There is no evidence whether kinesiophobia affects women and men with femoroacetabular impingement (FAI) syndrome differently.
ObjectiveTo explore the association between kinesiophobia, quality of life (QoL), pain, and physical function in people with FAI syndrome, and to compare the level of kinesiophobia between women and men with FAI syndrome.
MethodsOne-hundred-fifty participants with FAI syndrome (51% women) completed assessment of the following: kinesiophobia with the Tampa Scale for Kinesiophobia; patient reported outcome measures (PROMs) (pain, physical function, health- and hip-related QoL); physical function (side bridge, hop for distance, and one leg rise); and active hip range of motion (flexion, external rotation, internal rotation).
ResultsGreater kinesiophobia was correlated with worse hip-related QoL (rho=-0.58; p<0.001), self-reported physical function (rho=-0.42; p<0.001), health-related QoL (rho=-0.46; p<0.001), and pain levels (rho=-0.46; p<0.001). In women, kinesiophobia was also associated with worse physical function (hop for distance r=-0.38; p=0.001 and side bridge rho=-0.24; p=0.036) explaining 36% of the variation of the hip-related QoL, 29% of the health-related QoL, and 27% of the self-reported physical function. In men, kinesiophobia explained 35%, 12%, and 10%, respectively.
ConclusionIn people with FAI syndrome, greater kinesiophobia was associated with worse PROMs, but not with hip range of motion. No sex-related differences in mean kinesiophobia scores were found. In women, an association was found between kinesiophobia and worse performance in physical tests. These findings might indicate that kinesiophobia plays a more important role in the clinical presentation of women with FAI syndrome than men.
Femoroacetabular impingement (FAI) syndrome is a common cause of hip-related pain in young and middle-aged active adults.1,2 FAI syndrome is defined as a motion-related clinical disorder of the hip, with a triad of symptoms, clinical signs, and imaging findings.3 It refers to possible premature contact between the femoral head-neck junction and acetabulum and acetabular labrum.3 Cam morphology may overload the femoroacetabular joint during functional movements in the position of hip impingement leading to pain, articular cartilage damage,3 and increased risk of developing hip osteoarthritis later in life.3,4
Altered psychological factors have been found in several persistent musculoskeletal conditions linked to poor condition-specific outcomes and quality of life.5-9 Pain is often perceived as a threat of body damage in people with persistent musculoskeletal conditions, which may trigger kinesiophobia, defined as an excessive, irrational, and debilitating fear of physical movement and activity resulting from a feeling of vulnerability to painful injury or (re)injury.10,11 A recent cross-sectional study12 demonstrated the presence of kinesiophobia and pain catastrophising in people with FAI syndrome.
There is evidence suggesting that men with persistent musculoskeletal pain have higher levels of kinesiophobia than women and that both, kinesiophobia and sex, are predictors of lower physical function.13-16 In people with FAI syndrome, higher kinesiophobia seems to be associated with lower physical function.12 However, women with FAI syndrome have more prominent impaired physical function and are more likely to undergo surgery than men.17,18 These findings raise the questions: (i) do women with FAI syndrome have higher levels of kinesiophobia than men?; and (ii) does kinesiophobia affect women and men differently? A better understanding of whether high levels of kinesiophobia impact people with FAI syndrome, and if there are sex-related differences, may help to inform tailored intervention strategies. The aims of our study were to (i) explore the association of kinesiophobia with hip- and health-related self-reported quality of life, pain, and physical function in people with FAI syndrome, and (ii) compare the level of kinesiophobia between women and men with FAI syndrome. We hypothesised that women with FAI syndrome have higher levels of kinesiophobia than men and that greater kinesiophobia are related to lower hip- and health-related self-reported quality of life, physical function, and greater pain.
MethodsThis cross-sectional observational study is reported according to STROBE (The Strengthening the Reporting of Observational Studies in Epidemiology) recommendations.19 The data used in this study are from a larger clinical trial20 approved by the La Trobe University Human Research Ethics Committee (approval number 17-080).
