Scapular rehabilitation exercises should target appropriate muscles. Recently, adding external rotation resistance to scapular exercises has gained interest. Moreover, clinical experts advise kinetic chain integration into shoulder rehabilitation exercises.
ObjectiveTo investigate scapular muscle activity during kinetic chain variations of a prone elevation exercise.
MethodsActivity of the upper (UT), middle (MT), and lower (LT) trapezius and serratus anterior (SA) muscles was determined with surface electromyography (EMG) in 31 asymptomatic participants during six prone elevation exercise variations. Variation was created by adding external rotation resistance, adding trunk extension, or changing exercise position (prone on a Swiss ball with knees or feet supported, or prone on a physiotable). All data were normalized as a percentage of maximal voluntary isometric contraction (% MVIC). For each muscle, a Friedman's ANOVA was conducted to analyse statistical differences in EMG signal intensity between exercises.
ResultsThe LT was moderately (42 - 48% MVIC) and MT highly (63 - 66% MVIC) activated during all exercise variations. No significant differences between exercises for these muscles could be detected. Adding external rotation to a prone elevation exercise decreased UT activity while adding trunk extension increased UT activity. Altering exercise position had no influence on scapular muscle activity except increased UT activity when lying prone on a physiotable with trunk extension.
ConclusionProne elevation exercises are appropriate for facilitating LT and MT activity. Adding external rotation inhibits UT activity while UT facilitation could be achieved when adding trunk extension.
Shoulder pain has been associated with abnormal scapular position or motion, also referred to as scapular dyskinesis.1-5 Although it is still unclear whether scapular dyskinesis is the cause or consequence of shoulder pathology, alterations in scapular kinematics have been related to a variety of shoulder pathologies such as shoulder instability and rotator cuff related shoulder pain.3-6 Different possible underlying mechanisms could potentially contribute to abnormal scapular kinematics such as a lack of soft tissue flexibility or a lack of muscle performance.7 Regarding the latter, decreased or excessive scapular muscle activation might hinder adequate scapular function.8 Scapular dysfunction is often related to a lack of activity in serratus anterior (SA) and middle (MT) and lower (LT) trapezius with no consensus on whether the upper trapezius (UT) is activated too much9,10 or too little.11,12 Additionally, research has shown that exercise therapy, targeting the appropriate scapular muscles, could improve scapular dysfunction.13-15 Exercise selection should thus be focused on producing high activity in hypoactive muscles combined with low activity in hyperactive muscles.7
Electromyography (EMG) is a frequently used method to investigate scapular muscle activity during therapeutic exercises and could aid in suggesting recommendations for appropriate exercise selection.16-21 Several studies have examined scapular muscle activity during elevation exercises while standing.8,22-24 But, performing shoulder elevation exercises from a prone position could be of interest for several reasons. First, exercises in prone could be chosen to match sport-specific characteristics. As such, swimmers have to exercise lying supine or prone mainly focusing on scapular concentric endurance.7,25 In this population, positions that require considerable amounts of core stability are preferred, which could be enhanced by performing exercises on an unstable surface. A prone elevation exercise is mentioned for this purpose where individuals are lying prone on a Swiss ball performing bilateral arm elevation movements.7 Second, exercises in prone have been proposed to better target trapezius muscle activity.26,27 Werin et al.27 found significantly higher EMG signal intensity in the 3 trapezius muscle parts in the prone compared with side and standing positions. The elevated arm position in prone is probably more demanding for the trapezius muscles due to gravity compared to the other positions. Enhancing MT and LT activity could also be achieved by adding a humeral external rotation resistance to a scapular elevation exercise.22,28 Therefore, the first purpose of this study was to investigate the effect of adding humeral external rotation to variations of a prone shoulder elevation exercise on scapular muscle activity (UT, MT, LT, and SA).
Furthermore, clinical experts advise integration of the kinetic chain into shoulder rehabilitation exercises to address functional daily activities and sport-specific demands.7,29-31 Previous studies have found altered scapular muscle activity by changing upper body position,32 lower body position/exercise position,20,27,32,33 or by adding trunk rotation.34,35 Therefore, the second purpose of this study was to assess scapular muscle activity during kinetic chain variations of a prone shoulder elevation exercise. This variation is achieved by (1) altering the exercise position of a prone shoulder elevation exercise or (2) adding trunk extension to a prone shoulder elevation exercise.
