Low back pain is a highly prevalent and disabling musculoskeletal disorder. Physical activity is widely used as a prevention strategy for numerous musculoskeletal disorders; however, there is still conflicting evidence as to whether physical activity is a protective or risk factor for low back pain or whether activity levels differ between people with and without low back pain.
ObjectiveTo investigate the association between low back pain and different types (occupational and leisure) and intensities (moderate and vigorous) of physical activity.
MethodsThis is cross-sectional observational study. We included in this study a total of 1059 individuals recruited from a Spanish twin registry with data available on low back pain. Outcome: Self-reported leisure and occupational physical activity were the explanatory variables. The low back pain outcome used in this study was recurrent low back pain.
ResultsOur results indicate that leisure physical activity is associated with a lower prevalence of recurrent low back pain. In contrast, occupational physical activity, such as carrying, lifting heavy weight while inclined, awkward postures (e.g. bending, twisting, squatting, and kneeling) are associated with a higher prevalence of recurrent low back pain. There was no statistically significant association between other occupational physical activities, such as sitting or standing, and low back pain.
ConclusionLeisure and occupational physical activity are likely to have an opposed impact on low back pain. While leisure physical activity appears to be protective, occupational physical activity appears to be harmful to low back pain. Future longitudinal studies should assist in formulating guidelines addressing specific types and intensity of physical activity aimed at effectively preventing low back pain.
Low back pain (LBP) is the musculoskeletal disorder responsible for the greatest level of disability worldwide,1,2 with 84% of individuals expected to experience LBP during their lifetime.3 The point-prevalence of chronic LBP is approximately 23%, and about 12% of people will experience activity limitations because of their LBP.4,5 In addition to these impressive figures, the impact of LBP continues to grow.6 According to the latest global burden of disease report, the burden of LBP has increased by 60% between 1990 and 2015 (assessed using disability-adjusted life years).7 It is believed that this growth is partially due to the widespread effect of poor lifestyle choices, including sedentary behavior.8–10
The benefits of physical activity on an individual's social, psychological, and biological health are substantial.11,12 Engagement in regular moderate-intensity physical activity can reduce the risk of morbidity and all-cause mortality,13–17 while physical activity is widely used as a prevention strategy for chronic diseases such as diabetes, osteoporosis, cardiovascular disease, depression, and numerous musculoskeletal disorders, including LBP.18,19 Physical activity has been widely recommended in clinical guidelines for LBP.20 However, the guidelines are silent in regards to which types and intensities of physical activity.21
Despite increasing research investigating the relationship between physical activity and LBP, there is still conflicting evidence as to whether physical activity is a protective or a risk factor for LBP.22 Issues related to the direction of the relationship and strength of association remains unclear.23 For instance, systematic reviews have found contradictory evidence for the association between LBP and leisure physical activity and sports participation.23,24 However, exposure to high occupational workloads and frequent lifting activities appear to be strongly associated with LBP.23 A potential limitation of previous studies is that physical activity is assessed as the sum of all leisure or occupational activities, making it difficult to identify the intensity and type of physical activity that impacts on LBP. The discrepancy in the literature is likely attributed to the different definitions of levels of physical activity.23,25
To our knowledge, no single study has investigated the association between different types (occupational or leisure) and intensities (moderate or vigorous) of physical activity and LBP. The aim of this study is to investigate the association between LBP and different types and intensity of occupational (e.g. twisting, bending, lifting weight), and leisure (walking, moderate, and vigorous-intensity) physical activity.