One-hundred-fifty participants were recruited via advertisements in clinic waiting rooms, gyms, sporting clubs, and on social media. Participants between 18 to 50 years of age with a history of hip-related (anterior hip or groin) pain greater than 3/10 on a numerical pain scale for at least 6 weeks aggravated by prolonged sitting or hip movements into positions of impingement and a positive flexion-adduction-internal rotation (FADIR) test were included if their radiological exams confirmed the presence of cam morphology (alpha angle of 60o or greater on either anterior/posterior pelvic or Dunn 45o hip radiographs).3,20-22 Potential participants who (i) had received physical therapy treatment in the past 3 months, (ii) had previous hip or back surgery, (iii) had other musculoskeletal conditions, (iv) presented moderate to severe hip osteoarthritis,23 or (v) had contraindications to radiographs were excluded.
Included participants completed written, informed consent, then provided demographic data (age, height, weight, body mass index (BMI)). The participants completed the following PROMs using the online platform PROmptus-Research (Promptus, Melbourne, Australia) and physical tests.
PROMsTampa Scale for Kinesiophobia (TSK) consists of 17 statements that measure fear of movement and (re)injury due to movement and physical activity in people with chronic musculoskeletal pain.24 Each statement is answered on a 4-point Likert scale scored from 1 to 4, and total scores range from 17 to 68, with a higher score indicating more fear of movement. The TSK demonstrates good test-retest reliability and validity when tested in people with chronic musculoskeletal pain.25
The Copenhagen Hip and Groin Outcome Score (HAGOS) consists of six subscales that measure pain, symptoms, physical function in daily living, physical function in sport and recreation, participation in physical activities, and hip and/or groin-related quality of life. Each item is answered on a 5-point Likert scale scored from 0 to 4, and each of the HAGOS subscales are scored out of 100 points (with higher score indicating no hip/groin problem). The HAGOS has acceptable reliability and validity in young people with hip and groin pain.26,27
Workplace Activity Limitations Scale (WALS) consists of 12 items that measure the degree of difficulty with various job-related tasks such as mobility, prolonged sitting and standing, lifting, bending, or kneeling. Each item is answered on a 4-point Likert scale scored from 0 to 3, and total scored range from 0 to 36 with higher score indicating greater workplace activity limitations. The WALS demonstrates good reliability and validity when tested in people with chronic conditions such as osteoarthritis and rheumatoid arthritis.28,29
5-Level EuroQol group's 5-Dimension (EQ-5D-5L) was used as a measurement of health-related quality of life and consists of five dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Each dimension has five severity levels ranging from “no problems” to “extreme problems.” The EQ-5D-5L has acceptable reliability and validity in people with chronic musculoskeletal conditions.30 The EQ-5D-5L index was calculated using a United Kingdom valuation set31 and used with permission from the EuroQol Research Foundation.
Functional physical testsBefore each functional physical test, participants performed a practice trial to allow familiarization with the test and environment. All physical tests were performed on the most affected side.
Side-bridge test of trunk endurance consisted of participants laying on their sides with one leg resting directly on top of the other. Participants were instructed to support their weight through their foot and their forearm lifting their hips off the mat to maintain a straight line over their full body length. This position was held for as long as possible. The time (seconds) was recorded from the start of the test until the participant's hips touch the exercise mat or was not able to maintain a straight line over their full body length. Participants were not provided with verbal feedback during testing procedures.32-34
Single-leg hop for distance test is a clinical test aimed to assess hopping performance in people with lower limb injury. The participants were asked to stand barefoot on a starting line, weight bearing on a single leg with both hands held behind their back and were instructed to hop as far forward as possible, landing on the same foot. The distance was recorded from the starting line to the posterior aspect of the heel of the landing foot. The test was performed three times with the greatest distance for each leg recorded.22,32,35
One-leg rise test involves standing and sitting from a plinth with only one foot on the ground. The height of the plinth was adjusted to achieve 90o of knee flexion. The participants were asked to perform as many repetitions of sit-stand-sit movements as possible at a constant self-selected speed. One foot remained on the floor in a self-chosen position and arms crossed on their chest.22,35,36 The test stopped when the participant failed (if the contralateral non-weight bearing leg/foot touch the ground or if they stopped rising) or when the participant achieved 50 repetitions.37
