There is a lack of standardized criteria for diagnosing rotator cuff related shoulder pain (RCRSP).
ObjectiveTo identify the most relevant clinical descriptors for diagnosing RCRSP.
MethodsA Delphi study was conducted through use of an international physical therapists expert panel. A 3-round Delphi survey involving an international panel of physical therapists experts with extensive clinical, teaching, and research experience was conducted. A search query was performed in Web of Science, along with a manual search, to find the experts. The first round was composed of items obtained from a previous pilot Delphi study along with new items proposed by the experts. Participants were asked to rate items across six clinical domains using a five-point Likert scale. An Aiken's Validity Index ≥ 0.7 was considered indicative of group consensus.
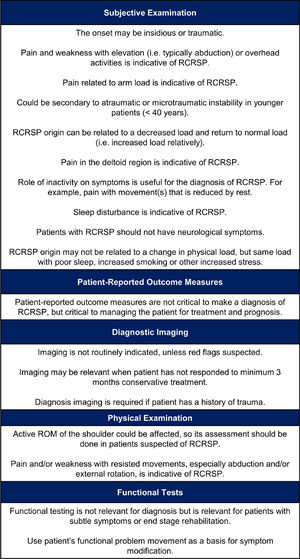
ResultsFifteen experts participated in the Delphi survey. After the three rounds, consensus was reached on 18 clinical descriptors: 10 items were included in the “subjective examination” domain, 1 item was included in the “patient-reported outcome measures” domain, 3 items in the “diagnostic examination” domain, 2 items in the “physical examination” domain”, and 2 items in the “functional tests” domain. No items reached consensus within the “special tests” domain. The reproduction of symptoms in relation to the application of load, the performance of overhead activities, and the need of active and resisted movement assessment were some of the results with greatest consensus.
ConclusionIn this Delphi study, a total of 18 clinical descriptors across six clinical domains were agreed upon for diagnosing RCRSP.
Shoulder pain is the third leading cause of musculoskeletal pain in primary care consultations.1–3 Incidence rates range from 14.7 to 29.3 per 1000 person-years2–4 with a lifetime prevalence that can reach up to 70% in the general population.5 Shoulder pain is common among people between 45 and 55 years old4 and, despite heterogeneity in the terms used to identify specific pathologies,6,7 the most frequent finding among patients with shoulder problems is pain originating from the rotator cuff and other subacromial structures.8,9
Historically, the term used to describe this condition was subacromial impingement syndrome.10 Findings from recent surgical research11 have challenged the basis for the acromion as the cause of the pathology leading to pain. In addition, research has shown that exercise therapy has the same short, medium, and long-term benefit as acromioplasty in combination with exercise therapy,12 further questioning impingement as the primary mechanism of symptoms.13 A series of clinical terms have emerged to actively move away from the flawed term impingement syndrome. These terms include, among others, subacromial pain syndrome,14,15 rotator cuff disease,16 and rotator cuff-related shoulder pain (RCRSP),13 that were introduced to move away from an incorrect pathoanatomical explanation for the presenting symptoms. Particularly, RCRSP was suggested as an overarching term that includes subacromial pain syndrome, subacromial impingement syndrome, rotator cuff tendinopathy, and subacromial bursitis.13 Non-traumatic RCRSP includes non-traumatic partial and full-thickness tears of the rotator cuff and traumatic RCRSP involves traumatic tears of these structures.13 This term was proposed aiming to reduce patients’ concerns related to aberrant acromial spurs causing symptoms and thus beliefs that surgery was needed for symptoms resolution. In this regard, there is recent evidence showing that diagnostic labels for shoulder pain may influence people's perceived need for surgery,17 as well as how patients can perceive the potential effectiveness of physical therapy.18 In particular, Zadro et al.17 found that the labels “rotator cuff tear” and “subacromial impingement syndrome” were those that most encouraged people to consider surgery. Interestingly, there was no significant difference in terms of considering surgery between these labels and the label “RCRSP”, so it is not clear that the use of this term solves the apparent problem.
