Shoulder injuries are common in individuals who use wheelchairs.
ObjectivesThis study investigated the presence of mechanical pain hypersensitivity and trigger points in the neck-shoulder muscles in elite wheelchair basketball players with/without shoulder pain and asymptomatic able-bodied elite basketball players.
MethodsEighteen male wheelchair basketball players with shoulder pain, 22 players without shoulder pain, and 20 able-bodied elite male basketball players were recruited. Pressure pain thresholds were assessed over C5-C6 zygapophyseal joint, deltoid muscle, and second metacarpal. Trigger points in the upper trapezius, supraspinatus, teres minor, infraspinatus, teres major, latissimus dorsi, subscapularis, pectoralis minor, pectoralis major and deltoid muscles were also examined.
ResultsWheelchair basketball players with shoulder pain showed lower pressure pain thresholds over the C5-C6 joint and second metacarpal than elite wheelchair basketball players without pain (between-groups differences: 1.1, 95%CI 0.4, 1.8 and 1.8, 95%CI 0.8, 2.8, respectively) and able-bodied basketball players without pain (between-groups differences: 0.8, 95%CI 0.4, 1.2; 1.6, 95%CI 0.8, 2.4, respectively). The mean number of myofascial trigger points for wheelchair basketball players with unilateral shoulder pain was 4.8±2.7 (2±1 active, 2.9±2.2 latent). Wheelchair basketball players and able-bodied basketball players without shoulder pain exhibited a similar number of latent trigger points (2.4±2.0 and 2.4±1.8, respectively). Wheelchair basketball players with shoulder pain exhibited higher number of active myofascial trigger points than those without pain (either with or without wheelchair), but all groups had a similar number of latent trigger points (P<0.05).
ConclusionsThe reported mechanical pain hypersensitivity suggests that active trigger points may play a role in the development of shoulder pain in elite male wheelchair basketball players.
Shoulder pain is probably the most common symptom experienced by both adults1 and adolescent2 athletes practicing sports requiring frequent upper extremity use such as judo, basketball, or handball. There is also epidemiological data suggesting that the shoulder is the most common anatomical location of symptoms in wheelchair athletes.3 In fact, it has been shown that as many as 45% of the general population of wheelchair users will exhibit joint degeneration, rotator cuff injury, or muscular conditions affecting the shoulder.4,5 Further, subjects who participate in wheelchairs sports are significantly more likely to experience upper extremity symptoms than the general population using wheelchair.6 The prevalence of shoulder pain can reach up to 76% in wheelchair athletes.7
One potential reason for the presence of shoulder pain in this population could be related to the repetitive overuse of the upper extremity associated with a quick use of wheelchairs combined with the frequent use of the upper extremity, e.g., basketball. Although it has been observed clinically that 52% of women participating in wheelchair basketball (WCB) experienced shoulder pain, a recent study has reported that male WCB players are at higher risk than females.8 A recent review concluded that the source of shoulder pain in wheelchair athletes is poorly understood and is likely multifactorial in nature; therefore, further research is needed to better understand this common and debilitating condition in wheelchair athletes.9 One commonly reported contributor to shoulder pain is the presence of trigger points (TrP) in musculature that surround the shoulder.10 Trigger points are sensitive spots of taut bands within skeletal muscles, which can be either active or latent.11 Trigger points are considered active if they elicit referred pain, which reproduces the patient's symptoms during mechanical stimulation11 or, when subjected to excessive stress similar to activities performed by a patient. Conversely, latent TrPs do not reproduce the patient's symptoms when they are mechanically stimulated.11 Two studies have found that the referred pain elicited by active TrPs within the supraspinatus, infraspinatus, subscapularis, and upper trapezius reproduced the symptoms that many subjects with shoulder pain experience.12,13 Another study found the presence of active TrPs in elite swimmers with shoulder pain in a similar musculature.14 However, to the best of the author's knowledge, no study has reported the presence of TrPs in elite male WCB players with and without shoulder pain. Therefore, the objective of the current study was to investigate the presence of pressure pain sensitivity and active TrPs in the neck/shoulder muscles in elite male WCB players. We hypothesized that elite male WCB players with shoulder pain would exhibit higher sensitivity to pressure pain than elite WCB players or elite able-bodied basketball players without shoulder pain. In addition, we also hypothesized that the referred pain elicited by TrPs in the neck and shoulder muscles would reproduce shoulder symptoms in elite male WCB players with shoulder pain.
MethodsParticipantsMale WCB players from the Spanish First Division were screened for eligibility criteria. Elite male WCB players were considered according to the classification committee of the international wheelchair basketball federation (IWBF, 2008).15 To be included in the study, WCB players had to satisfy the following criteria: 1, aged between 18 and 50 years; 2, have a valid license from the Spanish Federation of Sports for people with disabilities; and, 3, be actively playing WCB greater than 5h/week. Elite male WCB players with and without unilateral shoulder pain were included. They were included within the shoulder pain group if they exhibited unilateral shoulder pain with a duration at least 3 months and were positive on the Neer and Hawkins tests.16 Individuals were excluded if they presented with a history of shoulder or neck surgery, fracture on the shoulder, bilateral shoulder symptoms, cervical radiculopathy or they had received any therapeutic intervention for the neck-shoulder area in the 6 months prior to the study. All participants received a completed medical examination before participating in the study.
