The hammock positioning within the incubators simulates the intrauterine environment, however, there is little evidence of its benefits and possible risks.
ObjectivesThe aim of this study was to assess the effects of hammock positioning on behavioral status, vital signs, and pain in very low birth weight preterm newborns.
MethodsThis is a quasi-experimental/case series study in which premature infants (<1500g) were positioned in supine for one hour in a hammock. The preterm newborns were assessed 10min before, during (2, 20, 40, and 60min), and 10min after hammock positioning with the Brazelton Neonatal Behavioral Assessment Scale, vital signs and pain by the Neonatal Facial Coding System.
Results28 preterm infants between 28 and 36 weeks of gestational age were evaluated. Regarding the behavioral state, the preterm newborns progressively evolved to light or deep sleep during hammock positioning. There was a statistically significant reduction of the heart and respiratory rate from 2 to 60th minute in a hammock, which was maintained after the positioning. The oxygen saturation remained within normal values. No changes in pain scores were observed.
ConclusionThe hammock positioning can be considered a safe method of positioning that can be used to reduce the stress levels in very low birth weight preterm newborns. We did not observe worsening in either pain or vital signs.
The hammock positioning (Hp) refers to the positioning of newborns in a small rectangle fabric (hammock) fixed by extremities within the incubators. Hp is a simple and low-cost method for the therapeutic positioning of newborns. This technique has been used by physical therapists in several Neonatal Intensive Care Units (NICU), although little is known about Hp.1
Preterm newborns are exposed to a stressful environment and painful interventions in the NICU.2 Low birth weight is also associated with increased morbidity and mortality and motor development delay in preterm infants.3 The adequate therapeutic positioning of the preterm can minimize postural abnormalities and asymmetries related to prematurity and stay in NICU, also favors the development of spontaneous and functional motor abilities of newborns.4 Studies indicate that the positioning directly influences the cardiovascular, respiratory, and sleep-wake states.4–6
The Hp intends to promote preterm containment, vestibular stimulus, sensory integration, tonic, and behavioral reorganization, thus reducing the noxious sensory stimuli to which the immature brain is exposed in the NICU.4,5 In addition, Hp potentially simulates the intra-uterine environment, provides relaxation, stimulates the harmonization of movements, and reduces the energy expenditure of very low birth weight newborns.5 Some studies indicate that the technique promotes the reduction of stress during the period of hospitalization, so it can be considered a strategy to humanize the care in the NICU.7–9
However, some Hp related outcomes such as vital signs,10 pain and behavioral status11 and motor development are still controversial due to low methodological quality used in most studies.6 Some studies also point to the risks of apneas or desaturation during Hp.10,11 Recent reviews1,12 on this topic highlight the lack of scientific evidence that proves the benefits and possible risks of Hp. Therefore, the objective of this study was to evaluate the effects of Hp on the behavioral states, pain, and vital signs of very low birth weight preterm newborns.
MethodsDesign and local of studyIt consists of a quasi-experimental/case series study carried out in the NICU of the Hospital Sofia Feldman – a philanthropic institution linked to the Unified Health System and located in Belo Horizonte, Minas Gerais, Brazil.
Ethical aspectsThe research project was approved by the Ethics and Research Committee of the Hospital Sofia Feldman, Belo Horizonte, MG, Brazil (number 1.684.322). All mothers or legal guardians for the preterm signed the free and informed consent term to authorize their participation in the research.
SubjectsSubjects inclusion criteria were: very low-weight preterms (infants with 1500g or less who was born before 37 weeks of pregnancy) with more than 24h of life, respiratory and hemodynamic stability, without continuous sedation, and/or use of amines.
We excluded preterm newborns that presented neurological signs or symptoms, use of continuous diet, gastroesophageal reflux, the presence of malformations, grade 2 or higher of peri-intraventricular hemorrhage, severe heart disease, immediate postoperative period, use of surfactant in less than 72h, phototherapy or under minimal manipulation.
Data collectionThe included preterms were positioned for one hour in the supine position in a hammock for at least 60min after the last diet. The hammocks were made of cotton fabric 1cm thick. A fabric was also placed between the cervical and scapular region of the NTBs so there was no hyperflexion or hyperextension of the head, which could impair respiratory function. To fix the hammocks in the incubators, the circular openings were used to pass the ropes and the ropes were tied in the upper part of the incubator as shown in Fig. 1. The behavioral state, vital signs, and pain were evaluated in newborns according to the following instruments.
The pain evaluation was performed with the Neonatal Facing Coding System (NFCS).13 This scale is based on the evaluation of the presence of the following facial expression: wrinkled foreheads, compressed palpebral fissures, deep nasolabial groove, half-open lips, mouth vertical or horizontal outstretched, tense tongue, tongue protrusion, and the chin quivering.14 The presence of each item scores 1 point from the maximum score of 8 points. It is considered the presence of pain when 3 or more facial movements quoted appear during the evaluation.
The sleep/wake cycle was evaluated by the Brazelton Neonatal Behavioral Assessment Scale (NBAS).15 The scale scores the behavioral state respectively from 1 to 6: deep sleep, light sleep, drowsy, alert, eyes open, and crying.
