The relationship between hip pathology and patient reported outcome responses following hip surgery has been previously investigated. No studies have investigated the relationship between pathology and patient reported outcome responses prior to surgery.
Objectives(1) Determine the prevalence of chondral and labral pathology identified during hip arthroscopy. (2) Determine the association between intra-articular findings and patient reported outcome scores in a pre-arthroscopy hip pain population.
MethodsSixty-seven (22 female) participants scheduled for hip arthroscopy after clinical examination and radiographic assessment completed a series of patient reported outcomes (Hip Disability and Osteoarthritis Outcome Score; International Hip Outcome Tool; Pain on Activity; Visual Analogue Scale). Pathology discovered/addressed during arthroscopy was classified. Univariable and multivariable linear regression models were used to assess the relationship between demographics, pathology and patient reported outcome responses.
ResultsNinety-one percent of participants had labral pathology; 76% had acetabular chondropathy and 31% had femoral head chondropathy. Across the ten patient reported outcome subscales, severe femoral head chondropathy and large labral tears had the greatest number of significant associations with patient reported outcome scores. The strongest association was with ‘Hip Disability and Osteoarthritis Outcome Score symptoms and stiffness’ subscale, where severe femoral head chondropathy explained 22% of variability in symptoms and stiffness, when adjusted for Body Mass Index and presence of pincer morphology (p=0.002).
ConclusionSevere femoral head chondropathy and large labral tears along with a high prevalence of labral pathology and acetabular chondropathy were relatively common findings during hip arthroscopy. Severe femoral head chondropathy and large labral tears are most associated with patient reported outcome's, however, at best only explain 22% of the variability.
Hip and groin pain are common in the community1 and in sporting populations.2 Contributing conditions include femoroacetabular impingement syndrome (FAI), which affects younger adults and is thought to contribute to early degeneration of the labrum and adjacent cartilage,3 and osteoarthritis (OA) in older populations.4 Other forms of intra-articular hip pathology such as acute labral and ligamentum teres tears may occur through trauma or excessive load and be unrelated to bony morphology or degenerative change.5
Arthroscopy is utilized to treat patients in the early stages of hip pathology by osteoplasty of femoral and acetabular deformities (cam and pincer, respectively), and repair of injuries of the acetabular labrum and adjacent cartilage.6 Pathologies that exist in the advanced stages of OA, such as cartilage defects on the femoral head or in the acetabular region, are considered to be poor prognostic indicators7–10 and a limiting factor for clinical improvement.11,12 When patients with advanced chondropathy or pre-existing OA undergo hip arthroscopy, they report lower patient satisfaction and lower outcomes for function and pain12,13 and tended to be unimproved or even deteriorated at follow-up11,14 when compared to individuals with mild hip chondropathy. The population considered most appropriate for hip arthroscopy are younger, physically active people with unaffected gait and inguinal pain related to movement (flexion and internal rotation) who possess imaging signs of FAI or dysplasia without joint space narrowing, labral tears, or damage in chondrolabral junction.6 Arthroscopic labral debridement in patients without chondropathy resulted in significant improvement post surgery in the clinical scoring systems when compared to patients with articular cartilage lesions,11 with severe chondropathy associated with worse pain and function at eighteen months post surgery.14
Before and following arthroscopy, hip pain and function are frequently measured using patient-reported outcomes (PROs) questionnaires.15,16 Several specific PROs are used to reliably evaluate hip arthroscopic surgery outcomes,17,18 present a patient-focused perspective19 and capture outcomes that are important to patients.20 The intra-class correlation coefficient values for most subscales of the Hip Disability and Osteoarthritis Outcome Score (HOOS) and the International Hip Outcome Tool (iHOT-33) equal or exceed 0.90 indicating that these questionnaires meet acceptable levels of reliability and precision for application at the individual level and group level.21 Along with functional PROs using a Likert scale, such as the Pain on Activity (POA), they measure hip pain and function.22,23 While many studies have outlined the relationship between various pathologies and PRO response post surgery,24–26 the post-operative responses may be mitigated by surgery. The relationships between intra-articular hip pathology and PRO responses prior to surgery have yet to be fully identified. Although PROs are not designed to differentiate between types or severity of pathology, determining the relationship between frequently-used PROs to the intra-articular conditions provoking symptoms may help refine clinical decision making and shape opinion regarding the likely severity of findings during surgery.
The purpose of our study was to determine:
- (1)
The prevalence of femoral head, acetabular, labral and ligamentum teres pathology in a population assessed by clinical examination and radiological assessment as appropriate for arthroscopic hip surgery.
- (2)
The association between pre-operative PROs (HOOS, iHOT-33 and POA) and intra-articular findings at hip arthroscopy in people with hip and groin pain.
Our hypothesis was that people with more severe forms of pathology would show significantly poorer PRO and pain scores prior to surgery.
