Individuals with short resting pectoralis minor muscle length have been shown to have aberrant scapulothoracic motion when compared to individuals with long resting pectoralis minor muscle length. However, the degree to which the pectoralis minor muscle can be lengthened and whether or not scapulothoracic motion differs between individuals with short and typical resting pectoralis minor muscle length is unknown.
ObjectivesTo determine if: (1) pectoralis minor muscle elongation (percent pectoralis minor muscle can be actively and passively lengthened beyond resting length), (2) pectoralis minor muscle percent length change during overhead reaching, and (3) scapulothoracic motion during overhead reaching differ between individuals with short and typical resting pectoralis minor muscle length.
DesignTwo group comparison.
MethodsThirty healthy individuals were placed into a short or typical resting pectoralis minor muscle length group. A caliper was used to measure resting pectoralis minor muscle length and pectoralis minor muscle length during active and passive muscle lengthening. An electromagnetic tracking system was used to measure pectoralis minor muscle length change as well as scapular, humeral, and trunk motion during several arm elevation tasks. Pectoralis minor muscle elongation and length change during arm elevation tasks were compared between groups using independent t-tests. Two-factor mixed-model analyses of variance were used to compare scapulothoracic motion at arm elevation angles of 30°, 60°, 90°, and 120°.
ResultsPectoralis minor muscle elongation and pectoralis minor muscle length change during arm elevation did not differ between groups. Scapulothoracic motion did not differ between groups across arm elevation tasks.
ConclusionsAlthough resting pectoralis minor muscle length differed between groups, pectoralis minor muscle lengthening and scapulothoracic motion were similar between participants with short and typical resting pectoralis minor muscle length. Additional studies are needed to better understand the role of pectoralis minor muscle elongation on scapulothoracic motion.
The Alignment-Impairment model provides a framework for evaluating the role of shoulder girdle alignment, neuromusculoskeletal impairments, and aberrant movements in the development of shoulder pain and dysfunction.1 A postulate of this model is that various factors contribute to scapular alignment including thoracic spine alignment, shoulder girdle muscle strength, and soft tissue flexibility.1,2 Of the anteriorly located shoulder girdle muscles, the pectoralis minor muscle (PMm) is believed to influence scapular alignment and scapulothoracic motion.3
The relationship between resting PMm length and scapulothoracic motion has been studied in a healthy, young population.4 Individuals with short resting PMm length have been shown to have increased scapular internal rotation and reduced scapular posterior tilting during arm elevation when compared to individuals with long resting PMm length.4 This information is important because these motion patterns are similar to those reported in individuals with shoulder pain secondary to subacromial impingement,5 rotator cuff disease,6 and glenohumeral instability.6
It should be noted that Borstad and Ludewig4 compared motion between individuals with short and individuals with long resting PMm lengths. While this study provides information about the influence of resting PMm length on scapulothoracic motion, additional research is needed to better understand how to use these findings for clinical decision making. From a clinical perspective, it would also be important to know if scapulothoracic motion differs between individuals with short and individuals with typical resting PMm lengths. Information of this nature is in line with how findings obtained from clinical tests of muscle strength, ligamentous laxity, posture, and reflexes, for example, are used.
To the best of our knowledge, research on the influence of resting PMm length on PMm elongation (percent by which the PMm can be actively or passively lengthened beyond resting length) and percent PMm length change during arm elevation is lacking. Information about PMm elongation in individuals with different resting PMm lengths would help determine the extent to which resting PMm length measures can be used to make inferences about muscle tightness or shortness. Additionally, information about PMm length changes during overhead motions in individuals with different resting PMm lengths would allow for a better understanding of the role of PMm length on scapulothoracic motion. Furthermore, the influence of resting PMm length on scapulothoracic motion has only been studied during constrained tasks (tasks restricted to a specified plane of motion).4 However, functional overhead reaching tasks typically are not constrained to a specific plane of motion, and scapulothoracic motion has been shown to differ between constrained and unconstrained elevation tasks.7
The purposes of this study were to determine if: (1) PMm elongation, (2) PMm percent length change during overhead reaching, and (3) scapulothoracic motion during overhead reaching differ between individuals with short and typical resting PMm length. We hypothesized that when compared to individuals with typical resting PMm length, individuals with short resting PMm length would have: (1) decreased PMm elongation values, (2) smaller PMm percent length changes during overhead reaching, and (3) increased scapulothoracic internal rotation and less posterior tilt during overhead reaching.