The heart rate (HR) and peripheral oxygen saturation (SpO2) was monitored with a multiparametric monitor DX 2022® (Dixtal, Brazil) by a sensor positioned on the external side of one foot. The respiratory rate (RR) was assessed by visual inspection of respiratory cycles per minute.
The evaluations were performed 10min before the positioning in hammock, at the second, twentieth, fortieth, and sixtieth minutes after the positioning of the newborn in hammock, and 10min after the return of the newborn to your incubator.16 The newborn when removed from the Hp was placed in the incubator in the same position as the baseline evaluation. Data were collected in the morning and afternoon. The NFCS and NBAS scales were applied at each evaluation, in addition to the vital signs collected.
The study would be discontinued if vital signs of the newborn presented a variation greater than 20% of the baseline or signs of respiratory effort (use of accessory muscles in the neck, intercostal, subcostal, and suprasternal retractions or nasal flaring), or constant crying.
Statistical analysisThe sample size was calculated using the G * Power 3.1.9.2 software, considering the comparison of the six measurements in one group using repeated measures ANOVA with alpha level or probability of error of 0.05. The minimum sample for the survey was then calculated in 28 participants.
Data were analyzed by the BioEstat software version 5.3 (Pará, Brazil). The Shapiro–Wilk test analyzed the distribution of study variables. Numerical variables were presented in mean and standard deviation and categorical variables in absolute value (relative). ANOVA for repeated measurements with the Tukey post hoc test was performed to compare the numerical variables with parametric distribution between the evaluations at different times. Friedman test with Dunn's post hoc test was performed to compare numerical variables with no parametric distribution. Cochran's Q and Friedman tests were performed to compare the categorical variables. A significance level of p<0.05 was considered.
ResultsOf the eligible population, 28 preterms were included, of which 17 (61%) were female. Only 1 newborn was not included due to lack of consent. The newborns gestational age varied from 24 to 31 weeks. The other characteristics of newborns included in this study are described in Table 1.
Characteristics of preterm newborns studied.
| Variable (n=28) | Mean±SD | Minimum–maximum |
|---|---|---|
| Chronological age (days) | 21.8±16.5 | 6–67 |
| Gestational age at birth (weeks) | 28.1±1.6 | 24–31 |
| Post-conceptional age at evaluation (weeks) | 31.2±2.1 | 28–36 |
| Weight at birth (g) | 954.6±191.4 | 605–1390 |
| Weight at evaluation (g) | 1124.2±258.9 | 685–1470 |
SD, standard deviation.
Regarding oxygen supplementation, 15 (54%) were breathing ambient air and 4 (14%) using a nasal catheter. Regarding ventilatory support, 9 newborns were in ventilatory support: 6 (21%) were using the nasal continuous positive airway pressure mode and 3 (11%) noninvasive positive pressure ventilation with two levels of pressure.
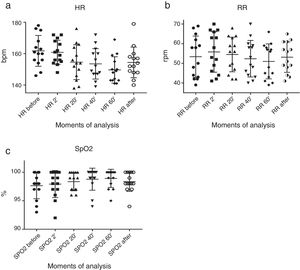
Regarding the behavioral assessment (Table 2), a significant difference was observed when comparing the moments before, during, and after the Hp (p<0.001). Most of the preterm newborns gradually evolved into light sleep or deep sleep during the Hp. At 60min, 7 (25%) of the 28 newborns assessed were in deep sleep and 18 (64%) in light sleep. Results for vital signs are shown in Fig. 2. HR and RR showed a significant reduction from 2° to 60° minute of Hp (p<0.001). However, this reduction in HR and RR values were not clinically relevant. SpO2 presented non-significant oscillations, remaining between 92% and 100%. Vital signs varied within normal limits.
Neonatal behavioral assessment of preterms before, during, and after hammock positioning.
| Before | During | After | ||||
|---|---|---|---|---|---|---|
| 2min | 20min | 40min | 60min | |||
| Deep sleep | 0 (0) | 0 (0) | 2 (7.1) | 4 (14.3) | 7 (25.0) | 0 (0) |
| Light sleep | 15 (53.6) | 2 (7.1) | 15 (53.6) | 21 (75.0) | 18 (64.3) | 11 (39.3) |
| Drowsy | 5 (17.9) | 9 (32.1) | 8 (28.6) | 2 (7.1) | 1 (3.6) | 12 (42.9) |
| Alert | 1 (3.6) | 4 (14.3) | 1 (3.6) | 0 (0) | 1 (3.6) | 4 (14.3) |
| Eyes open | 7 (25.0) | 11 (39.3) | 2 (7.1) | 1 (3.6) | 0 (0) | 1 (3.6) |
| Crying | 0 (0) | 2 (7.1) | 0 (0) | 0 (0) | 1 (3.6) | 0 (0) |
Data presented in absolute and relative number: n (%). Cochran's Q test p<0.001.
There was no significant difference in pain scores when compared the moments before, during, and after Hp (p=0.42). Only 1 newborn had a facial expression of pain before Hp, which got better after the 20° minute. In the second minute, 2 newborns had a facial expression of pain and another one had the same expression at 60° minute of positioning.