The term RCRSP acknowledges that we currently don't know the underlying cause of the shoulder pain. It is one of many painful shoulder presentations which is characterized by pain and/or weakness most commonly experienced in shoulder elevation and external rotation, absence of referred pain (i.e. from cervical spine), and occurrence related with a change in shoulder loading behavior and potential changes in lifestyle.13,19 It is important to note that to establish a diagnosis of RCRSP, differential diagnosis with other clinical conditions such as shoulder instability or frozen shoulder syndrome should be made as their clinical presentation may sometimes be similar.20,21
Establishing a functional diagnosis is the primary objective within the professional practice of physical therapists22; this is often challenging in people with shoulder pain. The coexistence of multiple pathologies,23 the lack of reliability of orthopedic tests,24–27 the lack of direct association between imaging findings and clinical symptoms,9,28–30 as well as the possible implication of proximal segments31 make it very difficult to pinpoint the exact source of shoulder pain.
Regarding RCRSP diagnosis, no standardized diagnostic criteria are currently available.32 Some proposals for diagnosing RCRSP have been published,13,15,33,34 but in no study a strong enough methodology was used enabling the proposed diagnostic criteria to be accepted as universal for this clinical condition. This fact, added to the need to accurately differentiate RCRSP from other shoulder clinical conditions, justified the aim of this study which was therefore to identify the most relevant clinical descriptors for RCRSP based on the opinion of an international panel of experts with a high level of clinical, teaching, and research experience.
MethodsA three-round online Delphi survey was employed to obtain a consensus on which clinical descriptors are necessary and sufficient for RCRSP diagnosis. Clinical descriptors are defined as findings obtained throughout the examination and assessment processes that may guide the diagnosis of a clinical condition.35,36 Initially developed by Dalkey,37 the Delphi method is commonly used in health science research as a reliable way to reach a consensus on clinical issues.38,39 The Delphi method involves both a workgroup and a participant (respondent) group of experts.40 The study was approved by the Centro Superior de Estudios Universitarios La Salle Ethics Committee (ES) (CSEULS-PI-025/2020). The research was conducted according to the Declaration of Helsinki.
ParticipantsThe expert panel comprised physical therapists purposely selected based on their experience and knowledge in RCRSP.41,42 Only physical therapists were included in the study to make this study more relevant to physical therapy teaching, research, and practice. Additionally, trying to establish an acceptable diagnosis/label such as RCRSP may help patients to understand their problem and facilitate adherence to a treatment (i.e., exercise)18 that has been shown to be as effective as a surgical procedure.43 To assemble a representative group of experts, a list of inclusion criteria was established and the Web Of Science database was queried using a search of relevant terms related to the study topic (Supplementary File - Table 1). Additionally, a manual search was performed to verify that a series of additional experts proposed by the working group also met the inclusion criteria. The selection process is depicted in Fig. 1.
The working group consisted of five investigators, physical therapists (NRS, RFM, ELG, RLT, JTL), who were responsible for designing the survey and collecting and analysing the data from each round of questions.
ProcedureFor all three Delphi rounds, the experts received an invitation by email with a link to an online questionnaire. The experts had 3 weeks to complete each round, with reminders emailed weekly.
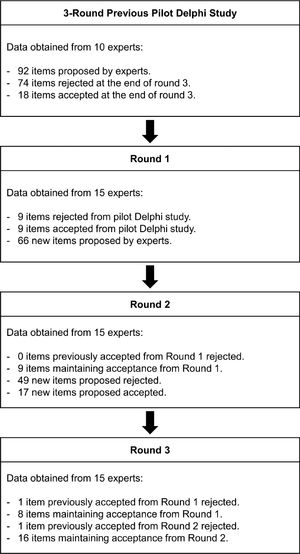
First, the expert panel was sent three documents via email: a letter inviting them to participate in the study, an informed consent document created by the working group, and a questionnaire. The first part of this questionnaire included a list of sociodemographic questions. The second part was composed of items structured into six domains (subjective examination, patient-reported outcome measures [PROMs]), diagnostic examination, physical examination, special tests, and functional tests) as described in a previous DELPHI study.36 These initial items were chosen after two members of the working group (ELG and JTL) carried out a three-round non-published pilot Delphi study (with the same methodology as stated below for the final Delphi study) with 10 shoulder experts from February to March 2019 (Table 1). The use of a previous pilot study has been reported in some DELPHI studies44,45 and it has been suggested that it could ensure greater rigor, especially regarding the design of the first round questions.46 For the first round of the current Delphi study, participants were asked to rate the items from the pilot study using a five-point Likert scale (Strongly Disagree, Disagree, Neutral, Agree, Strongly Agree). In addition, in this first round, experts were invited to add items to each of the six examination domains.