Active range of motion (ROM) tests were performed using an inclinometer for hip flexion and a goniometer for hip internal and external rotation. Active hip flexion was examined with the participant in a supine position. Internal and external rotation with 90o of hip flexion were examined with the participant in a sitting position. The participants were instructed to move as far as was comfortable and report any pain experienced in the hip/groin area. Each test was performed three times and the average was recorded.38
Statistical analysisStatistical analyses were performed using SPSS version 26 software (IBM, SPSS inc., Chicago, Il). Significance was set at p < 0.05 a priori. The Kolmogorov-Smirnov test was performed to test the normality of the continuous variables. The normally distributed variables were presented as mean ± standard deviation and the non-normally distributed were presented as median [interquartile range]. The Pearson correlation coefficient (r) and the Spearman's rank correlation coefficient (rho) were used to explore the association between all normally and non-normally distributed outcomes, respectively. To guide interpretation of the strength of correlations identified, values from 0.00 to 0.25 were considered poor, 0.25 to 0.50 were considered fair, 0.50 to 0.75 were considered moderate, and 0.75 to 1.00 were considered excellent.39 When at least fair correlations were found, linear regression models were used to explore the percentage of variation of the dependent variables explained by the independent variable (kinesiophobia).40 As increased age and high BMI are predictors of poor outcome in people with FAI syndrome,41,42 we used the hierarchical regression method including age and BMI in the first step and kinesiophobia in the second step as independent variables. All models were tested for the main assumptions. The linearity and homoscedasticity were assessed by analysing the graphs of standardized predicted value against standardized residuals. The independent errors assumption was tested with the Durbin-Watson test. The normally distributed errors were assessed by analysing the histograms of the residuals and examining the casewise diagnostics. The multicollinearity assumption was assessed by analysing the variance proportions distributed across different eigenvalues, the VIF and tolerance statistics.43 The R square change, F change and B (95% confidence interval) were presented.
ResultsThe characteristics of all participants are presented in Table 1. Six (4%) participants had bilateral FAI syndrome. The Tampa Scale for Kinesiophobia ranged from 20 to 53 considering all participants, from 26 to 53 considering only the women, and from 20 to 51 considering only the men participants.
Characteristics of the participants.
| All participants (n=150) | Women (n=76) | Men (n=74) | |
|---|---|---|---|
| Age (years) | 37 [14]† | 39 ± 14 | 34 [17]† |
| Height (m) | 1.73 ± 0.10 | 1.66 ± 0.07 | 1.78 [0.10]† |
| Weight (kg) | 74.00 [22.50]† | 65.20 [16.40]† | 83.84 ± 14.15 |
| BMI (kg/m2) | 24.49 [5.61]† | 23.34 [6.15]† | 25.00 [5.12]† |
| Patient reported outcome measures | |||
| Kinesiophobia | 38.54 ± 6.08 | 37.59 ± 6.40 | 39.52 ± 5.61 |
| HAGOS pain | 62.50 [20.00]† | 63.45 ± 17.31 | 62.50 [16.9]† |
| HAGOS symptoms | 55.36 [21.43]† | 54.97 ± 15.39 | 53.13 ± 14.88 |
| HAGOS physical function / daily living | 70.00 [25.00]† | 75.00 [30.00]† | 68.89 ± 17.31 |
| HAGOS sport / recreation | 59.33 ± 20.39 | 61.44 ± 21.61 | 57.16 ± 18.96 |
| HAGOS physical activity | 37.50 [37.50]† | 43.75 [40.60]† | 37.50 [37.50]† |
| HAGOS quality of life | 45.00 [21.00]† | 44.66 ± 17.03 | 45.00 [15.00]† |
| Workplace activity limitations | 5.00 [5.00]† | 5.00 [5.00]† | 5.00 [5.00]† |
| Health-related quality of life | 0.68 [0.16]† | 0.71 [0.21]† | 0.65 [0.11]† |
| Physical function | |||
| Side bridge (seconds) | 51.13 ± 30.74 | 40.00 [41.00]† | 59.16 ± 30.52 |
| Single leg hop for distance (m) | 1.02 ± 0.35 | 0.85 ± 0.28 | 1.20 ± 0.34 |
| One leg rise (repetitions) | 21 [29]† | 22 ± 16 | 25 [37]† |
| Range of motion | |||
| Hip flexion (degrees) | 114 ± 14 | 117 ± 15 | 112 [17]† |
| Hip external rotation (degrees) | 33 ± 8 | 33 ± 8 | 33 ± 8 |
| Hip internal rotation (degrees) | 29 ± 9 | 31 ± 8 | 27 ± 9 |
BMI – Body Mass Index. Tampa Scale for Kinesiophobia total scores range from 17 to 68, with higher score indicating more kinesiophobia. HAGOS (Copenhagen Hip and Groin Outcome Score) subscales are scored out of 100 points (with higher score indicating no hip/groin problem). Workplace activity limitations total scores range from 0 to 36 with higher score indicating greater workplace activity limitations. Health-related quality of life (EQ-5D-5L) index scores range from −0.224 to 1, with higher score indicating better quality of life.
