Shoulder pain related to pathology of the long head of the biceps tendon (LHBT) can be debilitating. Chronic LHBT tendinopathy is a common condition that is difficult to treat. Little consensus exists regarding the optimal approach to treating individuals with LHBT tendinopathy.
ObjectiveTo systematically scope the literature to identify and present the available information regarding physical therapist interventions used for the management of individuals with LHBT tendinopathy including types of interventions used or recommended.
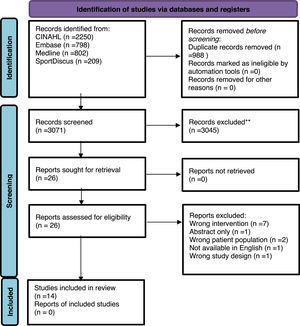
MethodsA scoping review of physical therapist interventions used to treat LHBT was conducted of the CINAHL, Embase, Medline, and SportDiscus databases. Full text records reporting physical therapist-based interventions in individuals with proximal LHBT pathology were included. Articles not written in English were excluded.
ResultsOf the 4059 records identified, 14 articles met the inclusion criteria. Interventions used to treat LHBT tendinopathy identified in quantitative studies included: extracorporeal shock wave therapy, polarized light, ultrasound, low-level laser, iontophoresis, general exercise, eccentric training, stretching, dry needling, and joint mobilization. Interventions described in literature reviews, clinical commentaries, and a Delphi study included: therapeutic modalities, manual therapy, exercise, dry needling, and patient education.
ConclusionThis scoping review reported interventions primarily based on therapeutic modalities in quantitative studies while literature reviews, clinical commentaries, and a Delphi study described the addition of manual therapy, patient education, exercise, and dry needling. Overall, there is a dearth of evidence detailing the conservative management of LHBT tendinopathy.
Shoulder pain is a common orthopedic condition often associated with incomplete resolution of symptoms and continued pain.1 Shoulder pain resulting from pathogenesis of the rotator cuff tendons and other subacromial tissues is referred to as subacromial shoulder pain2,3 and may be caused by overuse,4 capsular tightness,5 rotator cuff and scapular dysfunction,6 and poor posture.7 Proximal long head of the biceps tendon (LHBT) tendinopathy often presents as a secondary shoulder pathology with other primary shoulder pathologies including subacromial shoulder pain,8,9 and injury to the LHBT is recognized as a significant independent source of pain when left untreated.10 Discrete diagnosis of the pain generators in the shoulder joint can be difficult as it encompasses a variety of conditions and symptoms. Further, diagnosis of LHBT tendinopathy is described as being difficult8,11,12 and often involves a combination of clinical tests including palpation of the LHBT tendon for pain. Clinical tests (i.e. Speed's, Yergason's) used for diagnosing LHBT lesions have been shown to have high sensitivity, poor to moderate specificity, and low likelihood ratios,13–15 which makes diagnosis without the use of imaging challenging.16 Yet, recent evidence suggests that pain is the key clinical feature and imaging may not be helpful in diagnosing tendinopathy.17,18 Despite these identified challenges with diagnosis, provocation of pain through palpation of the LHBT may still be considered one the most useful clinical tests.8,9,13,16
Physical therapist management of individuals with suspected LHBT tendinopathy may involve a multimodal approach to remediate impairments of the shoulder, scapular region, and cervicothoracic spine through exercise, joint and soft tissue mobilization, as well as retraining dysfunctional movement.8 Contemporary research on tendinopathy describes the need for mechanical loading of the tendon, including eccentric exercise (EE) and heavy slow-load exercises, as an effective component of an exercise program with the overall intent of promoting tendon healing.19–22 However, exercise delivery including intervention details and dosing specific to LHBT management are not widely reported in the literature.
In addition to exercise as a component of a multimodal approach, management may include the use of therapeutic modalities or biophysical agents. Based on a recent review of systematic reviews specific to tendinopathies, only moderate-quality evidence supports low-level laser for pain and disability in the short-term yet the use of shockwave therapies showed a statistically significant improvement in pain and function at all follow-up periods.21 Further evidence exists stating therapeutic modalities are supported by weak evidence23 with moderate evidence of no effect for interventions including low-level laser therapy, extracorporeal shockwave therapy (ESW), pulsed electromagnetic energy, and ultrasound (US).3 Therefore, it is difficult to interpret best practices utilizing therapeutic modalities for treating tendinopathy specific to the shoulder region.
