Stroke may lead to several health problems, but positive effects can be promoted by learning to perform physical therapy techniques correctly.
ObjectiveTo compare two different types of observational practice (video instructions and demonstration by a physical therapist) during the use of incentive spirometry (IS).
MethodA total of 20 patients with diagnosis of stroke and 20 healthy individuals (56±9.7 years) were allocated into two groups: one with observational practice with video instructions for the use of IS and the other with observational practice with demonstration by a physical therapist. Ten attempts for the correct use of IS were carried out and the number of errors and the magnitude of response were evaluated. The statistic used to compare the results was the three-way ANOVA test.
ResultsThe stroke subjects showed less precision when compared to the healthy individuals (mean difference 1.80±0.38) 95%CI [1.02–2.52], p<0.0001. When the type of practice was analyzed, the stroke subjects showed more errors with the video instructions (mean difference 1.5±0.5, 95%CI [0.43–2.56] (p=0.08)) and therapist demonstration (mean difference 2.40±0.52, 95%CI [1.29–3.50] (p=0.00)) when compared to the healthy individuals.
ConclusionThe stroke subjects had a worse performance in learning the use of volume-oriented incentive spirometry when compared to healthy individuals; however, there was no difference between the types of observational practice, suggesting that both may be used to encourage the use of learning IS in patients with stroke.
Stroke is a neurological disorder characterized by a focal disturbance of cerebral function due to the interruption of normal blood flow that usually leads to persistent dysfunction depending on the structures that have been affected.1 The primary focus of the rehabilitation of these patients is based on motor learning. This learning process corresponds to the acquisition of new movement patterns and consequent retention of relevant information regarding the tasks to be performed.2
Stroke impairments may contribute to learning and attention deficits. Attention is essential for retaining information for subsequent interpretation and possible storage in long-term memory. On the other hand, its absence may impair learning directly.3 The organization and feedback during practice are variables that significantly influence the treatment plan strategies in the rehabilitation of neurological patients.4
According to Schmidt,2 the relearning of an activity can be determined by the physical therapist's direct instruction, a common practice in physical therapy. The therapist can demonstrate the goal of the movement or technique to be performed by the patient.5
According to the social learning theory of Bandura,6 the relearning of an action can be enhanced through observational learning. One example is that the physical therapist can be replaced by video, film, or photographs of the task to be performed by the patient.
Observational practice is processed when an observer reproduces the actions demonstrated by a model, so a new action is incorporated into his repertoire.5–7 Tasks with virtual elements provide an additional advantage since they increase the number of repetitions and the time of practice.8
The evaluation of the performance of a task can demonstrate the influence of teaching strategies on learning. This evaluation takes into account three factors: (1) precision, i.e., the number of errors when trying to perform the task; (2) speed; and (3) magnitude of response, i.e., the number of attempts until reaching a consistent response.4–9 Respiratory therapy has several techniques that rely on learning for greater effectiveness. One of these techniques is incentive spirometry (IS), which promotes lung expansion, reduction of regional differences in ventilation and perfusion, alveolar recruitment, and improved pulmonary ventilation.10,11 This technique is widely used in clinical practice for diseases that restrict chest wall movement, reducing expansion. In stroke patients, pulmonary ventilation is often compromised due to the loss of respiratory muscle contraction efficiency, either by hemiparesis or hemiplegia.
The aim of this study was to gain a better understanding of motor learning in patients after stroke by comparing the effects of two different types of observational practice (video instructions vs. demonstration by a physical therapist) during the use of IS.
MethodParticipantsThe study sample consisted of 40 participants of both genders. Of those, 20 were hemiparetic individuals with a clinical diagnosis of stroke determined by computed tomography, age between 39 and 74 years, time since stroke of 1–7 years, and preserved cognitive ability according to the Mini-Mental State Examination (score of at least 20 points for illiterate, 25 for 1–4 years of schooling, 26.5 for 5–8 years, 28 for 9–11 years, and ≥29 for more than 11 years of education). The other 20 participants were healthy individuals with preserved cognitive ability and without cardiac, respiratory, or neurological disease, matched to the other group for age, gender, and body mass index (BMI). All participants who presented fatigue and/or dyspnea during the learning test were excluded.