MethodsParticipantsSample size was based upon a power analysis intended to detect a medium effect in scapulothoracic motion between groups. The a priori analysis (G*Power 3.1.9.28; power=0.80, alpha=0.05, effect size f=0.25) suggested a total sample size of 24 participants, which was rounded up to 30 (15 per group). Participants completed a screening form that consisted of questions related to current and past shoulder pain and injury; previous diagnosis of scoliosis; brachial plexus injury; and current neck, back, elbow, forearm or hand pain. Participants were included if they were 18–45 years old, had no current dominant shoulder pain, and could elevate their dominant arm to at least 130°. They were excluded if they had a previous injury to their dominant shoulder that required medical attention; neck, back, elbow, forearm, wrist, or hand pain; scoliosis; brachial plexus injury; or nerve palsies that affected their shoulder girdle or upper extremity. Height and weight measures were obtained with participants wearing shoes. Individuals provided informed consent as per the research protocol approved by Drexel University's, Philadelphia, PA, USA Institutional Review Board.
ProceduresData collectors were trained by the lead author using previously established protocols.9 This consisted of two training sessions each lasting approximately 30–45min. During the first training session all measurement procedures were reviewed. Data collectors practiced the procedures and a second session was scheduled with the lead author to ensure that measurements were being performed correctly.
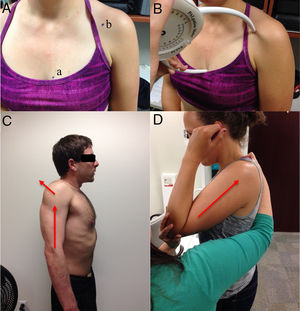
Pectoralis minor muscle lengthPectoralis minor muscle length was defined as the distance between the inferior-medial aspect of the fourth rib, one fingerbreadth lateral to the sternocostal junction, and the inferior-medial aspect of the coracoid process.4 These bony landmarks were palpated and marked with a pen following our previously established protocol (Fig. 1A).9 Dominant side PMm length was measured using a Palpation Meter (PALM; Performance Attainment Associates, St. Paul, MN) under three conditions: resting posture, actively lengthened, passively lengthened. PMm length during scapular plane arm elevation and shelf reaching tasks was measured with the Flock of Birds electromagnetic tracking system (Ascension Technology Corporation, Burlington, VT) and will be described in the shoulder girdle kinematics section.
Resting PMm length was measured with the participant standing in their natural relaxed posture with arms at their side (Fig. 1B). For actively lengthened measures, participants were asked to maximally elevate and retract their scapulae (Fig. 1C). While maintaining this position, bony landmarks were re-palpated and re-marked (if necessary) to account for any soft tissue movement. The passive length measure was performed by one of two physical therapists (KG or DE; 3 and 28 years of experience, respectively). The participant's dominant shoulder was placed in approximately 30° of flexion. The therapist placed their hand on the distal humerus and, while stabilizing the participant's trunk, pushed their shoulder in a superior/posterior direction until firm tissue resistance was encountered (Fig. 1D).10 To decrease examiner bias, the recording surface of the PALM faced away from the examiner for all measurements. The measurement was read and recorded by a second examiner (JM or TP) who then returned the PALM to the zero setting. For all PMm length measures the average of two measurements (within 0.5cm of one another) were used in subsequent analyses. Previous research in our lab has demonstrated acceptable measurement properties for our PMm length measurement procedures.9
Participant's resting PMm length and height were used to generate the PMm index (PMi=[PMm length/height]×100).4 Participants were assigned to either the short (PMi<8.9) or typical (8.9≤PMi<10.5) group. Individuals with a PMi≥10.5 were excluded from the study as they demonstrated a long resting PMm length. Group cut points were based upon the mean±one standard deviation4 of the PMi from previous work in our lab.9
Scapulothoracic motionKinematic data were collected with the Flock of Birds electromagnetic motion capture system. This system has a root-mean-square position accuracy of 0.07in./0.5° at a 36-in. range with a resolution of 0.03in./0.1°.11 Sensors were affixed to the participants’ sternum, acromion, and humerus on their dominant side using double-sided tape and a thermoplastic humeral cuff. Sensor placement, digitization, and establishment of local and global coordinate systems followed the International Society of Biomechanics recommendations.12 Additionally, the coracoid process and fourth rib were digitized to measure PMm length change during overhead reaching tasks. Bony landmarks for PALM PMm length measures were utilized for digitizing the coracoid process and fourth rib.