Younger, active patients who do not respond to conservative management or physical therapy, often pursue surgical options including biceps tenodesis.24 Surgery may be an unnecessary option, creating an additional burden on the healthcare system especially if evidence to support physical therapy intervention exists. There is a lack of well-defined or adopted physical therapy guidelines used to treat individuals with proximal LHBT tendinopathy yet there is a need to determine if evidence of interventions exist. Therefore, the purpose of this scoping review was to identify and present physical therapist interventions reported in the literature used to treat individuals with proximal LHBT tendinopathy. A scoping review allows for the researcher to thoroughly canvas the literature and analyze knowledge gaps. Thus, this is a first step to identifying information that will support future research in this area.
MethodsProtocol and registrationA scoping review of the literature was performed to fully explore the research question.25 The research team modified the review design from a systematic review to a scoping review after initial searches revealed a limited number of randomized controlled trials (RCTs) available. A systematic review was not possible yet it was deemed that initial intervention based information needed to be gathered. The review protocol was prospectively registered with PROSPERO (CRD42020193354) prior to changing the design. This scoping review was conducted following the Preferred Reporting Items for Systematic reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) checklist.26
Eligibility criteriaQuantitative studies that met the following criteria were included: 1) patients of any age diagnosed with LHBT tendinopathy and/or LHBT tendon pain, 2) treatment included a description of physical therapist-based interventions, and 3) were available in full text. Participants of any age and sex in randomized and nonrandomized trials, cohort trials, and case series were included if they had a proposed diagnosis of LHBT tendinopathy based on clinical examination findings and/or positive imaging and were treated with a physical therapist intervention in either the experimental or control groups. Physical therapist interventions were defined as exercise, manual therapy, patient education, and therapeutic modalities (heat, cold, electricity, sound waves, radiation, and other interventions). Physical therapist interventions combined with corticosteroid injection were included as an intervention as injections are strongly related to physical therapy rehabilitation, despite not being within the scope of practice of physical therapists.3 Studies with the following characteristics were not included: 1) diagnosis of biceps tear or labral tear or 2) treatment, surgery, or post-surgery follow-up that was only medical in nature. Other records reporting on the management of LHBT including literature reviews, clinical commentaries, and a Delphi study, were included if physical therapy intervention was described in the context of LHBT tendinopathy. We excluded publications that were not available in the English language.27
Information sources and searchThe electronic databases CINAHL, Embase, Medline, and SportDiscus were searched from inception to September 12, 2021, and updated on November 30, 2022. The search was developed and performed with assistance from a research librarian. The terms “bicep” and “tendinopathy/tenosynovitis” or “tendinitis” or “tendonitis” or “tendon injuries” or “inflammation and tendons” or “tendon inflammation or pathology” or “tendinosis” and “physical therapy specialty” or “physical therapy modalities” or “intervention” or “rehabilitation” were used to search the electronic databases. Depending on the database used, MeSH terms or subheadings related to these terms were included. Results were limited to publications describing humans. To retrieve all records, including any form of physical therapy rehabilitation, the search terminology was applied (an example of the search strategy is available in Supplementary material). In addition, bibliographic reference lists from identified publications were hand-searched for any other publication not identified during the database searches.
Study selectionAfter records were retrieved from the databases, duplicates were removed. Two authors (A.M, J.Y) independently screened records to identify those meeting the inclusion criteria, initially by title and abstract, followed by full-text review. If consensus could not be reached, disagreements between reviewers were resolved by a third author (J.C). Covidence systematic review software (Veritas Health Innovation Ltd, Melbourne, Australia) was used to manage search results and the included publications throughout the review.28
Data extraction and analysisThe data were extracted in Covidence with a standardized form based on the Cochrane Handbook for Systematic Reviews of Interventions (Version 5.1.0).29 Two authors (A.M, P.H) independently extracted data, and inconsistencies between the reviewers were resolved by a third reviewer (J.Y). The extracted data included the quantitative research study design or other type of record or report (literature review, clinical commentary, Delphi study), participant and treatment characteristics (if applicable), and intervention descriptions. The following data were extracted from the quantitative studies: author, study design, sample size, age, sex, criteria for diagnosis (if included), and a description of interventions and intervention groups. Specific descriptions of physical therapy interventions including parameters, timing, and dosing were also extracted for each quantitative study. A synthesis of the available evidence clinical commentaries, literature reviews, and a Delphi study were undertaken and narrative summaries of the information were constructed. Physical therapist intervention details (eg, specific interventions, progression criteria, and interventions recommended according to the phase of healing) were extracted and categorized into themes and summarized into tables.