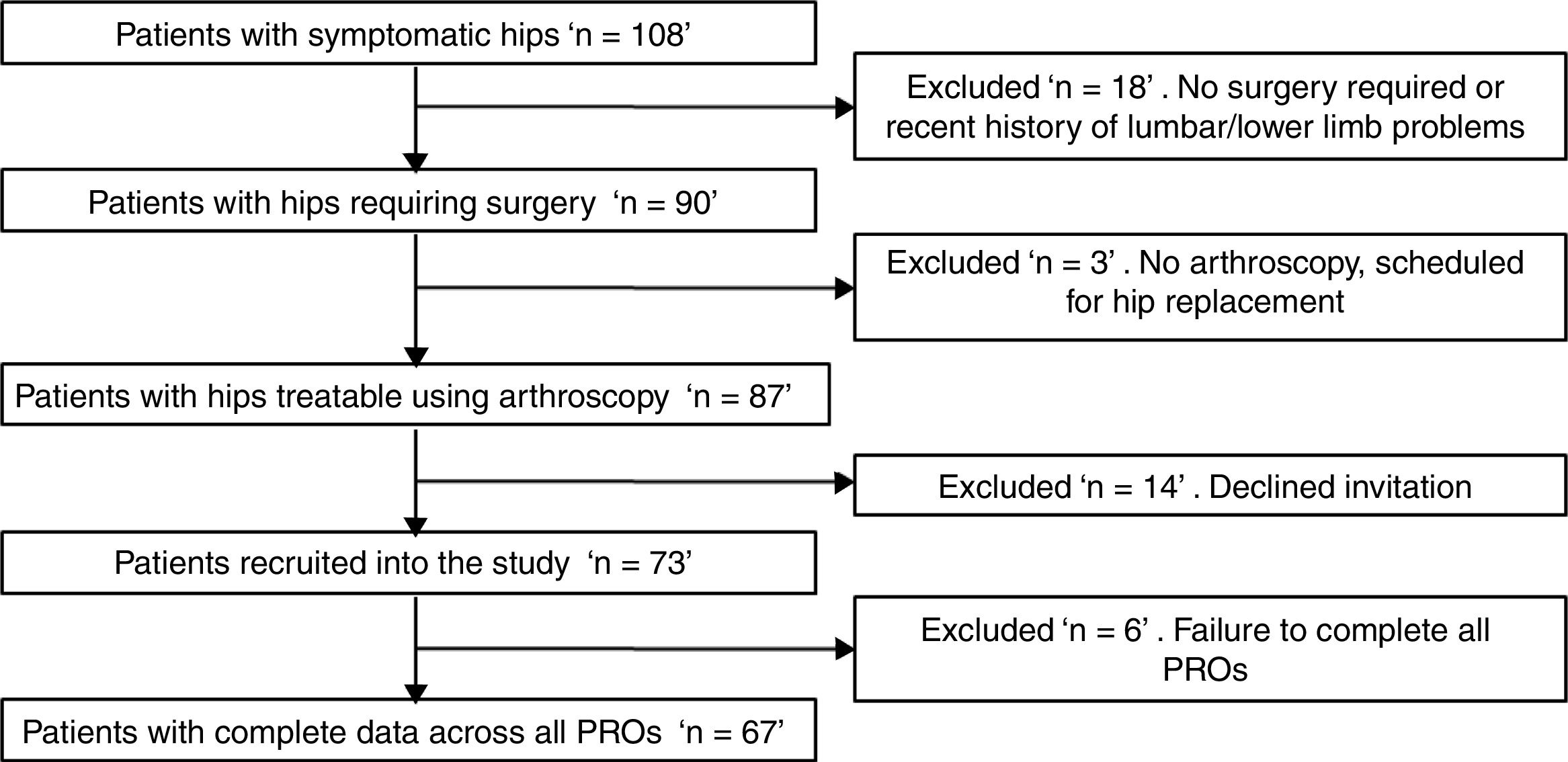
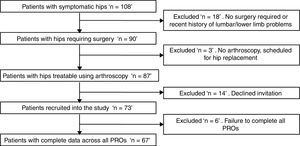
MethodsParticipantsOne hundred and eight people with hip pain within a metropolitan catchment area who presented for assessment by an orthopaedic surgeon between November 2015 and December 2016 were invited to participate in the study (Fig. 1). Hip pain prior to presentation ranged from four weeks to fifteen years based on the participant's recall of their first episode of hip pain; none of the participants had undergone previous hip surgery. All participants had undergone some form of unsuccessful non-operative treatment varying from relative rest to active manual and exercise therapies with a variety of practitioners. Participants underwent both clinical examination and radiographic assessment with the treating surgeon. Those with severe degenerative changes evident on imaging and unlikely to respond to arthroscopy were excluded. Those with symptoms and examination findings indicating appropriateness for hip arthroscopy6 were included in the study. Inclusion criteria were; (1) scheduled for hip arthroscopy; (2) no recent history (previous three months) of lumbar/knee/ankle/foot problems; and (3) no complaints of vestibular or neurological diseases. Exclusion criteria were inability to walk unassisted, and inability to read or speak English. The protocol for this study was approved by the Human Research Ethics committees of the University of Queensland, Australia (HREC – 2013000285). All participants completed written informed consent before participating in the study and were tested prior to surgery.
ProceduresHip arthroscopy was performed by one of two orthopaedic surgeons (85% by one of the surgeons) who were blinded to the PRO results. While pre-operative imaging helped determine the existence of cam and pincer morphology, the determination of existence in this study was defined by whether these bony morphologies were addressed during arthroscopy. While imaging of cartilage also aided clinical decision-making, it was not used to classify soft tissue and cartilage pathology as radiographic identification of structural hip deformities is complex and the optimal image set and specific parameters to identify these abnormalities are controversial27,28 leading to many pathologies being left undiagnosed.29 For reasons of accuracy,30 assessment and classification of intra-articular pathology, including the presence of chondropathy and labral pathology, were conducted at the time of surgery. Collection of PRO data was prospective and took place when the decision for surgery was made via paper or online questionnaires. Data were compiled by a single investigator. Questionnaire data included the HOOS, the iHOT-33 and the POA. Demographics collected for all participants included sex, age, height, weight, Body Mass Index (BMI), limb dominance, and employment type.
Primary outcome measureCartilage damage to the acetabulum and femoral head was classified according to the Outerbridge grading system.31 The final cartilage pathology classifications were designated strictly by observation and/or intervention during arthroscopic surgery. The intra-articular findings included: Cam morphology resulting in osteoplasty, pincer morphology resulting in acetabuloplasty, labral pathology sub-grouped surgically into labral debridement, “small” labral tears (requiring 1–2 sutures) and “large” labral tears (requiring 3+sutures), femoral head chondropathy (sub-grouped into “mild” grade I–II femoral head chondropathy and “severe” grade III–IV femoral head chondropathy), acetabular chondropathy (sub-grouped into “mild” grade I–II acetabular chondropathy and “severe” grade III–IV acetabular chondropathy) and ligamentum teres pathology resulting in debridement. Participants may have had multiple pathological findings.
