Virtual reality-based therapy (VRBT) has been recently used in rehabilitation programs, as it can improve patient's adherence to treatment. However, patients’ acceptance of VRBT has been scarcely investigated.
ObjectiveTo qualitatively analyze the perceptions and preferences of patients about the inclusion of VRBT to a conventional cardiovascular rehabilitation program (CRP).
MethodsFifteen patients from a randomized clinical trial participated in focus groups for qualitative assessment.
ResultsPatients demonstrated good acceptance and satisfaction of VRBT. Physical and psychosocial benefits were highlighted, and patients reported the perception of higher exercise intensity in VRBT then when doing conventional training. In addition, the frequency of VRBT (once a week), associated with conventional treatment was reported as satisfactory. Cognitive aspects that influenced participation to the new approach were also raised by study participants.
ConclusionPatients with cardiac conditions demonstrated satisfaction with the inclusion of VRBT in a conventional CRP, demonstrating that VRBT has the potential to be a new approach for this patient population, allowing training diversification. Benefits perceived by patients include physical, mental, and social aspects.
Trial RegisteredNCT04336306 (https://clinicaltrials.gov/ct2/show/NCT04336306)
Virtual reality-based therapy (VRBT) has been identified as a new tool for physical therapy treatments.1,2 Advantages of using this tool include, the variety of games that can be used for therapeutic purposes, the potential for offering resources that allow patients to adapt more easily, transparency for data storage, and remote access of online data. Another advantage is that VRBT can be applied using different equipment, such as smartphones,3 which can facilitate accessibility.
The literature shows that VRBT increases motivation,3 which is essential in the treatment of individuals with cardiac conditions, because lack of motivation is related to low adherence to treatment.4–7 Studies have demonstrated that VRBT application in individuals with cardiovascular diseases (CVD) is a therapy with potential to increase functional capacity in patients with heart failure,8 and may promote acute physiological hemodynamic and autonomic responses similar to those obtained in a conventional cardiovascular rehabilitation program (CRP).9,10
A previous study conducted by our research group11 showed that the inclusion of VRBT sessions to conventional CRP increased patient's adherence to the first sessions of treatment. To improve knowledge about the inclusion of VRBT with a conventional CRP, and obtain new perspectives from patients regarding this treatment combination, the present study aimed to qualitatively analyze the perceptions and preferences of patients regarding the inclusion of VRBT to a conventional CRP, and understand how VRBT affects patient's adherence to CRP. This information can allow the development of strategies with higher adherence levels.
MethodsParticipants from this study were part of a randomized clinical trial (RCT) that evaluated two physical training groups.9 One group performed only conventional CRP (three sessions of conventional CRP in a week) and the other group performed VRBT associated with conventional CRP (one session of VRBT and two sessions of conventional CRP in a week) for 12 weeks. In the CRP session, the warm-up consisted of stretches and exercises for the upper limbs, lower limbs, and both combined. The exercise training phase consisted of exercises performed on a treadmill. In the VRBT session, the warm-up was performed using "Just Dance 2015" game, in which patients reproduced choreography in a previously defined sequence. The exercise training phase was performed through "Shape Up" exercise games following a virtual therapist. The group that performed VRBT sessions included with conventional CRP training were invited to participate in this qualitative study. During VRBT, the exercise intensity was the same as used in the conventional CRP (40-70% HRR for patients with CVD and 60%-80% HRR for those with cardiovascular risk factors). The training protocol has been published in detail previously.9
At the end of the clinical trial, all 27 patients were invited to participate in focus groups to collect qualitative data. Fifteen patients opted to participate in this study and, after being informed about the study's procedures and objectives, signed the informed consent form. The qualitative study was approved by the Research Ethics Committee of Universidade Estadual Paulista (UNESP), Presidente Prudente, SP, Brazil (n° CAAE: 29742920.9.0000.5402).