For all participants, greater kinesiophobia demonstrated correlations with all other PROMs (Table 2). In women greater kinesiophobia correlated with worse performance of side bridge and single leg hop for distance (Table 2). The linear regression model adjusted for age, sex, and BMI indicated kinesiophobia significantly explained the variance of hip-related quality of life (R2 = 0.35; B (95% CI) = -1.54 (-1.89, -1.19)); physical activity (R2 = 0.22; B (95% CI) = -2.13 (-2.80, -1.46)); workplace activity limitations (R2 = 0.22; B (95% CI) = 0.31 (0.21, 0.41)); health-related quality of life (R2 = 0.20; B (95% CI) = -0.01 (-0.02, -0.01)); physical function (R2 = 0.19; B (95% CI) = -1.33 (-1.78, -0.88)); pain (R2 = 0.17; B (95% CI) = -1.07 (-1.46, -0.68)); symptoms (R2 = 0.16; B (95% CI) = -0.99 (-1.38, -0.61)); and sport/recreation (R2 = 0.15; B (95% CI) = -1.29 (-1.80, -0.77)).
Correlations between kinesiophobia and other outcome measures. The correlation coefficients are presented for all participants (n=150), women (n=76), and men (n=74).
| All participants | Women | Men | |
|---|---|---|---|
| Patient reported outcome measures | |||
| HAGOS pain | -0.43†* | -0.42* | -0.40†* |
| HAGOS symptoms | -0.38†* | -0.42* | -0.38* |
| HAGOS physical function / daily living | -0.42†* | -0.50†* | -0.33* |
| HAGOS sport / recreation | -0.39* | -0.41* | -0.35* |
| HAGOS physical activity | -0.44†* | -0.48†* | -0.39†* |
| HAGOS quality of life | -0.58†* | -0.60* | -0.58†* |
| Workplace activity limitations | 0.43†* | 0.46†* | 0.40†* |
| Health-related quality of life | -0.46†* | -0.50†* | -0.37†* |
| Physical function | |||
| Side bridge | -0.14 | -0.24†* | -0.18 |
| Single leg hop for distance | -0.09 | -0.38* | -0.02 |
| One leg raise | -0.14† | -0.21 | -0.13† |
| Range of motion | |||
| Hip flexion | -0.10 | 0.07 | -0.07† |
| Hip external rotation | -0.09 | 0.10 | -0.19 |
| Hip internal rotation | 0.09 | 0.09 | 0.12 |
HAGOS – Copenhagen Hip and Groin Outcome Score.
There was no sex-related difference for kinesiophobia (mean difference = 1.85; 95% CI = -0.10, 3.81). However, for women, greater kinesiophobia demonstrated moderate correlation with lower physical function, hip-related quality of life, and health-related quality of life (correlation coefficients from -0.60 to -0.50); fair correlation with greater pain (lower values in the HAGOS pain subscale), greater symptoms (lower values in the HAGOS symptoms subscale), greater workplace activity limitations, lower physical activity, and sports/recreation, lower single leg hop for distance (correlation coefficients from -0.48 to -0.38); poor correlation with lower side bridge (correlation coefficient of -0.24) (Table 2).