Secondary measuresPatient reported outcomesThe HOOS, the iHOT-33 and POA PROs were used to assess the participant's symptoms. The HOOS contains 40 questions with five subscales: those being symptoms and stiffness (HOOS-Symptoms), pain (HOOS-Pain), activities of daily living (HOOS-ADL), sport and recreation (HOOS-Sport), and quality-of-life (HOOS-QOL). The HOOS is used to evaluate outcomes in patients with hip dysfunction with or without OA and is recommended for use for a population undergoing hip arthroscopic surgery.22,23 The iHOT-33 contains 33 questions, with four subscales: symptoms and functional limitations (iHOT-33-Symptoms), sports and recreational activities (iHOT-33-Sport), job-related concerns (iHOT-33-Job) and social, emotional and lifestyle concerns (iHOT-33-QOL). It is used to evaluate patients undergoing hip arthroscopic surgery and is responsive to clinical change.32 Each subscale of the HOOS and the iHOT-33 has a maximum score of 100 points (best possible outcome). The POA questionnaire is a 100mm Visual Analogue Scale (VAS) that contains six questions to assess pain during hip specific functional tasks such as walking, sitting for one hour, rising from sitting, going up and down stairs, getting in/out of car and sitting with legs crossed. Each question is answered on a VAS and a total score is calculated by adding the scores from all questions, ranging from 0 (“no pain”) to 10 (“pain as severe as could be”) to achieve a score out of 60. The POA offers good opportunity for discrimination between pain levels 33 during functional tasks.
Data management and statistical analysisThe R statistical software package (https://www.r-project.org/) version 3.3.1, was used for data analyses. To examine the association between each iHOT33 and HOOS subscale, and the POA (dependent variables) and pathology at arthroscopy (independent variable), separate multivariable linear regression models were built for each PRO subscale. To limit the number of predictor variables in the model, compared with the number of observations, variables (pathology, and potential covariates BMI, age, gender) were selected for modelling based on trends for univariate, linear associations with the dependent variable (p<0.10). To further limit over-fitting data, a backwards stepwise regression model was performed, using the Akaike Information Criterion; where variables were removed one by one in order to achieve the optimum fit for the model, while penalizing for complexity (more variables). This method was automated using the stepAIC function of the MASS package in R. The adjusted regression coefficient of all independent variables entered into the multivariable model were displayed (with 95% confidence intervals) together with the adjusted R2 for each model, to indicate the strength of the model in explaining the variability in the dependent variable. The variance inflation factor (VIF) was used to explore collinearity between variables entered into each multivariable model, with mean collinearity of >4 and individual collinearity of >10 indicating collinearity that is deemed problematic.34 An α≤0.05 was used to determine significance of the overall model, and the significance of the association between independent variables within the model and the PRO subscale. The prevalence of pathology is reported descriptively as a percentage.
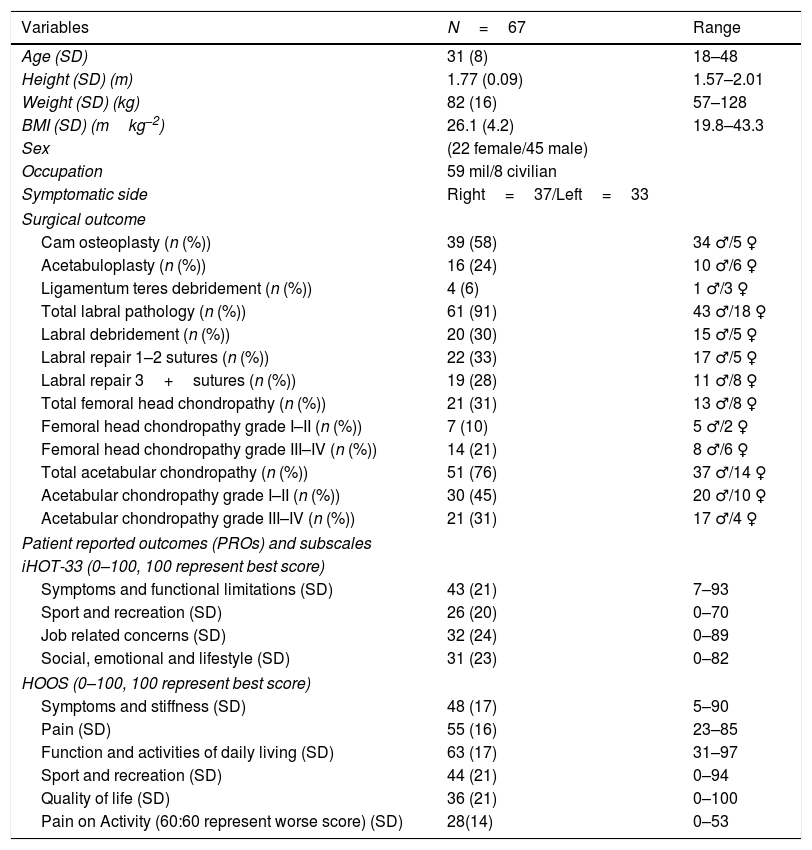
ResultsThe flow of participant recruitment is outlined in Fig. 1. Briefly, 108 patients underwent assessment for hip and groin pain, of which 87 fulfilled the inclusion criteria and were scheduled for arthroscopy. A total of 73 patients responded to an invitation to participate in the study. Six were excluded because they failed to complete all PRO questionnaires. Sixty-seven patients (45 men) with an average age of 31 years old fulfilled the eligibility criteria, consented to participate and were included in the final study cohort. Fifty-nine of the sixty-seven (88%) participants were serving in the military. The demographic characteristics are summarized in Table 1.
Characteristics of participants.