MethodsParticipantsIndividuals were recruited via advertisement on social media. They were included in this cross-sectional study if they were free from pain in the upper limbs, lower limbs, and spine for at least 6 months prior to testing and never had fractures or orthopedic surgery. They were excluded if they performed overhead sports or upper limb strength training for more than 6 hours per week. Informed consent was obtained from all individual participants included in the study. This study was approved by the Ethical Committee of Ghent University Hospital and was conducted in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans.
An a priori sample size calculation was conducted in G*Power (version 3.1.9.2) with an effect size of 0.62, a significance level of .05, and a desired power of 0.80 (t tests; Wilcoxon singed-rank test). The effect size was calculated based on EMG signal intensity of the UT reported in a previous study that investigated scapulothoracic muscle activity during kinetic chain variations of a bilateral elevation exercise.32 The calculation revealed that a total sample size of at least 24 participants was required.
InstrumentationBefore surface electrode placement, the skin surface was shaved, scrubbed, and cleaned with alcohol to minimize skin impedance. Bipolar surface electrodes (Ag/AgCl Ambu® BlueSensor P, REF P-00-S/50, 40.8 × 34 mm, Ballerup, Denmark) were placed parallel to the muscle fibers of the three parts of the trapezius muscle and the SA on the dominant shoulder with a reference electrode over the ipsilateral clavicle. Arm dominance was determined as the arm used to throw a ball. The recommendations from the Surface EMG for the Noninvasive Assessment of Muscles (SENIAM) were followed for electrode placement and interelectrode distance.36 All surface electrodes were looped and taped on the skin to prevent them from being accidentally detached during arm movements with consideration of a full elevation range of motion. The electrodes were connected to a 16-channel Myosystem 2000 EMG receiver (Noraxon USA Inc, Scottsdale, AZ). The sampling rate was 1000 Hz, and all raw myoelectric signals were preamplified (overall gain, 1000; common rate rejection ratio, 115 dB; signal-to-noise ratio, <1mV root-mean-square baseline noise). Additionally, an OptiTrack Flex 3 highspeed camera (100 frames per second) was used to track direction of motion during all exercises for the purpose of automatically and more precisely mark the start and end for each exercise repetition during analysis. For this purpose, one reflective marker was applied in the middle of the dorsal side of the dominant upper arm with double adhesive tape. The camera was installed perpendicular to this reflective marker.
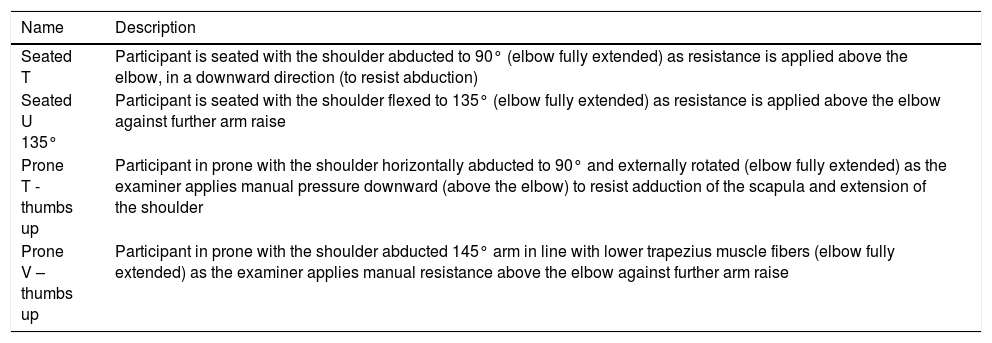
Testing procedureIn the first part of the investigation, maximal voluntary isometric contractions (MVICs) were performed in a randomized order for normalization.37 Consistent with the protocol of Castelein et al.,37 a set of 4 different isometric test positions were performed for normalizing the EMG data: (1) seated T, (2) seated U 135°, (3) prone T - thumbs up, and (4) prone V – thumbs up. The 4 different test positions are described in Table 1. Resistance was applied by the same researcher just proximal to the elbow into further upward movement. The researcher held the resistance while the individual exerted a maximal force against it. Three repetitions of five seconds were performed with 15 seconds of rest in between as controlled by a metronome (60 beeps/min). Individuals were verbally encouraged to reach their maximal effort in 2 seconds and sustain that effort for another 5 seconds. Between MVIC measurements of two different muscles, 15 seconds of rest was provided.38
Description of the 4 tests for maximum voluntary isometric contractions.