The study was approved by the Research Ethics Committee of Universidade Federal do Rio Grande do Norte (UFRN), Natal, RN, Brazil (protocol number 095/11) and conducted in accordance with Resolution 466/12 of the National Health Council. All participants agreed to take part in the study by signing an informed consent form (ICF).
Non-probability sampling was used to select the participants, and randomization to the type of observational practice was performed by drawing lots. The sample size was calculated according to data collected from 10 volunteers breathing at rest and during the IS. The effect size was calculated by standard deviation of the volunteers’ tidal volume. Considering a significance level of 0.05 and a statistical power of 0.80, the ideal sample was estimated to be 20 subjects for the experimental group.
The mean quantity of errors and attempts was considered to calculate the effect size. A Cohen f of 1.06 was found, considering an α error probability of less than 0.01 (p<0.01) with 0.95 power. Based on the previous findings, the study effect is considered large.
ProceduresFirst, the participants of the experimental group were evaluated for cognitive function using the Mini-Mental State Examination (MMSE).12,13 After that, their neurological impairment level was assessed using the National Institute of Health Stroke Scale (NIHSS).14 Finally, post-stroke motor function was evaluated with the Functional Independence Measure (FIM).15,16 The control group was evaluated as well.
To determine the effect size of the sample, tidal volume during quiet breathing was assessed with optoelectronic plethysmography, used to calculate the changes in tidal volume of chest wall during 90s before the protocol with the IS.17 After that, the participants performed a spirometric assessment to determine individual inspiratory capacity. For this procedure, a spirometer (KoKoDigiDoser, nSpire Health, Longmont, CO, USA) was used according to the acceptability and reproducibility criteria of the Brazilian Society of Pneumology and Pathophysiology.18
The volume-oriented IS was performed by all participants on a Voldyne® 5000 device (Sherwood Medical, St. Louis, MO, USA). The technique consisted of slow deep inspiration, followed by a post-inspiratory pause. The pause was performed at the predetermined volume of 80% of the individual inspiratory capacity shown on the device and sustained for 3s, followed by slow expiration. The inspiratory pause was timed by a physical therapist with a chronometer until the participant reached the predetermined volume. The vital signs assessed were respiratory rate (RR), heart rate (HR), and blood oxygen saturation (%SpO2) with a pulse oximeter (Nonin 2500, PalmSAT, USA).
After the initial assessment, the sample was randomly divided into two groups: one with observational practice with video instructions (VG) for the use of IS and the other with observational practice with demonstration by a physical therapist (TG). The VG watched a four-minute video with visual and audio instructions on the use of IS. It included a physical therapist supervising the action and giving verbal commands to a patient who performed ten repetitions of the exercise with the spirometer. The TG received instructions directly from the physical therapist, including the same information about the technique and the same verbal commands, but without seeing the patient performing the exercise.
To evaluate the effects of the types of observational practice, the accuracy and magnitude of response were registered. Accuracy corresponded to the number of errors during the attempts, and magnitude of response referred to the number of attempts to obtain a response considered consistent. In this case, response was considered consistent or correct when the individual performed the task satisfactorily (i.e., the patient reached the pre-determined breathing lung volume as shown on the device, sustained the post-inspiratory pause of 3s, exhaled air slowly, kept the device upright, and performed the technique in the correct posture2,10,19).
Statistical analysisData analysis was performed using Statistica Software version 7.0. The normality of data distribution was verified by the Kolmogorov–Smirnov test. For descriptive analysis, the mean was used as a measure of central tendency and the standard deviation as a measure of dispersion. For the inferential analysis, we used the three-way repeated measures ANOVA to compare the number of errors, types of practice, and the number of attempts in the patients with stroke and the healthy participants. The effect size was calculated using the Software G*Power (G*Power 3.1.9.2, Kiel, Germany).