MethodsDesign, study sample and data collectionA cross-sectional observational design was used. The sample for this study comprised monozygotic (MZ) and dizygotic (DZ) twins registered in the Murcia Twin Registry (MTR), a population-based twin registry of adult multiples born between 1940 and 1966 in the region of Murcia, Spain. The MTR is a joint effort between the University of Murcia and the Regional Health Authority and currently has over 2300 participants. In brief, participants were recruited through the public health system, which keeps up-to-date records of all the residents in the area. People who were born on the same date and had the same family name were contacted and invited to participate in the MTR provided both twins in a pair were alive at the time of enrolment, and neither had any disorder or disability which would limit their voluntary and conscious participation.26
Twin samples are classically used to disentangle the relative effect of genetics and environment on complex phenotypes, but that is not their only utility. A cohort of twins is a great opportunity for epidemiological research as twins can be treated as a regular cohort of individuals; especially when population-based and representative of the general population.27 The MTR sample has shown to adequately represent the reference population in its geographical area.28 Consequently, since the objective of this study was not the determination of the relative effects of genetic and environmental factors on the relationship between LBP and physical activity, data on twin zygosity and subsequent analyses are not provided.
For this cross-sectional study, data were collected in 2013 including demographics, anthropometric data, a basic health history, and self-reported health-related questionnaires, using phone and face-to-face interviews. All registry and data collection procedures involved in the development of the MTR were approved by the University of Murcia ethics committee, Murcia, Spain. All participants included in the MTR were requested to sign an informed consent form. All data collection was conducted by trained assessors who were blinded to the outcomes of the study.
Assessment of LBPLBP was comprehensively assessed in 2013 from questions derived from standardized definitions aimed to facilitate uniformity across epidemiological studies.29 The LBP outcome used in this study was recurrent LBP. We selected the cases with a more recent presentation of LBP to more efficiently synchronize the assessment of LBP with participants’ report of physical activity engagement in the past week. Initially, the presence of lifetime chronic LBP was assessed by the following question: (i) “Have you ever suffered from chronic LBP?” Chronic LBP was described as pain in the lower back lasting for six months or longer, including seasonal and recurrent episodes. Participants responding ‘yes’ were asked a follow-up question: (ii) When was the last time you experienced LBP?” This question was followed by (iii) “How long has it been since you have had a whole month pain free?” Participants indicating they have suffered from chronic LBP (i), experienced LBP ‘within the past 4 weeks’ (ii), and have had a pain free month within the last ‘3 months’ (iii), were considered to have a history of chronic LBP, experiencing current symptoms consistent with a new recurrent episode.
Assessment of leisure physical activityLeisure physical activity was assessed with questions adapted from the Active Australia Survey,30 which has been proved to be valid and reliable for accessing physical activity in large-scale population-based studies.31–34 First, participants were asked about their engagement in walking during the past week. The variable walking was created based on the participant's response to the following questions: (i) “In the last week, how many times have you walked continuously, for at least 10min for recreation, exercise, or to get to or from places?”; (ii) “What do you estimate was the total time that you spent walking in this way in the last week?”
Second, participants were asked about their engagement in vigorous-intensity physical activity. The variable vigorous physical activity was determined by participants’ response to the following questions: (i) “In the last week, how many times did you do any vigorous physical activity for at least 10min which made you breathe harder or puff and pant? (e.g. jogging, cycling, aerobics, competitive tennis)”, (ii) “What do you estimate was the total time that you spent doing this vigorous physical activity in the last week?”
Finally, participants were asked about their engagement in moderate-intensity physical activity:
(i) “In the last week, how many times did you do any other more moderate physical activities for at least 10min that you have not already mentioned? (e.g. gentle swimming, social tennis, golf)”; (ii) “What do you estimate was the total time that you spent doing these activities in the last week?”
Since it is likely walking is a common form of exercise in the Spanish population, we included walking as a type of moderate-intensity physical activity despite being unable to assess intensity.
We also created a total physical activity category combining the total time spent in vigorous-intensity physical activity, plus moderate-intensity physical activity and walking, in the last week, considering that many people may not engage in only one type of physical activity but a combination of different types. We used as variables, the total time in minutes of each category: moderate (including walking), vigorous, and total physical activity.