Three-dimensional scapulothoracic data were collected at a sampling frequency of 100Hz per sensor. Variables of interest were scapular: internal rotation, upward rotation, and posterior tilt. Reliability of these variables during arm elevation has previously been reported to range from moderate to excellent.13 Participants were asked to perform three arm elevation tasks that were constrained to a plane of motion: flexion, abduction, and scapular plane elevation. Participants were instructed to raise their arm over the span of three seconds and lower over three seconds with their thumb up and elbow extended. Participants were also asked to perform an overhead reach to a shelf which was considered an unconstrained task as participants did not have to raise their arm in a specified plane. The shelf was set to a height above the participant's shoulder equal to 50% of their arm length.7 Participants were instructed to reach up and touch the top of the shelf in their natural manner and then lower their arm back to their side. For each of the four arm elevation tasks participants were asked to perform three repetitions of arm raising and lowering. A 2-min rest was provided between tasks to reduce the risk of fatigue. Elevation tasks were performed in random order. Following data collection, data were processed with the Motion Monitor™ software (Innsport Inc., Chicago, IL).
Data analysisActive and passive PMm elongation were calculated as follows: [(active or passive PMm length−resting PMm length)/resting PMm length]×100. PMm length during shelf reaching and scapular plane elevation tasks was calculated by the Motion Monitor software as the distance between digitized points on the fourth rib and coracoid process. PMm length change was determined as follows: [(PMm length at 90° of humeral elevation (shelf) or 120° of humeral elevation (scapular plane)−resting PMm length)/resting PMm length]×100. Active and passive PMm elongation, and PMm length change during shelf and scapular plane arm elevation tasks were compared between groups with separate independent t-tests. Significance was set to α=0.05. Cohen's d effect sizes were calculated and defined as small=0.20, medium=0.50, and large=0.80.14
Kinematic data were processed using a custom-written MATLAB program (MathWorks, Natick, MA). For each constrained task, scapular internal rotation, upward rotation, and posterior tilt were extracted at four points of humeral elevation (30°, 60°, 90°, and 120°) and averaged across the three repetitions. For the shelf task, scapular rotations were extracted at 30°, 60°, and 90° of humeral elevation. Two-factor mixed-model analyses of variance were conducted (one for each scapular rotation and elevation task) with humeral elevation the within-subjects factor and PMi group the between-subjects factor. Significance was set to α=0.05. Interpretation of effect size (η) was: small=0.10, medium=0.24, large=0.37.14
ResultsFifty-six individuals volunteered to participate in the study and were screened for eligibility in order to identify 30 participants for complete data collection and analysis. Of the 26 individuals who did not complete the study, 3 were excluded for not meeting inclusion criteria (scoliosis, shoulder pain, long resting PMm), and 23 were excluded due to typical PMm length quota being reached (n=21), sickness during testing (n=1), and palpation error (n=1). As expected, groups differed on PMm length and PMi measures but did not differ on any other anthropometric measure (Table 1).
Participant demographics (mean±SD).
| Variable | Typical group (n=15) | Short group (n=15) | p |
|---|---|---|---|
| Sex | 6 males, 9 females | 3 males, 12 females | 0.43a |
| Age (years) | 26±4 | 26±4 | 0.76b |
| Height (m) | 1.70±0.08 | 1.67±0.09 | 0.34b |
| Mass (kg) | 66.2±10.3 | 66.1±10.4 | 0.97b |
| BMI (kg/m2) | 22.8±2.9 | 23.6±2.7 | 0.49b |
| PMm length (cm) | 16.2±1.2 | 13.9±1.2 | <0.01b |
| PMi | 9.5±0.4 | 8.3±0.5 | <0.01b |
BMI, body mass index; PMm, pectoralis minor muscle; PMi, pectoralis minor index.