When significant differences were found, the post hoc Newman–Keuls test was used. For all statistical analyses, we adopted a significance level of 5% (p<0.05).
ResultsSample characterizationThe analysis of the anthropometric variables showed sample homogeneity, with no significant differences between the subjects with stroke and the healthy individuals. The subjects with stroke had significantly higher RR values and lower %SpO2 values, when compared to the healthy individuals, as shown in Table 1.
Anthropometric characteristics and vital signs of subjects with stroke and healthy individuals.
| Variables | Stroke subjects | Healthy individuals | p |
|---|---|---|---|
| n=20 (15M; 5F) | n=20 (15M; 5F) | ||
| Age (years) | 56±9.7 | 56.5±10.3 | 0.97 |
| Weight (Kg) | 70.5±12.6 | 74±9.8 | 0.95 |
| Height (cm) | 165±6.1 | 168.5±6.6 | 0.17 |
| BMI (kg/m2) | 25.7±3.8 | 25.6±2.8 | 0.53 |
| SBP (mmHg) | 130±15 | 120±12.8 | 0.37 |
| DBP (mmHg) | 80±11 | 80±10.3 | 0.42 |
| HR (bpm) | 76±11.3 | 74±11.3 | 0.78 |
| RR (rpm) | 18.1±1.3 | 17±1.6 | 0.01* |
| SpO2 (%) | 97±1.1 | 98±0.7 | 0.00* |
Values are mean±standard deviation; M, male; F, female; BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; HR, heart rate; RR, respiratory rate; SpO2, blood oxygen saturation. Unpaired t-test.
Data regarding the side of hemiparesis, time of brain injury, years of study, level of neurological impairment (NHISS), functional ability (FIM), and cognitive evaluation (MMSE) of the subjects with stroke are presented in Table 2. The results showed a similar frequency in side of hemiparesis and an average time since stroke of 3.65 years. The number of years of study was lower for the stroke subjects and they also had a mild neurological impairment according to the NHISS. The average functional ability score as assessed by the FIM was 86 points, indicating functional independence for the stroke subjects. These subjects had significantly lower values in the cognitive assessment when compared to the healthy individuals.
Sample characterization regarding side hemiparesis, time of injury, degree of neurological impairment, functional independence measure, and cognitive assessment.
| Sample | Stroke subjects | Healthy individuals | p |
|---|---|---|---|
| n=20 (15M; 5F) | n=20 (15M; 5F) | ||
| Hemiparesis | |||
| Right | 9 (45%) | – | – |
| Left | 11 (55%) | – | – |
| Time of injury | 3.65±3.2 | – | – |
| Years of study (years) | 8.67±5 | 11.8±3.7 | 0.03* |
| NIHSS (n=20) | 4±2.3 | – | – |
| FIM (n=20) | 86±7.9 | – | – |
| MMSE (score) | 28±1.2 | 30±1.1 | 0.00* |
Values are means±standard deviation; M, male; F, female; NIHSS, National Institute Health Stroke Scale; FIM, Functional Independence Measure scale; MMSE, Mini-Mental State Examination. Unpaired t-test.
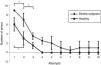
When comparing the precision data, the stroke group made more errors (2.9±1.3 errors) when compared to the healthy individuals (1.1±0.9 errors) 95%CI [1.02–2.52], p<0.0001. There was no significant difference in the number of errors between stroke subjects and the healthy individuals in any of the attempts (p>0.05). However, for stroke subjects, there was a significant difference between the errors of the first and second attempts (p=0.00) and between the second and third attempts (p=0.01). In contrast, the healthy individuals showed a significant difference only between the first and second attempts (p=0.02), as shown in Fig. 1.
When evaluating the performance of participants according to the type of practice (video vs. therapist), there was no significant difference between the number of errors of the stroke group (p=0.20) and the healthy individuals (p=0.36), as shown in Fig. 2.
