Radiographs are used to monitor thoracic kyphosis in individuals with certain pathologies (e.g. osteoporosis), exposing patients to potentially harmful radiation. Thus, other measures for monitoring the progression of thoracic kyphosis are desirable. The gravity-dependent inclinometer has been shown to be reliable but its validity as a measure of thoracic kyphosis has not been investigated.
ObjectivesTo determine the validity of the gravity-dependent (analogue) inclinometer for measuring thoracic kyphosis.
DesignCross-sectional study.
MethodParticipants (n=78) were recruited as part of a larger study of shoulder impingement syndrome. Healthy participants (n=39) were age and gender matched to the shoulder impingement syndrome group (n=39). Measurements of thoracic kyphosis using a gravity-dependent inclinometer were compared with modified Cobb angle results obtained from a sagittal view of lateral radiographs. A Bland–Altman plot assessed agreement. The Pearson correlation coefficient and linear regression was used to determine the association between modified Cobb angles and inclinometer measurements.
ResultsThe Bland–Altman plot demonstrated good agreement. The Pearson correlation coefficient, r=0.62 (p<0.001), and linear regression model established a strong association between the thoracic kyphosis angle from the inclinometer readings and the modified Cobb angle measured from the radiographs (β=0.47, 95% CI 0.29, 0.65, p<0.001, R2=0.52, n=78). Age as a confounder was included in the model (β=0.35, 95% CI 0.19, 0.51, p<0.001).
ConclusionsThe gravity-dependent (analogue) inclinometer produces angles that are comparable to the modified Cobb angle obtained from radiographs, establishing its criterion validity as a safe clinical tool for measuring thoracic kyphosis.
Accurate measurement of the degree of kyphosis of the thoracic spine in the sagittal plane is important in conditions such as osteoporosis, ankylosing spondylitis and Scheuermann's disease,1–5 which require regular monitoring, usually with radiographic imaging.6 In 2011, $4.6 billion was spent in Canada on osteoporosis alone.7 Early detection of increased angles of thoracic kyphosis could result in early intervention and rehabilitation, potentially preventing health complications and saving costs.8
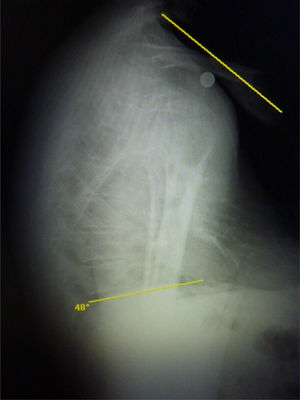
A common measure of the curvature of the thoracic spine in the sagittal plane is the modified Cobb angle (termed ‘modified’ as the original Cobb angle was designed for coronal plane radiographs). The gold standard for measuring the modified Cobb angle is using lateral thoracic spine radiographs.9 From the lateral radiographs, projected lines are drawn along two different thoracic vertebra endplates of the section of the thoracic spine being measured. For example, to measure the entire thoracic spine, projections of the top endplate of T1 and the bottom endplate of T12 would be drawn. Their intersection is called the modified Cobb angle. Before the introduction of digital radiographs, the intersection of these lines was hand drawn directly on radiographic films. Currently, the modified Cobb angle is calculated on digital images using computer software.10
Using lateral radiographs to monitor the angle of thoracic kyphosis in osteoporosis, ankylosing spondylitis or Scheuermann's disease is undesirable, as it exposes patients to excessive radiation given frequent repeated measures are required. Hence, other clinical measurement tools are needed which are valid, reliable, safe, cost effective, and easily and quickly applied. A systematic review (2014) of non-radiographic measures of thoracic kyphosis11 identified the gravity-dependent (analogue) inclinometer as a simple economical tool that had previously been shown to be a reliable measure of thoracic kyphosis,11,12 but at that time, no studies had established its validity.