No differences were found in active (typical [14.0%], short [15.0%], p=0.70) or passive (typical [19.1%], short [19.8%] p=0.79) PMm elongation between groups (Table 2). No group differences were found in PMm percent length change during the shelf reach (typical [10.4%], short [11.0%], p=0.74) or scapular plane elevation (typical [16.0%], short [17.2%] p=0.59) tasks (Table 2).
Pectoralis minor percent muscle length change (mean±SD).
| Condition | Typical group (n=15) | Short group (n=15) | Effect size (d) (95% confidence interval) |
|---|---|---|---|
| Actively lengthened | 14.0±7.3% | 15.0±6.1% | 0.15 (−0.57, 0.87) |
| Passively lengthened | 19.1±6.4% | 19.8±8.0% | 0.10 (−0.62, 0.82) |
| Shelf reach | 10.4±5.7% | 11.0±4.5% | 0.12 (−0.60, 0.84) |
| Scapular plane elevation | 16.0±6.7% | 17.2±5.2% | 0.20 (−0.52, 0.92) |
There were no significant interactions between humeral elevation and group for any scapular rotation across all arm elevation tasks. There were no significant main effects of group for any scapular rotation across all arm elevation tasks. Significant main effects of humeral elevation were observed for most scapular rotations and arm elevation tasks. Findings from these main effects are not reported as they were expected and are not directly related to the study's purposes. Group means, absolute differences, and effect sizes (η) for arm elevation tasks and scapular rotations are provided in Table 3. One participant failed to reach 120° of humeral elevation during arm abduction and was excluded from the abduction analyses.
Comparison of group means and standard deviations (SD) for arm elevation tasks and scapular rotations.
| Arm elevation task and scapular rotation | Humeral elevation angle (°) | Typical group Mean±SD (°) | Short group Mean±SD (°) | Absolute mean difference (°) | Group main effect | Interaction |
|---|---|---|---|---|---|---|
| Flexion (n=30) | ||||||
| Internal rotation | 30 | 34.3±8.7 | 33.3±10.2 | 0.9 | p=0.434 η=0.14 | p=0.295 η=0.20 |
| 60 | 39.3±9.0 | 37.7±10.2 | 1.6 | |||
| 90 | 42.6±9.6 | 39.1±10.9 | 3.5 | |||
| 120 | 40±10.9 | 34.5±16.1 | 5.5 | |||
| Upward rotation | 30 | 5.7±8.5 | 8.0±5.7 | 2.3 | p=0.289 η=0.18 | p=0.718 η=0.08 |
| 60 | 14.9±8.9 | 17.8±6.4 | 2.9 | |||
| 90 | 24.0±10.4 | 28.1±8.2 | 4.1 | |||
| 120 | 33.7±13.0 | 37.5±11.1 | 3.8 | |||
| Posterior tilt | 30 | −4.6±6.8 | −5.6±4.8 | 1.0 | p=0.212 η=0.21 | p=0.388 η=0.17 |
| 60 | −3.7±7.1 | −6.4±6.6 | 2.7 | |||
| 90 | −1.3±5.2 | −4.9±8.7 | 3.5 | |||
| 120 | 6.6±5.3 | 2.0±12.3 | 4.6 | |||
| Scapular plane elevation (n=30) | ||||||
| Internal rotation | 30 | 29.1±9.3 | 27.6±9.4 | 1.5 | p=0.301 η=0.19 | p=0.199 η=0.24 |
| 60 | 31.3±8.9 | 29.1±9.3 | 2.2 | |||
| 90 | 32.9±9.2 | 29.3±9.2 | 3.5 | |||
| 120 | 32.8±11.6 | 25.7±14.3 | 7.1 | |||
| Upward rotation | 30 | 4.1±7.3 | 7.2±6.8 | 3.1 | p=0.173 η=0.23 | p=0.653 η=0.10 |
| 60 | 13.0±8.3 | 17.0±7.0 | 4.0 | |||
| 90 | 21.5±10.3 | 26.9±7.7 | 5.3 | |||
| 120 | 32.5±12.8 | 36.6±11 | 4.1 | |||
| Posterior tilt | 30 | −4.3±5.9 | −4.8±5.4 | 0.5 | p=0.480 η=0.12 | p=0.494 η=0.14 |
| 60 | −2.9±6.4 | −4.0±6.4 | 1.1 | |||
| 90 | 0.0±5.8 | −2.4±8.7 | 2.4 | |||
| 120 | 6.3±4.3 | 3.5±12.7 | 2.9 | |||
| Abduction (n=29) | ||||||
| Internal rotation | 30 | 19.0±7.5 | 19.1±10.7 | 0.1 | p=0.414 η=0.15 | p=0.237 η=0.23 |
| 60 | 17.5±7.5 | 15.8±10.2 | 1.7 | |||
| 90 | 18.8±8.8 | 14.7±10.1 | 4.1 | |||
| 120 | 22.9±13.0 | 17.4±12.8 | 5.5 | |||
