Few studies have demonstrated postural abnormalities in patients with chronic obstructive pulmonary disease - when compared with healthy individuals. However, none of these studies have compared postural abnormalities in different phenotypes of chronic obstructive pulmonary disease.
ObjectiveTo compare the thoracic posture between two phenotypes of chronic obstructive pulmonary disease (emphysema and chronic bronchitis) with healthy individuals.
MethodsForty individuals with chronic obstructive pulmonary disease (20 with chronic bronchitis, 67±3.5 years, 20 with emphysema, 67.7±4 years) and 20 age-matched healthy individuals (67.3±3.9 years) underwent postural assessment which was performed using photogrammetric measurements of head protraction, shoulder protraction, thoracic kyphosis angle, coronal shoulder angle, and scapular elevation.
ResultsSignificant differences were found amongst the groups in protraction of head (emphysema vs. chronic bronchitis, mean difference=7.63°, 95% confidence interval [CI]=2.10, 13.15°; emphysema vs. healthy, 7.91°, 95% CI=2.38, 13.43°), protraction of shoulder (emphysema vs. healthy, 13.69°, 95% CI=6.96, 20.43°; chronic bronchitis vs. healthy, 8.11°, 95% CI=1.38, 14.85°), thoracic kyphosis (emphysema vs. healthy, −11.59°, 95% CI=−17.26, −5.92°; chronic bronchitis vs. healthy, −6.75°, 95% CI=−12.41, −1.08°), coronal shoulder angle (emphysema vs. chronic bronchitis, 1.01°, 95% CI=.22, 1.80°; emphysema vs. healthy, 1.59°, 95% CI=.80, 2.38°) and scapular elevation (emphysema vs. chronic bronchitis, =.74cm, 95% CI=.34, 1.15cm; emphysema vs. healthy, .99cm, 95% CI=.59, 1.40cm).
ConclusionPeople with emphysema show greater degree of postural malalignments in terms of head and shoulder protraction, thoracic kyphosis, symmetry of shoulders and scapular elevation than patients with chronic bronchitis and age-matched healthy individuals. These observations emphasize the importance of postural assessment in individuals with chronic obstructive pulmonary disease, particularly if they are emphysematous.
According to the World Health Organization (WHO), chronic obstructive pulmonary disease (COPD) is a progressive respiratory disease that affects 251 million people worldwide.1 WHO estimates that about 65 million people have moderate to severe COPD.2 In India, there are about 30 million people with COPD.3 COPD can be divided into two clinical phenotypes: emphysema and chronic bronchitis.4 Recognizing different phenotypes within COPD is clinically relevant due to their differential response to therapeutic intervention.5 Chronic bronchitis is clinically defined as a productive cough occurring daily at least for three months and for two successive years, whereas, pulmonary emphysema is termed as permanent abnormal enlargement of any part of the acinus accompanied by destruction of respiratory tissue.6
Neck pain, chest pain, and upper and lower back pain are common in people with COPD. Although the exact cause of pain in the above mentioned spinal regions is not clear, postural abnormalities have been hypothesized to be inducing excessive strain on the musculoskeletal system due to overloading of the respiratory muscles in patients with COPD.7–9
While breathing, people with advanced COPD activate the muscles of forced inspiration in addition to the other primary muscles of inspiration. This may result in muscle shortening, reduced flexibility and alterations in head position, shoulder girdle, thoracic spine and pelvic spine.7–9 The thorax typically shows a barrel-shaped appearance, which alters the geometry of the lungs during inspiration. The diaphragm flattens and remains abnormally low in the thorax. The change in the length–tension relationship of the diaphragm compromises the production of force, even at rest, and the ventilation appears to be labored.10
A few studies done in the past have demonstrated the existence of postural abnormalities in patients with COPD. Gonçalves et al.7 compared the postural alignment between patients with COPD and their healthy counterparts.7 They found increased thoracic kyphosis and anterior tilting of pelvis in patients with COPD when compared with apparently healthy individuals.
In another study Pachioni et al.11 observed postural changes in COPD and healthy individuals and concluded that these changes could be associated with the disease itself. A study conducted by Dias et al.12 showed that patients with COPD had more scapular elevation when compared with healthy individuals. They, however, did not find any significant postural differences in the thoracic spinal region and the cervical spinal region between the two groups. They concluded that changes in the scapula alignment might have occurred due to hyperinflation of the lungs.
