Cervical proprioception is a common term used in neck rehabilitation, and it is examined using neutral head position (NHP) and target head position (THP) tests.
ObjectiveTo investigate intra- and inter-rater reliability of the NHP and THP tests in patients with neck pain and in healthy controls.
MethodsThe intra-rater (between-day) and inter-rater (within-day) reliability of the NHP and THP tests were assessed in 36 patients with neck pain and 33 healthy subjects. NHP testing was evaluated in cervical extension, while THP testing was evaluated in six directions of cervical motion: cervical flexion, extension, side bending right, side bending left, rotation right, and rotation left.
ResultsThe intra-rater reliability for the NHP tests had intraclass correlation coefficient (ICC) values of 0.74–0.78 and a standard error of measurement (SEM) of 1.78–1.88; the THP tests had ICC values of 0.70–0.83 and SEM of 1.45–2.45. Likewise, inter-rater reliability for NHP had ICC values of 0.74–0.79 and SEM of 1.79–1.87. For the THP test, the inter-rater reliability had ICC values of 0.62–0.84 and SEM of 1.50–2.23.
ConclusionIntra- and inter-rater reliability ranged from good to very good agreement both for NHP and for THP tests of cervical proprioception.
Neck pain is a prevailing condition in the general population. It is reported to be the second most common musculoskeletal complaint, next to back pain.1,2 The one-year prevalence estimates of global neck pain range from 30 to 50% among adults.3 At any given point in time, approximately 12–14% of the middle-aged population reports having neck pain.3 Neck pain often causes impairment and disability and can contribute to work absences, which increases the cost both for compensation as well as treatment, thereby affecting health related quality of life.4,5
Proprioception refers to the afferent information sent by muscles, ligaments, joints, tendons, and associated mechanoreceptors to the nervous system.6,7 Proprioceptive inputs from periphery muscles, joints, joint capsules, and ligaments are processed in the spine, brainstem, cerebellum, and cortex in order to produce efficient and precise movement patterns with appropriate neuromuscular yield.7
Methods for assessing cervical proprioception include the neutral head position (NHP) and target head position (THP) tests.8,9 During an NHP test, the subject tries to re-position the head to a neutral head position after being moved away from the NHP, whereas during a THP test, the subject re-positions the head to a target position predetermined by the investigator.10
Cervical muscle fatigue and whiplash injuries can lead to proprioception deficits, which can also be considered a contributing factor in chronic neck pain.8,11–13 NHP and THP tests are sensitive to differences between patients with neck pain and healthy controls.14,15 In patients with neck pain, whiplash injury, and spondylosis, impaired proprioception measured by THP is associated with both poor functional performance measured by neck disability index and poor subjective estimation of neck function, measured by the visual analog scale. Thus, one can infer that proprioception is an important indicator for neck pain and neck injury deficits.10,16
As cervical proprioception (joint position error) is a frequently evaluated in physical therapy practice for patients with neck problems, it is important for therapists to have an objective tool for its measure. Cervical proprioception was evaluated in patients with and without neck pain using different measurement methods and techniques.17–20 Objective tests measure alterations in proprioception awareness as “errors” in head and neck re-positioning. Different analytic devices, such as the electromagnetic tracking device (3-space FastTrack) and the ultrasound-based measuring device (Zebris), show good intra- and inter-session reliability (intraclass correlation coefficient – ICC≥0.61–0.84) for cervical joint position error evaluation.20–22
The digital inclinometer is a clinical tool used to measure cervical proprioception. From a clinical point of view, the digital inclinometer is easy to use, requires less time than the above-mentioned devices, and can be equipped quickly to test cervical proprioception in all directions. Furthermore, it is an affordable tool for clinics, compared to other motion analysis systems. The digital inclinometer can be used to assess a subject's ability to relocate the head to NHP and THP (active cervical range of motion). However, the reliability of these cervical proprioception clinical tests is still unknown. The aim of this study is to assess the intra- and inter-rater reliability of the NHP and THP tests in patients with neck pain and in healthy controls.
