In some occupational groups, prolonged standing is associated with adverse symptoms. While the introduction of sit-stand workstations in office workers is increasingly common, the profile of symptom development is not known.
ObjectivesTo identify and describe the location, intensity, quality, and timing of symptoms experienced by office workers while standing at a sit-stand workstation.
MethodsThis cross-sectional observational study was performed in an university campus laboratory simulated as an office with a sit-stand workstation. Sixty-three office workers without low back pain or prior exposure to a sit-stand workstation participated. For primary outcome measures, participants recorded any symptoms of pain, stiffness, and/or fatigue on a body chart every 15 min during a 2-hour standing task. Participants rated symptom intensity on an 11-point numerical rating scale (NRS).
ResultsFifty-three participants (84%) experienced symptoms during the 2-hour standing task, with 30 participants (48%) reporting at least one symptom within 30 min of standing. A greater number of participants reported symptoms rated ≥2 on the NRS in the lumbar spine, lower extremity, and feet/ankle than the upper quadrant (odds ratios from 3.84 to 6.86). Mean maximal symptom intensity for the lumbar spine was greater than that for the upper quadrant and feet/ankles (incidence rate ratios: 1.46 to 1.79).
ConclusionSymptoms of pain, stiffness, and fatigue, especially those affecting the lumbar spine, lower extremity and feet/ankles are common in office workers who stand at a workstation. Study findings suggest that physical therapists should advise workers using sit-stand workstations to monitor symptoms and consider changing position within 30 min.
Populations are increasingly adopting sedentary lifestyles, which are associated with increased risk of mortality.1 Much of this sedentary behaviour is accumulated in prolonged periods of occupational sitting.2,3 It is estimated that approximately 82% of office work is sedentary.2 Sit-stand workstations have been introduced to many office environments to reduce sedentary behaviour at work and provide opportunity for regular postural change. This is based on the rationale that postural variation and incorporation of standing opportunities may mitigate the detrimental impact of sedentary behaviour on overall health.4,5
In occupational groups such as hairdressers, nurses, cashiers, and manufacturing workers, prolonged standing is thought to increase the risk of pain in the low back,6 legs, and feet.7 A systematic review of epidemiological studies identified that greater than four hours of occupational standing per day was associated with low back pain (LBP).8 While there is some inconsistency in findings,9,10 studies predominately using samples of students,11-15 and less frequently office workers,16 have indicated that prolonged standing at workstations may be associated with LBP. However, few studies have investigated whether office workers using standing workstations experience symptoms in other areas, such as the lower limbs and feet,8,17 that are commonly experienced by other professions who stand for prolonged periods.7,18 In light of evidence that standing episodes among office workers using sit-stand workstations vary from 15 min to one or more hours,19-21 it is important to understand the profile of symptom development in this population. This information will guide recommendations from physical therapists and ergonomists for sit-stand workstation use.
The aim of this study was to identify and describe the location, intensity, and onset of symptoms experienced by office workers who stand at a sit-stand workstation.
MethodsParticipantsVolunteers were recruited for this cross-sectional observational study via an online newsletter at a university campus between May and November 2016. Participants were eligible if they were 18-65 years of age, worked a minimum of 30 hours/week performing predominantly computer work and had not previously used a sit-stand workstation. Exclusion criteria were: a history of lower limb or spinal surgery; circulatory disorders; pregnancy; pain, discomfort, stiffness, or fatigue anywhere in the body prior to testing; LBP in the last six months requiring treatment from a health professional; or neurological conditions. Ethical approval was obtained from The University of Queensland Medical Research Ethics Committee, Brisbane, Queensland, Australia (Approval #2015000469). All participants provided written informed consent prior to participation.