ResultsThe electronic database searches resulted in 4059 records. After duplicates were removed, 3071 unique records underwent title/abstract screening and 3045 records were excluded for not meeting inclusion criteria. Twenty-six full-text articles were assessed for eligibility. Ultimately, 12 were excluded for various reasons (e.g., wrong intervention, abstract only; see Figure 1, PRISMA flow diagram) leaving 14 records8,11,12,30–39 to be included in this scoping review.
Study characteristicsThe 14 records included five RCTs,30,31,33–35 one observational cohort study,36 one case series,32 four literature reviews,11,12,37,38 two clinical commentaries,8,39 and a Delphi study.40 The publication years ranged from January 2004 to June 2022. Specific physical therapy interventions were provided to participants in all quantitative studies, and physical therapy interventions were described in the remaining literature reviews, clinical commentaries, and Delphi study. Diagnoses of study participants (n = 513) included biceps tendonitis,30 tendinopathy of biceps brachii muscles,31 tendinopathy of the long head of the biceps tendon,32,33 bicipital tenosynovitis,35 and proximal biceps tendon pathology.34 Study participants included males and females ranging in age from 19 to 69 years old from seven countries. Literature reviews, clinical commentaries, and a Delphi study had varying descriptions of interventions for managing individuals with LHBT tendinopathy. Table 1 summarizes the characteristics of included records including, the type of study or report, diagnoses criteria of included participants, and descriptions for all interventions. Table 2 summarizes the frequency of the identified themes of the physical therapy interventions among the quantitative studies and other included literature.
Description of physical therapy interventions for long head of the biceps tendinopathy.
| Publication Type n | Participant characteristics and criteria for diagnosis | Description of physical therapy intervention |
|---|---|---|
| Alizadeh et al30Randomized Controlled Trialn=206 | Male=121, female=83; mean age not reportedShoulder pain (> 3 months); local tenderness in bicipital groove; at least one biceps positive test (Yergason's test or Speed's test); positive LHBT tendinopathy signs with indirect magnetic resonance arthrography (IMRA); lack of any evidence of complete or incomplete rupture of rotator cuff. | US: 10 sessions of US (3 times per week) with frequency of 1 MHz and intensity of 1 W/cm2 with the pulse mode duty cycle of 2:8 and a probe surface of 5 cm2 were applied for 5 min in each session. L/US: Type and frequency of US were same as US group. In addition, LLLT was performed using gallium-arsenide-aluminum infrared laser 9 with a pencil probe. ISCI: In the supine position, the arm of the injection site was bent at 90° at the elbow and it was put on the body; with the help of the linear probe at a range of 2–20 MHz and based on the depth of anatomical structure, LHBT was found in bicipital groove. One mL of 40 mg/mL methylprednisolone acetate solution and 1 mL of 2% lidocaine solution were mixed and intra tendon sheath injection under US guidance by 1.5-inch length gauge 25-needle was done.ESCl: All steps and equipment were those used for ISCI however, extra tendon sheath injection of the solution was applied. |
| Barbosa et al31Randomized Controlled Trialn=14 | Male=5, female=9; mean age 46.14 +/- 7.62Shoulder pain (> 6 months); did not have a diagnosis of a frozen shoulder; pain with palpation of the biceps brachii muscle tendons; positive in one or more special tests for biceps brachii muscle tendon (Speed's test and Yergason's test) | US: utilized frequency of 3 MHz with dosage of 1.0 W/cm2 and pulsed of 1:1. US was applied for 4 min to the long head of the biceps brachii muscle.EMT: consisted of 3 sets of 20 reps each session. Patient performed either “empty can” movement when treating supraspinatus or “right curl” movement when treating biceps brachii dysfunctions. Movement resistance was offered manually, always by the same researcher and respecting the patient's pain limit.JM: accessory movements of the shoulder were performed: front, back, lower longitudinal, and lateral relaxations of the glenohumeral joint, anteroposterior movements of the acromioclavicular (squeeze) joint and anteroposterior, inferior to superior, and superior to inferior movements of the sternoclavicular joint. The following series was applied twice every session: one minute of mobilization for each movement (two to three cycles per second), and one minute of active free abduction movement in the scapular plane, over the arc of movement without pain.* Both groups received treatment for 10 sessions (3 per week). Experimental group added JM in conjunction with US and EMT; control group only received US and EMT. |
