Low back pain (LBP) is a common but complex musculoskeletal disorder responsible for a huge economic and social burden.1 In 2015, LBP affected around 540 million people and accounted for 60.1 million years lived with disability.2 The publication of The Lancet Low Back Pain Series1,3,4 in 2018, provided worldwide recognition of the LBP problem amongst healthcare professionals and the general public.5 Nonetheless, LBP is still the number one cause of disability in the world and many patients are still not receiving the right care.6
In Argentina, LBP is the main cause of years lived with disability, similar to other Latin American countries.2 It is one of the main reasons for physical therapy consultation in the public7,8 and private health systems.9 No reliable data regarding the economic burden of LBP in Argentina are available; however, the excessive use of imaging10 and the high rate of work absenteeism,11 suggests that costs (direct and indirect) due to LBP are likely to be as significant as is seen for other countries worldwide.12
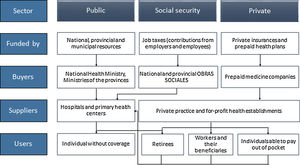
An overview of Argentina's health systemArgentina is an upper-middle income country with an estimated population of 45 million people, of which more than 90% live in large cities.13 The Argentine healthcare system is a complex and federal system, where the national government, 24 jurisdictions, and three subsystems interact: the public care subsector (funded by public taxes; public health funds usually flow from national to provincial budgets), the social security subsector (based on job taxes; the revenues from contributions from wages of employers and employees are collected by the AFIP [Federal Administration of Public Revenues], which in turn allocates a percentage back to the entities in charge of social security), and the private subsector (private insurances and prepaid health plans) (Fig. 1).13,14 This health system is fragmented and segmented, with evidence of inequalities in the use of healthcare services, to the detriment of the most vulnerable population (i.e., pregnant women, children, low-income population).15,16 According to data from the latest Census (2010 Census), 36% of the population do not have medical coverage, social security, or the capacity to pay for private care (https://www.indec.gob.ar/). Thus, they are treated in public hospitals and health centers.
Argentine health system structure. Adapted from Belló e Becerril-Montekio.13
The Argentine healthcare systems seek to provide effective universal free health coverage (i.e. that people actually receive prioritized health care services).14,15 Despite the healthcare expenditure (9.4% of Gross Domestic Product) in Argentina being similar to other countries of the region like Brazil, Uruguay, and Chile, and even similar to Spain, Finland, Australia, and New Zealand;14 the results are not as expected and healthcare outcomes lag behind the country's potential.17 Most public primary health care programs and services in Argentina are still focused on maternal and child health rather than chronic non-communicable diseases for adults14 even though LBP is the leading cause of disability.2
Epidemiology of low back pain in ArgentinaThere is a lack of reliable data regarding LBP prevalence in Argentina. However, a few epidemiological studies of different populations have been published. A study involving 139740 full time workers reported LBP as the third most frequent work-related injury, with an incidence rate of 5.2 episodes every 1000 worker-years. Only 2.4% of those episodes did not lead to work absenteeism. Individuals who received magnetic resonance imaging (MRI) or computerized tomography (CT) and those who underwent surgery reported more lost workdays with a median of 61.5 and 164 days, respectively.11 Another study aimed to compare employment conditions, psychosocial working conditions, and prevalence of LBP among migrant and local construction workers in Argentina.16 The 7-day prevalence of LBP was higher among migrant construction workers (80%) compared to local workers (42%). Furthermore, being a migrant worker (odds ratio [OR]=2.1, 95% confidence interval [CI]: 1.4, 3.0) and working without a contract (OR=1.7, 95% CI: 1.4, 2.1) were both associated with a higher prevalence of LBP. Informal employment is common in Argentina, with one in every 4 workers having informal employment – (http://www.trabajo.gob.ar/estadisticas/Bel/index.asp), which leads to the absence of social security protection and poor employment conditions. Within the Argentine indigenous Wichi and QOM population, LBP was also the most prevalent musculoskeletal disorder.18,19 From 2006 to 2010, the most common reason for admission to hospital for a musculoskeletal condition was LBP and the mean length of stay was 3.8 days.20
Recommendations for the management of low back pain based on clinical practice guidelinesGuidelines recommend that a clinical assessment is used to triage patients with LBP into those with (i) a problem beyond the lumbar spine, (ii) radicular syndromes, (iii) suspected serious pathology, or (iv) non-specific LBP. Further diagnostic workup e.g., imaging and pathology is only required for the small number of patients with suspected serious pathology. For many patients with non-specific LBP, simple care (advice, reassurance, and self-management) and a review at 1 to 2 weeks is all that is required. If patients need additional care, non-pharmacological treatments (e.g., physical and psychological therapies) are trialed before pharmacological treatments. If pharmacological treatments are used, they should be used at the lowest effective dose and for the shortest period of time possible. Most guidelines advise caution or discourage the use of opioid medicines. For patients with persistent LBP, exercise and/or cognitive behavioral therapy is recommended with multidisciplinary treatment reserved for more complex presentations and those who do not respond to simpler measures. Electrotherapy, traction, orthoses, bed rest, surgery, injections, and denervation procedures are not recommended for patients with non-specific LBP.21
Current issues in low back pain management in ArgentinaLack of local clinical practice guidelineEvidence-informed clinical practice guidelines (CPGs) provide recommendations to help decision making about health interventions bridging the gap between policy, best practice, local contexts, and patient values.22 Currently, 15 CPGs are available for non-specific LBP around the globe, of which two belong to Latin American countries (Brazil and Mexico).22 The adherence to CPG in the management of LBP has been related to better outcomes (fewer functional limitations and less treatment sessions).23 Argentina lacks a local CPG for managing LBP, which may in part explain the departures from guideline-endorsed care.