The abovementioned studies have already evaluated postural abnormalities in patients with COPD. However, the difference in postural abnormalities between the two phenotypes of COPD (chronic bronchitis and emphysema) is still unknown. Therefore, the primary objective of this study is to compare the postural abnormalities between individuals with either condition and age-matched healthy individuals. Additionally, we also aimed to compare the pulmonary function tests and the functional capacity between the two phenotypes of COPD and age-matched healthy individuals.
MethodsStudy designA cross-sectional exploratory study was conducted after receiving approval from the Institutional Ethics Committee of Jamia Millia Islamia, New Delhi, and Metro Hospital, Noida, Uttar Pradesh, India (no. 16/9/144/JMI/IEC/2017). All the participants signed a written informed consent. The study was reported following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.13
ParticipantsA total of 60 male individuals aged more than 60 years (20 in each group, i.e., individuals with emphysema, with chronic bronchitis and healthy individuals) participated in the study. Though female individuals were also considered initially, due to their reluctance in participating in the photographic procedures for the present study which involved baring the upper body, we had to exclude them. Only those who were diagnosed with severe to very severe COPD according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) classification - Forced Expiratory Volume in first second (FEV1) ≤50% predicted, FEV1/FVC (Forced Vital Capacity) ≤.70, and radiographic changes were included in the study. The age-matched healthy individuals had normal pulmonary functions and normal spirometry (FEV1/FVC ≥.7; FEV1 ≥80% of predicted, FVC ≥80% of predicted). Additional inclusion criteria were chronic bronchitis which has been diagnosed when the patients with COPD produced cough and sputum on most of the days for a minimum of 3 months per year for the last 2 years14; emphysema has been diagnosed according to CT scanning15; and the patient has been able to walk independently without any assistive device. The exclusion criteria were clinically unstable patients; or patients who had exacerbation during the study; patients with recent thoracic, abdominal, or spinal surgeries; patients with congenital musculoskeletal deformities; history of idiopathic scoliosis; patients who had cognitive problems; patients with restrictive lung disorders; patients with neurological disorders that could have affected posture and lung functions; and patients with shoulder or back pain.
Outcome measuresDemographic information and information about the current respiratory medicines used by the patients were collected. Anthropometric, 6MWD (six-minute walk distance), and pulmonary function data (using spirometry) were collected, followed by the measurement of postural angles. Same evaluator measured all the measures. The postural assessments were carried out randomly to minimize the order effect.
Six-minute walk test (6MWT)The 6MWT was performed according to the ERS/ATS guidelines.16 Each subject was asked to walk as much as possible on a course of 30m in 6min. To eliminate the learning effect, two 6MWTs were performed with a 30-min rest period, and the best 6MWD was recorded. Verbal encouragement and instructions were given to the individuals in the standardized form. The following prediction equation was used to calculate the percentage of predicted six-minute walk distance: 6MWD (in m)=[(7.57×height in cm)−(5.02×age)−(1.76×weight in kg)]−309m.17
SpirometryA digital spirometer was used to assess pulmonary function. It was calibrated prior to the test, according to American Respiratory Society and European Respiratory Society standards.18 COPD classification was determined according to the GOLD.6
ProcedureThe postural assessment was performed using photogrammetry using UTHSCSA image tool software (University of Texas Health Science Center at San Antonio) at the Human Performance Laboratory, Jamia Millia Islamia, New Delhi, and at Metro Hospital, Noida, India. The subjects wore a pair of Bermuda without shoes and were bare from waist up. Straw markers were used as passive markers to label anatomical points based on the previous studies: tragus of the ear, seventh cervical spinous process (C7), center of lateral shoulder, centroid of scapula (the centroid of the three digitized scapular points: the root of the spine of the scapula on the medial border of the scapula, the inferior angle of the scapula, and the acromion at the acromioclavicular joint),19 the virtual C7 (horizontal line passing across C7 markers), the 12th thoracic spinous process (T12) and the coracoid processes of the scapulae.12 Using an 18 MP DSLR camera (Canon EOS 1300D), photographs were taken by positioning the subject 3m away from the lens of the camera, which was set at a height of about half of the subject. The individuals were asked to stand against the wall and look straight toward the camera with their habitual posture, and turn both left and right sides for lateral photographs. For the posterior view, the individuals were asked to stand facing the wall and look straight comfortably. Anterior, posterior, lateral full-figure photographs of each subject were taken. The photographs were then imported into the UTHSCSA software installed on a computer to obtain the values of desired angles, which then were exported to a Microsoft Excel spreadsheet.20 Following angles were measured thrice and an average of the three readings of each measure was taken for data analysis.