| Liu et al35Randomized Controlled Trialn=79 | Male=54, female=25; age 27–79Bicipital groove pointtenderness; pain confirmed through Yergason's testand Speed's test | rESWT: 1500 pressure pulses were irradiated at a repetition frequency of 8 Hz at the nominal peak pressure set on the rESWT device to 3 bar.Sham: treatment head was deflated to avoid forming pressure pulse in the pathological site, and no coupling gel was applied. The machine makes a noise ‘‘bang bang’’ when each pressure pulse is delivered to enhance the sham design.* All treatments were dosed once per week for 4 weeks. |
| McDevitt et al32Case Seriesn=10 | Male=8, female=2; age 24–64Anterior shoulder symptoms (> 3 months); pain with palpation of the LHBT; positive results on a combination of tests including active shoulder flexion, Speed's test, HawkinsKennedy test, Neer test, and Yergason's test | DN: standard, disposable stainless-steel needles inserted into the skin over the most painful and/or thickened areas of the tendon. The technique utilized was a fast-in and fast-out (pistoning) technique for 20–30 repetitions per area in up to three areas.EE: emphasized the eccentric component of the movement and was performed after the DN intervention in two positions. In both positions, they would eccentrically lower the arm for a count of 3–4 s. Then, the concentric component of the exercise was performed for a count of only 1 s. 3 sets of 15 were performed of each exercise.Stretching: Stretching of the biceps muscle/tendon was performed following the EE for 2 × 30 s. |
| Taskaynatan et al34Randomized Controlled Trialn=47 | Male=19, female=28; mean age 56 +/- 9.96Shoulder pain >4 weeks; soft tissue ultrasound examination that revealed biceps tendon pathology | SI: SI [0.5% hydrocortisone acetate with the negative electrode placed anterior side of the shoulder, 3–4 mA galvanic current, 15 min] was appliedET: ET [interferential current, 0–100 Hz, 15 min] was applied in the second group for 15 sessions.* Both groups received hot pack [15 min], US [1.5 W/cm2,continuous mode, 5 min], and a standard exercise program including pendulum, strengthening, and ROM exercises in painfree range. |
| Zivanovic et al36Observational Cohort Studyn=65 | Male=25, female=40; age 19–69Tenderness of the biceps brachi tendon; positive Yergason's test | Control group: provided with anti-rheumatic: diclofenac natrijum 2 × 100 mg or nimesulid 2 × 50 mg depending on the gastrointestinal tolerance and diazepam 2 × 5 mg as a miorelaxant and anxiolytic. Experimental group: provided with corticosteroid injection (combination of the betametasone, Na-phosphate and betametasone dipropionate) periarticular and anti-rheumatic, and for the following 10 days the disease localization was treated with polarized light. |
| Xiao et al33Randomized Controlled Trialn=93 | Male=54, female=39; age 34–68Diagnosed with LHBT based on relevant examinations; unilateral lesion; the tendon sheath of the LHBT was not completely torn | Control group: received extracorporeal shock wave treatment with standard therapeutic head (15 mm). This was performed in concert with MSUS. Treatment was performed once every week, with continuous treatment of 5 applications as a course of treatment.Observation group (CI, PL): received injections consisting of 2 ml of water for injection + 0.5 ml of compound betamethasone injection (CBI) + 0.5 ml of 2% lignocaine injection. During treatment, upper limb of the affected shoulder joint was kept with palm facing upwards and close to the body side, the forearm was kept bent at 90° after rotation, and the site to be operated was positioned. Once the injured site was identified, the probe was rotated at a right angle, and kept parallel to the long axis of the biceps brachii. Drugs were injected using long axis needle insertion technique. Full treatment was course of 1 treatment. |
| Chen and Voloshin37Literature Review | N/A | Conservative management includes activity modification, nonsteroidal anti-inflammatory drugs, ice, gradual strengthening exercises and corticosteroid injections (into the biceps tendon sheath and/or subacromial). |
| Ejnisman et al12Literature Review | N/A | Conservative treatment is indicated for primary tendinopathy and in older and/or inactive patients with secondary pathology. Conservative treatment includes rest, medication, physical therapy, strengthening of periscapular muscles. |