| Upward rotation | 30 | 2.4±8.5 | 6.4±6.6 | 3.9 | p=0.127 η=0.27 | p=0.523 η=0.13 |
| 60 | 12.5±9.2 | 18.0±8.2 | 5.5 | |||
| 90 | 22.3±11.0 | 29.2±9.4 | 6.9 | |||
| 120 | 33.8±13.4 | 38.8±12 | 5.1 | |||
| Posterior tilt | 30 | −3.7±5.8 | −4.9±6.2 | 1.3 | p=0.413 η=0.13 | p=0.675 η=0.11 |
| 60 | −0.5±5.5 | −2.2±7.5 | 1.7 | |||
| 90 | 4.0±5.8 | 1.2±9.1 | 2.8 | |||
| 120 | 8.0±5.1 | 5.3±11.8 | 2.7 | |||
| Shelf (n=30) | ||||||
| Internal rotation | 30 | 27.5±8.7 | 24.6±10.4 | 3.0 | p=0.204 η=0.23 | p=0.131 η=0.28 |
| 60 | 32.8±9.5 | 28.5±10.0 | 4.3 | |||
| 90 | 39.6±10.3 | 33.2±10.2 | 6.3 | |||
| Upward rotation | 30 | 8.0±7.8 | 11.6±4.9 | 3.6 | p=0.091 η=0.30 | p=0.283 η=0.20 |
| 60 | 17.4±7.9 | 21.1±5.5 | 3.7 | |||
| 90 | 24.5±9.1 | 30.3±7.4 | 5.8 | |||
| Posterior tilt | 30 | −4.1±5.6 | −5.1±5.8 | 1.0 | p=0.091 η=0.19 | p=0.129 η=0.28 |
| 60 | −2.3±5.7 | −4.4±6.7 | 2.1 | |||
| 90 | 0.8±4.2 | −3.2±8.2 | 3.9 | |||
The purposes of this study were to determine whether PMm elongation during active or passive movements and scapulothoracic motion differed between participants with short versus typical resting PMm lengths. Contrary to our hypotheses, our findings revealed no group differences in PMm elongation during active or passive PMm lengthening maneuvers, or during overhead reaching tasks. Furthermore, our study failed to find group differences in scapulothoracic motion during a series of arm elevation tasks. Although we powered our study to detect a moderate effect size in scapulothoracic motion, only 2/12 (16.6%) of our kinematic results for the main effect of PMi group had a moderate effect. The remaining results (10/12 [83.3%]) had a small to moderate effect.
It has been suggested that decreased resting PMm length indicates a tight, or shortened PMm.4,15 However, until now, no study has investigated whether resting PMm length was related to the magnitude of PMm elongation during active or passive movements. Although participants in our short and typical PMm length groups had different resting PMm lengths, the amount to which the PMm could be actively or passively lengthened with respect to resting length was not different between groups. Based on this finding it can be argued that utilizing resting PMm length alone to determine whether a stretching intervention is warranted is inappropriate. This may in part explain why a recent study by Rosa et al.15 failed to find resting PMm length changes following a stretching program in individuals with short resting PMm length. It is possible that the PMm's in these individuals were not tight or shortened and therefore did not respond to the stretching program.
Based on a musculoskeletal model, it has been suggested that the PMm lengthens by 67% when the arm is raised from the side to full elevation.16 Our study revealed smaller muscle length changes, with no difference in the amount of length change between the short (17%) and typical (16%) groups during scapular plane elevation. These smaller length changes may partially be explained by the fact that our muscle length change was based on 120° of arm elevation for scapular plane elevation and 90° for the shelf task whereas the change computed by the model was based upon full arm elevation. We based our analysis on 120° and 90° of arm elevation as that was the elevation angle achieved by all study participants during the scapular plane elevation and shelf reach tasks.