- a)
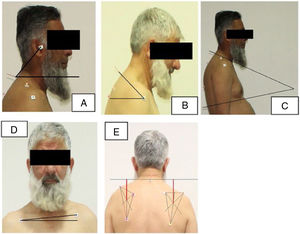
Protraction of the head: The angle formed by the intersection of a straight line drawn over the midpoint of the tragus of the ear and the virtual C7 marker (seventh cervical spinous process) with a straight horizontal line intercepting the virtual C7 on the sagittal plane.12 A lesser value of angle shows a more forward protraction of the head in relation to the virtual C7 (Fig. 1A).
Figure 1.Pictorial representation of postural variables. (A) Protraction of head angle (between tragus, C7 and horizontal), (B) protraction of shoulder angle (between lateral shoulder, C7 and horizontal), (C) thoracic kyphosis angle (between T12 and C7), (D) coronal shoulder angle (between coracoids and horizontal), and (E) scapular elevation (between virtual C7 and centroid of scapula).
- b)
Protraction of shoulder: A horizontal line was drawn through the lateral shoulder and another line was drawn from the C7 marker to lateral shoulder. The angle of the intersection was calculated in degrees.21 A lesser angle indicates a more forward position of shoulder in relation to C7 markers, and it represents the degree of roundness of the shoulder (Fig. 1B).
- c)
Thoracic kyphosis angle: The lines drawn from T12 (thoracic 12th spinous process) and C7 markers when intersected together form the thoracic kyphosis angle or thoracic flexion angle. A lesser value indicates less kyphosis22 (Fig. 1C).
- d)
Coronal shoulder angle: The angle between a horizontal line and a line joining the two-coracoid process of shoulders. Its normal value is 180°. It is used to identify the symmetry of both shoulders21 (Fig. 1D).
- e)
Scapular elevation: It is the linear vertical distance between virtual C7 and centroid of the scapula. A lesser distance between the markers indicates greater scapular elevation12 (Fig. 1E).
To evaluate the test–retest reliability of the postural angles measured by photogrammetric method, a subsample of 30 patients with COPD were randomly selected from 40 COPD participants. These individuals were recalled for a second postural assessment after 2 days and their posture were measured by the same investigator. The test-retest reliability for all postural indices demonstrated ICC2,1 values of .75–.99 and SEM values of 0.55–1.42° and 0.05cm.
Data analysisData were analyzed using one-way ANOVA to find out differences between the groups. When a significant difference was found, a Tukey's test was employed as a post hoc analysis to conduct multiple comparisons of the variables between the groups.
ResultsThe descriptive statistics of patients with emphysema and with chronic bronchitis as well as the age-matched healthy individuals are presented in Table 1. All three groups were similar in age and height while they differed in weight and BMI. The spirometry result shows significant differences among all three groups in FEV1 percentage predicted (emphysema vs. healthy, mean difference=71.80%, p<0.001; chronic bronchitis vs. healthy, mean difference=64.85%, p<0.001) and FEV1/FVC% ratio (emphysema vs. healthy, mean difference=61.65%, p<0.001; chronic bronchitis vs. healthy, mean difference=56.40%, p<0.001). The functional capacity (6MWD and 6MWD percentage predicted) measured by 6MWT also showed significant differences among the groups (6MWD: emphysema vs. chronic bronchitis, mean difference=120.30m, p=0.002; emphysema vs. healthy, mean difference=203.65m, p<0.001; chronic bronchitis vs. healthy, mean difference=83.35m, p<0.040 and 6MWD percentage predicted: emphysema vs. chronic bronchitis, mean difference=21.70%, p=0.001; emphysema vs. healthy, mean difference=34.95%, p<0.001).