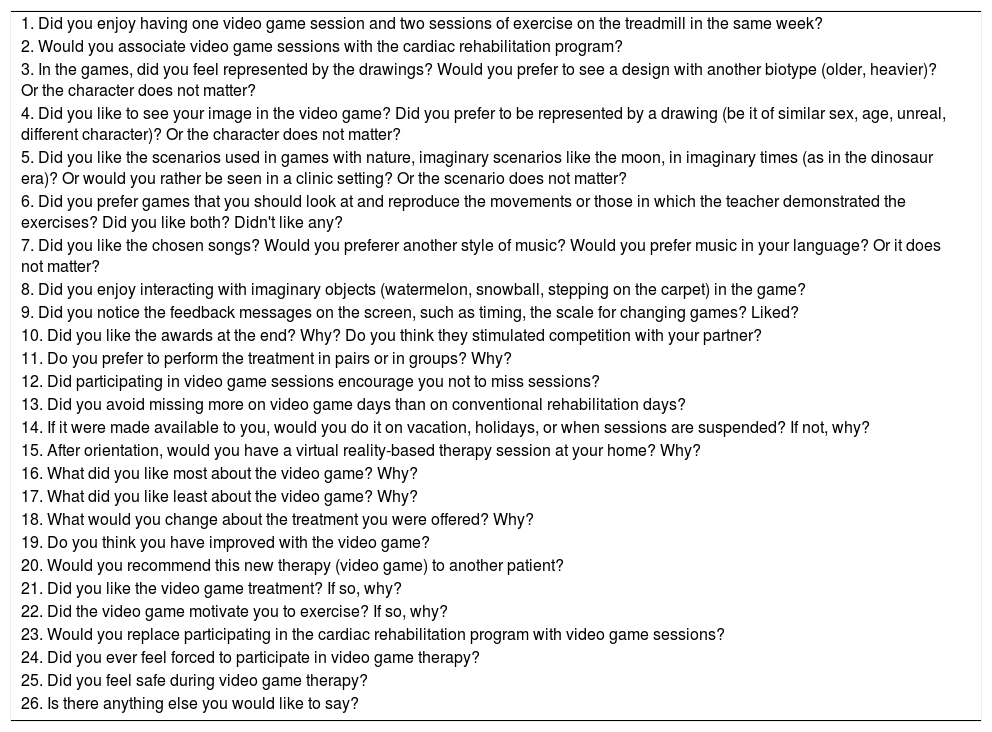
The focus group meetings were performed with 3 to 7 participants, had an average duration of 60 minutes, and were conducted by a female moderator, a PhD student, with previous experience in qualitative research and cardiovascular rehabilitation, who had no previous contact with the participants. A second researcher, who also had no previous contact with study participants, participated in the interview to take notes. To conduct the focus group, the moderator used an interview script, previously developed, containing the open-ended questions listed in Table 1.
Script of questions used in the focus group with patients.
The focus group meetings were conducted in a university study laboratory, where the clinical trial was conducted. The meetings were audio-recorded using a recording device (OLYMPUS / VN-8100PC, Tokyo, Japan) and transcribed verbatim. During the focus group meetings, data were collected up to the theoretical saturation point, that is, until the moment when no new information was obtained.12,13
Analysis of qualitative dataAfter the verbatim transcriptions of the statements obtained in the focus group meetings, analyses for identification and classification into categories were performed by three independent researchers. The analysis was developed by categorization, organization, and compaction of the data. Thus, a content analysis was performed, which consists of the description of phenomena, allowing the researcher to understand the data by refining the words into smaller categories related to the content.13 Therefore, it is possible to reduce the number of words in fewer categories, aiming at providing new knowledge for new actions.13
Finally, the researchers performed a triangulation, which consisted of a discussion about the differences in the results, to reach a consensus. Subsequently, the results were forwarded to 10% of the participants to confirm whether the results were consistent with the focus groups, and whether they really reflected participants’ views and perspectives.
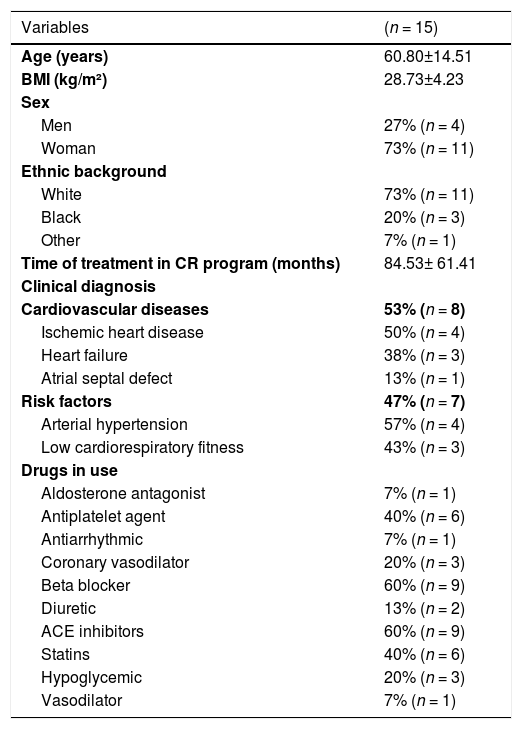
ResultsThe sample characterization is presented in Table 2
Patients'charactheristics.
Legend: ACE, angiotensin II converting enzyme; BMI, body mass index; Ca+, calcium;. The results are expressed as mean and standard deviation, or as a percentage and absolute number.
A qualitative analysis identified the following three themes: 1) “VRBT Features that influence patients' motivation and adherence”; 2)“Patient profile ”; and 3) “VRBT home viability”.