LBP is poorly oriented to primary careAccording to the CPGs, an episode of LBP should be managed in primary care, where after the screening of serious pathologies (e.g. vertebral fracture), reassurance and messages to stay active and at work should be delivered. However, in Argentina there is a hospital-centered model of care poorly oriented to primary care. As a consequence, LBP was the most frequent cause of hospitalization due to musculoskeletal disorders in Argentina between 2006 and 2010.20 Moreover, trauma doctors (specialist) both in private and public healthcare treat the majority of people with back pain. While some patients will receive physical therapy referral, physical therapists are not primary contact practitioners in Argentina. Primary care is not well developed in Argentina with general practitioners and family physicians being uncommon.
Overuse of imaging in non-specific LBPThe majority of CPGs strongly discourage the routine use of imaging in episodes of non-specific LBP. A recent systematic review and meta-analysis showed that across the world, 16.3% (95% CI: 12.6%, 21.1%) of patients who presented to primary care with LBP received simple imaging (plain radiography or ultrasound) while complex imaging (CT, MRI) was performed for 9.2% (95% CI: 6.2%, 13.5%).24 In Argentina, a prospective study including an outpatient rehabilitation population with LBP from a public hospital found that 80% received radiographs and 25% received a CT or MRI.10 Soriano et al.11 reported a 10% prevalence of MRI and CT scans in patients with LBP associated with occupational activities. These two studies suggest an overutilization of imaging in the Argentine health system. This excessive imaging increases healthcare costs12 and exposes patients to radiation. There is also some evidence that incidental findings such as disc bulge, which are common even in people without LBP, may cause concern and worry amongst patients and lead to unnecessary surgeries.25
Lack of research productivityResearch is central to improving healthcare and outcomes for people with LBP.26 At present, 18 of the 23 most productive countries in LBP research belong to the high-income group. According to the ranking of the website “http://www.expertscape.com/” (based on the quantity and quality of peer-reviewed clinical research publications in the National Library of Medicine's MEDLINE database), Argentina ranks 6th in Latin America with only 10 articles published in the last decade concerning LBP. In contrast, the research productivity of Brazil, another upper-middle income country from the region, is much higher with 398 (#1) published papers. Several factors might contribute to the poor research productivity in Argentina, such as inappropriate government policy, low research funding, and the fact that musculoskeletal disorders are not a health priority.
Misconceptions of the general population regarding LBPUnhelpful beliefs have a negative impact on LBP clinical outcomes, and are considered an important treatment target for the prevention and treatment of pain-related disability.27,28 Misconceptions about LBP are common globally, and Argentina is not an exception. A recent online survey showed that the Argentine general population has negative beliefs about the vulnerability of the back; they see the back as a fragile structure that needs to be protected.29 Beliefs can be influenced by a range of sources; friends and family, the media, but especially health care professionals.30,31 A survey targeting Argentine physical therapists showed that their clinical practice was not consistent with the recommendations of CPGs, which may be related to the misconceptions of the general population.32
Steps required to improve low back pain management in ArgentinaThere are a number of possible solutions to improve the management of LBP in Argentina:
- 1
There is an urgent need to develop and disseminate a local CPG. To expedite this process it would be prudent to borrow the evidence review from a recent guideline from another country and then adapt the management recommendations to the context of the local Argentinian healthcare setting.
- 2
It would be possible to improve knowledge of LBP among the general population using the mass media campaign approach that was successful in Australia.33 It would be sensible to explore the use of more contemporary media opportunities such as social media. There is also the potential to incorporate education on LBP into the school curriculum to supplement coverage of other common non-communicable diseases.
- 3
To better understand the precise evidence-practice gaps and to track progress it would be sensible to improve data collection system and quality of epidemiological data (electronic database, etc.).
- 4
There is a need for the Government to invest in LBP research to build much needed research capacity. While much research can be borrowed from other countries, there are some research questions that can only be answered by local researchers studying the local context. Partnering with countries in the region with a strong LBP research portfolio (e.g., Brazil) or further afield (e.g., Australia) would provide opportunities for research training and exchanges that would accelerate progress in building research capacity.
- 5
The healthcare policies and healthcare systems need to be revised so that they encourage high value care and discourage low value care. For example, currently, the population can more easily access a medical specialist than a physical therapist, a situation that encourages over-medicalization of LBP.
- 6
There is a need to regulate conditions of work and employment for informal workers. The lack of regulation and poor development of musculoskeletal health policies contribute to disability due to LBP. Moreover, promoting employment in the formal sector in Argentina is a necessary measure that may improve the population's health.
Argentina currently faces major challenges and barriers for optimal management of LBP. Acknowledging the burden, shifting to a healthcare model oriented to primary care, and developing a local CPG are crucial actions that can help to promote high value care and address the increasing burden of LBP in Argentina.