Experimental protocolThe study was performed in a university campus laboratory simulated as an office with a sit-stand workstation. Participants arrived at testing via their own means. Participants performed their own computer work during a 2-hour standing task.22 They were asked to wear flat footwear that would be comfortable to stand in for two hours. Participants stood fist-width away from a standing workstation that was set up according to the Workplace Health and Safety Queensland guidelines.23 The desk height was 3 cm below the olecranon process of the elbow with the elbow flexed at 90°, and the top of the monitor was at eye-level at a distance equal to the length of the participant's reach. Participants placed the mouse and keyboard in their preferred location. They were instructed to remain within a 0.61×1.22 m area marked on the ground and weight shift as much as required, but not lean on the desk.
At baseline (0 min) and every 15 min throughout the 2-hour test, participants marked any symptoms on a body chart and completed a pain Numeric Rating Scale (NRS). The standing task ceased after 2 h or earlier if the participant requested to stop the test or reported severe pain (defined as greater ≥7 out of 10 on the NRS24).
MeasuresLocations of symptoms experienced at baseline and during the standing task were recorded on a body chart. Participants were asked to ‘shade in any areas of the body in which they felt pain, discomfort, stiffness, or fatigue.’ Participants were then asked to rate the symptom intensity using an 11-point NRS anchored with ‘no pain or discomfort’ at 0 and ‘worst pain or discomfort imaginable’ at 10.
An online questionnaire was used to collect information on participant demographics (age, height, weight, sex), physical activity level, and work history to describe the study sample. Physical activity level was evaluated using the Active Australia Survey (AAS) which has acceptable reliability and validity,25 and quantifies leisure and transport related physical activity levels to classify individuals as: inactive (0min/week), insufficiently active (1-149min/week), or sufficiently active (≥150-300min/week). Participants were asked the number of hours they worked in the last seven days. The Occupational Sitting and Physical Activity Questionnaire (OSPAQ)26 was used to assess the time (minutes) spent sitting, during a typical workday. This questionnaire has acceptable validity and reliability in office workers.27
Data managementThe number of individuals who experienced symptoms and the NRS symptom intensity were calculated for different body areas, with data combined for left and right sides. For comparisons between symptom locations, body areas were combined into four regions: upper quadrant (head, face, neck, cervical and thoracic spines, upper limbs); lumbar spine (lumbar spine and upper buttocks); lower extremity (hips, thighs, knees, and lower legs to the Achilles tendon); feet/ankles. Due to suggestions that pain ≥2/10 on the NRS is clinically meaningful,28 data on the number of participants with symptoms of this intensity were also reported. Maximal symptom intensity across the entire standing task and mean symptom intensity for each 15-minute epoch for each body region were calculated from participants who reported a symptom in the region (i.e. participants who did not report a symptom were not included in the calculation of the mean or maximum.)
Statistical analysesStatistical analyses were conducted using Stata (Version 13.0, StataCorp, USA). Data are presented as mean ± standard deviation and range for continuous variables, and number and percentage for categorical variables. Statistical significance was set at p<0.05. Logistic regression was used to examine differences in the number (frequency) of participants reporting symptoms across the four body regions, with data presented as odds ratio (OR). Analyses were conducted for participants who reported symptoms with NRS ≥1, and again for participants who reported symptoms with NRS ≥2. Poisson regression models were used to investigate differences in mean NRS scores between the four body regions at the end of the standing task, and mean maximal NRS scores during the standing task. Data are presented as incidence rate ratios (IRR). Linear regression was used to examine possible associations between maximal symptom intensity during the standing task and body mass index (BMI), for each of the four body regions, with age and sex as covariates.
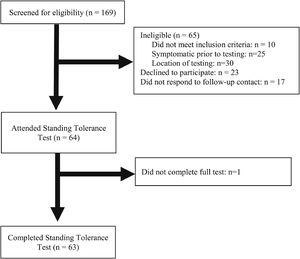
ResultsA total of 169 people responded to study advertisements, of which 104 were eligible to participate (62%). After removing individuals who did not respond to contact (n = 17) and declined to participate (n = 23), 64 participants attended testing. One individual withdrew during testing for voiding requirements (n = 1). 63 participants completed the study (Fig. 1). Participation rate from those eligible for inclusion was 60% (63 out of 105). No participants were required to stop the test due to pain. Participant demographics for those who completed the study are presented in Table 1.