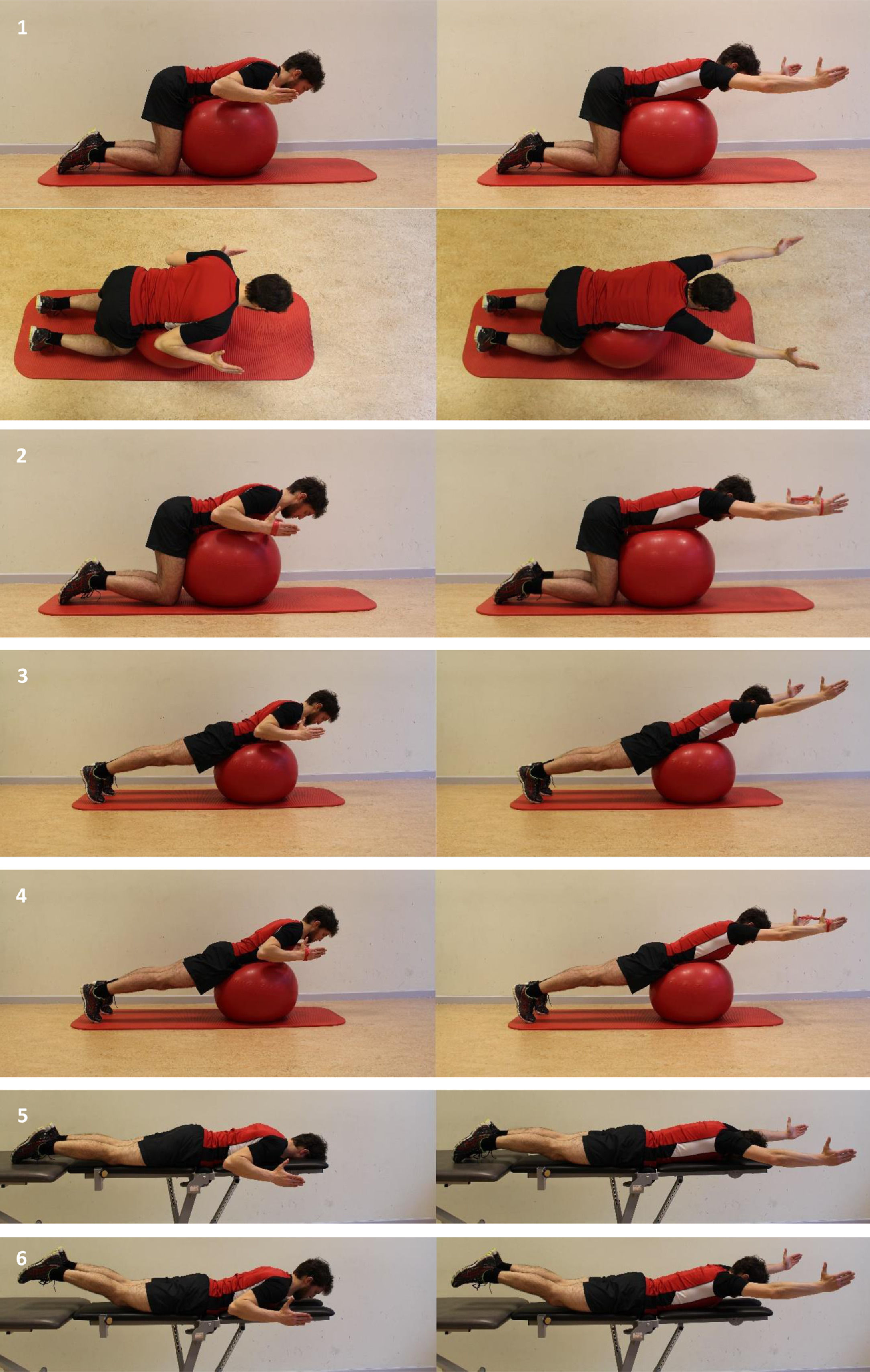
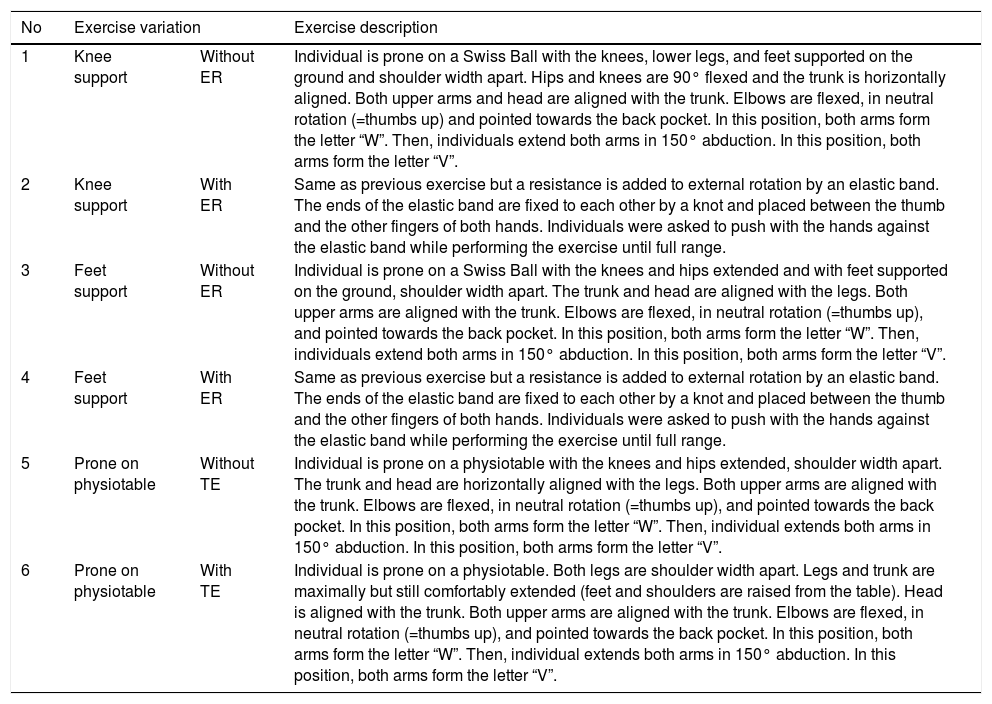
In the second part of the investigation, individuals randomly performed six variations of a prone elevation exercise, also called the “W-V” exercise because of the position of the arms at start and at end elevation (Fig. 1). In the starting position, elbows are pointing at the back pocket (=both arms together form the letter “W”). In three seconds, both arms are fully extended in 150° of abduction with the thumbs upwards (=both arms together form the letter “V”). In another three seconds, both arms were brought back into the starting position. A metronome was used to ensure correct exercise speed (60 beeps/min). In total, five repetitions of each exercise variation was completed with a resting period of four minutes in between each exercise variation. These six exercise variations consisted of a prone elevation on a Swiss Ball with the knees supported and without (exercise 1) or with addition of an external rotation resistance (exercise 2); on a Swiss Ball with the feet supported and without (exercise 3) or with external rotation resistance (exercise 4), on a physiotable without (exercise 5) or with trunk extension (exercise 6). Standardized exercise instructions are provided in Table 2. Quality of exercise performance was checked and corrected by the examiner. For exercises 2 and 4, the resistance to external rotation was created by an elastic band. The amount of applied resistance (i.e. color of the elastic band) was chosen so that participants rated the exercise effort between 12 and 18 on a 20-point Borg scale, which is considered as needed