Clinical descriptors obtained in the previous pilot Delphi study.
RCRSP, rotator cuff related shoulder pain; ROM, range of motion.
The level of agreement among the experts was analysed by means of the Aiken's V coefficient of validity (V). This coefficient is used to quantify the content validity or relevance of an item with respect to a content domain evaluated by several experts’ judgement. Aiken's V is calculated as the ratio of the sum of agreement score obtained from all authors for a given item, with respect to the maximum possible score (i.e. maximum value of the Likert scale * number of experts rating that item). The value of Aiken's V ranges from 0 to 1, the latter representing perfect agreement. An Aiken's V ≥ 0.7 was considered reflective of group consensus, as recommended for Delphi studies.47
The second round of questions included items that reached at least a 0.7 validity index in the first round and the suggestions made by the expert panel members. No open-ended questions were included, and the experts were asked to indicate their degree of agreement with each proposed item using the previously mentioned five-point Likert scale.
For round 3, participants were informed of the results from round 2 using descriptive statistics and asked to reconsider their degree of agreement with each item before expressing their final opinion. Each participant was, therefore, asked to re-grade the criteria that reached consensus in round 2 using the same Likert-type scale.
Data analysisAll analyses were performed with statistical software R version 4.1.0 (R Core Team (2021). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/). Mean and standard deviation (SD) and absolute and relative frequencies were used for the descriptive analyses of the continuous and nominal variables, respectively. The agreement between experts was analysed using the Aiken's Validity Index (Aiken's V), an agreement index for ordinal data with scores ranging from 0 (no agreement) to 1 (perfect agreement).48
ResultsAfter three consecutive rounds, conducted between March and May 2020, a consensus was reached among experts across the six initially proposed examination domains.
Expert panel resultsFor the first round, 56 physical therapists who were experts in the study topic were selected using the inclusion criteria, and 29 participants responded to the initial email. Of the 29 respondents, 14 declined to participate in the study for different reasons (most common: not having enough time) and 15 (26.78%) completed the three rounds of questions. The final expert panel consisted of 15 physical therapists from diverse work fields (research, clinical practice, education, or mixed). The group had an average ± standard deviation of 23.3 ± 8.1 years of experience with RCRSP and an average of 24.9 ± 17.3 scientific publications related to shoulder pain. Demographic information for the expert panel members is provided in Table 2.
Characteristics of the Delphi participants.
*Mean ± standard deviation or frequency; RCRSP, Rotator Cuff Related Shoulder Pain; pro bono, services to those who are unable to afford them.
At the end of the three rounds, a total of 24 RCRSP-related items were obtained (Supplementary File -Table 2). They were distributed amongst the six diagnostic domains as follows: subjective examination (n = 11), PROMs (n = 1), diagnostic examination (n = 4), physical examination (n = 6), and functional tests (n = 2). No items reached consensus within the “special tests” diagnostic domain. Two items from the "subjective examination" were merged (“Pain with movement of the arm – typically abduction or overhead activities is indicative of RCRSP” and “Pain and weakness with elevation or overhead activities are indicative of RCRSP“) and one from "diagnostic examination" (“Diagnosis imaging is required if the patient has a history of trauma”) was eliminated after reaching consensus among the working group because it was highly similar to another item. A total of 22 clinical descriptors for diagnosing RCRSP were obtained. However, some were unified and grammatically edited by the working team to simplify understanding, leaving a total of 18 items (Fig. 2). The original items of Round 3 without unification or editing are presented in Supplementary File - Table 2.
Overall, 44.4% (8/18) of the items from the initial Delphi pilot study remained at the end of the third round and 92.31% (24/26) of the items that reached consensus in round 2 remained in round 3. The complete item selection process is represented in Fig. 3.
Subjective examinationIn round 1, 20% (1/5) of the items from the initial pilot study did not reach the Aiken's V required for consensus (Supplementary File - Table 3). The experts proposed 18 additional items (Supplementary File - Table 4). In round 2, 10 items were discarded and a total of 12 items (54.6%) were kept for round 3 (Supplementary File - Table 5), where 91.6% (11/12) reached consensus (Supplementary File - Table 2).