Demographic characteristics for individuals with emphysema, chronic bronchitis and healthy control individuals.
| Dependent variable | Emphysema(mean±SD)(n=20) | Chronic bronchitis(mean±SD)(n=20) | Healthy controls(mean±SD)(n=20) | (I) group | (J) group | Mean difference (I–J) | p value | 95% confidence interval | |
|---|---|---|---|---|---|---|---|---|---|
| Lower bound | Upper bound | ||||||||
| Age (years) | 68±4.03 | 67±3.5 | 67±3.93 | Chronic bronchitis | Emphysema | −.70 | 1.000 | −3.70 | 2.30 |
| Healthy control | Chronic bronchitis | .25 | 1.000 | −2.75 | 3.25 | ||||
| Healthy control | Emphysema | −.45 | 1.000 | −3.45 | 2.55 | ||||
| Height (cm) | 163.4±7.4 | 166.9±1.5 | 164.3±5.8 | Chronic bronchitis | Emphysema | 3.55 | 0.143 | −.78 | 7.88 |
| Healthy control | Chronic bronchitis | −2.65 | 0.409 | −6.98 | 1.68 | ||||
| Healthy control | Emphysema | .90 | 1.000 | −3.43 | 5.23 | ||||
| Weight (kg) | 55.1±17.07 | 67.4±67.4 | 68.2±10.7 | Chronic bronchitis | Emphysema | 12.35* | 0.040 | .41 | 24.29 |
| Healthy control | Chronic bronchitis | .75 | 1.000 | −11.19 | 12.69 | ||||
| Healthy control | Emphysema | 13.10* | 0.027 | 1.16 | 25.04 | ||||
| BMI (kg/m2) | 20.3±4.7 | 24.1±5.8 | 25.2±3.5 | Chronic bronchitis | Emphysema | 3.81* | 0.045 | .06 | 7.55 |
| Healthy control | Chronic bronchitis | 1.09 | 1.000 | −2.64 | 4.84 | ||||
| Healthy control | Emphysema | 4.91* | 0.006 | 1.16 | 8.65 | ||||
| 6MWD (m) | 256±144.9 | 376±84.4 | 460±61.4 | Chronic bronchitis | Emphysema | 120.30* | 0.002 | 39.85 | 200.75 |
| Healthy control | Chronic bronchitis | 83.35* | 0.040 | 2.90 | 163.80 | ||||
| Healthy control | Emphysema | 203.65* | <0.001 | 123.20 | 284.10 | ||||
| 6MWD (% predicted) | 48.90±26.4 | 70.6±14.3 | 83.8±10.2 | Chronic bronchitis | Emphysema | 21.70* | 0.001 | 7.38 | 36.02 |
| Healthy control | Chronic bronchitis | 13.25 | 0.079 | −1.07 | 27.57 | ||||
| Healthy control | Emphysema | 34.95* | <0.001 | 20.63 | 49.27 | ||||
| FEV1 (% predicted) | 31.7±9.9 | 38.6±9.1 | 103.5±22.4 | Chronic bronchitis | Emphysema | 6.95 | 0.454 | −4.84 | 18.74 |
| Healthy control | Chronic bronchitis | 64.85* | <0.001 | 53.06 | 76.64 | ||||
| Healthy control | Emphysema | 71.80* | <0.001 | 60.01 | 83.59 | ||||
| FEV1/FVC % | 51.40±12.2 | 56.6±18.1 | 113.05±10.1 | Chronic bronchitis | Emphysema | 5.25 | 0.717 | −5.63 | 16.13 |
| Healthy control | Chronic bronchitis | 56.40* | <0.001 | 45.52 | 67.28 | ||||
| Healthy control | Emphysema | 61.65* | <0.001 | 50.77 | 72.53 | ||||
FEV1%, percent of predicted of forced expiratory volume in one second; 6MWD, six-minute walk distance; FEV1/FVC %, forced expiratory volume in one second/forced vital capacity; SD, Standard deviation; BMI, Body Mass Index.
Postural alignments were significantly different between patients with emphysema and those with chronic bronchitis and healthy individuals. Significant differences were found between the chronic bronchitis and healthy controls groups in thoracic kyphosis (p=0.014) and protraction of shoulder (p=0.013).
Table 2 shows the postural outcomes for all groups. All postural variables were significantly different in people with emphysema when compared with the age-matched healthy controls. In addition, the emphysema group, when compared with the chronic bronchitis group, showed significant difference of 7.63° in head protraction (p=0.004), 1.01° in shoulder coronal angle (p=0.008), and 0.74cm in scapular elevation (cm p<0.001). The results showed that emphysema group demonstrated more head protraction and greater scapular elevation than the chronic bronchitis and healthy control groups.