to train strength.39 This was determined in a pilot study with subdivision into sex and body weight (50-59kg, 60-69 kg, 70-79kg, and 80-89kg).38,40 This resulted in the use of a yellow elastic band (Thera-Band®) for women and red (Thera-Band®) for men for all weight categories.
Demonstrating the 6 exercises studied: prone elevation exercise: (1) with knee support without external rotation (above, lateral view; below, superior view) (2) with knee support with external rotation, (3) with feet support without external rotation, (4) with feet support with external rotation, (5) on physiotable without trunk extension, (6) on physiotable with trunk extension
Standardised exercise instruction for the six W-V exercise variations.
Abbreviations: ER, external rotation; TE, trunk extension.
The Noraxon Myovideo module MR3.6 software program (Noraxon USA, Inc) was used for signal processing. For all raw EMG signals, cardiac artefact reduction was performed followed by rectification and smoothing (Root Mean Square, window 100 ms). For all MVICs, the mean EMG signal intensity of the three intermediate seconds of every repetition and for each muscle was used for further analysis. The normalization reference level for each of the scapular muscles was taken as the maximal activity level generated across the four MVIC tests.37 For all exercises, the analysis of marker motion identified the start and end of each repetition. Mean EMG signal intensity for each muscle was calculated across the three intermediate repetitions for all exercises. Those values were then normalized and subsequently expressed as a percentage of MVIC for further analysis.