To the best of our knowledge this is the first study to report information about PMm elongation using techniques that have been shown to be reliable and clinically applicable.9,17 Additionally, these PMm elongation measures have been shown to be sensitive enough to detect differences in PMm length in individuals with spinal cord injury and varied duration of manual wheelchair use.18 Based on this information, we propose that measures of PMm elongation should be used for clinical decision-making when it comes to determining if stretching is indicated for a tight or shortened PMm. Future research is needed to determine PMm elongation cut points for identifying individuals with a tight or shortened PMm.
Across all arm elevation tasks, scapulothoracic motion did not differ between participants in the short and typical resting PMm length groups. This finding is in contrast to the findings of Borstad and Ludewig,4 who reported increased scapular anterior tilt and scapular internal rotation in participants with short compared to those with long resting PMm lengths. The difference in study findings is most likely explained by the groups recruited for each study. While both studies included a short resting PMm length group, Borstad and Ludewig4 included a long PMm length group and the current study a typical PMm length group. It may be that kinematic differences do not become apparent unless groups at the ends of the resting PMm length spectrum are compared, or higher degrees of arm elevation need to be studied to find potentially significant scapulothoracic motion difference between individuals with short and typical resting PMm lengths. Our rationale for including a typical PMm length group was twofold. First, we wanted to build upon the work of Borstad and Ludewig.4 Second, we wanted to provide comparative information that is more in line with how clinicians compare patient specific muscle length or movement pattern information to typical values of muscle length or movements.
Another factor to consider when comparing findings from our and Borstad and Ludewig's4 studies is the criteria used for determining cut points for PMm groups. While both studies used±one standard deviation from the mean of a group of healthy individuals’ PMm length, the sample size upon which these values were calculated differed. In Borstad and Ludewig's4 study, six healthy individuals were used to derive cut points for defining short (PMi<7.65) and long (PMi>8.61) groups. In the current study data from a previous study9 on 34 healthy individuals were used to derive cut points for defining the short (PMi<8.9) and typical (8.9≤PMi<10.5) groups. The mean PMi value from this previous work9 is in line with that reported by Struyf et al.19 and Rosa et al.15 but greater than that reported by Borstad and Ludewig4 (Table 4). Assuming that researchers accurately palpated the coracoid process and fourth rib, we believe the strength of the relationship between height and PMm length could be a possible reason for mean PMi variability across studies. Using data from this and our previous study9 (n=64) we found a stronger correlation between PMm length and clavicular length (r=0.72) than PMm length and height (r=0.61). Perhaps using clavicular length as a variable for calculating PMi should be considered in future studies.
Comparison of pectoralis minor muscle length and index across studies.
| Author | Sample size | Mean age±SD (yrs) | Height±SD (cm) | Mean resting PMm length±SD (cm) | Resting PMi±SD |
|---|---|---|---|---|---|
| Ebaugh et al. (current study) | 54 healthy | 26±6 | 170±8.5 | 15.3±1.7 | 9.0±0.8 |
| 15 healthy w/ “short” PMm | 26±4 | 167±9.0 | 13.9±0.2 | 8.3±0.5 | |
| 15 healthy w/ “typical” PMm | 26±4 | 170±8.0 | 16.2±1.2 | 9.5±0.4 | |
| Finley and Ebaugh18 | 23 w/ SCI | 41.7±4.6 | 177.5±8.6 | 16.5±2.0 (dominant) | 9.4±1.1 |
| 17.2±2.2 (non-dominant) | 9.8±1.2 | ||||
| Finley et al.9 | 34 healthy | 23.9±1.6 | 169±8.9 | 16.3±1.6 (dominant) | 9.7±0.7 |
| 16.4±1.6 (non-dominant) | 9.7±0.8 | ||||
| Rosa et al.15 | 25 symptomatic w/ “short” PMm | 25.8±7.0 | 169±8.0 | 16.4±1.6 | 9.7a |
| 25 asymptomatic w/ “short” PMm | 27.0±5.8 | 169±7.0 | 16.0±1.3 | 9.5a | |
| Struyf et al.19 | 25 healthy | 20.8±1.5 | 175.7±9.8 | 16.2a | 9.2±0.6 |
| 25 w/ shoulder pain | 50.8±16.3 | 169.0±9.9 | 16.3a | 9.7±0.7 | |
| Borstad20 | 26 healthy | Not reported | Not reported | 15.6±0.3 | Not reported |
| Borstad and Ludewig4 | 6 healthy (pilot) | Not reported | 174.1a | 14.1±0.8 (SE) | 8.1±0.5 (SE) |
| 25 healthy w/ “long” PMm | 28.6±1.3 (SE) | 172.6±1.7 (SE) | 15.8±0.3 (SE) | 9.1±0.1 (SE) | |
| 25 healthy w/ “short” PMm | 25.8±0.9 (SE) | 168.3±1.4 (SE) | 12.5±0.2 (SE) | 7.4±0.1 (SE) |
SD, standard deviation; SE, standard error; yrs, years; SCI, spinal cord injury; PMm, pectoralis minor muscle; PMi, pectoralis minor index [(PMm length/height)×100)].