MethodsStudy designAn intra-rater (between-day) and inter-rater (within-day) design with a three-phase reliability protocol that consisted of: (1) preparation phase, (2) training phase, and (3) overall agreement phase was used. The reliability protocol is recommended by the International Academy of Manual/Musculoskeletal Medicine (IAMMM).23 The preparation phase consisted of agreement of study conditions and strategy. The training phase focused on replicating test procedures and judgment. The focus of overall agreement phase was designed to establish an overall agreement percentage greater than 80% between the two examiners. Once the protocol was completed, examiners A and B agreed upon the cut-off point, as well as how to perform and standardize each test. Each subject attended two evaluation sessions. Both examiners evaluated the subject on both occasions. Intra-rater reliability was established based on examinations that took place on two different days (≤3 working days apart). Inter-rater reliability between examiners A and B was established by comparing their examinations on both the first and second assessment sessions.
SubjectsThe study was conducted in the department of physical therapy, approved by the Research Ethical Board of King Khalid University (HA-06-B-001), Abha, Kingdom of Saudi Arabia. All subjects were required to provide informed consent prior to the commencement of the study. The subjects with neck pain were recruited from the university's physical therapy clinic. Patients were eligible to participate in the study if they met the following inclusion criteria: (1) patients had non-specific neck pain, (2) patients had visited a physical therapist for neck pain, and (3) patients were 18 years of age or older. Patient exclusion criteria were (1) spine surgery, (2) whiplash injury, (3) pregnant women, (4) musculoskeletal or neurological problems, and (5) symptoms of radiculopathy confirmed by positive Spurling's test and upper limb tissue tension test.24 Healthy subjects were recruited using poster advertisements and word of mouth. Healthy subjects included in the study were 18 years of age or older. Exclusion criteria for the control group were: (1) neck pain in the last year, (2) any upper quarter problem, and (3) any rheumatic diseases or neurological disorders. Neck pain subjects did not receive any treatment during participation in the study. All the subjects were instructed not to engage in exertional activities and to follow their daily living routine activities between evaluation sessions.
ExaminersClinical data were collected by two physical therapists (examiners A and B) working in the university's physical therapy clinic. Both examiners have a minimum of ten years of experience. Two data recorders were employed; recorder 1 teamed up with examiner A, and recorder 2 teamed up with examiner B to record data. The respective recorders collected data using standardized record sheets. The order of examinations was randomized so that no examiner evaluated all patients first. Examiners were also blind to each other's results and to whether the subject had neck pain.
Data collectionPrior to the study's commencement, all subjects were informed about the study's procedures in detail. Subjects who met the inclusion criteria became participants, and their first evaluation session was scheduled. Demographic variables (age, height, weight, education level) were recorded. Neck pain was evaluated using the 100-mm visual analog scale (VAS), with 0mm indicating “no pain” and 100mm indicating “worst imaginable pain.” In addition, all of the subjects completed the neck disability index (NDI), a self-reported questionnaire used to evaluate disability due to neck pain. The NDI is a 10-item questionnaire with six response categories for each item (range 0–5, total score between 0 and 50); a lower score means better function.
Upon completion of the questionnaire, subjects were asked to carry out NHP and THP testing with examiner A, followed by a short 15-min break. After the break, subjects continued the NHP and THP testing with examiner B. Each test session lasted for approximately 15min. Efforts were made to ensure that all subjects were tested at the same time of day for both of their evaluation sessions.
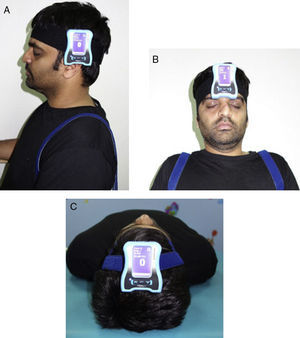
Measurement of cervical proprioception (NHP and THP testing)Subjects sat upright on a chair with back support for the measurement of NHP. The subject sat erect with hip and knee bent at approximately 90 degrees, and feet placed firmly on the ground. A strap was used to secure the thoracic spine to the chair during cervical movements. A digital inclinometer (Dualer IQ; JTECH Medical, Salt Lake City, UT, USA) was placed on the side of each patient's head to measure NHP from extension (Fig. 1A). NHP was tested while patients maintained their heads in a neutral position, with eyes closed. The inclinometer was calibrated to its starting position (0 degrees) by the examiner. Subjects memorized this neutral position for a few seconds, then performed active full extension, and finally relocated to the neutral position. Subjects were instructed to perform the test as accurately as possible and to verbally indicate when they were sure they returned to the starting position. This relocation accuracy was then measured; no visual or verbal feedback was given to the subjects during the test. The NHP test was performed in one direction only (cervical extension). Three trials were performed, and the average of the three trials was used for analysis.