Statistical analysisStatistical Package for the Social Sciences (SPSS) version 25 (IBM Corporation, Armonk, NY) was used for statistical analysis. Trial-to-trial reliability for the three MVIC trials for each test position was calculated with intraclass correlation coefficients (ICCs) (2-way random model, type consistency). To examine absolute reliability, the standard error of the measurement (SEM) was calculated, using the method of Weir.41 Data showed nonnormal distribution based on the outcome of the Shapiro-Wilk test and visual inspection (histogram). As a result, descriptive data are presented as median and interquartile range (Table 3). Although less suited for nonnormal distributed data, means, standard deviations (SD), and confidence intervals (CI) were also determined for the normalized EMG values (% MVIC) for each muscle and for each exercise variation (Table 3) to compare our results with others. To facilitate the interpretation, the values of EMG were categorized as low activity (<20% MVIC), moderate activity (20%-50% MVIC), or high activity (>50% MVIC).38
| Muscle | Descriptives | Exercise number | p value | p value | |||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | Friedman's ANOVA | Pairwise comparisons (Bonferroni correction) | ||
| UT | Median [IQ range]aMean ± SD [95% CI]b | 33 [20] | 22 [17] | 35 [22] | 23 [15] | 34 [23] | 40 [30] | <0.001c | 1-2: <0.001d |
| 1-3: 0.8 | |||||||||
| 1-4: <0.001d | |||||||||
| 36 ± 20 (29, 43) | 28 ± 20 (21, 35) | 36 ± 19 (29, 43) | 27 ± 17 (21, 33) | 36 ± 18 (29, 42) | 42 ± 23 (34, 51) | 1-5: >0.9 | |||
| 1-6: 0.002d | |||||||||
| 2-3: 0.001d | |||||||||
| 2-4: 0.6 | |||||||||
| 2-5: 0.0031d | |||||||||
| 2-6: <0.001d | |||||||||
| 3-4: <0.001d | |||||||||
| 3-5: >0.9 | |||||||||
| 3-6: 0.001d | |||||||||
| 4-5: 0.002d | |||||||||
| 4-6: 0.001d | |||||||||
| 5-6: 0.001d | |||||||||
| MT | Median [IQ range]a | 62 [54] | 66 [43] | 58 [49] | 61 [47] | 62 [42] | 63 [42] | 0.4 | N.A. |
| Mean ± SD [95% CI]b | 63 ± 29 (52, 73) | 63 ± 29 (53, 74) | 64 ± 31 (53, 76) | 64 ± 29 (53, 74) | 66 ± 28 (56, 77) | 64 ± 29 (53, 75) | |||