Participant characteristics (n = 63).
| Demographic characteristics | Data |
|---|---|
| Age, years | 39 ±14 |
| Female sex, % | 44 (70%) |
| Height, m | 1.70 ±0.10 |
| Weight, kg | 69 ±14 |
| Body mass index, kg/m2 | 23.9 ±3.8 |
| Body mass index categorya | |
| Underweight | 2 (3%) |
| Normal weight | 37 (59%) |
| Overweight | 19 (30%) |
| Obese | 5 (8%) |
| Physical activity levelb | |
| Inactive | 0 (0%) |
| Insufficiently active | 6 (10%) |
| Sufficiently active | 55 (90%) |
| Hours worked in the last 7 days | 38.1 ±12.5 |
| Percent of typical work day spent sitting | 82 ± 15 |
Data are mean ± standard deviation or frequency (proportion).
Fifty-three of the 63 participants (84%) experienced symptoms during the 2-hour standing task. Thirty-six participants (57%) reported symptoms in multiple body regions (feet/ankles, lower extremity, lumbar spine, upper quadrant): 19 participants (30%) reported symptoms in two regions, 15 participants (24%) in three regions, and 2 participants (3%) in all four regions. Seventeen participants (27%) reported symptoms in only one region. The number of participants who developed symptoms in each body region after 15, 30, 60, 90, and 120 min of the standing task is displayed in Table 2.
Number (%)a of participants who reported symptoms within each time period (minutes) of the standing task.
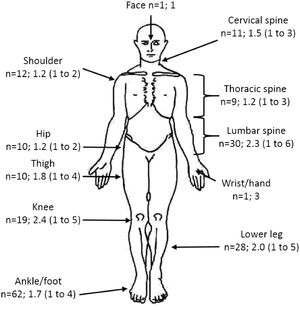
The distribution of symptoms around the body during the standing task is shown in Fig. 2. Analysis of body regions indicate similar numbers of participants reported symptoms (NRS ≥1) in the feet/ankles (n = 31, 49%), lumbar spine (n = 30, 48%), and lower extremity (n = 28, 44%). The number of participants reporting upper quadrant symptoms (n = 19, 30%) was significantly lower than those with feet/ankle symptoms (OR = 2.24; 95% CI: 1.12, 4.49). Considering symptoms with NRS ≥2, the number of participants who reported symptoms in each body region was: 20 (32%) in the lumbar spine; 15 (24%) in the lower extremity; 13 (21%) in the feet/ankles; and 4 (6%) in the upper quadrant. The number of participants reporting upper quadrant symptoms of NRS ≥2 was lower than the number of participants reporting lumbar (OR = 6.86; 95% CI: 2.28, 20.67), lower extremity (OR = 4.61; 95% CI: 1.55, 13.74), and feet/ankles (OR = 3.84; 95% CI: 1.09, 13.52) symptoms.
The distribution of symptoms reported for individual body areas during the 2-hour standing task. The number of participants (n) and mean (range) maximal numeric rating scale (NRS) intensity across the standing task are displayed. When n = 1, the raw NRS data point is reported. Symptoms from the left and right sides of the body were collapsed into a single category (e.g., ‘shoulder’ presents data from the left and right shoulders).
Mean ±SD maximal symptom intensity across the test (calculated from symptomatic participants) was 2.3 ±1.3 out of 10 for the lumbar spine (n = 30), 1.8 ±1.0 for the lower extremity (n = 28), 1.6 ±0.8 for the feet/ankles (n = 31), and 1.3 ±0.6 for the upper quadrant (n = 19). Maximal lumbar spine symptom intensity was significantly greater than that experienced in the upper quadrant (IRR = 1.79; 95% CI: 1.13, 2.86) and feet/ankles (IRR = 1.46; 95% CI: 1.01, 2.12). There were no differences in maximal symptom intensity between other body regions. Linear regression did not demonstrate a significant relationship between maximal symptom intensity during the standing task and BMI for any of the body regions (data not shown).