There are three recent studies comparing inclinometer measurements of the thoracic spine with the modified Cobb angle from lateral radiographs. Two used digital inclinometers to obtain their clinical measure of thoracic kyphosis.13,14 Azadinia et al.13 measured 105 hyperkyphotic participants, aged 10–80 years, though only those participants aged between 10 and 30 years were used to establish agreement between the digital inclinometer measure of thoracic kyphosis and the modified Cobb angle.13 Sangtarash et al.14 measured 20 women with back pain, aged between 45 and 70 years.14 Both of these studies obtained their thoracic kyphosis measurements from digital inclinometers and compared them to radiographs taken on previous occasions, with no description of instructions to the participant during the radiograph or the time-frame between the X-ray and the inclinometer measurement.13,14 The most recent study by Barrett and colleagues15 used gravity-dependent inclinometers, with each of the 11 participants (mean age 40.9 years, SD 20.1) having both their shoulders and elbows flexed at 90 degrees for the radiograph, but with arms by their sides for the inclinometer measurement.15 These different arm positions for each measurement may have introduced differences in thoracic posture for the radiographs compared to the posture for the inclinometer measurements. Hence there are no studies that measure the angle of thoracic kyphosis using the gravity-dependent inclinometer and lateral radiograph where both measurements were performed at the same time with the participant standing in the same position.
If the inclinometer was established as a valid clinical tool for measuring an individual's thoracic kyphosis, as comparable to the modified Cobb angle from lateral radiographs, clinicians could confidently use it to regularly monitor changes in thoracic kyphosis in individuals with conditions such as osteoporosis, ankylosing spondylitis and Scheuermann's disease. This would decrease the exposure of patients to harmful ionising radiation as well as save costs.
This study aimed to assess the criterion validity of the inclinometer as a clinical instrument to measure thoracic posture by comparing the angle of thoracic kyphosis, calculated using inclinometer measurements, to the modified Cobb angle obtained from lateral radiographs, the gold standard.
Method and materialsParticipantsThis study was part of a case–control study investigating the possible relationship between thoracic posture and shoulder impingement syndrome (SIS). Eighty individuals participated. Forty healthy individuals with no shoulder symptoms were age and gender matched to 40 participants with SIS. Individuals with SIS were included if they had experienced shoulder pain for at least three months and were positive for at least three out of five orthopaedic clinical tests for SIS,16 and also confirmed as having SIS by a radiologist using ultrasound.
Healthy individuals without shoulder pain were included if they were confirmed as not having SIS by a radiologist using ultrasound, had not sought treatment for symptoms in their shoulder, back or neck within the last three months and had never had shoulder symptoms lasting longer than three weeks.
Potential participants were excluded if they had any condition where undertaking a radiograph was contraindicated (e.g. pregnancy); any history of previous traumatic injury or surgery to the shoulder, neck or back; any known, diagnosed malignancy, infectious disease, or inflammatory disease of the shoulder or spine; or any known, diagnosed neurological conditions (e.g., multiple sclerosis or stroke).17,18
The sample size was determined based on the number of participants required for the case–control study, which investigated differences in posture between individuals with and without SIS. A 5 degree difference in modified Cobb angle between groups (participants with SIS and healthy controls), with a standard deviation of 10 degrees (estimated from Katzman et al.19 and Fon et al.20) required 34 participants per groups to achieve a 5% level of significance with 80% power. The recruitment target was set at 40 participants per group.
Potential participants were sought from two sources: community advertising and a volunteer research register maintained by a local research institute. Advertising within the general community was in the form of a flyer advertisement displayed on noticeboards throughout a university campus, on local public noticeboards in shopping centres, on private health professional practice noticeboards, and on radio noticeboards. The volunteer research register was a list of individuals in the community who had previously agreed to have their contact details listed as being potential participants in research.
Human ethics approval was obtained from the University of Newcastle (H-2014-0192), Callaghan, NSW, Australia and all participants provided written informed consent before the commencement of this study.
Participant characteristicsThe participant's age, height and weight were recorded using a stadiometer (Health-o-meter, Bridgeview, Illinois, USA) and standard analogue scales (A & D, Seven Hills, NSW, Australia).21 From the height and weight measurements, a score for body mass index (BMI) was obtained.