Patient-reported outcomes measuresThe one item from the pilot study did not reach the necessary degree of consensus (Supplementary File - Table 3) and seven new items were proposed by the respondent group (Supplementary File - Table 4). In the second round, only one item (14.3%) reached consensus (Supplementary File - Table 5), which was also maintained at the end of round 3 (Supplementary File - Table 2).
Diagnostic examinationIn round 1, 50% of the items from the pilot study (1/2) did not reach sufficient consensus (Supplementary File - Table 3) and experts proposed 12 additional items (Supplementary File - Table 4). In the second round, 30.7% of the items (4/13) reached consensus (Supplementary File - Table 5); these four items maintained the consensus among the experts at the end of round 3 (Supplementary File - Table 2).
Physical examinationOf the nine initial items proposed, five (44.4%) did not reach consensus in round 1 (Supplementary File - Table 3). Ten more items were proposed by the experts (Supplementary File - Table 4). From round 2, 42.9% (6/14) of the items continued to round 3 (Supplementary File - Table 5) and remained at the end of the study (Supplementary File - Table 2).
Special testsThe single initially proposed item did not reach the necessary level of consensus (Supplementary File - Table 3). Ten items were proposed by experts in this first round (Supplementary File - Table 4). In round 2, only one item (10%) reached consensus (Supplementary File - Table 5) but failed to do so at the end of the third round (Supplementary File - Table 2).
Functional testsNo items were included from the pilot study in this diagnostic domain. However, the experts proposed nine items in round 1 (Supplementary File - Table 4) of which two (22.2%) earned Aiken's V scores sufficient for consensus in round 2 (Supplementary File - Table 5). These same two items remained at the end of round 3 (Supplementary File - Table 2).
DiscussionThe objective of this study was to obtain a consensus on the most relevant diagnostic criteria for RCRSP. A total of 18 clinical descriptors across six domains were identified using the Delphi method. This approach is proven valid for obtaining expert opinions on a given topic and is widely used in health science research.40,42,49 The Delphi method has three important features: anonymity, controlled feedback, and statistical group response.37,50
Respondent group characteristicsThe respondent group included 15 experts. There is currently no consensus on the ideal sample for a panel of experts with some authors recommending a minimum of 15,51 10,52 or even seven members.53 The quality of the panel of experts seems to be more important than the number when judging the level of representativeness of the results obtained in a Delphi study.49,54 Additionally, the criteria for defining an expert within a Delphi study are not clearly established.55 Levels of knowledge and professional experience have been proposed as main criteria.55 After analysing the characteristics of the panel members, their years of clinical experience treating people with RCRSP (23.3 ± 8.1), the number of scientific publications in a topic related to shoulder pain (24.9 ± 17.3), and the percentage of experts with PhD as the highest professional degree (80%), the quality of the panel of experts of this Delphi study seems high. This fact is important when considering the results.
Subjective examinationThe subjective examination is such a fundamental part of a physical therapist assessment that 75 to 83% of diagnostic decisions are reached based on its results.56,57
Pain related to mechanical load emerged as one of the main descriptors indicative of RCRSP in the subjective examination domain. Although the origin of RCRSP is multifactorial,13 poor load management (e.g., excessive loading, alterations to regular loading on subacromial structures) seems to be the most determining causal factor58 and plays a critical role in its progression.59 Furthermore, although the nociceptive sources of RCRSP are not only tendinous,13,23 it seems likely that the pain behavior in RCRSP is similar to that described for tendinopathies (e.g., on/off pain behavior dependent on the amount of load applied).60 A clear evidence of the influence of mechanical load on the genesis of RCRSP is that this condition is related to the performance of activities involving load in shoulder elevation,61–63 and is more prevalent on the dominant side, in active, working populations61 and overhead sports.64,65 In addition, RCRSP is more prevalent in individuals who have performed overhead activities for a long time.66–69
Regarding the location of the pain, the experts agreed that the most frequent area reported by those with RCRSP is the deltoid region, which is in line with a previous consensus report34 and experimental pain models.70 Pain reaching the forearm has also been reported in people with RCRSP.71 To the authors’ knowledge, the utility of pain distribution (e.g., using pain drawings) to assist with the differential diagnosis of shoulder pain has not fully been investigated. As experimental pain models have considerable limitations as models for clinical shoulder pain,72 future research may focus on exploring differences between patients in terms of clinical pain distribution.