| LT | 43 [19] | 47 [20] | 40 [20] | 47 [16] | 44 [20] | 39 [28] | 0.045c | 1-2: 0.04 | |
| 1-3: 0.3 | |||||||||
| 1-4: 0.3 | |||||||||
| 1-5: 0.8 | |||||||||
| 1-6: 0.02 | |||||||||
| 2-3: 0.1 | |||||||||
| 2-4: 0.4 | |||||||||
| 2-5: 0.08 | |||||||||
| 2-6: 0.02 | |||||||||
| 3-4: 0.1 | |||||||||
| 3-5: 0.6 | |||||||||
| 3-6: 0.3 | |||||||||
| 4-5: 0.4 | |||||||||
| 4-6: 0.07 | |||||||||
| 5-6: 0.3 | |||||||||
| Mean ± SD [95% CI]b | 46 ± 21 (39, 54) | 48 ± 15 0 (42, 53) | 45 ± 21 (37, 52) | 46 ± 13 (41, 51) | 46 ± 22 (38, 54) | 42 ± 20 (35, 50) | |||
| SA | Median [IQ range]a | 19 [12] | 18 [12] | 18 [11] | 17 [10] | 18 [12] | 21 [12] | <0.001c | 1-2: 0.8 |
| 21 ± 10 (17, 24) | 20 ± 11 (16, 24) | 21 ± 9 (18, 24) | 19 ± 7 (16, 21) | 20 ± 9 (17, 23) | 23 ± 9 (20, 27) | 1-3: 0.8 | |||
| 1-4: 0.2 | |||||||||
| 1-5: 0.7 | |||||||||
| 1-6: 0.01 | |||||||||
| 2-3: 0.6 | |||||||||
| 2-4: 0.2 | |||||||||
| 2-5: 0.7 | |||||||||
| 2-6: 0.007 | |||||||||
| 3-4: 0.03 | |||||||||
| 3-5: 0.4 | |||||||||
| 3-6: 0.03 | |||||||||
| 4-5: 0.4 | |||||||||
| 4-6: 0.001d | |||||||||
| 5-6: 0.005 | |||||||||
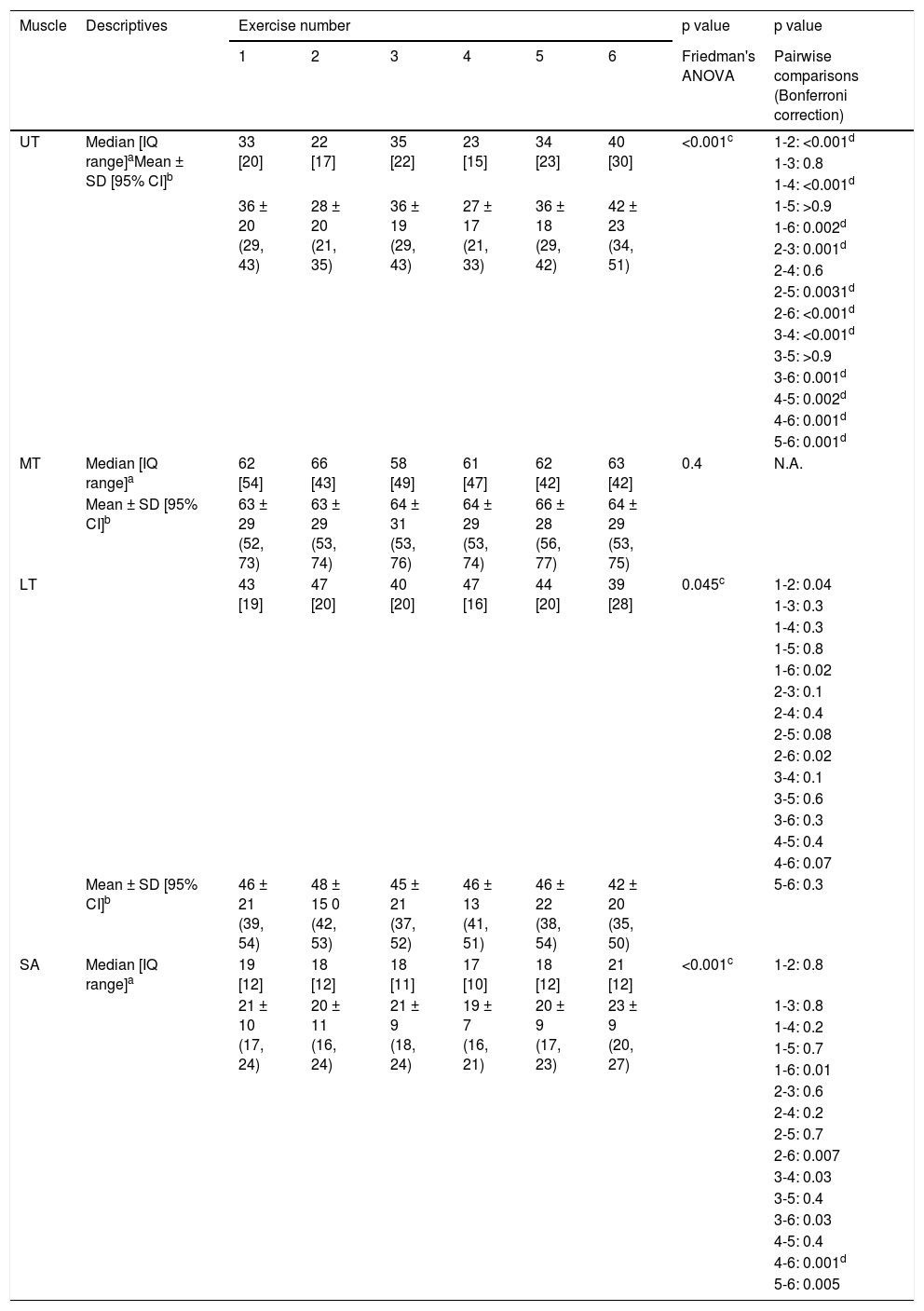
Data reported as mean ± SD (95% CI). Values are expressed in percentage of maximal voluntary isometric contractions (%MVIC): low <20 %MVIC, moderate 20-50 %MVIC, high >50 %MVIC.
p <0.0033 indicates statistical significance for the results of the pairwise comparisons after Bonferroni correction.
(1) Prone elevation with knee support without external rotation (2) prone elevation with knee support with external rotation, (3) prone elevation with feet support without external rotation, (4) prone elevation with feet support with external rotation, (5) prone elevation on physiotable without trunk extension, (6) prone elevation on physiotable with trunk extension
Abbreviations: ANOVA, analysis of variance; IQ, interquartile; LT, lower trapezius; MT, middle trapezius; N.A., not applicable; SA, serratus anterior; UT, upper trapezius.