Assessment of occupational physical activityA detailed assessment of occupational physical activity was performed with questions adapted from the Hollmann questionnaire,35 which is a reliable and valid instrument for assessing physical workload. Participants were asked how often they work in a specific position on their current job (e.g. trunk upright, trunk twisted, squatting, etc.) and whether they lift or carry light or heavy weight while working (Appendix 1). We used the data from 17 different work postures, with some variables being created through the combination of different postures.
Assessment of co-variablesWe performed univariate logistic regression to explore potential confounders that should be adjusted for in the multivariate models. Investigation of potential confounders such as age, gender, Body Mass Index (BMI), sleep quality, and symptoms of depression or anxiety was based on previous studies in the field.36,37 If the univariate association between co-variables, the outcome and the predictor, reached a significance of <0.2, these variables were adjusted for in the multivariate logistic regression models.
Data analysisData analysis was performed using STATA statistical software (version 13.0, STATA Corp., College Station, TX). We conducted descriptive analyses for all study variables to summarize the data. Our outcome variable was recurrent LBP. Our explanatory variables were leisure physical activity and occupational physical activity. We conducted an unadjusted univariate total sample analysis to explore the association between LBP and the different types of physical activity. In addition, we performed multivariate analysis including the pre-selected confounders as described above. We set the α level for all the final regression models at <0.05. Odds ratios (OR) with 95% confidence intervals (CIs) were calculated.
ResultsSample characteristicsThere were 1059 twins (384 MZ, 675 DZ) with data available on LBP from the 2013 data collection wave. The mean age [standard deviation (SD)] of participants in the total sample was 56.7 (7.1), and 884 (55%) were females. Of those that responded the follow-up wave, only 4% reported recurrent LBP. Further details regarding sample characteristics can be found in Table 1.
Characteristics of participants at baseline divided by subgroups according to low back pain status.
| Variables | Recent LBP | |||
|---|---|---|---|---|
| Yes | No | |||
| n | Mean (SD) or % | n | Mean (SD) or % | |
| Age (years) | 43 | 53.7 (7.3) | 1016 | 53.4 (7.2) |
| Gender (male) | 43 | 23.2 | 1016 | 46.8 |
| Zigosity (MZ) | 15 | 3.9 | 369 | 96.0 |
| Moderate PA | 43 | 46.5 | 1009 | 68.9 |
| Vigorous PA | 43 | 2.3 | 1000 | 21.0 |
| Always upright | 14 | 92.8 | 352 | 92.0 |
| Any inclination | 14 | 71.4 | 354 | 54.8 |
| Any awkward posture | 14 | 50.0 | 362 | 22.6 |
| No load | 14 | 92.8 | 362 | 97.5 |
| Straight upright | 14 | 64.2 | 374 | 49.1 |
| Slightly inclined | 14 | 64.2 | 377 | 48.5 |
| Strongly inclined | 14 | 14.2 | 369 | 15.7 |
| Twisted | 14 | 21.4 | 366 | 15.2 |
| Sitting | 14 | 14.2 | 373 | 39.9 |
| Standing | 14 | 14.2 | 317 | 26.5 |
| Squatting | 13 | 7.6 | 233 | 3.4 |
| Kneeling | 13 | 7.6 | 234 | 3.8 |
| Walking | 14 | 14.2 | 340 | 31.1 |
| BMI (kg/m2) | 40 | 27.1 (5.4) | 951 | 27.1 (4.2) |
LBP, low back pain; PA, physical activity; BMI, Body Mass Index; n, number of participants; SD, standard deviation; MZ, monozygotic; DZ, dizygotic.
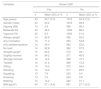
The results showed a strong inverse association between moderate (OR=0.44, 95% CI: 0.25 to 0.78, p=0.006), vigorous (OR=0.12, 95% CI: 0.01 to 0.91, p=0.041), and total physical activity and LBP (OR=0.36, 95% CI: 0.20 to 0.65, p=0.001) (Table 2) (Fig. 1). These analyses were adjusted for age, gender, and symptoms of depression or anxiety.