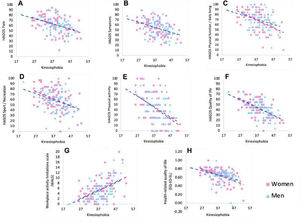
For men, greater kinesiophobia demonstrated moderate correlation with lower hip-related quality of life (correlation coefficient of -0.53); fair correlation with greater pain, greater workplace activity limitations, lower physical activity, health-related quality of life, greater symptoms, lower physical function, and lower sports/recreation (correlation coefficients from -0.48 to -0.38) (Table 2). Fig. 1 represents the correlations between kinesiophobia and the other PROMs for women and men.
Kinesiophobia explained 36% of the variation of the hip-related quality of life, 29% of the health-related quality of life, 27% of the physical function, 25% of the physical activity, 24% of the workplace activity limitations and less than 20% of the variation of pain, symptoms, sport/recreation, and single leg hop for distance in women with FAI syndrome (Table 3).
Linear Regression models, adjusted for age and BMI, exploring the percentage of variation of the dependent variables explained by the independent variable (kinesiophobia) for women with femoroacetabular impingement syndrome.
| Dependent variable | R2 | F | B (95% CI) |
|---|---|---|---|
| HAGOS quality of life | 0.36 | 41.22 | -1.60 (-2.09, -1.10) |
| Health-related quality of life | 0.29 | 28.41 | -0.01 (-0.02, -0.01) |
| HAGOS physical function / daily living | 0.27 | 26.05 | -1.59 (-2.21, -0.97) |
| HAGOS physical activity | 0.25 | 24.60 | -2.23 (-3.12, -1.33) |
| Workplace activity limitations | 0.24 | 22.42 | 0.31 (0.18, 0.45) |
| Single leg hop for distance | 0.16 | 17.64 | -0.02 (-0.03, -0.01) |
| HAGOS pain | 0.18 | 15.30 | -1.13 (-1.71, -0.55) |
| HAGOS symptoms | 0.18 | 15.01 | -1.00 (-1.52, -0.49) |
| HAGOS sport / recreation | 0.17 | 13.95 | -1.37 (-2.10, -0.64) |
| Side bridge | 0.05 | 4.79 | -1.04 (-1.98, -0.09) |
HAGOS – Copenhagen Hip and Groin Outcome Score. From linear regression output: R2 indicates R square change, F indicates F change, and B (95%CI) indicates B (95% confidence interval).
Kinesiophobia explained 35% of the variation of the hip-related quality of life, 20% of the variation of the workplace activity limitations, and less than 20% of the variation of the physical activity, pain, symptoms, sport/recreation, and health-related quality of life in men with FAI syndrome (Table 4).
Linear Regression models, adjusted for age and BMI, exploring the percentage of variation of the dependent variables explained by the independent variable (kinesiophobia) for men with femoroacetabular impingement syndrome.
| Dependent variable | R2 | F | B (95% CI) |
|---|---|---|---|
| HAGOS quality of life | 0.35 | 36.29 | -1.50 (-2.00, -1.00) |
| HAGOS pain | 0.15 | 13.07 | -0.96 (-1.49, -0.43) |
| HAGOS physical activity | 0.18 | 15.25 | -1.99 (-3.01, -0.98) |
| Workplace activity limitations | 0.20 | 17.47 | 0.31 (0.16, 0.45) |
| Health-related quality of life | 0.12 | 9.06 | -0.01 (-0.02, -0.003) |
| HAGOS sport / recreation | 0.13 | 9.91 | -1.19 (-1.96, -0.44) |
| HAGOS symptoms | 0.14 | 10.96 | -0.99 (-1.59, -0.39) |
| HAGOS physical function / daily living | 0.10 | 8.14 | -0.96 (-1.64, -0.29) |
HAGOS – Copenhagen Hip and Groin Outcome Score. From linear regression output: R2 indicates R square change, F indicates F change, and B (95%CI) indicates B (95% confidence interval).
Greater kinesiophobia was associated with worse PROMs, but not with physical function or range of motion, in people with FAI syndrome. Although we did not find sex-related differences in our cohort of people with FAI syndrome, kinesiophobia seems to affect women and men differently. In women, kinesiophobia explained 36% of the variation of the hip-related quality of life, 29% of the health-related quality of life, and 27% of the hip-related self-reported physical function. While in men, it explained 35%, 12%, and 10%, respectively.