| Variables | N=67 | Range |
|---|---|---|
| Age (SD) | 31 (8) | 18–48 |
| Height (SD) (m) | 1.77 (0.09) | 1.57–2.01 |
| Weight (SD) (kg) | 82 (16) | 57–128 |
| BMI (SD) (mkg−2) | 26.1 (4.2) | 19.8–43.3 |
| Sex | (22 female/45 male) | |
| Occupation | 59 mil/8 civilian | |
| Symptomatic side | Right=37/Left=33 | |
| Surgical outcome | ||
| Cam osteoplasty (n (%)) | 39 (58) | 34 ♂/5 ♀ |
| Acetabuloplasty (n (%)) | 16 (24) | 10 ♂/6 ♀ |
| Ligamentum teres debridement (n (%)) | 4 (6) | 1 ♂/3 ♀ |
| Total labral pathology (n (%)) | 61 (91) | 43 ♂/18 ♀ |
| Labral debridement (n (%)) | 20 (30) | 15 ♂/5 ♀ |
| Labral repair 1–2 sutures (n (%)) | 22 (33) | 17 ♂/5 ♀ |
| Labral repair 3+sutures (n (%)) | 19 (28) | 11 ♂/8 ♀ |
| Total femoral head chondropathy (n (%)) | 21 (31) | 13 ♂/8 ♀ |
| Femoral head chondropathy grade I–II (n (%)) | 7 (10) | 5 ♂/2 ♀ |
| Femoral head chondropathy grade III–IV (n (%)) | 14 (21) | 8 ♂/6 ♀ |
| Total acetabular chondropathy (n (%)) | 51 (76) | 37 ♂/14 ♀ |
| Acetabular chondropathy grade I–II (n (%)) | 30 (45) | 20 ♂/10 ♀ |
| Acetabular chondropathy grade III–IV (n (%)) | 21 (31) | 17 ♂/4 ♀ |
| Patient reported outcomes (PROs) and subscales | ||
| iHOT-33 (0–100, 100 represent best score) | ||
| Symptoms and functional limitations (SD) | 43 (21) | 7–93 |
| Sport and recreation (SD) | 26 (20) | 0–70 |
| Job related concerns (SD) | 32 (24) | 0–89 |
| Social, emotional and lifestyle (SD) | 31 (23) | 0–82 |
| HOOS (0–100, 100 represent best score) | ||
| Symptoms and stiffness (SD) | 48 (17) | 5–90 |
| Pain (SD) | 55 (16) | 23–85 |
| Function and activities of daily living (SD) | 63 (17) | 31–97 |
| Sport and recreation (SD) | 44 (21) | 0–94 |
| Quality of life (SD) | 36 (21) | 0–100 |
| Pain on Activity (60:60 represent worse score) (SD) | 28(14) | 0–53 |
Continuous variables are reported as means±SD and categorical variables as frequencies and percentages. Percentages and PRO scores may not add up to 100% due to rounding.
SD, standard deviation; HOOS and iHOT-33 – 0–100, 100 indicating no symptoms and 0 indicating extreme symptoms, POA, the higher the index, the greater the person's disability due to pain. Mil, serving in military.