| Harwood and Smith38Literature Review | N/A | Conservative management is more favorable for middle aged to older patients due to minimal strength loss and a 30% failure rate with surgical intervention. Treatment options include restoration of strength and function, physical therapy, rotator cuff strengthening and surrounding structures to minimize stress on the biceps tendon. |
| Krupp et al.8Clinical Commentary | N/A | The initial approach to both primary and secondary bicipital tendinopathy is nonoperative, beginning with rest and withdrawal from aggravating activities. Additional treatment includes ice, a course of anti-inflammatory medication, and formal physical rehabilitation. Establishing a causal relationship between physical impairments and biceps pathology is important as the treatment plan needs to address impairments. The individual should be advanced through a four-phase rehabilitation protocol while monitoring response to treatment, including pain, swelling, and motion. A four-phase approach to rehabilitation is recommended.Phase 1: Acute Phase-Pain management, restoration of PROM and restoration of accessory motion; treatment includes clinical modalities, ROM, joint mobilization, stretching, and early scapular strengthening including lower trapezius facilitation.Phase 2: Subacute Phase, Early Strengthening-AROM and early strengthening; treatment includes: active shoulder ROM, rotator cuff strengthening (sport cord), scapular strengthening (sport cord), and clinical modalities as necessary.Phase 3: Advanced Strengthening-consists of rotator cuff and periscapular strengthening as well as a focus on improving dynamic stability; treatment includes: PNF, push up progressions, plyometric exercise, resisted training (sport cord), and weight training.Phase 4: Return to Activities-consists of return to sport exercises focused on improving power and speed; treatments include return to sport and re-evaluation, plyometric training, rhythmic stabilization, and PNF plyometrics. |
| Lewis et al11Literature Review | N/A | Conservative therapy includes rest, NSAIDs, ice, activity modification, corticosteroid injection, and physical therapy.Mechanical stimulation using dry needles have been shown to increase blood flow to the area in animal studies. Once the acute phase has passed physical therapy may include stretching of anterior shoulder and pectoralis minor, mechanical stimulation with dry needling, ROM, core and scapular strengthening, stretching of the low back and hamstring, rotator cuff strengthening of progressive difficulty. If the individual is a thrower, they would begin a more rigorous throwing regimen once the rotator cuff is strengthened sufficiently. |
| McDevitt et al40Delphi Study | Consensus based on Delphi survey (over 3 rounds) from 31 identified experts in the management of shoulder pain. | Consensus (based on agreement) for interventions was established across six themes after three rounds of surveys.
|
| Paynter39Clinical Commentary | N/A | Most cases of biceps tendinitis are secondary to a primary impingement syndrome. Conservative treatment is warranted for primary or secondary bicipital tendonitis including rest, ice, NSAIDs, steroid injections and physical therapy. In the acute stage, aggressive physical therapy should be avoided. Initially, physical therapy should include gentle ROM, pulley, wand, wall walking, and towel aided stretches followed by PROM, AROM, stretching of posterior capsule, strengthening of rotator cuff and scapular stabilizers with isometrics progressing to isotonic exercises or stretch band exercises. It is important to avoid positions of impingement including overhead exercises and shoulder abduction. |
Abbreviations: US, ultrasound; L/US, low level laser treatment and ultrasound; MHz, megahertz; W/cm, watts/centimeter; LLLT, low level laser therapy; ISCl, intrasheath ultrasound guided corticosteroid injection; LHBT, long head of the biceps tendon; ESCl, extrasheath ultrasound guided corticosteroid injection; EMT, eccentric muscle training with manual resistance; JM, joint mobilization; rESWT, radial extracorporeal shock wave therapy; DN, dry needling; EE, eccentric exercise; SI, steroid iontophoresis; ET, electrotherapy; MSUS, musculoskeletal ultrasonography; CI, corticosteroid injection; PL, polarized light; ROM, range of motion; PROM, passive range of motion; AROM, active range of motion; PNF, proprioceptive neuromuscular facilitation; NSAIDS, non-steroidal anti-inflammatory drugs.
Symbols: +/- = standard deviation.
Key themes for physical therapy interventions (n = 14).