Theme 1- VRBT Features that influence patients' motivation and adherenceIn general, patients reported the perception of higher exercise intensity during VRBT then during conventional training, and the importance of a familiarization period with the new therapy. In addition, the frequency of VRBT (once a week), associated with conventional treatment was reported as satisfactory. The patients did not reach a consensus regarding the accomplishment of the VRBT in pairs or in groups, some patients reported that the pair activity provides better game / patient interaction and other patients reported that group activity could increase the fun of the therapy. The games used are commercial games, with prizes at the end of the games, which generated competition during the therapy, which provided greater stimulus when performing the exercises. On the other hand, the disappointment of loss in the game was mentioned by some patients. Game components, such as characters, scenarios, music, interaction with imaginary objects, and feedback messages were aspects that drew patients` attention. In general, patients were satisfied with the VRBT and enjoyed the variety of approaches used in the program. In addition, patients reported physical, mental, and social benefits provided by VRBT. However, most patients believe that VRBT did not influence adherence and motivation. Only one patient reported greater adherence to treatment due to VRBT, and two other patients reported that they felt more motivated to perform the VRBT sessions. - “I would associate. Because I loved it, that's exactly what she said, because we work hard too.” (Subject 7, woman, 72 years old) - “Ah, I think it was good for me, right? I even got better, because I could even follow the exercises correctly, except in the first days, but then I thought it was good.” (Subject 9, woman, 80 years old) - “So, look why it happened, there were two of us, so there was a little competitiveness. I think it's good for us ... because you are looking to improve yourself.” (Subject 7, woman, 72 years old) - “When you are winning, you are happy, but when you lose you get a little upset ...” (Subject 1, woman, 46 years old) - “I think our image was really cool! (in-game image feedback) ... I think even to be correcting posture, seeing the sequence of exercises.” (Subject 3, male, 47 years old) - “The award, she valued what we were able to do best.” (Awards) (Subject 3, male, 47 years old) - “Was good. Mainly because I have been participating for 10 years, you know, and I found something different, like, it left that routine, you know, from exercise and everything.” (Subject 5, woman, 39 years old) - “It improved agility, because it works more the head, more the body, more everything.” (Subject 7, woman, 72 years old) - “I would definitely recommend ... mainly to people over 50, 60 years old, I think so ... Because ... for example, because of the mind.” (Subject 8, woman, 64 years old) - “For me, yes ... I keep doing it at home ... I stopped physical therapy and I keep doing it by application.” (Subject 13, woman, 30 years old)
This theme encompasses information related to individual characteristics that can influence VRBT practice. Patients reported that advanced age and lower cognitive and functional capacity are factors that limit the performance of the proposed exercises. As a suggestion, they suggested that a homogeneous selection of participants would be interesting, as people with the same functional level would present better VRBT performance as a group. - “A little because of my age, mine, my structure, I can't take much effort.” (Subject 10, woman, 79 years old) - “It is in pairs I think it would be more interesting if you put two people on the same level of physical conditions, right?” (Subject 15, woman, 57 years old)
VRBT was considered to be a potential home therapy, without face-to-face supervision of therapists, after receiving previous guidance. On the other hand, some patients reported that they would face problems in performing this therapy at home, due to the need for commitment required, and safety concerns. Finally, some patients reported that the viability depends on intrinsic capacity of self-knowledge. - “Today we have the experience. Just like the question you already asked, “Would you do it at home?”, Today with experience, but within the limits of each one.” (Subject 3, male, 47 years old) - “Yes, but all this in my case, with limitations! Likewise, I still have cardiac problems that I feel bad with excess. So, everyone knowing their limit to perform at home alone, has to be careful.” (Subject 3, male, 47 years old) - “You are safe (presence of the therapist in the VRBT), you are not left with that insecurity, “oh something will happen”.” (Subject 7, woman, 72 years old)
In general, the inclusion of VRBT to a CRP demonstrated good acceptance by patients, who reported physical and psychosocial benefits gained with the therapy. In addition, elements related to the intensity and frequency of carrying out the VRBT were identified, as well as the physical and cognitive aspects of the individuals who influence the conduct of this therapy.
The satisfaction and perception of benefits regarding physical, mental, and social aspects, reported by patients, corroborate the findings of a study developed by Meneghini et al,14 where, adults and elderly, submitted to a training protocol with sports exergames (Xbox 360 Kinect Sportstm) reported psychological benefits, such as improved self-esteem, concentration, mood, and even reasoning and memory, in addition to improvements in agility and benefits in social interaction, resulting from the exchange of experiences and the creation of friendships. The perception of physical, mental, and social benefits found in our study, may explain the fact that patients mention VRBT to other individuals with CVD.