Further, sex- and age-matched able-bodied elite basketball players were recruited as control subjects from volunteers training at a Professional Basketball Club in Madrid (Spain). Individuals were excluded if they exhibited a history of cervical or shoulder pain, history of trauma to the shoulder, diseases or were playing basketball less than 5h per week. The study was approved by a local Ethics Committee Universidad Rey Juan Carlos (URJC), Alcorcón, Madrid, Spain (code 10/2015). All participants signed an informed consent prior to their inclusion in the study.
Pressure pain thresholdsPressure pain thresholds (PPT), defined as the minimal amount of pressure needed for the pressure sensation to first change to pain,17 were assessed with a mechanical pressure algometer. This device consists of a round rubber disc (1cm2) attached to a pressure (force) gauge (kg) with a range score from 0 to 10kg (kg/cm2). Subjects were instructed to press a switch when the sensation changed from pressure to pain. A 30-second rest was allowed between each measure and the mean of 3 trials was calculated for the analysis. This method of evaluating PPT has been shown to exhibit high intra- and inter-examiner reliability.18 In our study, PPT was assessed bilaterally over the C5-C6 zygapophyseal joint, deltoid muscle, and second metacarpal.
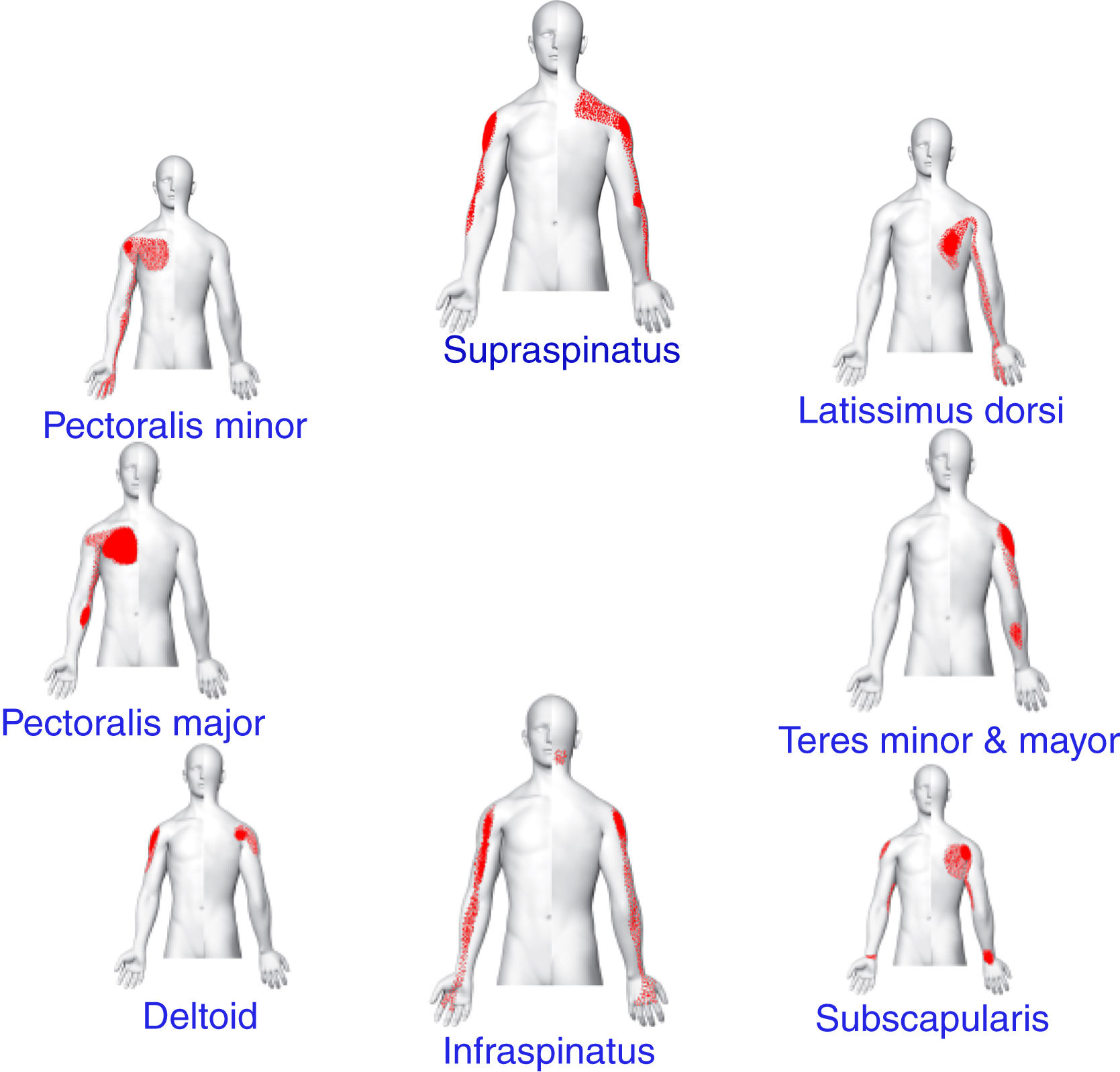
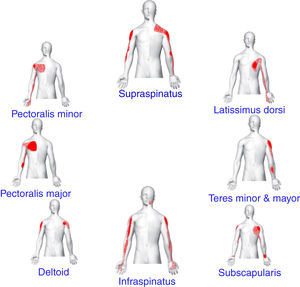
Muscle TrP examinationTrigger points were examined bilaterally within the upper trapezius, supraspinatus, infraspinatus, teres minor, teres major, latissimus dorsi, subscapularis, pectoralis minor, pectoralis major and deltoid muscles by a blinded assessor with 7 years of experience in TrP diagnosis. The diagnosis was performed following the criteria described by Simons et al.11 and confirmed in a Delphi study19 which included: 1, a palpable taut band in a skeletal muscle; 2, the presence of a hypersensitive spot within a taut band; 3, presence of referred pain in response to TrP compression (Fig. 1); and, 4, local twitch response elicited by snapping palpation of the taut band. TrPs were considered to be active when the local and referred pain reproduced the symptoms experienced by the individual. TrPs were considered latent when the local and the referred pain elicited by compression did not reproduce any familiar pain symptom.11 These criteria have shown to have good inter-examiner reliability when applied by an experienced examiner.20