Cross-sectional association between leisure physical activity and low back pain adjusted for confounders.
| Multivariate models | OR (95% CI) | p-Value | R2 |
|---|---|---|---|
| Moderate PAa,b (n=1052) | 0.44 (0.25–0.78) | 0.01 | 0.06 |
| Vigorous PAa,b (n=1043) | 0.12 (0.01–0.91) | 0.04 | 0.07 |
| Total Leisure PAa,b (n=1010) | 0.36 (0.20–0.65) | 0.00 | 0.06 |
PA, physical activity; OR, odds ratio; CI, confidence interval; n, number of participants.
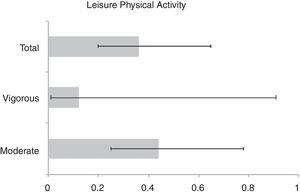
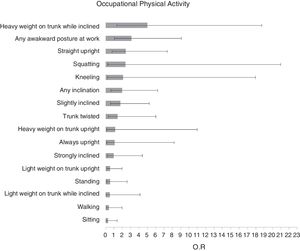
The results showed a strong association between lifting or carrying heavy weight on trunk while inclined and LBP (OR=5.0, 95% CI: 1.3 to 18.7, p=0.02). Likewise, any awkward posture at work was strongly associated with LBP (OR=3.1, 95% CI: 1.0 to 9.0, p=0.04). For the other variables (e.g. sitting or standing). There was no statistically significant association between the remaining occupational physical activity variables (e.g. sitting, standing) and LBP (Table 3) (Fig. 2). These analyses were also adjusted for age, sex, and symptoms of depression or anxiety were included in these multivariate models.
Cross-sectional association between occupational PA (workload variables) and the presence of recent LBP adjusted for confounders.
| Multivariate models | n | OR (95% CI) | p-Value | R2 |
|---|---|---|---|---|
| Straight uprighta,b | 338 | 2.39 (0.77–7.39) | 0.13 | 0.06 |
| Always uprighta,b | 366 | 1.07 (0.13–8.22) | 0.95 | 0.01 |
| Slightly inclineda,b | 391 | 1.75 (0.58–5.25) | 0.31 | 0.05 |
| Strongly inclineda,b | 383 | 0.95 (0.20–4.41) | 0.95 | 0.04 |
| Trunk twisteda | 380 | 1.43 (0.34–6.01) | 0.62 | 0.04 |
| Sittinga,b | 387 | 0.28 (0.05–1.38) | 0.12 | 0.07 |
| Standinga | 332 | 0.53 (0.11–2.58) | 0.44 | 0.05 |
| Squattinga | 246 | 2.37 (0.26–20.99) | 0.44 | 0.01 |
| Kneelinga | 247 | 2.08 (0.24–17.97) | 0.50 | 0.01 |
| Walkinga | 354 | 0.40 (0.08–1.96) | 0.26 | 0.05 |
| Light weight on trunk uprighta,b | 390 | 0.54 (0.15–1.96) | 0.35 | 0.01 |
| Heavy weight on trunk uprighta,b | 374 | 1.16 (0.12–11.01) | 0.89 | 0.01 |
| Light weight on trunk while inclineda | 390 | 0.51 (0.06–4.13) | 0.53 | 0.01 |
| Heavy weight on trunk while inclineda | 377 | 4.99 (1.33–18.74) | 0.02 | 0.04 |
| Any inclinationa | 368 | 1.98 (0.63–6.24) | 0.24 | 0.02 |
| Any awkward posture at worka,b | 376 | 3.08 (1.05–9.07) | 0.04 | 0.07 |
OR, odds ratio; CI, confidence interval; n, number of participants.
In this cross-sectional study, we investigated the relationship between different types and intensity of leisure and occupational physical activity, and recurrent LBP among people with a history of chronic LBP. Our findings demonstrate that leisure physical activity is associated with a lower prevalence of LBP. Likewise, because of the cross-sectional nature of our study, the results also show that people with recurrent LBP are engaging less in leisure physical activity. In contrast, some postures that people adopt in the occupational setting, such as carrying, lifting heavy weight while inclined, or adopting awkward postures (e.g. bending, twisting, squatting, and kneeling) are associated with a higher prevalence of recurrent symptoms of LBP. However, less complex postures such as sitting, standing, or walking are not associated with the prevalence of recurrent LBP.