Comparison of posture between emphysema, chronic bronchitis and healthy individuals.
| Postural variable | Emphysema(mean±SD)(n=20) | Chronic bronchitis(mean±SD)(n=20) | Healthy controls(mean±SD)(n=20) | (I) group | (J) group | Mean difference (I–J) | p value | 95% confidence interval | |
|---|---|---|---|---|---|---|---|---|---|
| Lower bound | Upper bound | ||||||||
| Head protraction (°) | 40.2±7.8 | 47.8±5.2 | 48.1±7.8 | Chronic bronchitis | Emphysema | 7.63* | 0.004 | 2.10 | 13.15 |
| Healthy control | Chronic bronchitis | .28 | 1.000 | −5.24 | 5.80 | ||||
| Healthy control | Emphysema | 7.91* | 0.002 | 2.38 | 13.43 | ||||
| Shoulder protraction (°) | 29.16±7.2 | 34.7±8.6 | 42.8±9.8 | Chronic bronchitis | Emphysema | 5.58 | 0.137 | −1.15 | 12.31 |
| Healthy control | Chronic bronchitis | 8.11* | 0.013 | 1.38 | 14.85 | ||||
| Healthy control | Emphysema | 13.69* | <0.001 | 6.96 | 20.43 | ||||
| Thoracic kyphosis (°) | 53.15±9.1 | 48.3±2.9 | 41.5±8.1 | Chronic bronchitis | Emphysema | −4.84 | 0.118 | −10.51 | .82 |
| Healthy control | Chronic bronchitis | −6.75* | 0.014 | −12.41 | −1.08 | ||||
| Healthy control | Emphysema | −11.59* | <0.001 | −17.26 | −5.92 | ||||
| Coronal shoulder angle (°) | 176.7±.80 | 177.8±1.1 | 178.3±1.04 | Chronic bronchitis | Emphysema | 1.01* | 0.008 | .22 | 1.80 |
| Healthy control | Chronic bronchitis | .58 | 0.228 | −.21 | 1.37 | ||||
| Healthy control | Emphysema | 1.59* | <0.001 | .80 | 2.38 | ||||
| Scapular elevation (cm) | 3.3±.46 | 4.1±.48 | 4.36±.60 | Chronic bronchitis | Emphysema | .74* | <0.001 | .34 | 1.15 |
| Healthy control | Chronic bronchitis | .25 | 0.398 | −.15 | .65 | ||||
| Healthy control | Emphysema | .99* | <0.001 | .59 | 1.40 | ||||
SD, Standard deviation.
This study showed that patients with emphysema possess a greater degree of postural malalignments in terms of head protraction, shoulder protraction, thoracic kyphosis, symmetry of shoulders and scapular elevation than patients with chronic bronchitis and age-matched healthy individuals.
In the present study, we observed that patients with emphysema had worse pulmonary function (FEV1) than patients with chronic bronchitis and age-matched healthy controls. Therefore, patients with emphysema exhibited greater difference (11.6) in thoracic kyphotic angle when compared with normal healthy individuals. Garreau de Loubresse and Wolff23 have observed that thoracic kyphotic angle is closely associated with lung function. Previous studies7,11 demonstrated that patients with COPD have exaggerated kyphotic posture than healthy controls. Furthermore, Lee et al.9 reported more thoracic kyphotic values in patients with COPD than healthy individuals 51.8 vs. 39.1 respectively. In our study, patients with emphysema demonstrated more thoracic kyphotic changes than reported by Gonçalves et al.7 in people with COPD. These changes could be due to the fact that the individuals recruited for our study were more severely impaired. In contrast, Dias et al.12 did not find any difference in the thoracic kyphotic angle between COPD and healthy individuals.
Shoulder protraction is commonly seen in patients with COPD, which may be due to increased forward leaning posture as a result of dyspnea.24 Ghanbari et al.25 observed that the degree of forward shoulder protraction (FSP) increases due to decrease in the respiratory values of forced vital capacity (FVC), vital capacity (VC), and expiratory reserve volume (ERV). Muscular imbalance is also seen in FSP, which may adversely affect the volume and pressure of the lung.25 In the present study, patients with emphysema exhibited more protraction (lesser angle indicates more protraction) of shoulders than patients with chronic bronchitis and age-matched healthy individuals. Raine and Twomey21 reported a greater tendency of protraction of shoulder with aging. The results of the present study suggest that postural alteration is more evident in patients with emphysema than in patients with chronic bronchitis when compared to healthy individuals.