The examination was conducted in a blinded manner. After TrP assessment in all muscles, participants were asked: “when I pressed each of these muscles, did you feel any pain locally, and in other areas (referred pain). Please tell me whether the pain that you feel in the other area reproduced any symptom that you usually experience”. Participants had to indicate whether the pain elicited by manual palpation reproduced their symptom (familiar pain) or another non-familiar pain around the shoulder region.
Self-reported measuresThe clinical history included the reason for the need to use a wheelchair, number of years of wheelchair use, and scoring using the classification committee of the IWBF were completed via self-reported questionnaire. Players scoring 1 to 2.5 were classified as “without trunk control”, whereas players scoring 3 to 4.5 were classified as “with trunk control”. An 11-point Numerical Pain Rating Scale21 (NPRS: 0, no pain; 10, maximum pain) was used to determine the mean intensity of shoulder pain, the worst, and the lowest intensity of shoulder pain experienced in the preceding week.
Additionally, participants completed the wheelchair user's shoulder pain index (WUSPI),22 a 15-item self-report questionnaire assessing the impact of shoulder pain on daily activities in individuals using a wheelchair. Items are assessed by using a visual analogue scale with a higher score representative of more severe pain. The total score ranges from 0 (no pain) to 150 (severe pain in all activities) points. The WUSPI has been shown to be reliable and valid for use in this population.23
Statistical analysisData were analyzed with the SPSS statistical package (21.0 version). Results are expressed as means with standard deviation (SD) or 95% confidence interval (95%CI). The Kolmogorov–Smirnov test revealed that all data exhibited a normal distribution (p>0.05); therefore, parametric tests were used in the analyses.
Differences in the number of TrPs (active or latent TrPs) between groups were assessed with a one-way analysis of variance (ANOVA). Chi-square (X2) was used to investigate the differences in the distribution of TrPs for each muscle between groups. A 2-way analysis of covariance (ANCOVA) was used to evaluate differences in PPTs assessed over each point (C5/6 zygapophyseal joint, deltoid, second metacarpal) with side (affected/unaffected, or dominant/non-dominant) as within-subjects factor, group (WCB players with/without shoulder pain, able-bodied basketball players) as between-subjects factor, and trunk control (yes/no) as covariate. The Bonferroni test was used as post hoc analysis. Spearman rho test (rs) was used to analyze the association between the number of TrPs (total, active, latent), PPTs and shoulder pain intensity. The statistical analysis was conducted at a 95% confidence level, and a p<0.05 was considered statistically significant.