The average Tampa Scale for Kinesiophobia score in our cohort was lower than the scores recently reported.12 We did not find differences in kinesiophobia score between women and men. However, in previous studies13-16,44 investigating larger cohorts with persistent musculoskeletal pain, men were reported to have greater kinesiophobia than women. There is no normative value for people with FAI syndrome, the participants in our study reported a wide range of kinesiophobia values, with scores ranging from 20 to 53. The diversity of scores reflects the likely variation seen in clinical practice. Greater kinesiophobia was correlated with lower hip- and health-related quality of life in our cohort, which reflects previous findings for people with patellofemoral pain,5 low back pain,6 and other chronic musculoskeletal pain.8 A systematic review of observational prospective studies reported that greater levels of kinesiophobia at baseline can predict poor quality of life at six months in people with chronic musculoskeletal pain.8 Interestingly, they only found this association with the physical-related quality of life component of the SF-12 questionnaire.45 This finding may indicate that activity avoidance behaviour (caused by kinesiophobia) negatively affects the quality of life in people with persistent pain. However, in a sex-related analysis, we observed that in women, kinesiophobia explained 29% of the variation of the health-related quality of life, while in men it explained only 12%. These findings highlight the importance of addressing kinesiophobia during the assessment and treatment program for people with FAI syndrome, especially women.
Greater kinesiophobia was associated with lower physical function assessed in our cohort supporting 46 cross-sectional studies with 9351 people who demonstrated an association between kinesiophobia and physical function in people with persistent musculoskeletal pain8 and one cross-sectional study in people with FAI syndrome.12 The link between greater kinesiophobia and lower physical function is logical considering the activity avoidance model explained by Vlaeyen and Linton10 In this model, fear is characterized by avoidance behaviours, of which the immediate consequences are that daily activities are not accomplished anymore, and avoidance of daily activities results in worse physical function.10 In our cohort, kinesiophobia explained higher percentages of variation of all other PROMs and some physical tests (single leg hop for distance and side bridge) in women than men. It seems that kinesiophobia plays a more important role in the clinical presentation of women with FAI syndrome than men. Similar to our findings, kinesiophobia explained 28% of the variation of self-reported function in a cohort of women with patellofemoral pain.5 In our cohort of men, kinesiophobia had more impact on workplace activity than physical function/daily living. A possible explanation for this is culturally- and socially-related, in that men's jobs may sometimes involve carrying heavy loads (i.e. construction workers), so the activity avoidance behaviour may affect more these components than occupational activities undertaken by women. Future studies are needed to investigate the relationship between kinesiophobia and physical workload of different jobs.
Greater kinesiophobia demonstrated fair correlation with greater pain in our cohort, regardless of sex. There is strong evidence from 38 cross-sectional studies confirming this association in people with chronic musculoskeletal pain.8 However, a recent study in people with FAI syndrome did not find correlation between kinesiophobia and pain level measure using a visual analogue scale.12 The design of our study does not allow any causality inference, however, a well disseminated model suggests that pain is considered a threatening stimulus that activates an immediate defensive system.46 Subsequently, people start to anticipate the occurrence of pain by gathering information about the association between neutral cues or conditioned stimuli and pain.46 In this case, people learn from their direct experiences. Although chronic pain cannot always be avoided, it is possible to avoid the activities assumed to increase pain or (re)injury. Consequently, people can develop fear of movement, which may explain the association between kinesiophobia and pain in our cohort.