Another item obtained by consensus was that RCRSP affects sleep. The relationship between the presence of shoulder pathology and sleep disturbances has been already established in other studies.73,74 Overall, aspects related to a patient's lifestyle such as sleep quality can be relevant in people with musculoskeletal pain.75,76 For example, according to the majority of the studies, sleep deprivation produces hyperalgesic changes.77 Furthermore, poor sleep can compromise the physiological processes underlying tendon recovery.78 Sleep disturbances are frequently associated with anxiety and depression, which highlights the value of performing a psychological evaluation in people with RCRSP.79,80 Also, there seems to be a dose and time-dependent relationship between tobacco consumption and the appearance of pathological changes in the rotator cuff,81 shoulder pain, and rotator cuff tear size.82 Other lifestyle-related factors (e.g., body mass index, alcohol consumption, and comorbidities like diabetes) may also be related to the development of RCRSP.66,83–85
The most frequent age of RCRSP onset related to tendon changes is between 45 and 55 years old.4 As such, being older than 50 years is a significant factor for developing rotator cuff tendinopathy among active populations.66 Moreover, being over 60 years old is a risk factor for rotator cuff tears.86 However, the item “age typically over 40″ did not reach consensus in the last round of questions (Supplementary file - Table 2). Rotator cuff disorders can appear in a wide age spectrum. Some authors even consider “two different rotator cuff diseases,” differentiating between patients under 40 years old with rotator cuff tendinopathy and older adults suffering from full-thickness tears.87 The main differences between these two populations are the potential for tissue healing, etiology, activity levels, physical demands and long-term expectations of recovery.87
Regarding age, the item “Could be secondary to atraumatic or microtraumatic instability in younger patients (< 40 years)” also reached consensus. It seems that in young people the development of rotator cuff tears may have a traumatic or atraumatic origin, this latter typical of overhead sports in the context of shoulder “microinstability.”87,88 The concept of shoulder microinstability is used to describe excessive laxity of the anterior capsule secondary to repeated movements of shoulder abduction and external rotation (i.e. overhead sports) which leads to abnormal glenohumeral biomechanics and internal shoulder impingement.89 The role of shoulder microinstability in the development of rotator cuff disorders is however controversial and some authors even consider that excessive laxity of the shoulder may act as a protective mechanism for avoiding impingement.90
The absence of neurological symptoms was reported by experts to be indicative of RCRSP, which agrees with a previous consensus report.34 Collecting sufficient data during the subjective examination can help to rule out a neurological component to the generation of symptoms.91
Patient-reported outcome measures (PROMs)There are several PROMs for assessing shoulder pain and function, such as the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire, the quick DASH, the Shoulder Pain and Disability Index (SPADI), the Constant (Murley) Score (CS), and the American Shoulder and Elbow Surgeons (ASES).92,93 Some questionnaires including the Rotator Cuff-Quality Of Life and the Western Ontario Rotator Cuff (WORC) index have been developed specifically for people with RCRSP.94 In the current Delphi study, PROMs were considered useful for guiding treatment and prognosis but not to make a diagnosis of RCRSP.95 Shoulder pain questionnaires have demonstrated to be valid, reliable, and responsive to changes93,96,97 but some are not specific to the shoulder joint (i.e., DASH) and few are specific to RCRSP.94
Diagnostic imagingDiagnostic imaging was considered necessary for people with RCRSP in three situations: red flags, history of trauma, and lack of response to a minimum of 3 months of conservative treatment. Imaging is widely used in medical practice for diagnosing patients with musculoskeletal pain.98–100 In people with RCRSP, magnetic resonance and ultrasound imaging have proven to be valid for diagnosing massive rotator cuff tears, with comparable levels of sensitivity and specificity.101,102 However, their sensitivity decreases with less extensive rotator cuff lesions.101,103,104 Furthermore, there is still controversy about the utility of imaging for guiding clinical decisions in people with shoulder pain including RCRSP, because it correlates poorly with symptoms.9,28,29,105 In patients with shoulder pain, it is difficult to identify the exact structure responsible for the symptomology due to the coexistence of multiple tissue alterations.32,106 However, radiological examination can help to rule out red flags.34 Finally, if we accept that exercise is key in the management of RCRSP107 and a minimum of 12 weeks is recommended to determine whether the results thereof are satisfactory,34,108 it follows that radiological examination be requested only after a lack of response to a minimum 3 months of exercise.