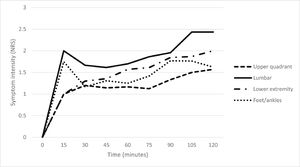
Mean symptom intensity for each 15-minute epoch throughout the standing task for the four body regions (for those participants who reported symptoms in the region) are presented in Fig. 3. On completion of the 2-hour standing task, the 23 participants who reported lumbar spine symptoms at 120 min had a mean intensity of 2.4 ±1.4. This intensity was higher than all other body regions (vs upper quadrant IRR = 5.09; 95% CI: 2.19, 11.82, n = 7; vs lower extremity IRR = 2.00; 95% CI: 1.11, 3.62, n = 14; vs feet/ankles IRR = 2.07; 95% CI: 1.17, 3.68, n = 14). Mean symptom intensity at the end of the standing task was also significantly higher in the lower extremity (mean = 2.0 ±1.2) than for the upper quadrant (IRR = 2.55; 95% CI: 1.09, 5.97). There was no difference in mean symptom intensity on completion of the standing task between the upper quadrant (mean = 1.6 ±0.8) and feet/ankles (mean = 1.5 ±1.4, respectively).
DiscussionThe aim of this study was to describe the location, intensity, and timing of symptoms experienced by office workers who stand at a sit-stand workstation for two hours. The majority of study participants (84%) experienced symptoms somewhere in the body during the standing task, with only 16% of participants remaining symptom-free. Symptoms were more commonly reported in the lumbar spine, lower extremity, and ankles/feet, than in the upper extremity. The intensity of symptoms reported was relatively low,24 with a mean maximal intensity ranging from 1.3 to 2.3 for different body regions. Onset of symptoms occurred early in the standing task for many individuals. Nearly half of participants reported experiencing at least one symptom after 30 min of standing.
Prevalence of standing-induced low back symptoms in our study was 48%, which is similar to that reported in previous research using a standing task (50-81%).12,14,15,29 Gallagher and colleagues found LBP that developed during a standing task among university students did not resolve spontaneously with sitting,12 and a specific exercise intervention was required.30 The mean maximal intensity of symptoms experienced in the low back by individuals who developed symptoms in our study increased from 0 at baseline to 2.3 out of 10 at some point throughout the test, which is considered clinically meaningful.28 These data suggest that LBP may be a problem among office workers who stand for prolonged periods. The mechanism underlying the development of LBP during prolonged standing in office workers is not well understood. Research has suggested that an individual's standing posture during the first 15 min at a standing workstation may be associated with the development of LBP.31 The amount of lumbar spine flexion/extension10,13 and fatiguability of the hip abductor muscles32 have also been proposed to be related to LBP development.
Our data indicate that when using a standing workstation, office workers also commonly develop symptoms in other areas of the body, particularly the feet/ankles and lower extremities. However, while symptoms in these areas were prevalent, the mean pain intensity was 1.5-2.0 out of 10, which may not be clinically meaningful. Similar to previous findings in sales and kitchen staff,33 half of the participants in our study developed symptoms in the feet and ankles during standing. In manufacturing employees, it has been suggested that higher pressure through the metatarsal heads during gait and footwear with hard soles may be related to the development of foot pain.34 Further research is needed to investigate the role of footwear in the development of foot/ankle pain in office workers using standing workstations.
In our study 44% of participants developed lower extremity symptoms. Calf pain/fatigue associated with standing is frequently reported in the literature, and is proposed to be associated with decreased muscle activity which reduces venous return and leads to blood-pooling, swelling, and metabolite build up in the legs.35 Previous research has shown that lower extremity symptoms are reduced and/or prevented when assembly-line workers move.36 Participants in our study were instructed to weight-shift as much as required, but the amount of weight-shifting or movement performed was not recorded. Further research on the relationship between weight-shifting and other forms of movement on the development of lower extremity symptoms in office workers using sit-stand workstations is warranted.