To analyze statistical differences in muscle EMG signal intensity between the 6 exercise variations, nonparametric statistics were used. For each muscle (UT, MT, LT, and SA), a separate Friedman's ANOVA (analysis of variance) with 6 variables was conducted. Alpha level was set at 0.05. In case the Friedman's ANOVA revealed a significant result, post hoc tests were performed using a Wilcoxon signed rank test with correction for the number of test (i.e. Bonferroni correction for multiple comparisons).40 More specifically, when mutually comparing the 6 exercise variations, a total of 15 comparisons were made. As a result, alpha level was reset at 0.0033 (0.05/15 comparisons).42
ResultsThirty-one healthy individuals (16 women, 15 men; mean age 22.5 ± 1.3 years, weight 66.4 ± 9.2 kg, and height 175.1 ± 7.1 cm) were included in this study. The ICCs for the 3 MVIC trials for each test position show high trial-to-trial reliability with ICC values ranging from 0.965 to 0.987. The SEMs for each MVIC test positions vary between 67.6 and 113.5 microvolts. An overview of ICC and SEM values for all 4 MVIC test positions can be found in Online supplementary material.
The descriptive analysis and results of the Friedman's ANOVA are presented in Table 3. The Friedman's ANOVA yielded a statistically significant difference for UT (ꭕ2 (5) = 51.2, p<0.001), LT (ꭕ2 (5) = 11.3, p=0.045), and SA activity (ꭕ2 (5) = 22.9, p<0.001). For MT, the result of the Friedman's ANOVA was not significant (ꭕ2 (5) = 5.3, p=381). The results of the post-hoc tests with Bonferroni correction revealed significant differences across exercises for UT and SA but not for LT (Table 3).
DiscussionThe most important finding of the present study was that only UT activity is influenced by variations of a prone elevation exercise. Adding external rotation decreases UT activity. UT facilitation could be achieved by (1) adding trunk extension to the prone elevation exercise on a physiotable or, (2) altering exercise position together with trunk extension.
To investigate the effect of adding external rotation (ER) on scapular muscle activity, exercises 1 versus 2, and 3 versus 4 were compared because the only difference between them is the presence of an ER resistance. Exercise 2 and 4 (with ER) showed significantly lower UT activity compared to exercise 1 and 3 (without ER). Mean differences (95% confidence interval (CI)) are 7% MVIC (4%, 10%) and 9% MVIC (6%,13%), respectively. The significant decreased in UT activity with addition of external rotation resistance in the prone elevation exercise is possibly due to the activation of the posterior shoulder muscles that are responsible for shoulder external rotation during the entire W-V exercise (i.e. infraspinatus and teres minor muscles). Activation of these muscles could possibly lead to decreased UT activity as the UT muscle is not part of the posterior chain.43 Some authors advise limiting UT activity during scapular rehabilitation exercises9,10 and adding an external rotation resistance to a W-V exercise is thus preferred based on our results. Previous studies advised the use of an external rotation resistance during a standing elevation exercise for increasing MT and LT activity.22,28 Our results do not support this recommendation because MT and LT activities were unchanged when adding external rotation. This could be due to the difference in test position: a standing arm elevation compared to a prone position, which could influence the stabilizing function of the MT and LT. Moreover, activation levels for both muscles were already moderate (>40% MVIC for LT) to high (>60% MVIC for MT) in our study, which might limit a further increase.
For the second objective, scapular muscle activity was assessed during kinetic chain variations of a prone elevation exercise by means of adding trunk extension or altering exercise position. To investigate the influence of trunk extension, exercises 5 and 6 were compared. Our results showed higher UT activity with trunk extension with no significant differences for MT, LT, and SA. Mean difference in UT activity between exercise 5 and 6 was -7% MVIC (-11%, -3%).
Trunk extension is performed by elevating the trunk and legs which makes the exercise considerably more challenging. Possibly, the UT muscle is compensating for this intensified effort by increasing its activity. Adding trunk extension might thus be useful for exercise progression in scapular rehabilitation to promote higher UT activity, which is supported by some authors for patients with shoulder pain.11,12 Additionally, we assumed that MT and LT activity would also be increased because trunk elevation might enhance scapular retraction. Possibly, trunk extensor muscle activity is increased although activity in these muscles was not investigated in this study. Previous research found similar results as ours with no significant differences in activity for these muscles when a prone scapular retraction was performed with and without trunk rotation.35
To investigate the effect of changing exercise position, exercises 1, 3, 5, and 6 on the one hand and exercises 2 versus 4 (both with external rotation) on the other hand were compared because the difference between them is the exercise position. No statistically significant differences were found between exercises where only one variable in body support was changed i.e. mutually comparing exercises 1, 3, and 5 or comparing exercises 2 and 4. When two variables in body support changed, UT activity is significantly increased i.e. when performing the exercise lying prone on a physiotable with trunk extension (exercise 6) compared to when the exercise is executed lying prone on a Swiss ball with knees (exercise 1) or feet (exercise 3) supported. Mean differences (95% CI) between exercise 1 and 6 was -6% MVIC (-10%, -2%) and between exercise 3 and 6 was -6% MVIC (-10%, -3%).