Physical examinationThere was consensus amongst the experts that pain with resisted movements, in particular in shoulder abduction and external rotation, is indicative of RCRSP. This finding is described by others,13,34,109 which together suggests that pain with resisted movements is key for diagnosing RCRSP. Depending on the stage of pathology in which the patient with RCRSP is58 and the level of tissue sensitization23,110 pain could probably be reproduced with other resisted movements (i.e., resisted flexion).
Assessment of muscle strength was reported as necessary for suspected RCRSP. In fact, RCRSP has also been called "weak and painful shoulder".21,34 Subacromial pain induces alterations in the electromyographic activity of shoulder musculature and its ability to produce strength.111–114 Although deficits in shoulder abduction and external and internal rotation strength have been described in those with RCRSP,115–117 there is conflicting evidence.118
Special testsNo special tests achieved the level for consensus at round 3 required to become a relevant clinical descriptor for RCRSP diagnosis. This finding is consistent with the current literature questioning the usefulness of orthopedic tests in the diagnosis of shoulder pain.24–26 Most orthopedic tests used for diagnosing shoulder pain,24–26 including RCRSP,119–122 have low diagnostic accuracy. This is likely due to the inability to isolate and specifically stress one single anatomic structure with any special test,13 the coexistence of several altered anatomical structures,23,123 and potential changes in the mechanosensitivity of local tissues.110 Therefore, currently, it is recommended to stop teaching and using special tests to establish the origin of shoulder pain.27
Interestingly, the item "depending on the condition some tests may be needed" was very close to reaching consensus in the final round (Aiken's V = 0.68). Some special tests and test clusters have been shown, for example, to improve the clinical diagnostic process for arriving at a pathology-based diagnosis in people with shoulder pain.124 In our opinion, such tests should be a component of a bigger picture, not a standalone diagnostic tool and are likely to be more useful for detecting full-thickness rotator cuff tears.
Functional testsPerformance-based functional tests are performed by clinicians in an attempt to quantify and discriminate impairments in patient's body functions.125 Several upper-extremity functional tests have been described and evaluated in the shoulder region both at rehabilitation and injury-prevention settings126 and their psychometric properties have been recently summarized.125
Experts considered functional tests to be relevant for patients with RCRSP reporting subtle symptoms or at end-stage rehabilitation. However, no functional test in isolation reached a sufficient level of consensus to be useful for diagnosing RCRSP. Based on these results, functional tests may then be useful for assessing people with RCRSP with low levels of irritability.127 Functional testing was also considered useful by experts as a basis for symptom modification. Symptom modification procedures based in part on symptom reproduction with patient-specific functional movements have been recommended for assessing people with RCRSP.128
As a final consideration, the diagnosis of RCRSP is, to a certain extent, a diagnosis by exclusion. This implies that other conditions must be ruled out before accepting a diagnosis of RCRSP as valid. Interestingly, experts did not reach consensus, for example, on screening the cervical spine129 or assessing passive shoulder movements130 to determine the involvement of the cervical spine as a source of pain contribution or exclude a frozen shoulder, respectively. The absence of distal neurovascular symptoms is another parameter that should be taken into account when excluding other pathologies.131
Research strengths and limitationsThis study involved a highly experienced panel of experts who were chosen using a systematic search strategy to avoid excessive selection bias. Furthermore, the preliminary pilot study likely strengthens the validity of the final results. On the other hand, the low response rate in the initial round (26.8%) might represent a limitation when considering the external validity of the proposed descriptors. Secondly, the decision of including only physical therapists in this study could consequently affect the external validity of the diagnostic criteria across other health professionals who manage shoulder pain (e.g. general practitioners, rheumatologists, sports doctors, orthopedic surgeons). Further studies are needed to validate the proposed clinical descriptors across other health professions.
ConclusionsThis is the first Delphi study to our knowledge to establish a standardized consensus among physical therapists on diagnostic criteria for RCRSP. A total of 18 clinical descriptors across six examination domains were obtained for diagnosing RCRSP. The results of this study could be useful to standardize the diagnosis of this condition both in clinical and research settings. In addition, this would help to improve the management and outcome of patients with RCRSP. The clinical descriptors obtained here should be reviewed and updated regularly to reflect developments in diagnostically relevant technology and clinical information.
FundingThis research received no funding.
The authors would like to thank the experts for their effort in participating in the study.