To measure THP, subjects were required to adopt two positions: (1) sitting position (measure THP/NHP into flexion, extension, side bending right and left) and (2) supine position (measure THP into rotation right and left). A digital inclinometer was placed on the side of the patient's head to measure THP into flexion and extension (Fig. 1A), on the center of forehead to measure THP into side bending right and left (Fig. 1B), and on the vertex of the head in the supine position to measure THP into rotation right and left (Fig. 1C). To test THP, the examiner moved the subject's head slowly to the predetermined target position, 50% of maximum range of motion. The head was maintained in the target position for three seconds, subjects were asked to remember that position, and then the head was brought back to the neutral position. Subjects were then asked to actively re-position themselves by moving their heads to the target position. When the subject reached the target position, relocation accuracy was measured in degrees. Subjects performed three trials in each movement direction (flexion, extension, side bending right and left, and rotation right and left). The order movement direction testing was randomized using a simple lottery method. Only the absolute error was taken as a measurement because it represented the difference between the actual angle relative to the target angle, which had no directional bias compared to constant error or relative error.
Statistical analysisData were analyzed using SPSS software version 20. The data was checked for assessing normality with the Shapiro–Wilk Test and was found to follow normal distribution. Intra- and inter-rater reliability were assessed using intraclass correlation coefficient (ICC) agreement values, with a 95% Confidence Interval (CI). The study adopted recommendations made by the consensus-based standards for the selection of health measurement instruments (COSMIN) checklist.25 ICC agreement was favored because it considered random and systematic errors. To evaluate agreement between the rater's scores, the Bland–Altman limits of agreements (LOA) method was used.26 Standard error of measurement (SEM) was recommended as the measure of agreement. The SEM can be interpreted as the standard deviation of measurement errors; the smaller the SEM, the smaller the deviation of measurement errors around the mean, and the more reliable the measure.27 SEM agreement was described by the formula: σ2o+σresidual2 where σ2o represented the variance due to systematic differences in testers (inter-rater reliability) or test–retest (intra-rater), and σ2residual represented random error variance.28 The minimum detectable change (MDC) was a clinically useful measure for absolute reliability that estimated the true change versus the error change. It indicated how much change must occur in a measure with a given degree of random error, and with 95% certainty, to conclude that change was due to true change and not error change. MDC was calculated using the formula: 1.96×2×SEM.25 We interpreted ICC agreement values as follows: >0.80 as very good, 0.61–0.80 as good, 0.41–0.60 as moderate, 0.21–0.40 as fair, and <0.21 as poor. ICC agreement values (model 2.1.A) and 95% CI was calculated using ‘scale analysis,’ with a two-way random effect model and ‘absolute agreement.’
ResultsSixty-nine subjects (36 subjects with neck pain, 33 healthy subjects) participated in the study. The demographic characteristics are summarized in Table 1. All 33 healthy subjects completed the first and second assessment sessions, and 35 of the patients with neck pain completed the first and second assessment sessions. One subject dropped out of the study due to increased neck pain following the first assessment session and refused to continue.