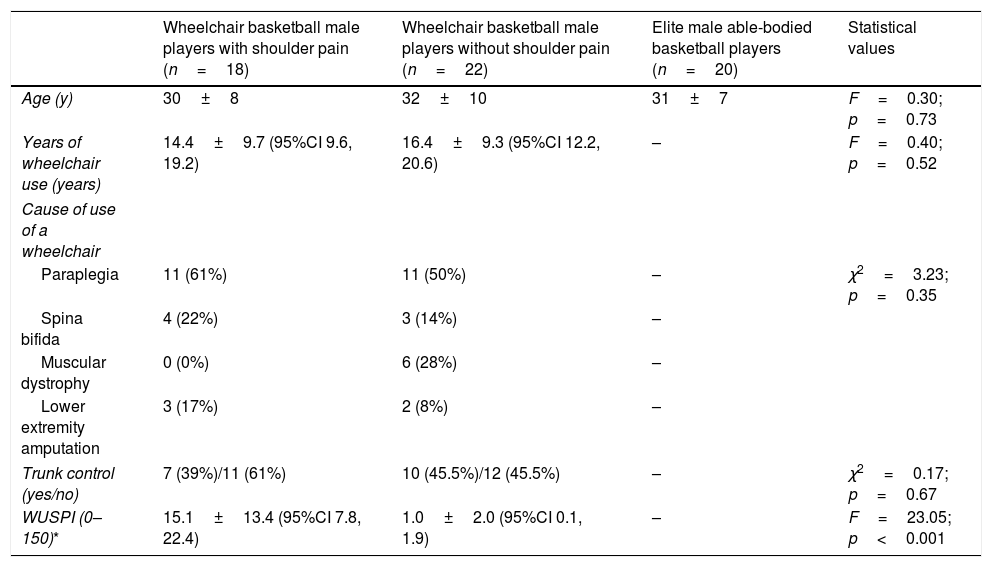
ResultsDemographic and clinical data of the participantsEighteen male WCB players, 18 to 49 years of age (mean: 30±8 years) with unilateral shoulder pain; 22 male WCB players, aged 19 to 51 years (mean: 32±10 years) without shoulder pain and 20 comparable elite male able-bodied basketball players, aged 18 to 50 years (mean: 31±7 years) were included. Demographic data for all participants can be found in Table 1.
Characteristics of the participants.
| Wheelchair basketball male players with shoulder pain (n=18) | Wheelchair basketball male players without shoulder pain (n=22) | Elite male able-bodied basketball players (n=20) | Statistical values | |
|---|---|---|---|---|
| Age (y) | 30±8 | 32±10 | 31±7 | F=0.30; p=0.73 |
| Years of wheelchair use (years) | 14.4±9.7 (95%CI 9.6, 19.2) | 16.4±9.3 (95%CI 12.2, 20.6) | – | F=0.40; p=0.52 |
| Cause of use of a wheelchair | ||||
| Paraplegia | 11 (61%) | 11 (50%) | – | χ2=3.23; p=0.35 |
| Spina bifida | 4 (22%) | 3 (14%) | – | |
| Muscular dystrophy | 0 (0%) | 6 (28%) | – | |
| Lower extremity amputation | 3 (17%) | 2 (8%) | – | |
| Trunk control (yes/no) | 7 (39%)/11 (61%) | 10 (45.5%)/12 (45.5%) | – | χ2=0.17; p=0.67 |
| WUSPI (0–150)* | 15.1±13.4 (95%CI 7.8, 22.4) | 1.0±2.0 (95%CI 0.1, 1.9) | – | F=23.05; p<0.001 |
WUSPI, Wheelchair User's Shoulder Pain Score.
Values are expressed as means±SD (95% confidence interval).
Male WCB players experienced a mean duration of shoulder pain for 2 years (95%CI 1.6, 2.4), whereas the mean, worst and the lowest intensity of shoulder pain was 2.8 (95% CI 1.7, 3.9), 5.6 (95%CI 4.6, 6.7), and 1.2 (95%CI 0.5, 1.9), respectively. No significant association between pain variables and years of wheelchair use was found.
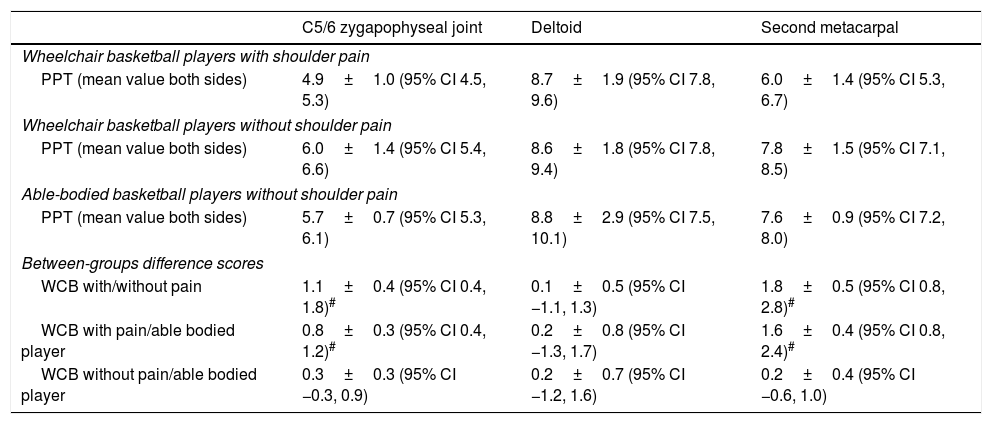
Pressure pain sensitivityThe ANOVA revealed significant differences among groups, but not between sides, for PPTs over the C5-C6 zygapophyseal joint (group: F=9.056, p<0.001; side: F=0.000; p=0.995) and second metacarpal (group: F=18.342, p=0.001; side: F=0.022, p=0.882). Post hoc analysis identified reduced PPTs bilaterally in male WCB players with unilateral shoulder pain as compared with both basketball players groups (either with or without wheelchair) without shoulder pain (Table 2). However, no significant effect for group or side for PPTs over the deltoid (group: F=0.134, p=0.874; side: F=0.409, p=0.524) was observed. No significant group by side interaction was found for C5-C6 zygapophyseal joint (F=0.238; p=0.789), deltoid (F=0.286, p=0.752) and second metacarpal (F=0.180, p=0.835). The inclusion of trunk control as covariate did not influence the results for PPTs (all p>0.05). Table 2 summarizes PPT (mean of both sides) assessed over each point for each study group as well as between-groups difference scores.