However, when analyzing each type of practice separately, there was a significant difference in the number of errors between the stroke subjects and healthy individuals in both the practice with the video (mean difference 1.5±0.5, 95%CI [0.43–2.56] (p=0.08) and the practice with the therapist (mean difference 2.40±0.52, 95%CI [1.29–3.50] (p=0.00), indicating more errors for the stroke group in both types of practice (3.3±0.4 vs. 2.6±0.4 errors for therapist and video, respectively).
Regarding the magnitude of response, there was a significant difference between the stroke subjects and healthy individuals for both types of observational practice (mean difference 1.10±0.35, 95%CI [0.38–1.81], p=0.03). Stroke subjects made more errors before the consistent response and in the practice with the video (2.0±0.2, p=0.00), as shown in Fig. 3.
DiscussionThis is an innovative study about observational practice of the use of volume-oriented IS. The results showed that both stroke subjects and healthy individuals improved their performance with each attempt; however, after the fourth attempt, the healthy individuals made no mistakes, unlike the stroke subjects who continued making errors until the tenth attempt. This result may indicate a delayed stabilization of performance in the stroke subjects. This finding may result from a worse cognitive-motor interaction. With practice or during the attempts, the individual has the opportunity to test alternatives in search for solutions to a particular task performance.20
Analyzing the performance in all attempts, we found that the stroke subjects made more errors than the healthy individuals. Furthermore, they needed more attempts to reach the correct or consistent response. No observational practice was found to be superior to the other. These results clearly show that a worse performance is related to neurological deficits resulting from stroke.21
Regarding the type of observational practice, there was no significant difference between the video instructions and the therapist's demonstration as observed in the similar performance for both stroke subjects and healthy individuals. This result suggests that both practices may be used to optimize the use of IS in patients with chronic stroke sequelae.
The inclusion of observational practice with video demonstration in the pulmonary rehabilitation of stroke patients may be important. The literature suggests that learning by watching another patient model a technique can assist the process of learning new tasks. In this process, the individual must distinguish similarities and differences between their actions and the demonstration. Several studies indicate that observational practice helps the neurological patient to better develop spatial and temporal characteristics of the actions, optimizing motor learning.22–24 Thus, the therapist needs to determine what aspects of the observed or learned action are relevant so the patient can perform the task properly and successfully.
Públio et al.25 found that verbal instructions can act as mediators in improving the cognitive representation of the observational model, directing the individual's attention to key aspects of the demonstration. The authors also concluded that visual representation is essential for individuals whose verbal skills about the movements are not sufficiently developed for the spatial and temporal aspects. However, the study by Sidaway et al.26 clearly illustrated that too much guidance during the practice of motor skills may have potentially deleterious effects. The availability of constant feedback can suppress the development of the process of detecting and correcting errors. The ability to detect performance errors and modify the motor action is fundamental to accurate performance.26,27
Recent studies have shown that stroke not only limits the motor sensory and intellectual areas, but also impairs lung function in several ways including changes in central respiratory rhythm, interruption of the impulses from the respiratory centers,28 and decreases in motor function and functional movement of the diaphragm in the affected hemithorax to lead to changes in respiratory muscle strength.29,30 The oxygen saturation assessed in the present study was significantly reduced in the stroke group compared to the healthy group, but this reduction had no clinical relevance. Nevertheless, it is important to evaluate this variable to avoid changes in oxygenation. Furthermore, following the correct recommendations for the use of IS may prevent fatigue.31 The limitations of this study are related to the inability to correlate the learning process with the affected location and side of the brain, as well as the extension of brain injury.
ConclusionIn conclusion, the subjects with stroke performed differently to the healthy individuals while learning to use volume-oriented spirometry. The stroke subjects made more errors and required more attempts to perform the proposed task correctly. However, there was no significant difference between the types of observational practice, suggesting that both video instructions and therapist demonstrations may be used to encourage patients with stroke to learn to use incentive spirometry.
Conflicts of interestThe authors declare no conflicts of interest.