Demographic characteristics of patients with neck pain and healthy subjects.
| Patients (n=36) | Healthy subjects (n=33) | p-Value for group difference | |
|---|---|---|---|
| Age (years) | 36 (14.8) | 56 (13.2) | <0.001 |
| Height (cm) | 174.8 (8.9) | 171.1 (9.2) | 0.546 |
| Weight (kg) | 72.6 (11.3) | 75.8 (13.5) | 0.475 |
| BMI (kg/m2) | 23.8 (3.2) | 25.9 (3.4) | 0.564 |
| VAS pain score (0–100mm) | 48.6 (21.3) | <0.001 | |
| NDI (0–50 score) | 17.2 (6.4) | <0.001 | |
| Education level | |||
| Elementary school, number | 2 | 12 | |
| High school, number | 14 | 10 | |
| Undergraduate, number | 16 | 7 | |
| Postgraduate and above, number | 4 | 4 | |
cm, centimeters; kg, kilogram; mm, millimeters; BMI, body mass index; VAS, visual analog scale; NDI, neck disability index. Elementary school=9–10 years of education, high school=10–12 years of education, Undergraduate=13–15 years of education, Postgraduate and above=>15 years of education, p values are based on 2-sample independent t-tests.
Intra-rater reliability of NHP and THP tests (examiner A and B) are summarized in Table 2. Intra-rater reliability for the NHP test showed good agreement with ICC values between 0.74 and 0.78. For THP tests, ICC values indicated good to very good agreement with ICC values between 0.64 and 0.83. For examiner A, the highest ICC values were found for neck flexion (0.82, 95% CI [0.71–0.89]) and neck rotation right (0.82, 95% CI [0.73–0.88]), with a 95% LOA measurement, ranging between −0.161 and 0.234 degrees (Table 2). Examiner B had the highest ICC values for neck rotation right (0.83 (95% CI [0.72–0.89]) and neck flexion (0.80 (95% CI [0.68–0.88]), with a 95% LOA measurement, ranging between −0.239 and 0.172 degrees. Bland–Altman plots showed that the differences between the two examiners were less than 2 degrees for neck flexion and neck right rotation and neck extension. The MDC ranged from 0.50 degrees (neck right rotation) to 1.88 degrees (neck extension), and SEM ranged from 0.55 degrees (neck right rotation) to 0.68 degrees (neck extension) (Table 2). Knowledge of specific MDC values can enable the therapist to better assess whether a true change in the patient's functional balance has occurred, and thus ensure quality-focused rehabilitation.
Intra-rater and inter-rater reliability of the NHP and THP tests.
| Intra-rater reliability | ||||||||
|---|---|---|---|---|---|---|---|---|
| ICC (Reliability) | 95% CI | Mean diff AB (SD diff AB) | σ2o | σ2 residual | SEM agreement | LOA | MDC | |
| Examiner A | ||||||||
| NHP | 0.78 | 0.65–0.86 | −0.10 (0.86) | 0.01 | 3.53 | 1.88 | −0.314 to 0.100 | 5.19 |
| THP into flexion | 0.82 | 0.71–0.89 | 0.03 (0.83) | 0.01 | 3.93 | 1.98 | −0.165 to 0.234 | 5.47 |
| THP into extension | 0.64 | 0.41–0.77 | −0.21 (0.97) | 0 | 2.62 | 1.61 | −0.256 to 0.212 | 4.44 |
| THP into SB right | 0.71 | 0.53–0.82 | −0.25 (0.87) | 0.03 | 2.79 | 1.67 | −0.467 to −0.048 | 4.61 |