Identifying key landmarksFor accuracy, participants were asked to remove all upper body clothing, with women wearing a gown, open at the back. Two pencil marks were placed on the skin over the spine on the C7 and T12 spinous processes. The C7 spinous process was found using palpation, as the C7 spinous process is considered to be the most prominent at the cervico-thoracic junction.22 To ensure the researcher was at the anatomically correct location, the participant was instructed to extend their neck and head. The C7 spinous process should not move while the C6 spinous process moves anteriorly.23 Shin et al.23 found this technique to be more accurate than relying on the C7 spinous process to be the most prominent.
Lumley22 has stated the most precise spinal landmark in the lower thoracic and lumbar spine is identifying L4 as being level with the line drawn between the iliac crests.22 Hence T12 was identified in the current study by locating L4 using the technique described by Lumley,22 and then counting up the spinous processes to T12 using palpation.
Modified Cobb angleFor this study, the modified Cobb angle measured from the lateral thoracic spine radiograph was the angle created by the intersection of the lines formed from the extension of the top of the endplate of T1 and the extension of the top endplate of T10 (Fig. 1). The top endplate of T10 was used as this was the last anatomically identifiable endplate able to be seen on every participant's radiograph. By using a radiographic computer package (Merge PACS, version 3.6, Merge Healthcare, Hartland, Wisconsin, USA) to calculate the angle, a consistent and accurate value for the modified Cobb angle was obtained.
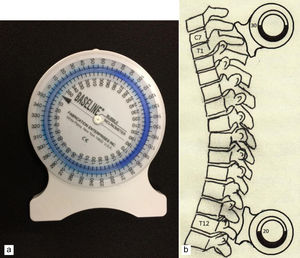
Clinical posture measureOnce the participant was in position for the radiograph, but before the radiograph was performed, the inclinometer measure for thoracic kyphosis was obtained. Participants stood with their left side to the X-ray bucky and were aligned with the X-ray field. They were given the single instruction: “leave your arms by your sides and face the wall” (which was approximately 1.5m in front of the participant). A gravity-dependent (analogue) bubble inclinometer (Baseline bubble inclinometer, Fabrication Enterprises Inc., White Plains, New York, USA) Fig. 2a was used to take the measurement. As the bubble inclinometer is gravity-dependent, it was first zeroed on a vertical wall prior to measurement. Using a standard clinical procedure, as outlined by Clarkson,24 the cephalic foot of the inclinometer was placed on the pencil mark already on the C7 spinous process.24 This procedure was repeated for the lower thoracic spine, with the caudal foot of the inclinometer placed on the pencil mark made for T12 (Fig. 2b). Both inclinometer angles were recorded, taking care to minimise parallax error with each measurement by ensuring the recorder's eyes were on the same horizontal plane as the inclinometer. The thoracic kyphosis measure from the inclinometer readings was obtained by taking the difference between the two measurements.
Lateral X-rayOnce the inclinometer measurements were recorded, the lateral radiograph of the thoracic spine was taken. Participants were already standing with their left side to the X-ray bucky and aligned with the X-ray field. They were again given the single instruction: “leave your arms by your sides and face the wall”, and they were allowed to breathe normally while the X-ray was taken.
Participants underwent a single lateral X-ray of their thoracic spine and a digital image of the radiograph was recorded. From this radiograph, the modified Cobb angle was automatically calculated using the “Cobb” tool of the Merge PACS software package and drawing lines parallel to the superior endplates of T1 and T10.
To test the reliability of the procedure for measuring the modified Cobb angle from the radiographs, two researchers (DH and IW) performed repeated measurements on 20 randomly selected digital radiographs. Both researchers were blinded to symptomatic status.
Statistical analysisStata statistical software (version 13, College Station, Texas, USA) was used to analyse the data. Descriptive statistics were calculated for participant characteristics. T-tests were used to determine if there were any significant differences in age or BMI between subgroups (painful SIS group and healthy without shoulder pain group) despite matching. A Bland–Altman plot was constructed to assess the level of agreement between the two measures of thoracic kyphosis.25 The Pearson product-moment correlation coefficient, r, and regression analysis were also calculated to establish whether a linear relationship between the modified Cobb angle, obtained from the lateral radiograph, and the thoracic kyphosis angle, from the inclinometer measurements, existed. For the correlation coefficient, the strength of correlation was assessed using the criteria established by Cohen (1988): large (r≥0.5), medium (0.3≤r<0.5) and small (0.1≤r<0.3).26 Age and BMI were assessed as potential confounders with the linear regression analysis, given the possibility they may were related to both the independent and dependent variables. Therefore, age and BMI were included as possible independent variables in the linear regression models that might further explain the relationship between the thoracic kyphosis measures. These analyses were applied to the whole sample (n=80) as well as the subgroups of participants with (n=40) and without (n=40) shoulder pain.