Ninety-one percent (n=61) of participants had labral pathology requiring surgical intervention (debridement or repair) with large labral tears requiring 3+sutures found in 28% (n=19). Acetabular chondropathy was present in 76% (n=51) of participants with severe acetabular chondropathy found in 31% (n=21). Femoral head chondropathy was present in 31% (n=21) of participants with severe femoral head chondropathy occurring in 21% of the study population (n=14), 58% (n=39) underwent osteoplasty for cam-type FAI with an additional 24% (n=16) under-going acetabuloplasty for pincer type FAI. The means with standard deviation and range are displayed in Table 1.
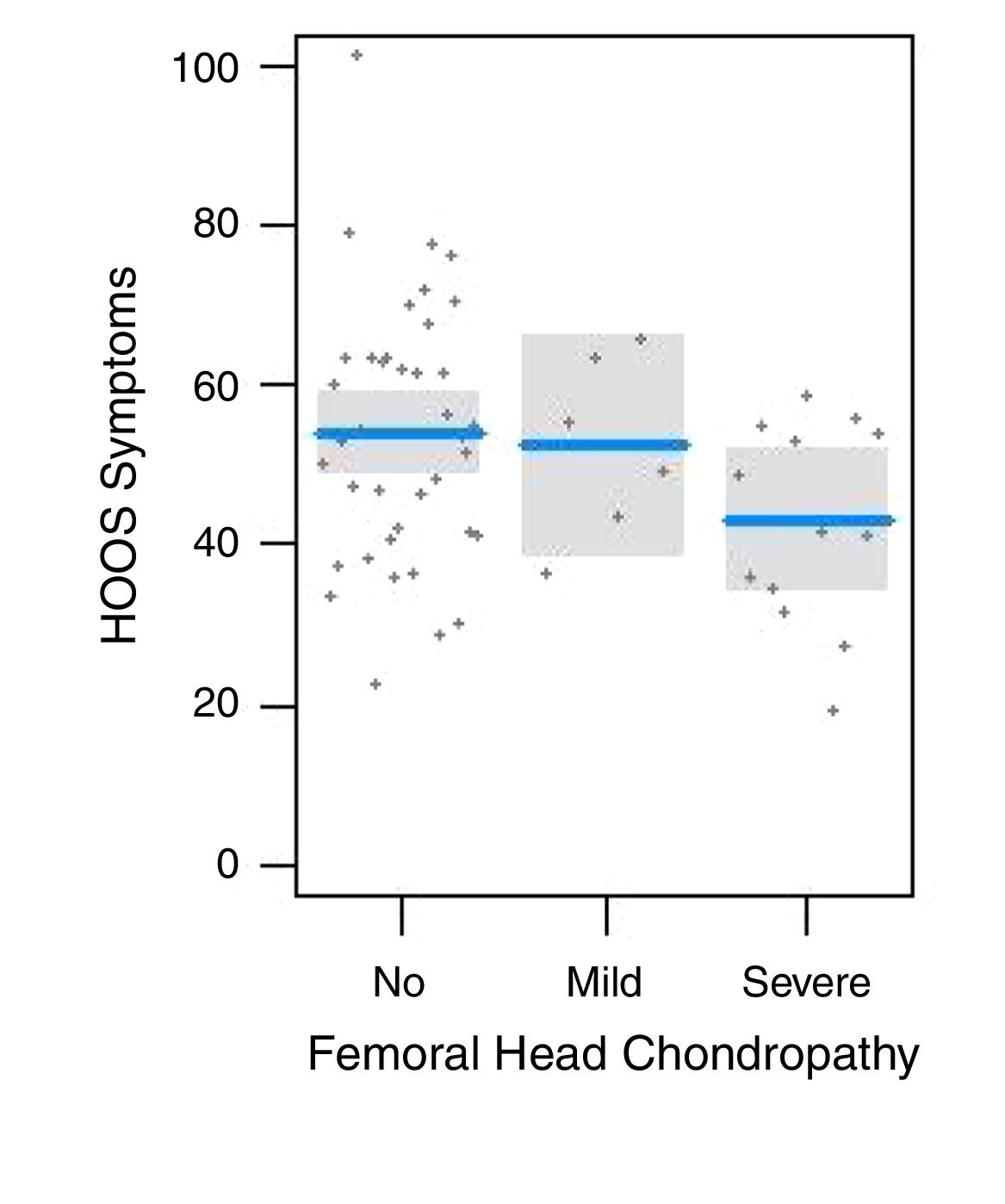
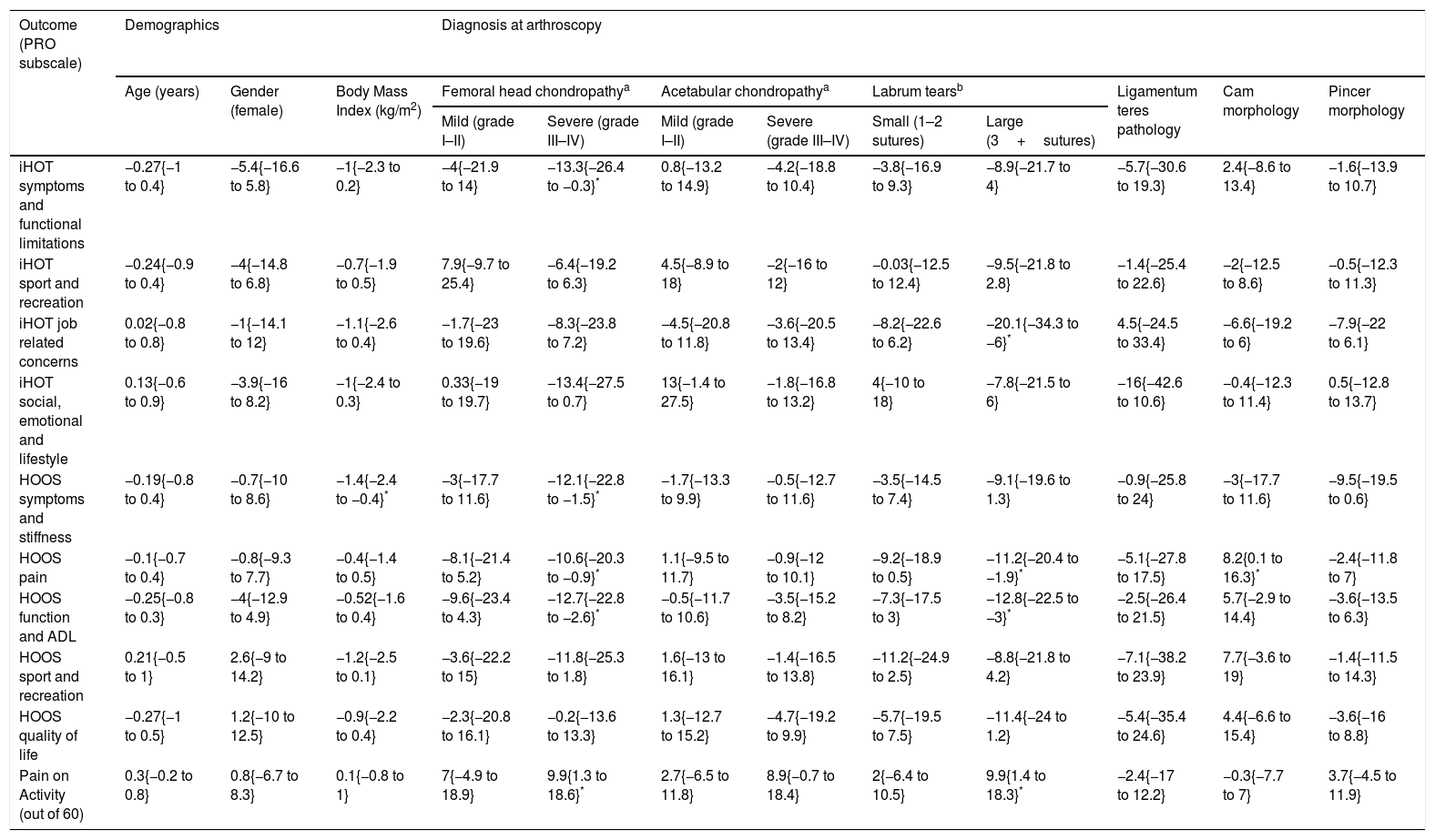
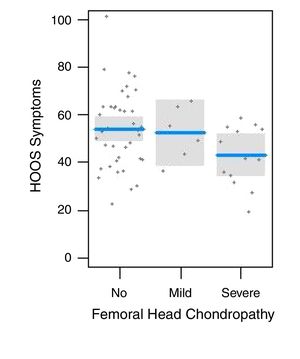
Univariable (crude) association between PROs and hip pathology.Table 2 presents the univariate associations between PRO subscales and pathology, and demographics. For example, the significant association between severe femoral head chondropathy and the iHot-33-Symptoms subscale suggests that those with severe chondropathy were likely to score 13 points less on this PRO subscale than those without chondropathy. Severe femoral head chondropathy was most highly associated with PRO subscales (POA, iHot-33-Symptoms, iHot-33-QOL, HOOS-Symptoms, HOOS-Pain, HOOS-Sport and HOOS-ADL). Large labral tears also demonstrated a high positive association (POA, iHot-33-Job, HOOS-Symptoms, HOOS-Pain, HOOS-QOL and HOOS-ADL) with sufferers reporting 10–20 points lower on these subscales. Cam and Pincer morphology were associated with the HOOS-Pain and HOOS-Symptoms subscales respectively. Severe acetabular chondropathy was associated with the POA and small labral tears were associated with the HOOS-Pain subscale. Ligamentum teres pathology, mild femoral head chondropathy and mild acetabular chondropathy were not associated with any of the PRO subscales or POA. Fig. 2 presents a scatter-plot of correlations between femoral head chondropathy and score on subscale of HOOS-Symptoms.