| Theme | Physical therapy intervention described | Quantitative studya(LR, CC, DS)a |
|---|---|---|
| Therapeutic Modalities | Acute modalities | 0 (1) |
| Ultrasound with a frequency of 1 MHz or 3 MHz and intensity of 1.0 W/cm2 −1.5 W/cm2 to the LHBT tendon and/or biceps brachii muscle | 3 (0) | |
| ESWT to the most seriously affected tendon and sheath areas (visualized by ultrasound) | 2 (0) | |
| Electrotherapy (interferential current) to anterior shoulder region | 1 (0) | |
| Polarized light | 1 (0) | |
| Low level laser therapy | 1 (0) | |
| Heat to anterior shoulder region | 1 (0) | |
| Ice | 0 (4) | |
| Manual Therapy | Joint mobilization or non-thrust manipulation (glenohumeral, acromioclavicular, and sternoclavicular joints) | 1 (3) |
| Joint mobilization or non-thrust manipulation (cervical and thoracic spine) | 0 (1) | |
| Thrust manipulation (thoracic spine and cervicothoracic junction) | 0 (1) | |
| Soft tissue techniques (biceps brachii, rotator cuff, periscapular, scapular muscles, and the cervical region) | 0 (1) | |
| Dry Needling | Dry needling to painful or thickened areas of the tendon based on palpation or the biceps brachii muscle | 1 (2) |
| Exercise | Eccentric muscle training using manual or mechanical resistance (biceps brachii muscle) | 2 (3) |
| Stretching (biceps brachii muscle/tendon) | 1 (3) | |
| Stretching (pectoralis major, pectoralis minor, upper trapezius, latissimus dorsi, posterior rotator cuff, and glenohumeral medial rotator muscles) | 0 (3) | |
| Strengthening exercises (shoulder and/or scapular region) | 1 (6) | |
| Progressive resistance exercises (latissimus dorsi, deltoid, biceps brachii, middle and lower trapezius, serratus anterior, rhomboid major and minor, rotator cuff medial and lateral rotator muscles) | 0 (3) | |
| Open/closed kinetic chain exercises (rotator cuff muscles, scapular stabilizers, biceps brachii muscles) | 0 (1) | |
| Task specific functional activities (reaching, lifting, overhead activity, occupation specific, sport specific) | 0 (3) | |
| Range of motion exercises in pain-free range | 1 (3) | |
| Education | General advice on activity modification | 0 (6) |
| Patient education (occupation modification, training/loading modification, medication, physical therapy treatment plan, pain neuroscience education, LHBT pathoanatomy, postural control) | 0 (1) | |
| Cognitive behavioral therapy | 0 (1) | |
| Physical Therapy | General recommendation for “physical therapy” as an approach to treatment | 0 (5) |
Therapeutic modalities are defined as thermal, mechanical, electromagnetic, and light energies administered for therapeutic purposes.41 Two quantitative studies30,31 evaluated the use of US on proximal biceps tendinopathy. Alizadeh et al.30 compared four groups: US, US plus low-level laser, and intrasheath or extrasheath US-guided corticosteroid injection. The US group received five minutes of US for 10 sessions over three weeks. Barbosa et al.31 compared US and EE to the combined interventions of US, EE, and joint mobilization for 10 sessions, with four minutes of US applied to the LHBT.31 One study (Taskaynatan et al.34) had both the experimental and control group receive US for five minutes over 15 sessions.
Two RCTs assessed the effects of ESW on tenosynovitis of the LHBT.33,35 Liu et al.35 assessed the effects of ESW versus sham and Xiao et al.33 assessed ESW versus corticosteroid injection. One study (Taskaynatan et al.34) described the use of electrotherapy; one group received hydrocortisone acetate through iontophoresis (3–4 milliamp, galvanic current, 15 min), and the other received electrotherapy (interferential current, 0–100 hertz, 15 min).34 Both groups received hot packs, US, and a standard exercise program over 15 sessions. Zivanovic et al.36 compared polarized light therapy (for 10 days) combined with a corticosteroid injection to a control group who were prescribed oral anti-inflammatories.
Manual therapyManual therapy is defined as skilled passive movements of joints and soft tissues intended to improve tissue extensibility and range of motion, induce relaxation, mobilize or manipulate soft tissues and joints, modulate pain, and reduce soft tissue swelling, inflammation, or restriction.42 Techniques may include manual lymphatic drainage, manual traction, massage, joint mobilization/manipulation, and passive range of motion.42 One quantitative study (Barbosa et al.31) described joint mobilization combined with US and EE muscle training over 10 sessions. Joint mobilization included several accessory movements to the shoulder, acromioclavicular joint, and sternoclavicular joint followed by one minute of passive shoulder abduction in the scapular plane.31 The Delphi study described grades of techniques recommended and regions treated (glenohumeral, cervical and thoracic spine, and shoulder) with thrust and non-thrust manipulation and soft tissue techniques.40 A literature review (Paynter et al.39) described stretching of the posterior capsule of the shoulder and range of motion while a clinical commentary (Krupp et al.8) recommended the restoration of accessory motion and joint mobilization.