Comparison of findings with previous researchIn regards to the relationship between leisure physical activity and LBP, our findings are consistent with the results of recent systematic reviews.22,38 Shiri and Falah-Hassani22 concluded that leisure physical activity might reduce the risk of chronic LBP by 11%–16%. Another systematic review38 investigating the relationship between physical activity and LBP concluded that people with chronic LBP with high levels of disability are likely to have low levels of physical activity. Other studies investigating the effect of physical activity intervention on a chronic pain population have suggested that physical activity may improve pain severity, physical function, as well as quality of life.39,40
Likewise, our results are in agreement with previous prospective studies investigating the effects of occupational physical activity for LBP. Heuch et al.41 conducted a longitudinal study with 14,915 adults aged 20 years or older and concluded that heavy physical workload increases the risk of chronic LBP. Another study42 showed that early exposure to heavier physical workload might have a long-lasting effect on the risk of LBP. Esquirol et al.43 also concluded that occupational factors have an important influence on the incidence of LBP. Whereas other studies,44,45 found that sitting or standing were not independently associated with LBP. However, a recently published systematic review could not confirm a causal relationship between occupational physical activity and LBP because there is still a lack of high-quality research investigating a causation pathway that can confirm this relationship.46
To date, the literature has provided insufficient evidence as to the extent which types and intensities of physical activity may increase or decrease the risk of developing LBP.47 The discrepancy in the literature is likely attributed to the different definitions of levels of physical activity and the lack of clarification on the type of physical activities investigated. Activities such as long walks and bike riding have been defined as strenuous physical activity in a longitudinal study identifying a protective effect,25 whereas the same types of physical activities were considered as of moderate intensity in another study that did not find any association with chronic LBP.23 A design limitation of previous studies is that comparisons across different types of physical activities are rarely performed in the same study.
Implications of study findingsClinicians should consider promoting the engagement in leisure physical activity in this population, such as encouraging walking as a leisure activity on a daily basis,48–50 especially through behavioral change techniques as there is growing evidence in the field suggesting that this approach might increase participation and adherence.51,52 However, the effects of such strategies should still be investigated in future prospective studies. Furthermore, given that some postures and loads adopted at work are more common in individuals with recurrent LBP, clinicians should consider performing a detailed assessment of an individual's occupational physical activities given these will probably have different effects on LBP.
Clinicians should also discuss the potential negative effect of frequent exposure to heavy lifting while inclined or awkward postures such as twisting, bending, squatting and kneeling in patients who frequently adopt these activities at work. Moreover, ergonomic advice regarding the use of body posture as a tool that can be changed to meet the job demands with minimum stress on the muscles, ligaments, bones and joints should be emphasized. A study looking at workplace prevention and musculoskeletal injuries in nurses showed that nurses with lifting devices and lifting teams in their workplace were significantly less likely to report neck or back pain.53 Another study investigating a multifaceted intervention consisting of participatory ergonomics, physical training, and cognitive behavior therapy showed a reduction in LBP among workers in eldercare.54 Therefore, multifaceted interventions aiming at reducing workers’ engagement in some occupational postures adopted at work, such as twisting, bending or lifting heavy weights, as well as encouragement to incorporate the practice of leisure physical activity while at work, may be relevant for improving LBP in a working population.
According to the latest global burden of disease report, occupational ergonomic factors are responsible for 31% of disability-adjusted life years due to LBP.7 The highest occupational risk is found in service industries and manual labor, especially agriculture. However, the management of most LBP cases remains mostly focused on pain relief and prevention of worsening outcomes through conservative care. Taking into consideration the great burden and the related economic consequences of lost work time, identification of effective preventive measures for LBP should be a priority for research.