| THP into SB left | 0.72 | 0.54–0.83 | −0.26 (0.83) | 0.03 | 2.71 | 1.65 | −0.465 to −0.620 | 4.55 |
| THP into rotation right | 0.82 | 0.73–0.88 | 0.03 (0.79) | 0 | 3.81 | 1.95 | −0.161 to 0.222 | 5.38 |
| THP into rotation left | 0.77 | 0.63–0.85 | −0.24 (1.18) | 0.02 | 4.21 | 2.05 | −0.530 to 0.375 | 5.66 |
| Examiner B | ||||||||
| NHP | 0.74 | 0.59–0.84 | 0.06 (0.89) | 0.02 | 3.16 | 1.78 | −0.146 to 0.282 | 4.91 |
| THP into flexion | 0.80 | 0.68–0.88 | −0.03 (0.85) | 0.01 | 3.77 | 1.94 | −0.239 to 0.172 | 5.36 |
| THP into extension | 0.70 | 0.52–0.81 | −0.02 (0.79) | 0 | 2.13 | 1.45 | −0.220 to 0.162 | 4.00 |
| THP into SB right | 0.72 | 0.54–0.82 | 0.19 (0.83) | 0.19 | 2.54 | 1.65 | −0.004 to 0.395 | 4.55 |
| THP into SB left | 0.74 | 0.56–0.83 | 0.17 (0.80) | 0.16 | 2.44 | 1.61 | −0.013 to 0.373 | 4.44 |
| THP into rotation right | 0.83 | 0.72–0.89 | 0.03 (0.79) | 0 | 4.08 | 2.01 | −0.293 to 0.107 | 5.55 |
| THP into rotation left | 0.71 | 0.53–0.82 | −0.24 (1.18) | 0.09 | 5.95 | 2.45 | −0.728 to 0.126 | 6.77 |
| Inter-rater reliability to first assessment | ||||||||
| NHP | 0.79 | 0.66–0.87 | 0.06 (0.89) | 0.10 | 3.41 | 1.87 | −0.146 to 0.282 | 5.16 |
| THP into flexion | 0.82 | 0.70–0.88 | 0.01 (0.83) | 0 | 3.81 | 1.95 | −0.195 to 0.204 | 5.38 |
| THP into extension | 0.62 | 0.39–0.76 | −0.13 (0.91) | 0 | 2.26 | 1.50 | −0.352 to 0.088 | 4.14 |
| THP into SB right | 0.69 | 0.49–0.81 | −0.29 (0.88) | 0.04 | 2.69 | 1.65 | −0.506 to −0.081 | 4.55 |
| THP into SB left | 0.67 | 0.46–0.79 | −0.29 (0.88) | 0.04 | 2.55 | 1.60 | −0.506 to −0.819 | 4.42 |
| THP into rotation right | 0.84 | 0.75–0.90 | 0.07 (0.79) | 0 | 4.08 | 2.01 | −0.119 to 0.264 | 1.52 |
| THP into rotation left | 0.76 | 0.43–0.82 | 0.04 (1.76) | 0 | 5.01 | 2.23 | −0.420 to 0.428 | 5.55 |
| Second assessment | ||||||||
| NHP | 0.74 | 0.59–0.84 | 0.06 (0.89) | 0 | 3.23 | 1.79 | −0.146 to 0.282 | 4.93 |
| THP into flexion | 0.81 | 0.69–0.88 | −0.06 (0.85) | 0 | 3.82 | 1.95 | −0.269 to 0.142 | 5.38 |
| THP into extension | 0.66 | 0.45–0.79 | −0.13 (0.90) | 0.01 | 2.42 | 1.55 | −0.511 to 0.086 | 4.28 |
| THP into SB right | 0.72 | 0.55–0.82 | 0.15 (0.84) | 0.01 | 2.60 | 1.61 | −0.043 to 0.362 | 4.44 |
| THP into SB left | 0.69 | 0.53–0.81 | 0.14 (0.82) | 0.01 | 2.50 | 1.58 | −0.053 to 0.343 | 4.36 |
| THP into rotation right | 0.82 | 0.70–0.88 | −0.05 (0.83) | 0 | 3.82 | 1.96 | −0.250 to 0.149 | 5.41 |
| THP into rotation left | 0.80 | 0.68–0.87 | −0.17 (0.88) | 0.01 | 4.10 | 2.02 | −0.389 to 0.035 | 5.58 |
NHP, neutral head position; THP, target head position; SB, side bending; 95% CI, 95% confidence interval; ICC agreement, intraclass correlation coefficients; Mean diff AB, mean difference between examiner A and B; SD diff AB, standard deviation of the mean difference between examiner A and B; σ2o, variance component of testers; σ2 residual, random error of variance; SEM, standard error of measurement; LOA, limits of agreement; MDC, minimal detectable change.