Dry needlingThe case series by McDevitt et al.32 described utilization of dry needling to the LHBT for up to six visits followed by EE (heavy slow load exercises) and stretching of the biceps muscle. The dry needling technique involved pistoning of the needle in and out of the most painful areas of the tendon (based on palpation) for 20–30 repetitions in up to three areas. The Delphi study40 reported consensus (based on expert input) on dry needling of the biceps brachii muscle while Lewis et al. recommended mechanical stimulation with dry needling to increase blood flow and growth factors.11
ExerciseThree quantitative studies,31,32,34 four literature reviews,11,12,37,38 two clinical commentaries,8,39 and a Delphi study40 described exercise as a component of physical therapy management of individuals with LHBT tendinopathy. Stretching of the biceps brachii muscle8,11,32,40 and other associated muscle groups11,39,40 was also frequently described. Strengthening exercises were described in two quantitative studies,32,34 four literature reviews,11,12,37,38 two clinical commentaries,8,39 and a Delphi study.40 Additional exercise descriptions included progressive resistance exercise,8,11,40 open and closed chain exercise,40 task specific or functional activities,8,11,32 and EE.8,31,32,40
An RCT (Barbosa et al.31) and a case series (McDevitt et al.32) included EE as an intervention to treat LHBT. The RCT (Barbosa et al.31) included EE muscle training in the experimental (US+EE+joint mobilization) and control (US+EE) groups.31 The EE muscle training exercise had participants perform a “bicep curl” movement (patient flexes their elbow) with manual resistance43 provided by the researcher for three sets of 20 repetitions per treatment session for 10 sessions over three weeks.31 The case series described combining dry needling with EE and stretching of the biceps muscle.32 Heavy slow load exercises, including EE, targeting the LHBT were dosed, as described by Alfredson,32,44 at three sets of 15 repetitions with 4–6 pounds (or until perceived patient discomfort) in two positions. The Delphi study40 described the use of isometrics, concentrics, and eccentric biceps brachii contractions with resistance.
EducationOne clinical commentary,39 and four literature reviews11,12,37,38 included the general recommendation to provide advice on activity modification and/or rest while the Delphi study40 and the clinical commentary by Krupp et al.8 included specific descriptions for patient education including return to sport and occupational advice.
DiscussionThe LHBT may be implicated as a pain generator in the anterior shoulder causing pain and disability in individuals with a primary complaint of shoulder pain,8–10 yet the overall incidence of bicipital tendinopathy remains unclear9 as it is considered a secondary pathology commonly associated with other pathologies of the shoulder. As a result, little consensus exists on the ideal management of LHBT.45,46 The primary purpose of this scoping review was to present and describe the content of physical therapy interventions used for the management of individuals with LHBT tendinopathy. We identified seven quantitative studies, two clinical commentaries and four literature reviews, describing interventions for individuals with LHBT tendinopathy.8,11-12,31–40 The following sections aim to better explain these findings and highlight the current gap and future directions for research.
Quantitative studiesNearly all of the quantitative studies included in this review investigated and described the use of therapeutic modalities as an intervention used to treat patients with LHBT.30,31,33–36
LHBT often begins as an inflammatory condition or tenosynovitis which may develop into a degenerative tendinopathy including the presence of tendon thickening, disorganization, adhesions, and scarring.8,9,45 Therefore, therapeutic modalities have historically been utilized by physical therapists to treat musculoskeletal conditions (including tendon pathology).47,48 It is unsurprising that therapeutic modalities would be studied quantitatively and utilized clinically to treat pain associated with LHBT. However, contemporary opinion persists that many available therapeutic modalities (specifically US, electrotherapy, ESW, low-level laser) are only supported by weak evidence,23 and for some therapeutic modality-based interventions, there is moderate evidence of no effect.3
A recent review of systematic reviews on interventions specific to various tendinopathies, reported moderate-quality evidence to support the use of low-level laser therapy for pain and disability in the short term. ESW therapies resulted in a statistically significant improvement in pain and disability at all follow-up periods.21 In contrast, a systematic review on the efficacy for US in individuals with rotator cuff tendinopathy found that US was not superior to placebo.49
In this review, only three of seven quantitative studies focused on studying and describing a multimodal approach, which is recommended by clinical practice guidelines focusing on the management of shoulder pain.50,51 The RCT by Barbosa et al.31 added joint mobilization to EE and US. Evidence exists for exercise therapy, as a component of a multimodal approach, specifically EE in treating individuals with tendinopathy.19–21 Similarly, the case series by McDevitt et al.32 utilized and described a multimodal approach of DN, EE, and stretching. Taskaynatan et al.34 included the combined therapy of iontophoresis with a standard exercise program. In summary, seven quantitative studies specific to physical therapy interventions describe the treatment of LHBT to include US, ESWT, electrotherapy, strengthening, joint mobilization, EE, dry needling, and polarized light therapy.