Univariable linear regression: crude, unadjusted estimates (regression coefficients 95% CI) of the association between PRO subscales and pathology and demographics.
| Outcome (PRO subscale) | Demographics | Diagnosis at arthroscopy | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (years) | Gender (female) | Body Mass Index (kg/m2) | Femoral head chondropathya | Acetabular chondropathya | Labrum tearsb | Ligamentum teres pathology | Cam morphology | Pincer morphology | ||||
| Mild (grade I–II) | Severe (grade III–IV) | Mild (grade I–II) | Severe (grade III–IV) | Small (1–2 sutures) | Large (3+sutures) | |||||||
| iHOT symptoms and functional limitations | −0.27{−1 to 0.4} | −5.4{−16.6 to 5.8} | −1{−2.3 to 0.2} | −4{−21.9 to 14} | −13.3{−26.4 to −0.3}* | 0.8{−13.2 to 14.9} | −4.2{−18.8 to 10.4} | −3.8{−16.9 to 9.3} | −8.9{−21.7 to 4} | −5.7{−30.6 to 19.3} | 2.4{−8.6 to 13.4} | −1.6{−13.9 to 10.7} |
| iHOT sport and recreation | −0.24{−0.9 to 0.4} | −4{−14.8 to 6.8} | −0.7{−1.9 to 0.5} | 7.9{−9.7 to 25.4} | −6.4{−19.2 to 6.3} | 4.5{−8.9 to 18} | −2{−16 to 12} | −0.03{−12.5 to 12.4} | −9.5{−21.8 to 2.8} | −1.4{−25.4 to 22.6} | −2{−12.5 to 8.6} | −0.5{−12.3 to 11.3} |
| iHOT job related concerns | 0.02{−0.8 to 0.8} | −1{−14.1 to 12} | −1.1{−2.6 to 0.4} | −1.7{−23 to 19.6} | −8.3{−23.8 to 7.2} | −4.5{−20.8 to 11.8} | −3.6{−20.5 to 13.4} | −8.2{−22.6 to 6.2} | −20.1{−34.3 to −6}* | 4.5{−24.5 to 33.4} | −6.6{−19.2 to 6} | −7.9{−22 to 6.1} |
| iHOT social, emotional and lifestyle | 0.13{−0.6 to 0.9} | −3.9{−16 to 8.2} | −1{−2.4 to 0.3} | 0.33{−19 to 19.7} | −13.4{−27.5 to 0.7} | 13{−1.4 to 27.5} | −1.8{−16.8 to 13.2} | 4{−10 to 18} | −7.8{−21.5 to 6} | −16{−42.6 to 10.6} | −0.4{−12.3 to 11.4} | 0.5{−12.8 to 13.7} |
| HOOS symptoms and stiffness | −0.19{−0.8 to 0.4} | −0.7{−10 to 8.6} | −1.4{−2.4 to −0.4}* | −3{−17.7 to 11.6} | −12.1{−22.8 to −1.5}* | −1.7{−13.3 to 9.9} | −0.5{−12.7 to 11.6} | −3.5{−14.5 to 7.4} | −9.1{−19.6 to 1.3} | −0.9{−25.8 to 24} | −3{−17.7 to 11.6} | −9.5{−19.5 to 0.6} |
| HOOS pain | −0.1{−0.7 to 0.4} | −0.8{−9.3 to 7.7} | −0.4{−1.4 to 0.5} | −8.1{−21.4 to 5.2} | −10.6{−20.3 to −0.9}* | 1.1{−9.5 to 11.7} | −0.9{−12 to 10.1} | −9.2{−18.9 to 0.5} | −11.2{−20.4 to −1.9}* | −5.1{−27.8 to 17.5} | 8.2{0.1 to 16.3}* | −2.4{−11.8 to 7} |
| HOOS function and ADL | −0.25{−0.8 to 0.3} | −4{−12.9 to 4.9} | −0.52{−1.6 to 0.4} | −9.6{−23.4 to 4.3} | −12.7{−22.8 to −2.6}* | −0.5{−11.7 to 10.6} | −3.5{−15.2 to 8.2} | −7.3{−17.5 to 3} | −12.8{−22.5 to −3}* | −2.5{−26.4 to 21.5} | 5.7{−2.9 to 14.4} | −3.6{−13.5 to 6.3} |
| HOOS sport and recreation | 0.21{−0.5 to 1} | 2.6{−9 to 14.2} | −1.2{−2.5 to 0.1} | −3.6{−22.2 to 15} | −11.8{−25.3 to 1.8} | 1.6{−13 to 16.1} | −1.4{−16.5 to 13.8} | −11.2{−24.9 to 2.5} | −8.8{−21.8 to 4.2} | −7.1{−38.2 to 23.9} | 7.7{−3.6 to 19} | −1.4{−11.5 to 14.3} |
| HOOS quality of life | −0.27{−1 to 0.5} | 1.2{−10 to 12.5} | −0.9{−2.2 to 0.4} | −2.3{−20.8 to 16.1} | −0.2{−13.6 to 13.3} | 1.3{−12.7 to 15.2} | −4.7{−19.2 to 9.9} | −5.7{−19.5 to 7.5} | −11.4{−24 to 1.2} | −5.4{−35.4 to 24.6} | 4.4{−6.6 to 15.4} | −3.6{−16 to 8.8} |
| Pain on Activity (out of 60) | 0.3{−0.2 to 0.8} | 0.8{−6.7 to 8.3} | 0.1{−0.8 to 1} | 7{−4.9 to 18.9} | 9.9{1.3 to 18.6}* | 2.7{−6.5 to 11.8} | 8.9{−0.7 to 18.4} | 2{−6.4 to 10.5} | 9.9{1.4 to 18.3}* | −2.4{−17 to 12.2} | −0.3{−7.7 to 7} | 3.7{−4.5 to 11.9} |
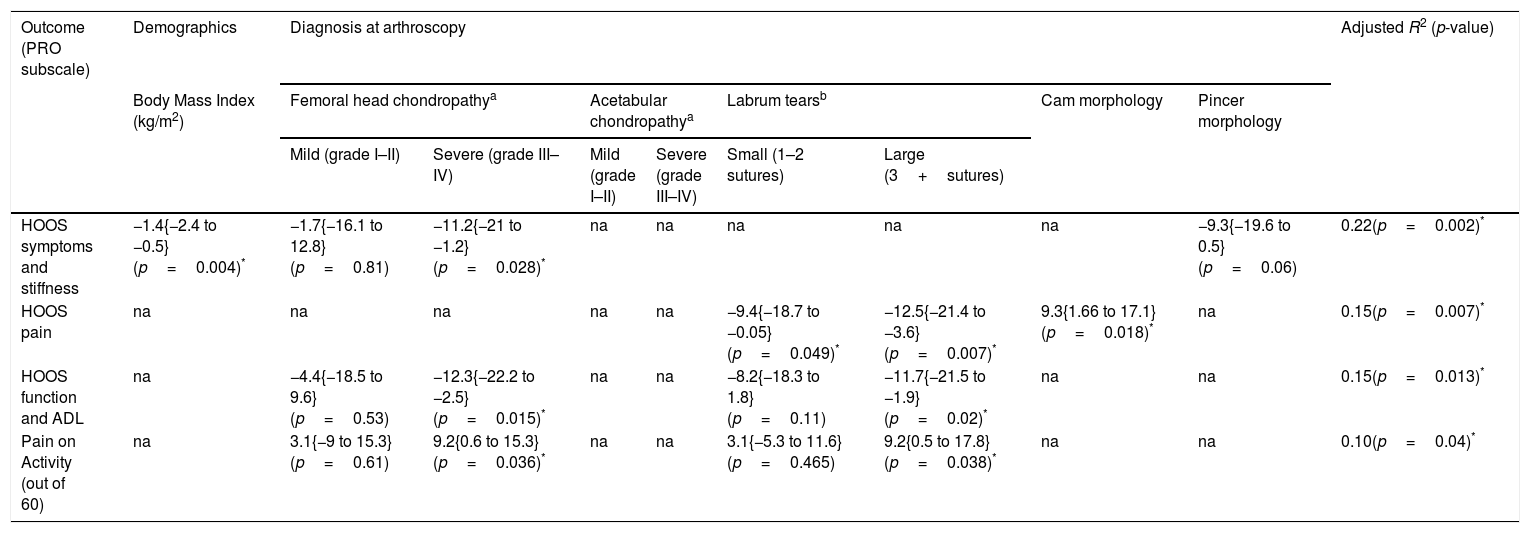
Table 3 presents the adjusted estimates of the association between PRO subscales and two or more categorical variables. The best model was the HOOS-Symptoms subscale, where severe femoral chondropathy scored 11.2 points less than those with no chondropathy, after adjusting for BMI, and the presence of pincer morphology. The iHOT-33 subscales were only associated with a maximum of one pathological finding, so no multivariable models were constructed for this PRO. For the HOOS-Symptoms subscale; severe femoral head chondropathy explained 22% of the variability of symptoms and stiffness, when adjusted for BMI and pincer morphology. Cam morphology and labral tears explained 15% of the variability in HOOS-Pain; severe femoral head chondropathy and large labral tears explained 15% of the variability in HOOS-ADL; while quality of life and sport and recreation scores were not significantly explained by any of the pathological findings. Severe chondropathy and large labral tears explained 10% of the variability in POA.