There were no adverse events or instability of the newborns during Hp that justified their return to the incubator.
DiscussionThe hammock positioning of preterm newborns with very low birth weight was safe, induced sleep in preterm infants, maintained vital signs within the normal range and did not cause any pain in our sample. The Hp induced relaxation in preterms, since most of the newborns evolved into a state of sleep, which may favor brain maturity and consequently the neuropsychomotor development.5 Moreover, the state of relaxation provided by Hp prevents energy expenditure, facilitates sleep, and may interfere positively in the neuromotor development of preterms.2 Non-pharmacological measures that increase preterms sleep time within NICUs should be stimulated in order to regulate the sleep-wake cycle, reduce stress levels and promote the sensory organization of preterms, which favors weight gain of newborns with very low birth weight.16
Cavalaria17 states that removing a preterms from the warmth of its mother and placing it on a flat and sometimes without coatings surface, is to be unaware the extreme need for support, restraint, and swinging. It is important to implement safe and humanized methods of sensory-motor stimulation within the NICU, which favor the neuropsychomotor development of preterm newborns, especially those who are subject to long periods of hospitalization. The main advantages of the hammock in relation to prone positioning are the greater contention to the newborn, not allowing constant changes as it occurs in the nest; better stimulus to flexor tone, favoring this postural pattern; better self-regulation, guaranteeing autonomic stability; and greater body symmetry stimulating the joining of the hands in the midline.11,18 Therefore, Hp could bring both short-term and long-term benefits to the development of preterms. Albuquerque et al.19 suggest the training of professionals working in the NICU to disseminate the use of hammock positioning.
We observed that Hp did not cause any type of discomfort in preterms. According to Costa et al.,11 Hp contributes to humanization in preterm newborns care. Hp demonstrated superiority compared to positioning in the nest because it promoted a greater reduction of stress levels, posture improvement, and preterms organization, and it may be recommended after a stressful stimulus, such as diaper changes. In our study was verified a reduction of HR and RR throughout the positioning, probably related to the relaxation provided to the preterms evaluated. Our results corroborate the findings of Costa et al.20 that also observed a reduction of HR and RR during Hp. Similar results were obtained by Keller et al.10 who compared Hp to prone positioning in very low weight preterm newborns. The authors found that the Hp showed better autonomic stability, maintaining the SpO2 within the normal range, lower RR, and HR and also better neuromuscular maturity compared to prone.10
Regarding oxygenation during Hp, Bottos et al.18 found no difference in oxygen levels in the supine position within the incubator and Hp. Another study that compared the positioning of healthy term infants placed in a hammock outside the incubator with the positioning in the crib also did not identify any changes in SpO2.21 Those results corroborate our findings. Still, Zanardo et al.22 evaluated Hp in oxygen-dependent preterms with bronchopulmonary dysplasia and observed a worsening of SpO2 after Hp. The authors suggest that these group of newborns may present severe hypoxemia during Hp. The preterms who were under ventilatory support in our study maintained the same parameters without adjustment needs. We did not observe any adverse events such as apneas or desaturation during Hp as it has been observed in other studies.10,11 We suggest as used in our study the use of a fabric placed between the cervical and scapular region of the preterms in order to reduce cervical hyperflexion, minimizing the risk of apnea and SpO2 fall.
Despite the absence of complications during the positioning in our study, the indication of Hp needs to be individualized and used in a careful way especially with low birth weight preterms. Newborns may regurgitate during Hp if they are placed in the hammock soon after the diet or if they have major gastroesophageal reflux. Moreover, the fixation of the hammock needs to be done safely so there is no risk of instability or fall of the preterms, thus providing adequate containment.
The absence of a control group may be considered as a limitation of our study. In addition, it would not be possible to blind the investigators to the intervention, but we kept them unaware of the purpose of the study. One possible bias is a subjective assessment of pain and NBAS scale, which evaluates facial expressions and behavioral status of the newborns. The fact of the data collection was not done at the same period of the day in all participants could be another bias. Future randomized controlled trials with a larger sample need to be conducted with the purpose of increasing the external validity of our findings, as well as monitoring newborns for more than one hour to comprehend how vital signs behave after this period.
From our findings, Hp may be indicated as a safe, simple, and low-cost therapeutic option for the humanization of NICUs. Non-pharmacological and low-risk measures that promote the reduction of stress levels and pain in very low birth weight preterm newborns should be stimulated in NICUs.
ConclusionHammock positioning seems to induce sleep, maintained the vital signs within the normal range, and did not cause pain in very low birth weight preterm newborns. Hp may be considered as a safe positioning method and a non-pharmacological therapeutic measure for the reduction of stress levels, as well as for the humanization of NICUs. Further randomized controlled trials, with a larger sample and longer follow-up, are needed to evaluate the long-term outcomes of hammock positioning especially concerning neuromotor development.
Conflicts of interestThe authors declare no conflicts of interest.
We are thankful to the multi-professional team of Hospital Sofia Feldman, especially to the physical therapy and nurse team, for the help to conduct this research.