Based on our results, it is difficult to attribute the altered UT activity to one specific reason because two variables in chain position were changed (i.e. body position and trunk extension). A possible explanation could be found as described above, the UT muscle is compensating by increasing its activity with increased exercise difficulty to perform the elevation as prime mover for upward scapular rotation. In contrast, when only one variable in body position was changed, scapular muscle activity was not influenced. These findings are useful in scapular rehabilitation for exercise progression by gradually loading the functional open chain. During the W-V exercise, this loading is created by altering body position. More specifically for swimmers, the sport-specific character of the W-V exercise could be made more challenging with changes in body position that require additional core stability.25 This could be established by exercise performance on a table (exercise 5) followed by lying prone on a Swiss ball with the knees supported (exercise 1) and finally with the feet supported (exercise 3). This functional exercise progression is possible without changing scapular muscle recruitment. Additionally, when decreased UT activity is desired in rehabilitation, exercise 1 and 3 could be replaced by exercise 2 and 4 respectively. If higher UT activity is desirable, exercise progression is also possible by performing the W-V exercise when lying prone on a table with trunk extension.
When looking at the mean normalized EMG values in Table 3, all scapular muscles (except SA in exercise 4) showed moderate (between 20% and 50% MVIC) to high (>50% MVIC) activity meaning that activity levels in all exercise variations might be suited for scapular muscle control or strength training purposes.19,44 The SA showed the lowest activity of all muscles with overall values of around 20% MVIC which is in line with previous research on SA activity during standing elevation exercises with and without external rotation22 or prone retraction exercises.35 It would be interesting to investigate whether addition of a load during a prone elevation exercise would affect scapular muscle activity because it has been shown to increase SA activity during standing elevation exercises.22,38
Overall UT muscle activity is the second lowest with significant fluctuations in EMG activity between exercise variations which is not the case for MT, LT, or SA activity. For this reason, exercises could be ranked with progressive UT activity. First exercise 4 (27% MVIC) and 2 (28% MVIC) with the lowest UT activity, followed by significantly higher UT activity in exercises 5 (36% MVIC), 3 (36% MVIC), and 1 (36% MVIC) and completed with the significantly highest UT activity in exercise 6 (42% MVIC). MT and LT activity was the highest during all exercise variations with activity levels between 40% and 50% MVIC for LT and >60% for MT. This finding supports the use of scapular retraction movements to enhance posterior shoulder muscle performance.19,40,45,46
The results of this study must be viewed with regard to its limitations. First, the influence of adding external rotation to a W-V exercise was only studied when lying prone on a Swiss ball with knees or feet supported. Due to practical reasons, it was not possible to add an external rotation resistance when lying prone on a physiotable. Second, extrapolation of these results to other age categories or patients with shoulder conditions should be done with caution because this study was performed on healthy, young participants. However, similar populations have been tested in previous EMG research, suggesting appropriate shoulder rehabilitation exercises.16,20,22,35,38,40 Third, this study evaluated four scapular muscles important for scapular control, which are often the scapular muscles of interest to examine with surface EMG. Other muscles such as the pectoralis minor, rhomboids, or levator scapulae might also have significant value in scapular control during rehabilitation exercises. But, these deeper lying muscles are not accessible through surface EMG. Fourth, this study did not include the timing of muscle activity which is also an important contributor to scapular dyskinesis. Fifth, the activity levels of shoulder external rotation muscles were not investigated in this study and could be the focus of further research. Additionally, investigating the effect of kinetic chain variations on core muscle activity (back and abdominal muscles) or shoulder external rotation muscles could be of interest.
ConclusionThe results of this research provide clinical information about which exercise variation to choose when targeting activity in specific scapular muscles, depending on which muscle is desired to be activated. Our research supports the use of a prone elevation exercise for enhancing LT and MT activity. Regarding UT activity, adding an external rotation resistance is preferred for decreasing UT activity while UT activity is facilitated when performing the prone elevation exercise lying prone on a table with trunk extension.
The authors would like to thank all participants for their voluntary participation and Adriaan Borms for the assistance with collecting the photo material.