Actigraph wGT3X-BT in a free living task (41% difference).27
ConclusionIn conclusion, our patient population receiving telerehabilitation reached their pre-operative PA level at 7-week post-surgery and subsequently maintained a steady state until 3 months post-surgery. Women with knee arthroplasty recovered slower and experienced more pain and symptoms. The PA level at 3 months could be moderately predicted by pre-operative step count, duration of using crutches post-surgery, and pre-operative symptoms level.
We wish to express our gratitude to Kerensa Tiberghien and Maxime Valet for their help in data processing, and Julie Lamsens for proofreading this document.