Multivariable backwards stepwise regression: adjusted estimates (95% CI) of the association between PRO subscales and pathology and demographics.
| Outcome (PRO subscale) | Demographics | Diagnosis at arthroscopy | Adjusted R2 (p-value) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Body Mass Index (kg/m2) | Femoral head chondropathya | Acetabular chondropathya | Labrum tearsb | Cam morphology | Pincer morphology | |||||
| Mild (grade I–II) | Severe (grade III–IV) | Mild (grade I–II) | Severe (grade III–IV) | Small (1–2 sutures) | Large (3+sutures) | |||||
| HOOS symptoms and stiffness | −1.4{−2.4 to −0.5}(p=0.004)* | −1.7{−16.1 to 12.8}(p=0.81) | −11.2{−21 to −1.2}(p=0.028)* | na | na | na | na | na | −9.3{−19.6 to 0.5}(p=0.06) | 0.22(p=0.002)* |
| HOOS pain | na | na | na | na | na | −9.4{−18.7 to −0.05}(p=0.049)* | −12.5{−21.4 to −3.6}(p=0.007)* | 9.3{1.66 to 17.1}(p=0.018)* | na | 0.15(p=0.007)* |
| HOOS function and ADL | na | −4.4{−18.5 to 9.6}(p=0.53) | −12.3{−22.2 to −2.5}(p=0.015)* | na | na | −8.2{−18.3 to 1.8}(p=0.11) | −11.7{−21.5 to −1.9}(p=0.02)* | na | na | 0.15(p=0.013)* |
| Pain on Activity (out of 60) | na | 3.1{−9 to 15.3}(p=0.61) | 9.2{0.6 to 15.3}(p=0.036)* | na | na | 3.1{−5.3 to 11.6}(p=0.465) | 9.2{0.5 to 17.8}(p=0.038)* | na | na | 0.10(p=0.04)* |
Most of the study population were classified as having labral pathology (91%) and degrees of acetabular chondropathy (76%). Cam morphology requiring osteoplasty was present in more than half the study population (58%) and the finding of large labral tears (28%) and femoral head chondropathy (31%) were also common, with severe femoral head chondropathy present in 21% of the study population. The strongest association between pathology and PROs was 22% of variability in the HOOS-Symptoms subscale being associated with severe femoral head chondropathy when adjusted for BMI and the presence of pincer morphology. Although the severe femoral head pathology and large labral tears noted during arthroscopy were related to lower scores in pre-operative PROs, their relatively low degree of association refutes the hypothesis that people with more severe pathologies would show significantly poorer PRO and pain scores prior to surgery.
The prevalence of severe femoral head chondropathy in the current study was similar to those reported previously (22%, N=100, mean age=34 years,35 28% of hips younger than 30 years27). However, other studies have reported much lower prevalence, between 7% (grade IV only, N=122, mean age=40.6)36 and 16% (N=2092, mean age=35 years).37 Chondral pathology at time of surgery24 affecting the acetabulum was more commonly reported in those undergoing hip arthroscopy with reported prevalence ranging from 42% (N=595, mean age=38)38 to 97%.35 It is possible that the high percentage of military participants (88%) in this study population affected the high prevalence of severe femoral head chondropathy (21%) and acetabular chondropathy (76%) at a relatively young age (mean=31 years). This may reflect the high mechanical loading associated with military life which also may induce differences in the subjective reporting of disability. It is also worth noting that potential participants with severe degenerative changes evident on imaging were not considered for arthroscopy. This suggests that the routinely used imaging techniques were ineffective at identifying all cases of severe chondropathy and indicates the importance of improved preoperative imaging assessment of cartilage status to help determine the best candidates for hip arthroscopy.10 As the average age of the participants in this study was younger than others referenced,35–37 clinicians should be aware of the high prevalence of severe femoral head chondropathy (21%) and large labral tears (28%) that are not obvious on pre-surgery imaging in relatively-young, military hip pain populations.