Greater kinesiophobia was correlated with worse performance on side bridge test in women with FAI syndrome, whereas no significant correlation was found in men. Interestingly, a systematic review reported that women with FAI syndrome have strength deficits in all hip muscle compared to asymptomatic people, whereas men were only impaired in flexion and adduction strength.47 Additionally, a cross-sectional study investigating sex-specific differences in hip muscle strength in people with FAI syndrome reported that abductor strength asymmetry between symptomatic and asymptomatic hips is related to hip pain, only in women.48 Kinesiophobia explained 16% of the variation of the single leg hop for distance in women with FAI syndrome. Interestingly, it is higher than most of the findings in men. Despite impairments in physical function being common in both women and men with FAI syndrome,35 it seems that physical impairments in men are associated with factors other than kinesiophobia. During the single leg hop test, the hip may move into a position of impingement resulting in pain, which might trigger the activity avoidance behaviour in people, especially women, with FAI syndrome. This avoidance behaviour may explain why, even 12 to 24 months after hip arthroscopy, people with chondrolabral pathology presented with worse performance on the single leg hop for distance on both sides.35 We cannot assume that kinesiophobia causes these impairments, however, when the activity avoidance behaviour occurs in anticipation of pain rather than as a response to pain, these behaviours may persist because there are fewer opportunities to correct the (wrongful) expectancies and beliefs about pain as a signal of threat of physical integrity.10 It highlights the importance of having specific components to address kinesiophobia incorporated into best evidence-based treatment for people with FAI syndrome.
Contradicting our hypothesis, kinesiophobia was not related to hip range of motion in people with FAI syndrome. A possible explanation for this finding is that evidence regarding reduced hip range of motion, especially during flexion and internal and external rotation, in people with FAI syndrome compared to asymptomatic controls is limited and conflicting,47,49 and there are no normative values for this population. Therefore, it is not clear if our cohort of people with FAI syndrome presented with reduced hip range of motion. An interesting research question to be addressed in the future would be if people with FAI syndrome presenting reduced hip range of motion have higher levels of kinesiophobia than people with FAI with normal hip range of motion.
LimitationsThe Warwick agreement statement3 defines FAI syndrome as a motion-related disorder of the hip with a triad of symptoms, clinical signs, and imaging findings. Therefore, we chose people with an alpha angle higher than 60° to be sure we had included people with FAI syndrome. It may impact the capability to generalise our results to other hip-related pain conditions. Future studies would need to examine other hip-related pain conditions to understand how kinesiophobia impact their clinical outcomes. The inclusion of only young to middle aged adults in this study limits the external applicability to other populations with FAI syndrome, such as adolescents. Different occupation and levels of physical activity may also result in different findings (i.e. athletes of elite sports may have less fear of pain associated with activity). We did not assess people who are asymptomatic, therefore, it is not possible to determine if these associations exist even without symptoms. A range of self-reported factors including pain, quality of life, and functional capacity could potentially influence our results if inserted as co-variates in our regression models. However, we could not control for these factors in our study because using subscales of the same questionnaire to predict each other violates the assumption of independence. Future studies could use independent tools to explore the contribution of self-reported measures from different constructs to explain the variance of clinical outcomes in people with FAI syndrome.
Clinical implicationsKinesiophobia may be a barrier to exercise-based treatment adherence. People with greater levels of kinesiophobia present with lower level of satisfaction following exercise-based treatment than people with lower levels.50 Some interventions targeting kinesiophobia have shown good results in people with persistent knee pain and other musculoskeletal conditions.51,52 Exercise plus cognitive behavioural therapy has been reported to reduce kinesiophobia for at least 6 months after total knee replacement.52 Strategies to combine rehabilitation exercises and education, to inform patients about kinesiophobia, and enable/facilitate effective autonomous management, could be instrumental in improving perceptions of disease severity and minimising overuse of vigilant protection.52,53 Based on the relationship we found between greater kinesiophobia and worse self-reported clinical presentation in people with FAI syndrome, especially women, the effect of education on management of kinesiophobia should be investigated in this population.
ConclusionIn people with FAI syndrome, greater kinesiophobia was associated with worse PROMs, but not with hip range of motion. While we did not find sex-related differences in the mean score, in women, kinesiophobia was associated with worse performance in physical tests and explained 36% of the variation of the hip-related quality of life, 29% of the health-related quality of life, and 27% of the hip-related physical function. In men, kinesiophobia explained 35%, 12%, and 10%, respectively. These findings might indicate that kinesiophobia plays a more important role in the clinical presentation of women with FAI syndrome than men. Kinesiophobia could be addressed as part of tailored, exercise-based interventions.
This work was supported by the Australian National Health and Medical Research Council (NHMRC); Early Career Fellowship (JLK): 1119971. ER is supported by an Early Career Fellowship from the NHMRC of Australia