Pressure pain thresholds (mean of both sides, kg/cm2) in wheelchair basketball players with/without shoulder pain and healthy basketball players and between-groups difference scores.
| C5/6 zygapophyseal joint | Deltoid | Second metacarpal | |
|---|---|---|---|
| Wheelchair basketball players with shoulder pain | |||
| PPT (mean value both sides) | 4.9±1.0 (95% CI 4.5, 5.3) | 8.7±1.9 (95% CI 7.8, 9.6) | 6.0±1.4 (95% CI 5.3, 6.7) |
| Wheelchair basketball players without shoulder pain | |||
| PPT (mean value both sides) | 6.0±1.4 (95% CI 5.4, 6.6) | 8.6±1.8 (95% CI 7.8, 9.4) | 7.8±1.5 (95% CI 7.1, 8.5) |
| Able-bodied basketball players without shoulder pain | |||
| PPT (mean value both sides) | 5.7±0.7 (95% CI 5.3, 6.1) | 8.8±2.9 (95% CI 7.5, 10.1) | 7.6±0.9 (95% CI 7.2, 8.0) |
| Between-groups difference scores | |||
| WCB with/without pain | 1.1±0.4 (95% CI 0.4, 1.8)# | 0.1±0.5 (95% CI −1.1, 1.3) | 1.8±0.5 (95% CI 0.8, 2.8)# |
| WCB with pain/able bodied player | 0.8±0.3 (95% CI 0.4, 1.2)# | 0.2±0.8 (95% CI −1.3, 1.7) | 1.6±0.4 (95% CI 0.8, 2.4)# |
| WCB without pain/able bodied player | 0.3±0.3 (95% CI −0.3, 0.9) | 0.2±0.7 (95% CI −1.2, 1.6) | 0.2±0.4 (95% CI −0.6, 1.0) |
Values are expressed as means±SD (95% confidence interval).
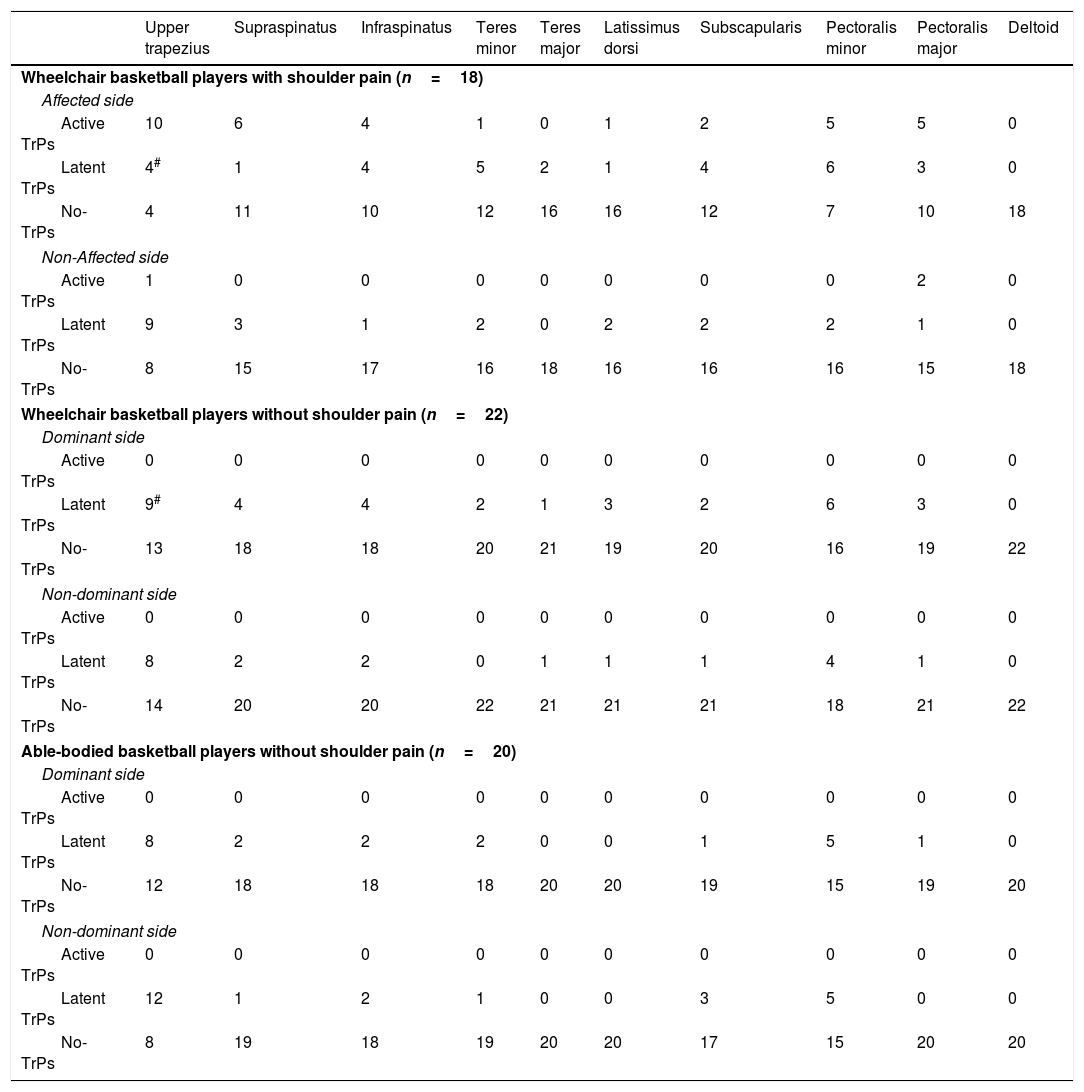
The mean±SD number of TrPs for elite male WCB players with shoulder pain was 4.8±2.7 of which 2±1 were active TrPs and the remaining 2.9±2.2 were latent TrPs. Wheelchair basketball players without shoulder pain and able-bodied basketball players exhibited latent TrPs (mean±SD: 2.4±2.0 and 2.4±1.8, respectively). Wheelchair basketball players with shoulder pain had a higher number of TrPs than basketball players without shoulder pain either with/without wheelchair (F=7.562, p<0.001). The post hoc analysis revealed that WCB players with shoulder pain exhibited a higher number of active TrPs (p<0.001) than the other two groups. However, all groups showed a similar number of latent TrPs (F=0.205, p=0.815). Within elite male WCB players with shoulder pain, no significant correlation between the total number of TrPs, the number of active or latent TrPs and shoulder pain were found.
Distribution of muscle TrPsTable 3 summarizes the distribution of active and latent TrPs by muscle for each group. Active TrPs in the upper trapezius (n=10, 55.5%) and supraspinatus (n=6, 33.3%) muscles were the most prevalent in elite male WCB players with unilateral shoulder pain; whereas latent TrPs in the upper trapezius and pectoralis minor muscles of the dominant shoulder were the most prevalent within male WCB players without shoulder pain (n=9, 40.9%, and n=6, 