At most, only 22% of variability in the HOOS-Symptoms subscale was associated with severe femoral head chondropathy prior to surgery when adjusted for BMI and the presence of pincer morphology. Severe femoral head chondropathy and large labral tears accounted for 15% of the variability in the subscale of Function and ADL (p=0.01) as well as 10% of the POA variability (p=0.04). The subscales most associated with large labral pathology and severe femoral head chondropathy were those with a higher component of movement-related questions, particularly emphasizing hip flexion and extension. Movement questions constitute 83% of the POA and 85% of the HOOS-ADL subscale with the latter over-lapping 5/6 of the POA questions. The HOOS-Symptoms and iHot-33-Symptoms subscales were most associated with severe femoral head chondropathy and contain only 40–60% of questions related to flexion/extension movement. They also contain more questions regarding stiffness, a symptom traditionally associated with OA.39 Large labral tears were associated with the HOOS-Pain and iHot-33-Job subscales which contain 50% and 75% movement related questions respectively. These associations may relate to compression or shearing of the larger labral tears during end of range movement, an act provocative of hip pain symptoms. Milder forms of labral and chondral pathology may be potentially less aggravated by end range hip movement so are not as strongly associated with PROs. The PRO subscales that involve psychological responses (iHot-33-QOL and HOOS-QOL) or higher levels of sports activity (iHot-33-Sport and HOOS-Sport) are least associated with pathology. It is possible that quality of life and sports participation were greatly reduced across all the pre-operative participants, regardless of the severity of pathology, and therefore not associated with distinct pathology types.
The impact of femoral head chondropathy severity on pain and function has been reported in post-operative hip populations.14 Severe chondropathy was associated with worse pain and function at 18 months post surgery14 and had a negative effect on clinical outcome10,11 with grade IV changes on the femoral head deemed unlikely to respond to joint-preserving treatment attempts used in arthroscopy.40 In this study, 10–22% of the variability of the HOOS-Symptoms subscale (p=0.002), HOOS- Function subscale (p=0.01), and the POA (p=0.04) was associated with severe femoral head chondropathy. The greater negative association of severe femoral head chondropathy with symptoms and function PROs concur with the findings of post-operative studies.14 This study found that large labral tears were negatively associated with PRO response for the subscales of iHot-33-Job and HOOS-ADL. Lower scores in the HOOS-Pain subscale were also associated with a combination of small and large labral tears and cam morphology (R2=0.15, p=0.007). Patients with labral tears often have underlying bony anomalies,25 which might explain the relationship with pain.
The pre-operative HOOS-ADL (62.7) and HOOS-Sport (44.4) in this study are similar to those reported by Stake et al.22 (69.9 and 41.9 respectively).22 While PROs give an indication of hip pain and function, they do not measure actual hip functional performance.19 Their usefulness lies in presenting a patient-focused perspective of outcomes important to the patient20 rather than reflecting the extent of intra-articular pathology. In this study, the more severe forms of chondral pathology and large labral tears accounted for up to 22% of the variability in PRO response. This suggests that at least 78% of variability arose from other factors and may benefit from non-surgical management. There is some evidence that risks potentially outweigh the benefits for arthroscopic meniscus debridement in OA knees.41,42 The same may be true of labral debridement and techniques addressing degenerative cartilage change in the hip joint. Patient factors, including mental health,43,44 activity level, sex, and smoking, are more predictive of baseline hip pain (as measured by HOOS) and function than intra-articular findings for FAI sufferers.30 Non-pathological features such as BMI, strength and range of movement may also influence PRO scores. Similar to the knee, non-surgical treatment strategies to address labral tears and OA change may help restore optimal joint mechanics and reduce load on damaged structures.45 Non-surgical interventions may include strengthening hip muscle,46 manual therapy techniques to improve joint range of motion and reduce impingement,47,48 movement retraining, neuromuscular programmes to improve gait biomechanics, and weight control.49
LimitationsThe present study has limitations. There is potential for selection bias. Eighty-eight percent of participants were serving military, an occupation characterized by high levels of physical load, thus limiting external validity of these results. This may have influenced the incidence of severe femoral head chondropathy, large labral tears and the reported reductions in physical capacity. There is some possibility of measurement bias, leading to misclassification or misdiagnosis according to other criteria. For example, diagnosis of FAI and labral lesions was based on the presence and degree of surgical repair determined by the clinical expertise of the treating surgeons. Radiographic measures such as alpha angles, lateral/anterior centre edge angles and Tonnis grade were not used to classify pathology in this study as not all participants underwent imaging compatible with the measurement of these variables and both FAI morphologic features and labral injuries are common in asymptomatic patients.50 Multiple and different combinations of pathologies were present in many of the participants. This may have affected the associations of individual pathologies to patient reported pain and function. There may also have been limitations to the classification of labral tears by the number of sutures used in repair. While size in millimetres and/or clock face location could have been employed, classifying by sutures required for repair provides a practical indication of the extent of the lesion.
ConclusionWithin this population, severe femoral head chondropathy and large labral tears were a relatively common finding during hip arthroscopy and were associated with poorer pre-operative scores on the HOOS-Symptoms and HOOS-ADL subscales, as well as the POA. Movement-related questions make up a high percentage of these subscales. The results of this study are useful to educate hip pain sufferers that degree of pathology seen in arthroscopy or clinical imaging is not necessarily indicative of pain or disability, and that much of the variability in pain and function is explained by other potentially modifiable factors.
FundingThe authors certify that they have no affiliations with or financial involvement in any organization or entity with a direct financial interest in the subject matter or materials discussed in the article.
Conflicts of interestThe authors declare no conflicts of interest.
The authors would like to acknowledge Brisbane surgeons Patrick Weinrauch and Gauguin Gamboa for their support of this study. Matthew Freke is supported in his research by the Australian Defence Force.