Regarding motivation, most patients reported that there was no VRBT influence on motivation and adherence to the CRP. Patients justify this aspect, as they state that previous awareness of the regular physical activity importance for patients with cardiac conditions is clear to them. In fact, the literature points out that the influence of beliefs prior to CRP, related to the benefits that physical training provides to patients with cardiac conditions, directly influences these individuals' adherence to physical exercise.15 Thus, we believe that this finding justifies the fact that most patients reported that their adherence to the practice of physical exercise is linked to awareness of its importance. In addition, the playful characteristic of this type of therapy provided motivation for two patients, which also meets the findings of previous studies.16,17
Patients with cardiac conditions report a perception of higher intensity in the VRBT program.9 In a previous study, a greater magnitude of RPE (p < 0.01) during the execution of VRBT and until 5 minutes of recovery was observed. Additionally, 74% (n = 20) of patients reached their heart rate reserve during the intervention and 33% (n = 9) exceeded heart rate reserve. However, this higher perception of exercise intensity, was related by some patients to difficulties in following the proposed exercises, highlighting the need for a period of familiarization to increase patient performance.
Patients also reported that the best way to perform the VRBT is in association with conventional therapy, as conducted in the present study. Patients stated that both therapies are important for physical well-being. There was no consensus regarding preferences to conduct the therapy in pairs or in groups, however, some patients reported that VRBT conducted in pairs helps to maintain the focus on therapy, improving game-patient interaction, while other patients reported that VRBT conducted in a group could increase the fun of the therapy and, consequently, the motivation.
It is important to note that the games used in this study are commercial games that have been adapted to the routine implemented for VRBT. These games promote the stimulus of competition among the participants with prizes at the end of the games and, in some cases, this competition provided a greater stimulus when performing the exercises.
Previous studies have shown that competition between patients stimulates motivation and improves individual's physical performance,18,19 however, this stimulus also depends on personal characteristics, and thus, in some cases, demotivation from this competition may occur.20 However, this fact was not observed in the present study.
Regarding the components of the games, such as characters, scenarios, music, interaction with imaginary objects, and feedback messages, patients showed contentment and satisfaction, the visualization of their own image on the game screen was a factor that helped in performing the exercise properly and enabled patient-game interaction by promoting greater stimulation.
The possibility of viewing the patient's image in real time allows the correction of postures and movements during the VRBT, which facilitates the correct execution of the exercises and the achievement of satisfactory results in terms of injury prevention due to the incorrect execution of exercises.21 The availability of greater diversification of music and games and translation into the source language, were characteristics of the games cited as aspects that needs improvement.
Factors such as advanced age, lower cognitive capacity, and lower functional capacity seem to make it difficult to perform the exercises proposed during the VRBT sessions. It is known that during the aging process there are physical and cognitive changes, which can negatively influence the practice of physical activity in general,22,23 which may explain why these complaints came from some of the patients. These factors influence the conduct of VRBT, considering that this type of therapy contains combined and more complex exercises than conventional therapies.9
In addition, the patients also stated that people with the same functional level would perform better in VRBT when conducted in pairs, so the homogeneous selection of the participants should be an aspect to be considered in future programs.
The VRBT advantages, related to data access and cost-benefit, associated with beneficial effects and safety,10 allow to consider its use as a potential home therapy without supervision. However, most patients believe that it would be possible if there was a previous period of familiarization. However, difficulties with adherence and concerns about the safety of VRBT without supervision, such as the fear of exceeding physical limits were presented as limiting factors for home therapy.
As a suggestion for the implementation of home VRBT without supervision, the assessment of viability considering the individual's ability to know their limitations is an important aspect, which was presented by some participants. It is known that this aspect is recommended for performing phase four of a CRP, that is, stable patients with the ability to assimilate self-monitoring of training are eligible to perform this phase,24 therefore, we assume that it is possible to conduct this VRBT at home.
As a limitation of this study, some of the patients who participated in the previous study did not participate in the focus group. All patients were invited, but 12 of them did not participate, with 11 giving a justification: moving to another city (n = 2), illness (n = 3), work (n = 4), and personal problems (n = 2).
ConclusionGiven the above, we can say there was satisfaction with the proposed therapy and its elements were well accepted by some patients. But most patients reported that there was no VRBT influence on motivation and adherence to the CRP, justifying that their adherence to the practice of physical exercise is linked to awareness of its importance.
The authors would like to thank the Laboratory of Stress Physiology and Laboratory of the Faculty of Sciences and Technology at São Paulo State University, for all assistance during this work. Source(s) of support: The present study was undertaken with grant funding from the Foundation for Research Support of the State of São Paulo (FAPESP) 2017 / 12254-8.