Intraclass correlation coefficients (ICC) were calculated for both the inter-rater and intra-rater reliability of the procedure for measuring the modified Cobb angle from the digital radiographs Based on the 95% confidence interval, reliability was considered excellent if ICC scores exceeded 0.9, good for scores between 0.75 and 0.9, moderate for scores between 0.5 and 0.75, and poor for scores lower than 0.5.27
ResultsUpon confirmation of SIS, or its absence, by the radiologist, two participants (one from each group) did not meet the eligibility criteria. Hence, data are presented for 78 of the full 80 participants originally recorded. Of the total 78 participants (mean age 56.4 years old, SD 10.8, range 40–77), 39 were female. Thirty-nine participants had SIS (19 female, mean age 57.1 years, SD 11.1, range 40–77) and there were 39 age and gender matched control participants with no shoulder symptoms (20 female; mean age 55.7 years, SD 10.6, range 41–74). There was no statistically significant difference in age between groups.
Mean BMI for participants with SIS was 29.3kg/m2 (SD 5.32), for healthy participants 25.7 (SD 3.53), and for the total sample 27.5 (SD 4.82). Participants with SIS had significantly higher BMI than those with shoulder symptoms (mean difference 3.53, 95% CI 1.49, 5.57, p<0.001).
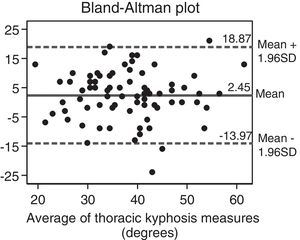
The Bland–Altman plot, Fig. 3, demonstrates good agreement between the modified Cobb angle and the thoracic kyphosis measure from the gravity-dependent inclinometer (mean difference 2.45 degrees, SD 8.38).
Bland–Altman plot comparing the thoracic kyphosis measurements from the inclinometer and radiographs (modified Cobb angle). The x-axis displays the mean of the two different thoracic kyphosis measurements, plotted against the difference (inclinometer value of thoracic kyphosis subtracted from the modified Cobb angle value) of the two measurements on the y-axis.
The Pearson's correlation coefficient was r=0.62 (p<0.001) (n=78) establishing a large linear relationship between the two measures for thoracic kyphosis. From the regression analysis, there was a significant association between the modified Cobb angle calculated from the radiographs (dependent variable) and the thoracic kyphosis angle measured using the inclinometer (independent variable) for the SIS group (β=0.62, 95% CI 0.31, 0.92, p<0.001, R2=0.31, n=39), the healthy group (β=0.58, 95% CI 0.31, 0.85, p<0.001, R2=0.34, n=39), and the groups combined (β=0.63, 95% CI 0.45, 0.81, p<0.001, R2=0.38, n=78). This association was adjusted for the potential confounders of age (Table 1) and BMI (Table 2) using multivariable linear regression.
Regression analyses where the dependent variable is the modified Cobb angle from the lateral radiographs and the independent variable is the angle calculated from the inclinometer measurements for the pain (SIS) and healthy (no shoulder symptoms) subgroups, and for all participants in total, with age included in the model as a confounder.
| Sample | Xi | Bi | 95% CI | p value | R2 |
|---|---|---|---|---|---|
| Pain (n=39) | 0.46 | ||||
| Inclinometer angle (°) | 0.41 | 0.10, 0.71 | 0.01 | ||
| Age (years) | 0.38 | 0.13, 0.63 | 0.004 | ||
| Healthy (n=39) | 0.49 | ||||
| Inclinometer angle (°) | 0.41 | 0.15, 0.67 | 0.003 | ||
| Age (years) | 0.35 | 0.13, 0.56 | 0.002 | ||
| Total (n=78) | 0.52 | ||||
| Inclinometer angle (°) | 0.47 | 0.29, 0.65 | <0.001 | ||
| Age (years) | 0.35 | 0.19, 0.51 | <0.001 |
Regression analyses where the dependent variable is the modified Cobb angle from the lateral radiographs and the independent variable is the angle calculated from the inclinometer measurements for the pain (SIS) and healthy (no shoulder symptoms) subgroups, and for all participants in total, with BMI included in the model as a confounder.