Inter-rater reliability results are summarized in Table 2. Overall, the inter-rater reliability for NHP showed good agreement with ICC values ranging between 0.74 and 0.79. For THP tests, inter-rater reliability (First Assessment) demonstrated good agreement with ICC values of 0.62 (95% CI [0.39–0.76]) for neck extension and 0.84 (95% CI [0.75–0.90]) for neck rotation right. Likewise, inter-rater reliability for the Second Assessment showed good agreement with ICC values of 0.66 (95% CI [0.45–0.79]) for neck extension and 0.81 (95% CI [0.69–0.88]) for neck flexion (Table 2). Overall, THP tests showed good agreement with ICC≥0.66. MDCs were between 1.52 and 1.77 degrees (Table 2). The mean differences between the examiners ranged from 0.01 degrees (SD=0.83) to 0.07 degrees (SD=0.79; Table 3). Bland–Altman plots showed that differences between the two examiners were less than 2 degrees for neck flexion and neck extension (Table 2).
Difference in scores between patients with neck pain and healthy controls.
| Patients (n=36) (Mean±SD) | Healthy subjects (n=33) (Mean±SD) | p-Value for group difference | |
|---|---|---|---|
| Examiner A – first assessment | |||
| NHP | 4.58±0.59 | 2.97±0.87 | <0.001 |
| THP into flexion | 4.80±0.61 | 3.01±0.86 | <0.001 |
| THP into extension | 4.93±0.86 | 3.91±0.77 | <0.001 |
| THP into SB right | 1.24±1.01 | 1.61±0.82 | 0.104 |
| THP into SB left | 1.24±1.01 | 1.64±0.78 | 0.073 |
| THP into rotation right | 4.80±0.61 | 3.03±0.84 | <0.001 |
| THP into rotation left | 4.54±1.27 | 2.47±1.30 | <0.001 |
| Examiner B – first assessment | |||
| NHP | 4.56±0.69 | 3.29±0.66 | <0.001 |
| THP into flexion | 4.56±0.69 | 3.26±0.68 | <0.001 |
| THP into extension | 5.02±0.67 | 4.09±0.58 | <0.001 |
| THP into SB right | 1.76±1.04 | 1.66±0.77 | 0.674 |
| THP into SB left | 1.76±1.04 | 1.70±0.72 | 0.802 |
| THP into rotation right | 4.56±0.69 | 3.13±0.76 | <0.001 |
| THP into rotation left | 4.48±1.00 | 2.52±1.40 | <0.001 |
| Examiner A – second assessment | |||
| NHP | 4.56±0.69 | 3.21±0.72 | <0.001 |
| THP into flexion | 4.56±0.69 | 3.19±0.70 | <0.001 |
| THP into extension | 5.01±0.69 | 3.87±0.76 | <0.001 |
| THP into SB right | 1.76±1.04 | 1.59±0.82 | 0.458 |
| THP into SB left | 1.76±1.04 | 1.63±0.77 | 0.569 |
| THP into rotation right | 4.56±0.69 | 3.22±0.65 | <0.001 |
| THP into rotation left | 4.56±0.69 | 2.96±0.63 | <0.001 |
| Examiner B – second assessment | |||
| NHP | 4.58±0.59 | 3.13±0.92 | <0.001 |
| THP into flexion | 4.80±0.61 | 3.07±0.92 | <0.001 |
| THP into extension | 5.12±0.62 | 4.04±0.75 | <0.001 |
| THP into SB right | 1.33±0.97 | 1.72±0.72 | 0.069 |
| THP into SB left | 1.33±0.97 | 1.79±0.65 | 0.027 |
| THP into rotation right | 4.80±0.61 | 3.07±0.92 | <0.001 |
| THP into rotation left | 4.80±0.61 | 3.07±0.92 | <0.001 |
NHP, neutral head position; THP, target head position; SB, side bending; p values are based on 2-sample independent t-tests.
An independent t-test was performed to compare mean scores between patients with neck pain and healthy subjects both for NHP and THP tests (Table 3). For NHP and THP, statistically significant differences were found in all of the movement directions, except for THP – side bending left and right. Patients with neck pain showed significantly larger repositioning errors than did healthy subjects (p<0.001; Table 3). Both examiners observed these significant differences.
DiscussionThis study assessed two aspects of neck proprioception (joint position sense), namely the repositioning of head to NHP and repositioning of the head to a THP, using an unsophisticated and inexpensive inclinometer device. Results revealed that both intra- and inter-rater reliability was high using the inclinometer as a measuring device both for the NHP and THP tests.