27.52%, respectively) and in able-bodied male basketball players (n=8, 40% and n=5, 25%, respectively). The distribution of latent muscle TrPs between WCB players with and without shoulder pain was significantly different for the upper trapezius (p=0.03) as male WCB players without shoulder pain showed a higher number of latent TrPs in this muscle. No significant differences in the distribution of latent TrPs between wheelchair basketball players without shoulder pain and able-bodied basketball players were found (all, p>0.05) (Table 3).
Distribution of patients with trigger points on each muscle for all groups.
| Upper trapezius | Supraspinatus | Infraspinatus | Teres minor | Teres major | Latissimus dorsi | Subscapularis | Pectoralis minor | Pectoralis major | Deltoid | |
|---|---|---|---|---|---|---|---|---|---|---|
| Wheelchair basketball players with shoulder pain (n=18) | ||||||||||
| Affected side | ||||||||||
| Active TrPs | 10 | 6 | 4 | 1 | 0 | 1 | 2 | 5 | 5 | 0 |
| Latent TrPs | 4# | 1 | 4 | 5 | 2 | 1 | 4 | 6 | 3 | 0 |
| No-TrPs | 4 | 11 | 10 | 12 | 16 | 16 | 12 | 7 | 10 | 18 |
| Non-Affected side | ||||||||||
| Active TrPs | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 |
| Latent TrPs | 9 | 3 | 1 | 2 | 0 | 2 | 2 | 2 | 1 | 0 |
| No-TrPs | 8 | 15 | 17 | 16 | 18 | 16 | 16 | 16 | 15 | 18 |
| Wheelchair basketball players without shoulder pain (n=22) | ||||||||||
| Dominant side | ||||||||||
| Active TrPs | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Latent TrPs | 9# | 4 | 4 | 2 | 1 | 3 | 2 | 6 | 3 | 0 |
| No-TrPs | 13 | 18 | 18 | 20 | 21 | 19 | 20 | 16 | 19 | 22 |
| Non-dominant side | ||||||||||
| Active TrPs | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Latent TrPs | 8 | 2 | 2 | 0 | 1 | 1 | 1 | 4 | 1 | 0 |
| No-TrPs | 14 | 20 | 20 | 22 | 21 | 21 | 21 | 18 | 21 | 22 |
| Able-bodied basketball players without shoulder pain (n=20) | ||||||||||
| Dominant side | ||||||||||
| Active TrPs | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Latent TrPs | 8 | 2 | 2 | 2 | 0 | 0 | 1 | 5 | 1 | 0 |
| No-TrPs | 12 | 18 | 18 | 18 | 20 | 20 | 19 | 15 | 19 | 20 |
| Non-dominant side | ||||||||||
| Active TrPs | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Latent TrPs | 12 | 1 | 2 | 1 | 0 | 0 | 3 | 5 | 0 | 0 |
| No-TrPs | 8 | 19 | 18 | 19 | 20 | 20 | 17 | 15 | 20 | 20 |
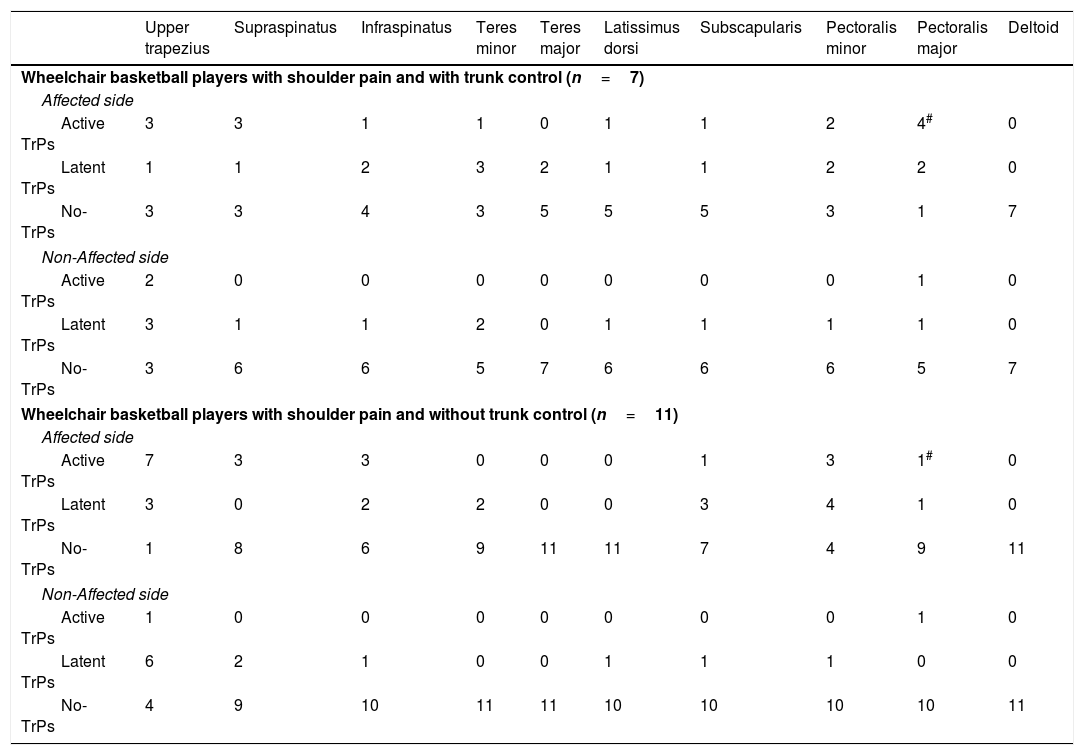
The distribution of TrPs within the elite male WCB players with shoulder pain group according to trunk control was only significantly different for the pectoralis major muscle on the affected shoulder (p=0.018), but not for the remaining muscles. Active TrPs in the pectoralis major muscle (n=4, 57%) on the affected shoulder was the most prevalent in male elite WCB players with shoulder pain and with trunk control (Table 4).