| Sample | Xi | Bi | 95% CI | p value | R2 |
|---|---|---|---|---|---|
| Pain (n=39) | 0.36 | ||||
| Inclinometer angle (°) | 0.59 | 0.28, 0.89 | <0.001 | ||
| BMI (kg/m2) | −0.39 | −0.90, 0.12 | 0.13 | ||
| Healthy (n=39) | 0.37 | ||||
| Inclinometer angle (°) | 0.54 | 0.26, 0.81 | <0.001 | ||
| BMI (kg/m2) | 0.44 | −0.23, 1.11 | 0.20 | ||
| Total (n=78) | 0.39 | ||||
| Inclinometer angle (°) | 0.64 | 0.45, 0.82 | <0.001 | ||
| BMI (kg/m2) | −0.08 | −0.45, 0.28 | 0.65 |
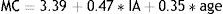
Including age as a covariate improved the regression models (higher R2 value, Table 1), but including BMI did not (Table 2). Therefore, to depict the relationship between the modified Cobb angle from radiographs and the thoracic kyphosis angle from the inclinometer measurements, the following equation was derived from the final regression model (including age) for the total sample (n=78), from Table 1:
where MC=modified Cobb angle from a digital radiograph, IA=the thoracic kyphosis angle calculated from the inclinometer measurements, and age=age of participant.Intra-rater reliability for measuring the modified Cobb angle from the digital radiographs was excellent for rater one (ICC2,1=0.99, 95% CI 0.98, 1.00) and good to excellent for rater two (ICC2,1=0.88, 95% CI 0.71, 0.95).27 Inter-rater reliability was good to excellent (ICC2,1=0.89, 95% CI 0.73, 0.96).
DiscussionThis study has demonstrated that the thoracic kyphosis angle obtained from inclinometer measurements was linearly related to, and had good agreement with, the modified Cobb angle obtained from a lateral radiograph, the gold standard. Hence, the analogue inclinometer has criterion validity measuring thoracic kyphosis in the sagittal plane. This means clinically that an increasing thoracic kyphosis due to the progression of a pathology, such as osteoporosis, ankylosing spondylitis or Scheuermann's disease can be monitored using an inexpensive gravity-dependent inclinometer, rather than repeated radiographic exposures.
This study is unique in that it is the first to establish criterion validity by comparing a thoracic posture measure from inclinometer readings to the modified Cobb angle from lateral radiographs, where both measurements were performed at the same time while participants maintained the same thoracic posture. Both of the dual digital inclinometer studies13,14 did not perform the different thoracic kyphosis measures at the same time, and provided no description of the participants’ posture for the lateral radiograph. Unlike the present investigation, the Barrett et al.15 study used different postures for their different thoracic kyphosis measures. Despite these methodological differences from the present investigation, all three previous studies demonstrated good agreement between the two different thoracic posture measures using Bland–Altman plots, comparable to the current study (mean difference 2.45 degrees, SD 8.38).
This is the first study to establish criterion validity of the inclinometer using both male and female participants aged over 40 years. The only other study comparing gravity-dependent, analogue inclinometer measurements to lateral radiographic measurements used a sample of only 11 participants.15 Two other validity studies compared thoracic posture measured using dual digital inclinometers to the modified Cobb angle from lateral radiographs, but with different population samples. The study by Azadinia et al.13 enlisted 105 participants in total, but to establish agreement, used 81 hyperkyphotic participants aged between 10 and 30 years. Sangtarash et al.14 recruited just 20 women with back pain aged 45–70 years.