Literature reviews, clinical commentaries, Delphi studyLiterature reviews, clinical commentaries, and a Delphi study recommended “physical therapy” which included therapeutic modalities, various forms of exercise (stretching and strengthening), manual therapy (soft tissue mobilization, thrust and non-thrust manipulation), dry needling, and patient education (advice on activity modification). Further, the inclusion of a multimodal approach (including exercise) was described by the literature reviews, clinical commentaries, and Delphi study.8,11,12,37–40 According to Krupp et al.,8 physical therapy management of LHBT tendinopathy should involve a multimodal approach addressing impairments of the shoulder, scapular region and cervicothoracic spine with the application of exercise, joint and soft tissue mobilization as well as retraining dysfunctional movement patterns.8 Further, in addition to addressing associated impairments, Krupp et al.8 described a four-phase exercise program (pain management, restoration of range of motion, active range of motion, early strengthening, rotator cuff and periscapular strengthening, and return to sport) for the management of individuals with LHBT tendinopathy. Two additional commentaries and the Delphi study described a multimodal approach including education on activity modification (to avoid positions of impingement), stretching (muscles and capsular tissue), joint mobilization, dry needling, and various forms of strengthening including: isometrics, isotonics, core, rotator cuff and scapular strengthening.11,39-40
Knowledge gaps and future researchDescriptions of interventions based on the 14 articles included in this scoping review are considered preliminary, and RCTs should be conducted before strong recommendations can be made. The quantitative studies in this review consist of RCTS with small sample sizes, and a small sample of patients in the form of a case series which limits translation to practice. Intervention information reported in the case series suggests that a combination of interventions, directed toward tendon pain, may be a complement treatment to traditional manual therapy and exercise typically utilized as a “first line” intervention to treat shoulder pain. However, further study of this hypothesis on a larger scale is necessary before recommendations can be made. Future quantitative investigations should report on interventions in sufficient detail to assure reproducibility including information on dosing and time-based interventions. Further, there is a need for consistent use of reporting guidelines for interventions such as the Template for Intervention Description and Replication (TIDierR) and the Consensus on Exercise Reporting Template (CERT) to improve reporting on exercise based interventions52,53 and manual therapy based interventions54 in individuals with musculoskeletal pain. Additional literature in this review consists of literature reviews, clinical commentaries and a Delphi study all describing and recommending interventions, however, further investigation in controlled trials using large samples of patients with LHBT tendinopathy are warranted to determine effectiveness of the recommended interventions. Future studies need to be intervention-based to explore the efficacy of interventions described throughout this review.
LimitationsDespite a systematic search strategy, it is possible that not all relevant studies were identified, and it is possible that other sources of information (blogs, conference proceedings), which were excluded, may have contributed additional information to this topic. A considerable limitation was that the quantitative studies included in this review were heterogeneous in design and content which precluded use of conclusive summative statements thus limiting the generalizability of our findings. Further, this scoping review included information from clinical commentaries, literature reviews, and a Delphi study due to the overall lack of literature reporting on interventions for LHBT. This impacts the quality of the reported information and limits generalizability. Further, we reported the frequency of intervention themes which does not necessarily reflect the importance of identified themes. Lastly, only English-language articles were included which increases the risk of language bias.
ConclusionsThe primary aim of this review was to present and describe interventions used to treat individuals with biceps tendinopathy. Six RCTs were identified that primarily reported on the use of therapeutic modalities to treat LHBT tendinopathy. Expert commentary based on literature reviews, clinical commentaries and a Delphi study described a multimodal approach (including exercise) for the treatment of biceps tendinopathy. Overall, physical therapy interventions described align with recommendations for individuals with shoulder pain, however, recommendations for the management of individuals with LHBT tendinopathy did not provide sufficient detail (including dosing and progression) to guide practicing clinicians. Future research is needed due to the overall lack of evidence and literature available.
This work was supported by The American Academy of Orthopedic Manual Physical Therapists (AAOMPT) under a grant from Cardon Rehabilitation (Ontario, Canada). Neither AAOMPT nor the funding agency had any role in the study design, analysis, interpretation, or decisions about publication.
This scoping review did not require ethics approval from the Colorado Multiple Institutional Review Board and from the Human Research Ethics Committee at the University of Newcastle, Australia.