The patients with emphysema who participated in our study demonstrated greater protraction of head than the individuals in the remaining two groups. The accessory neck muscles are utilized for ventilation because of the poor activation of the diaphragm in patients with COPD26 which could be the reason for the protraction of the head. A faulty posture involving the head to be in a forward position, which decreases the efficiency of the neck muscles as a result of hyperactivation of sternocleidomastoid has been observed.27 Additionally, we observed a 7.9° difference in the protraction of the head in patients with emphysema when compared with controls. These findings are in contrast with previous findings of Morais et al.28 (p=0.38) and Gonçalves et al.7 (p=0.63), who did not report any significant differences between patients with COPD and health controls. However, they do not describe the two phenotypes of COPD separately, and hence their results are different. Our results for protraction of head differ from previous results of Raine and Twomey,21 who reported 44° of protraction of the head for healthy individuals aged more than 55 years. However, their study was conducted approximately 20 years ago when lifestyle of people was different that present times. The differences in the values of protraction of head angle, as found in the present study, can be attributed to lifestyle changes, for example, use of smartphones and laptops now-a-days make a forward head posture more common.20
It may be assumed that long-standing emphysema could have increased thoracic kyphosis. Protraction of the head, occurring due to increased thoracic curvature as a compensatory mechanism to maintain body posture and balance, can affect the body's line of gravity29 which has to be maintained within the base of support. In patients with COPD, reduction of the pectoralis minor muscle's length in the non-dominant shoulder and an increase in protraction of the head is associated with a decrease in FEV1.28
In this study, significantly greater scapular elevation in patients with emphysema (4.36cm) was observed when compared with age-matched healthy controls (3.36cm) and patients with chronic bronchitis (0.75cm). However, we did not observe any significant differences in scapular elevation between patients with chronic bronchitis and age-matched healthy controls. This observed difference in our study was similar to the findings of a study conducted by Dias et al.12 Hyperinflation is a clinically relevant feature in COPD, which contributes to dyspnea.30 Cassart et al.31 reported that hyperinflation leads to reduction in both lung volume and thoracic cage expansion. They explained that these changes in respiration can result in the upward movement of ribs during inspiration and in the formation of a circular thoracic cage due to the overuse of the accessory muscles instead of the primary muscles of respiration. The combined motion of the sternoclavicular joint and the acromioclavicular joint helps the clavicle to elevate at the sternoclavicular joint and inferiorly rotate at the acromioclavicular joint respectively.10 These biomechanical alterations could be the possible reason for greater scapular elevation in patients with COPD in the present study.
The coronal shoulder angle has commonly been used as a criterion to measure the shoulder asymmetry in the coronal plane.21 In the present study, patients with emphysema demonstrated a 1.01° and 1.58° significantly greater asymmetry in the coronal shoulder angle when compared with patients with chronic bronchitis and healthy controls, respectively. Since patients with emphysema demonstrated greater protraction of head and shoulder, and more kyphosis than the other two groups, the finding of coronal shoulder angle being the least in patient in emphysema group is obvious (i.e., since patients with emphysema had poor overall posture than the chronic bronchitis and healthy control groups, they had more asymmetry in the frontal plane too).
Limitations of the studyDue to lack of female participation in our study, we cannot generalize the findings of this study to female patients with COPD. We have used a static postural assessment in our study; however, a dynamic postural assessment would have been more informative and could have provided a closer look at minute postural changes in patients with COPD during activity.
ConclusionIndividuals with emphysema presented more postural abnormalities than those with chronic bronchitis and age-matched healthy adults. Furthermore, the magnitude of airflow limitation was associated with postural impairments in the emphysema phenotype of patients with COPD. These observations emphasize the importance of including a postural assessment of patients with moderate to severe COPD, particularly if they have emphysema phenotype. The role of incorporating a specific type of postural muscle training strategies within the framework of pulmonary rehabilitation in this population also needs to be explored.
Conflicts of interestThe authors declare no conflicts of interest.