The findings also demonstrate that using the Merge PACS software to determine the modified Cobb angle from digital lateral radiographs has good to excellent intra-rater and inter-rater reliability. The small difference in intra-rater reliability between the two raters is likely due to the differences in experience in using the computer software. Rater one (intra-rater ICC=0.99) had been using the software over a period of approximately 15 months, measuring the modified Cobb angle for all 78 participants. The second rater (intra-rater ICC=0.88) performed their repeated measures (n=20) within a 24-hour period following training in the software. Despite this relative lack of experience, their intra-rater reliability was still good to excellent.
A previous study by Min et al.10 has compared the modified Cobb angle calculated using computer software from digital radiographs to the modified Cobb angle calculated using manual techniques from radiographic films. The results demonstrated that the modified Cobb angle calculated using computer software was more precise,10 supporting the method employed in our study. Notably only the study by Barrett et al.15 used computer software to calculate the modified Cobb angle, while the two studies which used digital inclinometers13,14 manually calculated the modified Cobb angles.
Osteoporosis, ankylosing spondylitis and Scheuermann's disease are usually progressive diseases, with increasing thoracic kyphosis a common clinical feature that is usually regularly assessed radiologically. Early diagnosis of osteoporosis and intervention to prevent, or at least slow, hyperkyphosis is considered important in maintaining quality of life.5 Appropriate exercise has been shown to be beneficial for osteoporosis, ankylosing spondylitis and Scheuermann's disease.5,28–30 A quick and valid clinical measure, such as the hand held gravity-dependent inclinometer, would enable health practitioners to know when to prescribe exercise or another intervention, assess whether the intervention was having the desired effect of maintaining, or even improving, a patient's thoracic kyphosis, and know when to progress to other appropriate management strategies.
The establishment and use of the linear regression model formula is important because using it would allow an estimated value for a modified Cobb angle to be obtained from inclinometer measurements. Medical practitioners working with ankylosing spondylitis and Scheuermann's disease decide on different treatments according to the degree of thoracic kyphosis31 from modified Cobb angle results from radiographs, with surgery required once the kyphosis has increased to a certain degree.32,33 Using the gravity-dependent inclinometer, accurate and more frequent monitoring of these conditions could occur, with less use of potentially harmful ionising radiation. This might lead to earlier diagnoses, earlier interventions, improved quality of life for patients and less cost to the health system.
One limitation of the current study is that neither the radiologist, nor the researcher, was blinded as to whether the participant was suffering from SIS or not when the radiograph and inclinometer measure of thoracic posture was performed. Another limitation is that the inclinometer measurements were taken from C7 to T12. Therefore, the validity of using the inclinometer for measuring the thoracic kyphosis angle over smaller regions of the thoracic spine, for example T3 to T8, is unknown. However, there is no reason to suspect it would be markedly different to the results of this study.
The main limitation of this study is that the results are limited to the sample population of individuals with and without SIS. It is difficult to know if these results can be directly extrapolated to individuals with conditions such as osteoporosis, ankylosing spondylitis or Scheuermann's disease. While the age range of our participants (both healthy and musculoskeletally impaired) was 40–77 years, consistent with the common age range for individuals with osteoporosis and ankylosing spondylitis,4,5 similar studies on participants with these pathologies may be appropriate. Results may be different if the inclinometer was compared to radiographs in individuals with Scheuermann's disease,2 which commonly occurs in adolescence, an age group not included in this paper.
A final limitation is that the sample size for this study was based on the number needed to detect a difference in the modified Cobb angle between individuals with SIS and asymptomatic controls (for a separate study), rather than specifically based on the number needed to establish criterion validity. Despite this, the sample adequately demonstrated criterion validity and is larger than previous studies examining the validity of thoracic posture measurements for individuals over 40 years using inclinometers.14,15
ConclusionThis study has established that the gravity-dependent (analogue) inclinometer has criterion validity when measuring thoracic kyphosis, comparable to the lateral thoracic spine radiograph, the gold standard. For those individuals presenting clinically with conditions where progressive kyphosis is problematic, it is possible for the clinician to monitor their condition using inclinometer measurements, potentially reducing the need for repeated radiographs that expose patients to harmful radiation.
Conflicts of interestThe authors declare no conflicts of interest.
The authors would like to thank the Hunter Medical Research Institute (HMRI) for assisting with participant recruitment.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.