Beliefs about the body and pain play a powerful role in behavioural and emotional responses to musculoskeletal pain. What a person believes and how they respond to their musculoskeletal pain can influence how disabled they will be by pain. Importantly, beliefs are modifiable and are therefore considered an important target for the treatment of pain-related disability. Clinical guidelines recommend addressing unhelpful beliefs as the first line of treatment in all patients presenting with musculoskeletal pain. However, many clinicians hold unhelpful beliefs themselves; while others feel ill-equipped to explore and target the beliefs driving unhelpful responses to pain. As a result, clinicians may reinforce unhelpful beliefs, behaviours and resultant disability among the patients they treat.
MethodsTo assist clinicians, in Part 1 of this paper we discuss what beliefs are; how they are formed; the impact they can have on a person's behaviour, emotional responses and outcomes of musculoskeletal pain. In Part 2, we discuss how we can address beliefs in clinical practice. A clinical case is used to illustrate the critical role that beliefs can have on a person's journey from pain and disability to recovery.
ConclusionsWe encourage clinicians to exercise self-reflection to explore their own beliefs and better understand their biases, which may influence their management of patients with musculoskeletal pain. We suggest actions that may benefit their practice, and we propose key principles to guide a process of behavioural change.
Musculoskeletal pain is a multi-factorial condition; it involves complex interactions between structural, physical, psychological, social, lifestyle, and comorbid health factors and is therefore best understood through a biopsychosocial framework.1–5 While in most cases, musculoskeletal pain is self-limiting, a significant proportion of society go on to experience long term pain and disability. Musculoskeletal pain is now a leading cause of disability world-wide6 and the prevalence of musculoskeletal pain-related disability is predicted to grow exponentially in the next two decades7 placing unsustainable strain on health systems.
A substantial body of research has shown that what one believes and does about their musculoskeletal pain predicts how long the pain will last and how disabled they will be by it.8–11 Given that these beliefs are modifiable, they are considered an important target for the prevention and treatment of pain-related disability. Clinical guidelines recommend addressing erroneous/unhelpful beliefs as the first line of treatment in all patients presenting with musculoskeletal pain.3 However, many clinicians hold erroneous beliefs themselves, while others feel unskilled to explore and target these beliefs, perceiving this to be outside of their scope of practice.12,13 Furthermore, clinicians who hold these negative beliefs are more likely to provide advice that reinforces unhelpful behaviours and resultant disability.14,15 To assist clinicians, in Part 1 of this paper we will discuss what beliefs are; how they are formed; the impact they can have on a person's behaviour, emotional responses and outcomes of musculoskeletal pain. In Part 2, we will discuss how we can address beliefs in clinical practice.