Distribution of patients with trigger points on each muscle in wheelchair basketball players with shoulder pain and with/without trunk control.
| Upper trapezius | Supraspinatus | Infraspinatus | Teres minor | Teres major | Latissimus dorsi | Subscapularis | Pectoralis minor | Pectoralis major | Deltoid | |
|---|---|---|---|---|---|---|---|---|---|---|
| Wheelchair basketball players with shoulder pain and with trunk control (n=7) | ||||||||||
| Affected side | ||||||||||
| Active TrPs | 3 | 3 | 1 | 1 | 0 | 1 | 1 | 2 | 4# | 0 |
| Latent TrPs | 1 | 1 | 2 | 3 | 2 | 1 | 1 | 2 | 2 | 0 |
| No-TrPs | 3 | 3 | 4 | 3 | 5 | 5 | 5 | 3 | 1 | 7 |
| Non-Affected side | ||||||||||
| Active TrPs | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| Latent TrPs | 3 | 1 | 1 | 2 | 0 | 1 | 1 | 1 | 1 | 0 |
| No-TrPs | 3 | 6 | 6 | 5 | 7 | 6 | 6 | 6 | 5 | 7 |
| Wheelchair basketball players with shoulder pain and without trunk control (n=11) | ||||||||||
| Affected side | ||||||||||
| Active TrPs | 7 | 3 | 3 | 0 | 0 | 0 | 1 | 3 | 1# | 0 |
| Latent TrPs | 3 | 0 | 2 | 2 | 0 | 0 | 3 | 4 | 1 | 0 |
| No-TrPs | 1 | 8 | 6 | 9 | 11 | 11 | 7 | 4 | 9 | 11 |
| Non-Affected side | ||||||||||
| Active TrPs | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| Latent TrPs | 6 | 2 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 0 |
| No-TrPs | 4 | 9 | 10 | 11 | 11 | 10 | 10 | 10 | 10 | 11 |
The purpose of the current study was to investigate the presence of pressure pain hypersensitivity and TrPs in the neck and shoulder musculature in elite male WCB players with shoulder pain compared to elite WCB players without shoulder pain and elite able-bodied basketball players without shoulder pain. We found that male elite WCB players suffering from shoulder pain exhibited lower PPTs at C5-C6 zygapophyseal joint and second metacarpal than elite male WCB players without shoulder pain and able-bodied basketball players without shoulder pain. In addition, the referred pain elicited by active TrPs in the neck-shoulder musculature reproduced the pain symptoms within the group of elite WCB players with shoulder pain. No differences in pressure pain sensitivity and the presence of latent TrPs between WCB players without shoulder pain and able-bodied basketball players were observed. These results would suggest a potential role of active TrPs in the development of shoulder pain in elite male WCB players and the presence of sensitivity to pressure pain in the presence of shoulder symptoms in this population.