Intra-rater and inter-rater data in this study demonstrated good reliability, with good ICC, SEM, and MDC values. A plot of LOA between the two did not show any systematic bias. This is to be anticipated as both examiners used the same instructions with specific and rigid protocol; as such, examiners had little opportunity to influence the subject's performances. We also believe that both examiners had considerable experience in testing cervical position sense. Without such collaboration, the same results might not have been obtained.
Few studies report information on intraclass correlation coefficient (ICC) confidence intervals, statistical power, SEM, or MDC in order to establish intra-rater reliability for cervical proprioception both in NHP and THP measurements. Studies have reported a lack of reliable and valid tools with which to measure proprioception.22 Neck endurance and proprioception have been investigated to some extent.29 The results of this study agree with Van Blommestein et al.,30 who demonstrated excellent intra-rater reliability of the inclinometer, with a reported ICC of 0.96. A systematic review of the literature identified only six studies that assessed reliability in patients with cervical disorders, and of these, only two studies had more than 30 subjects.31 Of the six studies, very few used ICC statistics to establish reliability.32 Further, although many studies claim that range of motion devices are reliable, most have not been properly tested for reliability in terms of statistical techniques and sample size adequacy.32 Swait et al.33 concluded that the test–retest reliability was obtained with five or more trials using intraclass correlation coefficients (0.73–0.84) and cervicocephalic kinesthesia (ICC: 0.90–0.97) tests.
In the current study, the NHP and THP tests showed significantly larger errors in subjects with neck pain when compared to healthy individuals in almost all movement directions (flexion, extension, rotation right, and rotation left) except side bending right and left. There is some evidence that patients with chronic neck pain have neck muscle weakness compared to healthy control subjects.34 Treleaven et al.35 have reported significantly larger errors in extension and right rotation in subjects with whiplash compared to controls. This study presented similar findings; subjects with neck pain had significantly larger errors in extension and right rotation compared to healthy individuals. There is consistency in the literature regarding the limits between physiological proprioceptive variation and proprioceptive deficits. Some studies have reported that a threshold value of 4.58 degrees can be used to distinguish patients with neck pain from healthy subjects, with >80% certainty.36 The current study showed an average threshold value of 4.56 degrees in patients with neck pain. Kristjansson et al.37 showed a higher mean proprioceptive threshold of 6.5 degrees and 5.21 degrees for right and left rotation, respectively, in neck pain subjects. In contrast, two recent studies failed to show any significant differences between healthy subjects and patients with cervicogenic headache or non-traumatic neck pain in terms of kinesthetic acuity.18,38
The THP results indicated that the mean repositioning errors were larger in sagittal (flexion and extension) and transverse (right and left rotation) plane directions compared to frontal (side bending right and left) plane directions. Both examiners noted this difference both for neck pain patients and for healthy subjects. Based on the assumption that repositioning ability is determined by the function of muscle spindles of the contracting muscles,39 one might interpret the difference in different planes as the differences in the repositioning ability of the muscle groups used to perform movement in these directions.40,41
This study calculated ICC, SEM, and LOA in order to provide representation of different aspects of reproducibility (reliability and agreement); failure to do so has been a common criticism of previous studies.42 Unfortunately, our data collection procedure did not allow for analysis of consistent over-shooting or under-shooting of head position as a part of the observed outcome variability. A tendency for the subjects with neck pain to overshoot the target compared to healthy subjects was noticeable. Similar findings have been found in previous studies that evaluated cervical position sense in different cervical pathologies.17,43,44
LimitationsOnly NHP and THP absolute errors were recorded in this study – constant and variable errors were not considered. Examiners in the study have good expertise in the field of physical therapy and in examining cervical proprioception, therefore intra- and inter-rater reliability should reflect results of other professionals. If data are collected with inexperienced physical therapists, then the reliability values may change. In the present study, the patients were significantly older than were the healthy subjects.
ConclusionThe intra- and inter-rater reliability for the NHP and THP tests ranged from good to very good agreement, both in patients with neck pain and in healthy subjects. The clinimetric properties in this study were related to non-specific neck pain only; in other cervical pathologies, the quality of the performance of the actual measurements might differ.
Conflicts of interestThe authors declare no conflicts of interest.