Strengths and limitationsThis study has several strengths. First, occupational physical activity examined the combination of different body postures at work, which reflects a more realistic scenario, compared to the adoption of single plane movement. Second, both the outcome and the explanatory variables referred to a close and synchronized time point. Our outcome of recurrent LBP referred to pain within the past four weeks, while leisure physical activity and occupational physical activity, referred to activities within the last week.
When interpreting the findings of our analyses we also need to take into account some general study limitations. First, our study employed a cross-sectional design which limits the possibility of identifying a causal relationship between physical activity and LBP (or eliminating reverse causation). Second, we could not run any within-pair twin case-control analysis as there was a dramatic decrease in the sample size when discordant twin pairs were identified, and therefore the effects of genetics on the LBP-physical activity relationship could not be explored. Lastly, data on leisure and occupational physical activity were self-reported, and it is known that participants are likely to overestimate or underestimate their engagement in physical activity.55 However, the detailed description of different types of physical activities that we employed could only be assessed via self-reported tools as the MTR is a large population-based study.
Future high-quality longitudinal research is needed to identify whether a specific type and intensity of physical activity increase the risk of developing LBP. This may be challenging due to difficulties in obtaining accurate, objective measurements of intensity, duration, frequency, and type of physical activity performed.56 However, advancements in technology are gradually assisting in overcoming this barrier, evident by many studies making the transition from self-reported measurements of physical activity to pedometers57 and accelerometers.58,59 Accelerometers have been identified to be a more accurate tool for measuring physical activity compared to pedometers60 and self-reported measurements,61 although they still present limitations regarding calibration and structural modeling.62 Future methods are required to obtain more accurate physical activity objective measurements.
ConclusionOur study highlights that leisure and occupational physical activities are likely to have a different and divergent influence on LBP. Our results suggest the relationship between physical activity and LBP is highly dependent on how it is defined and assessed. Clinicians may support their patients to engage in leisure physical activity with the support of informed assessment of risks and explanation of the range of potential benefits.
Conflicts of interestThe authors declare no conflicts of interest.
The Murcia Twin Registry is supported by the Seneca Foundation, Regional Agency for Science and Technology, Murcia, Spain (08633/PHCS/08 & 15302/PHCS/10) and Ministry of Science and Innovation, Spain (PSI11560 – 2009). This study has been supported by a grant from the Fundación MAPFRE, Spain (2012). ABA holds the International Post-graduate Research Scholarship “Science without Borders” award from the Brazilian Government.
| Study variables | Original variables |
|---|---|
| Always upright | Straight, uprightStandingWalkingLight weight, lifted/carried while upright trunkMedium weight, lifted/carried while upright trunkHeavy weight, lifted/carried while upright trunk |
| Any awkward posture at work | Trunk twistedtrunk laterally bentsquattingkneeling with one or both knees |
| Any inclination | Slightly inclinedStrongly inclinedLight weight, lifted/carried while inclined trunkMedium weight, lifted/carried while inclined trunkHeavy weight, lifted/carried while inclined trunk |
| No load | Straight uprightSlightly inclinedStrongly inclinedTwistedLaterally bentSittingSquattingKneelingStandingWalking |
| Straight upright | Straight, upright |
| Slightly inclined | Slightly inclined |
| Strongly inclined | Strongly inclined |
| Trunk twisted | Twisted |
| Sitting | Sitting |
| Standing | Standing |
| Squatting | Squatting |
| Kneeling | Kneeling |
| Walking | Walking |
| Light weight on trunk upright | Light weight, lifted/carried while upright trunk |
| Heavy weight on trunk upright | Heavy weight, lifted/carried while upright trunk |
| Light weight on trunk while inclined | Light weight, lifted/carried while inclined trunk |
| Heavy weight on trunk while inclined | Heavy weight, lifted/carried while inclined trunk |
OR, odds ratio; CI, confidence interval; n, number of participants. aAdjusted for age and sex; bAdjusted for depression/anxiety levels.