There continues to be dramatic increase in the number of individuals participating in wheelchair sports.24 Shoulder pain in individuals who are wheelchair athletes is highly prevalent and can be debilitating. The cause of shoulder pain in wheelchair athletes seems to be multifactorial and may include overuse of the shoulder musculature and associated structures with repetitive use for propulsion, use of the arms above shoulder height during the sport, and manoeuvring the wheelchair9 and also poor trunk control.25 We found that active TrPs in the upper trapezius and supraspinatus muscles were the most prevalent in elite male WCB players suffering from shoulder pain. This is an expected finding since these muscles are probably overloaded during basketball but also during wheelchair use and muscle overload has been proposed as a main contributing factor for development of TrPs.11 However, we observed that the presence of TrPs, in this case latent TrPs, was not significantly different between elite WCB players without shoulder pain and able-bodied basketball players, suggesting that the presence of latent TrPs is not related to the use of a wheelchair. It is possible that the presence of active TrPs is more related to the presence of symptoms rather than to wheelchair use. In fact, Hidalgo-Lozano et al. found similar musculature affected by active TrPs in elite swimmers with shoulder pain.14 Therefore, it would be interesting to compare if the presence of active TrPs is different between elite WCB players and able-bodied basketball players with shoulder pain to confirm a potential role of the wheelchair use.
The presence of latent, and not only active TrPs, in this population can also be a relevant factor since latent TrPs can result in altered motor recruitment and efficiency thereby predisposing subjects to potential injury.26 For instance, it is interesting to note that latent TrPs within the upper trapezius and pectoralis minor muscles of the dominant shoulder were the most prevalent in male WCB players without shoulder pain and in able-bodied basketball players compared to WCB players with shoulder pain. These muscles are highly relevant for proper control of the shoulder.27 In fact, Simons et al. suggested that treatment of latent TrPs might potentially reduce the likelihood of developing active TrPs in the future.10 Therefore, clinicians should consider identifying active and latent TrPs when examining sport players. Further research is necessary to identify appropriate preventive and management strategies in wheelchair athletes considering the presence of TrPs in the musculature.
Another potential clinical implication of the current study is that the presence of TrPs could reduce the efficacy of exercise programmes for the management of the shoulder. While there exists a paucity of literature examining the effects of therapeutic strategies for elite WCB, a recent study reported positive effects of a strengthening programme in wheelchair athletes on increasing shoulder range of motion and muscle strength.28 There was no mention of the presence of TrPs in this study. Since active29 or latent26 TrPs in the shoulder muscles are associated with a delay in muscle activation and alterations in their recruitment pattern, it is possible that management of TrPs in the shoulder area preceding the application of exercise programmes could lead to better improvements in function and disability in elite male WCB players.
There exist some limitations to the current study. First, we included elite male WCB players from one geographical location. Therefore, the results of this study should not be generalized to elite female WCB players, wheelchair athletes in general, and also subjects in wheelchairs who do not participate in athletics or are from other countries. Additionally, our sample size was relatively small. Future studies are needed with larger sample sizes to confirm our results. Finally, we cannot infer a cause and effect relationship between the decreased hypersensitive and TrPs with the presence of shoulder pain.
ConclusionThis study identified localized hypersensitivity and a significant number of active TrPs in elite male WCB players with shoulder pain compared to asymptomatic elite male WCB players and elite male able-bodied basketball players. The referred pain elicited by mechanical stimulation of active TrPs reproduced the reported symptoms in WCB players with shoulder pain. No differences between WCB players without shoulder pain and able-bodied basketball players were observed. It is possible that proper management of active TrPs could result in reduction of pain and disability in WCB players with shoulder pain.
Conflicts of interestThe authors declare no conflicts of interest.