Fewer than one third of our participants developed upper quadrant symptoms during the 2-hour standing task. While upper quadrant pain is reported to be a common persistent pain location among office workers, previous studies have investigated the 12-month prevalence of symptoms or have used traditional workstations which involve predominately sitting.37-39 A recently convened meeting of experts in sedentary behaviour concluded that standing at work is not associated with upper extremity discomfort.37,40 The workstation set-up to avoid awkward and extreme postures41 and the possible greater physical load being undertaken by the trunk and lower limbs in a standing position, and lower load undertaken by the upper extremity,42 may explain why our participants experienced few upper extremity symptoms.
When considering appropriate guidelines for the use of sit-stand workstations, timing of symptom onset must be taken into account. In our study, 48% of participants experienced symptoms within 30 min of standing at a sit-stand workstation. International guidelines recommend that it is safe to stand for up to one hour at a time.6 A recent systematic review recommended avoiding standing for longer than 40 min.43 Our data suggest that many office workers may need to stand for less than 30 min at a time to avoid development of symptoms. This is consistent with findings from previous studies showing high participant pleasantness and acceptability when standing for 30 min or less,11 and preference to stand for at least 15 min at a time.9 Together these data suggest that 15-30 min standing episodes may be ideal. This is important for physical therapists, ergonomists, and occupational health professionals to consider when establishing workplace guidelines for the use of sit-stand workstations and when managing patients with symptoms associated with standing at work.
To optimise cardiometabolic health outcomes, it is recommended that time spent in uninterrupted sitting be limited to 30 to 60 min.44 Little is known about the duration of sitting before returning to standing to avoid early onset of symptoms in subsequent standing bouts. Previous work found a 1:3 ratio of time spent sitting and standing (15 min sitting: 45 min standing) was associated with LBP development12; however, this is likely due to the length of time spent standing rather than the duration of time spent sitting. This is supported by work showing that development of pain within the first 15 min of standing distinguished those who would continue to experience LBP with standing.45 This suggests that individually monitoring symptoms and changing posture based on symptoms may be important.
Study limitations must be considered when interpreting data. Participants performed their own work at the computer, rather than a standardised task. This was done to replicate the actual work environment as closely as possible. Footwear was also not standardised between participants. Individuals were asked to wear flat comfortable footwear for two hours of standing. The amount of support and cushioning provided by different types of footwear could have influenced symptom development. Participants were to remain standing within a 0.61×1.22 m area for the duration of the study and were not allowed to walk around or sit down when they noticed the onset of discomfort. Our study participants were active (90% of participants classified as sufficiently active) and of normal body weight, with only 38% (n = 24) of participants overweight or obese (BMI>25kg/m2). Obesity46 and low physical activity participation47 have been identified as risk factors for the development of LBP. As the majority of our sample had a normal BMI and met physical activity recommendations this may have restricted our ability to detect an association with standing-induced back pain development; however, previous research has identified similar responses to sit-stand workstation in normal and overweight individuals.11
Participants in our study did not have previous experience using a sit-stand workstation, and therefore were unaccustomed to standing at work. It is not known whether symptoms are more common and severe in those new to using a sit-stand workstation. Further, individuals in this study were previously asymptomatic and did not have a history of LBP. It is not known whether the response to using a sit-stand workstation would be similar in symptomatic individuals or individuals with a history of LBP. Further research is needed to explore the development and management of symptoms among symptomatic workers who are transitioning to sit-stand workstations.
ConclusionThe findings from this study indicate that low back, foot/ankle and lower limb symptoms are common in office workers using standing workstations, and that nearly half of workers develop pain within 30 min of standing. This suggests that physical therapists and ergonomists should advise workers to change position within 30 min and monitor symptoms when using sit-stand workstations.
This study was funded by a Collaborative Research Grant from The University of Queensland. The authors thank The University of Queensland's Faculty of Health and Behavioural Sciences for funding this project, and the research assistants who conducted data collection.