If we were to apply Borstad and Ludewig's4 short group cut point (PMi<7.65) to our participants with a short PMm, only two of our 15 participants would have met their criteria. Nine of our short group participants would have been excluded from their study for falling within one standard deviation of the mean, and the remaining four would have been included in their long group (PMi>8.61). All of the participants in our typical group would have been placed into their long group. In an effort to directly compare our findings with Borstad and Ludewig's,4 we performed a descriptive subanalysis of scapulothoracic motion for two participants in our study with PMi's below Borstad and Ludewig's4 short cut point. We compared these participants with participants matched on age, sex, and BMI from our typical group (who would have been classified into Borstad and Ludewig's long group). Like Borstad and Ludewig's short group, the two participants with short PMi's had reduced scapular posterior tilt during flexion, abduction, and scapular plane elevation compared to the matched counterparts. However, we did not find an increase in scapular internal rotation. This subanalysis suggests that individuals with a very short resting PMm length may exhibit different patterns of scapulothoracic motion than individuals with a typical resting PMm length.
As with any study there are a few limitations that should be considered. The amount of force applied to the PMm was not measured during active and passive lengthening procedures. Consequently, similar levels of force may not have been applied to all participants. However, during the active lengthening procedure all participants received similar levels of verbal encouragement to elevate and retract their scapulae as much as they could. The therapists who performed the passive lengthening procedure underwent training prior to data collection to ensure each felt comfortable with the measurement procedure. This session consisted of reviewing the previously established measurement procedures9 and practicing on three individuals. The reliability of the PMm length change measure derived from the Motion Monitor is unknown. Skin markings used for measuring resting, actively, and passively lengthened PMm length were used to track muscle length change during the overhead tasks, and the distance between these landmarks was tracked with, and calculated by, the sternal and scapular sensors and Motion Monitor software. While reliability of this measure should be determined, it is reasonable to speculate that acceptable reliability would be found given that acceptable levels of reliability have been reported for using these landmarks and skin mounted sensors for measuring PMm length9 and scapular rotations,13 respectively. Another limitation related to our PMm length change measure is that we did not determine muscle length change above 120° of humeral elevation. Knowing that measures of scapulothoracic motion have higher amounts of error associated with them above 120°,17 we elected to limit our muscle length changes to 120°. Finally, like similar studies, we studied a healthy young population. Findings from this study should not be extrapolated to an older population or individuals with shoulder pain.
ConclusionsActive and passive PMm elongation as well as PMm length change during overhead arm motions did not differ between individuals with short and typical resting PMm length. Additionally, scapulothoracic motion during four different arm elevation tasks did not differ between individuals with short and typical resting PMm lengths. Further research is needed to provide a better understanding of what constitutes a tight or shortened PMm, the role that a tight or shortened muscle has on scapulothoracic motion, and how this information can be used for clinical decision-making.
FundingI affirm that I have no financial affiliation (including research funding) or any conflict of interest with any commercial organization that has a direct financial interest in any matter included in this manuscript, except as disclosed in an attachment and cited in the manuscript.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interestThe authors declare no conflicts of interest.
The authors would like to acknowledge Joseph Sarver, PhD, for lending his expertise with development of the data processing software program.
This study was approved by Institutional Review Board at Drexel University.