PART 1 – BeliefsWhat are beliefs and how are they formed?Beliefs can be defined as “Something one accepts as true or real; a firmly heldopinion” (Oxford dictionary). While modifiable, the core characteristics of beliefs can make them difficult to identify and target; (i) Beliefs are not always rational i.e. they can persist even after being presented with facts. For example, a patient might believe that structural changes seen on imaging are the source of their musculoskeletal pain, despite being told that the changes reflect ‘normal ageing’ and are widely prevalent among the asymptomatic population; (ii) Beliefs can be contradictory i.e. an individual can hold two or more conflicting beliefs at the same time. For example, a patient might believe that they need to strengthen their ‘weak’ joint and at the same time believe that exercise can damage their joint; (iii) Beliefs may be explicit, meaning that they are elicited deliberately upon reflection. For example, when asked about feared activities during the clinical interview a patient with back pain might recall being warned from a young age to protect the back while lifting; or (iv) Beliefs may be implicit, elicited only upon ‘automatic’ associations in memory. For example a patient when asked about their beliefs regarding lifting may deny protecting their back, but when asked to lift a load during the clinical examination, the patient might engage in behaviours such as avoidance of spinal flexion to ‘protect’ the back while lifting.16
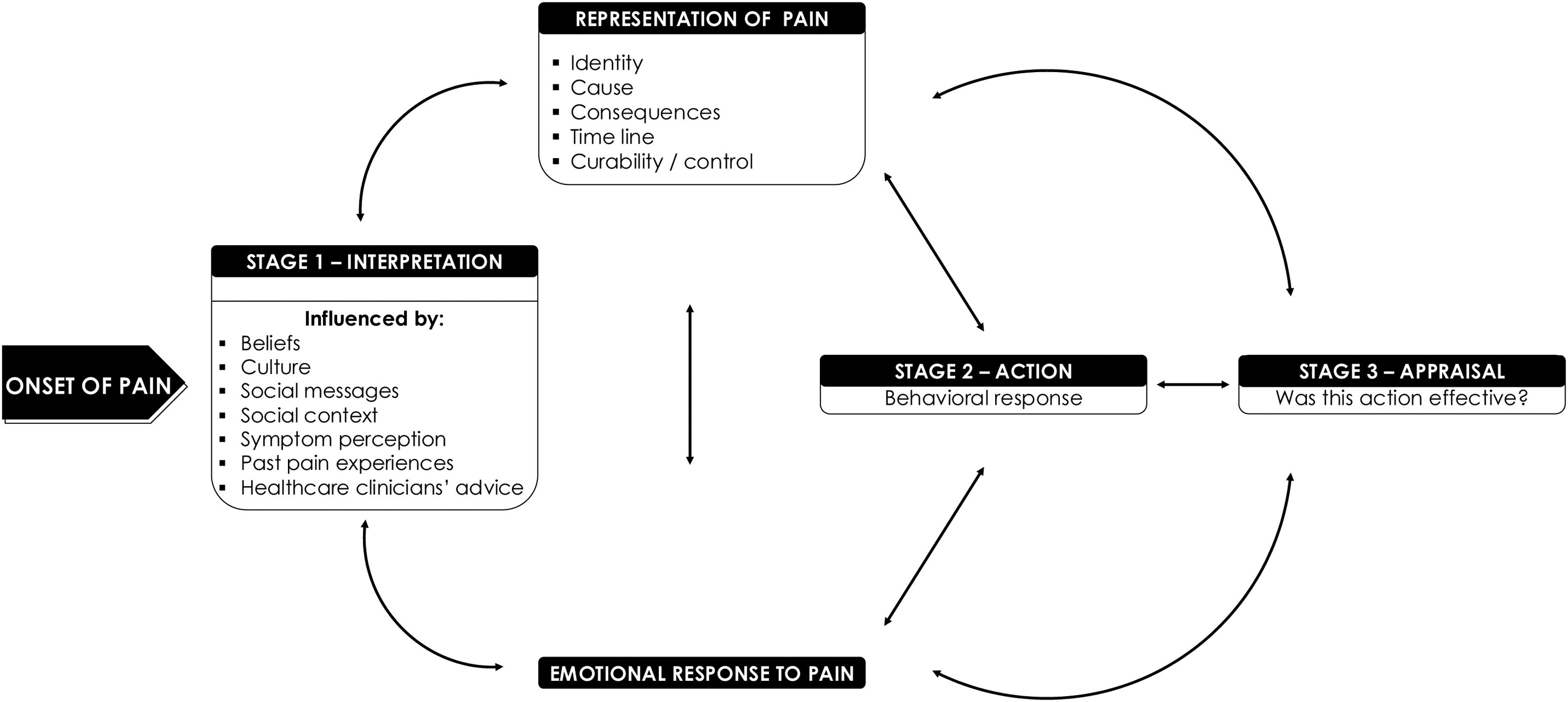
Beliefs can also be defined as “fundamental truths governingbehavior”.16 The health belief theory the Common Sense Model17 is a useful framework to understand the role beliefs about musculoskeletal pain play in governing coping responses. According to the Common Sense Model, when we experience a symptom, we attempt to make sense of the symptom by forming a ‘representation’ of it. This representation comprises of a set of beliefs about how the body functions in a given context, including beliefs about (i) the identity of the pain (what the pain is, e.g. “a slippeddisc”), (ii) the causes of the pain (e.g. “heavylifting”), (iii) the consequences of the pain (e.g. “physicalincapacity”), (iv) how controllable the pain is (e.g. “activity avoidance”, “surgery to fix thedamage”) and, (v) how long the pain will last (e.g. “here tostay”). These beliefs are formed through our previous direct (felt) experiences of the symptom; but can also be formed through our vicarious experiences observing others with similar symptoms, as well as information we have learned about the symptom from sources such as the media and clinicians.18 In this way, beliefs can pre-exist our own direct experiences of a symptom.
Based on our representation of the symptom, we will make a decision about what to do (action), referred to as problem solving behaviour. If the outcome of the behaviour is expected and in the direction of the target goal, then we will perceive that this representation was useful, and next time we experience the symptom we are likely to engage in the same behaviour. If the outcome of the behaviour is not expected, then we will perceive that the representation was not useful, and will update our beliefs and adjust our behaviour accordingly. The way we represent a symptom, and whether the behavioural response was effective, can also elicit an emotional response (positive or negative). In the absence of a useful cognitive representation to inform problem solving behaviour, subsequent behaviours may be driven by this emotional response18 (see Fig. 1). A person's representation of their symptom is dynamic, meaning it changes according to new information and experiences.
Common Sense Model framework (adapted from Leventhal et al., 1992).18
Beliefs related to the identity, cause, consequence, controllability and timeline of musculoskeletal pain influence problem solving behaviour and emotional responses (for a clinical illustration of this process, see Jamie's story in Table 1). As described by the Common Sense Model, these beliefs are constantly being updated to influence ongoing behaviour through a dynamic, continuous interaction between cognitive, behavioural and contextual factors. Thus, while the content of beliefs may differ between individuals and even within individuals at different time points, the way in which beliefs govern coping responses to pain will be the same.20
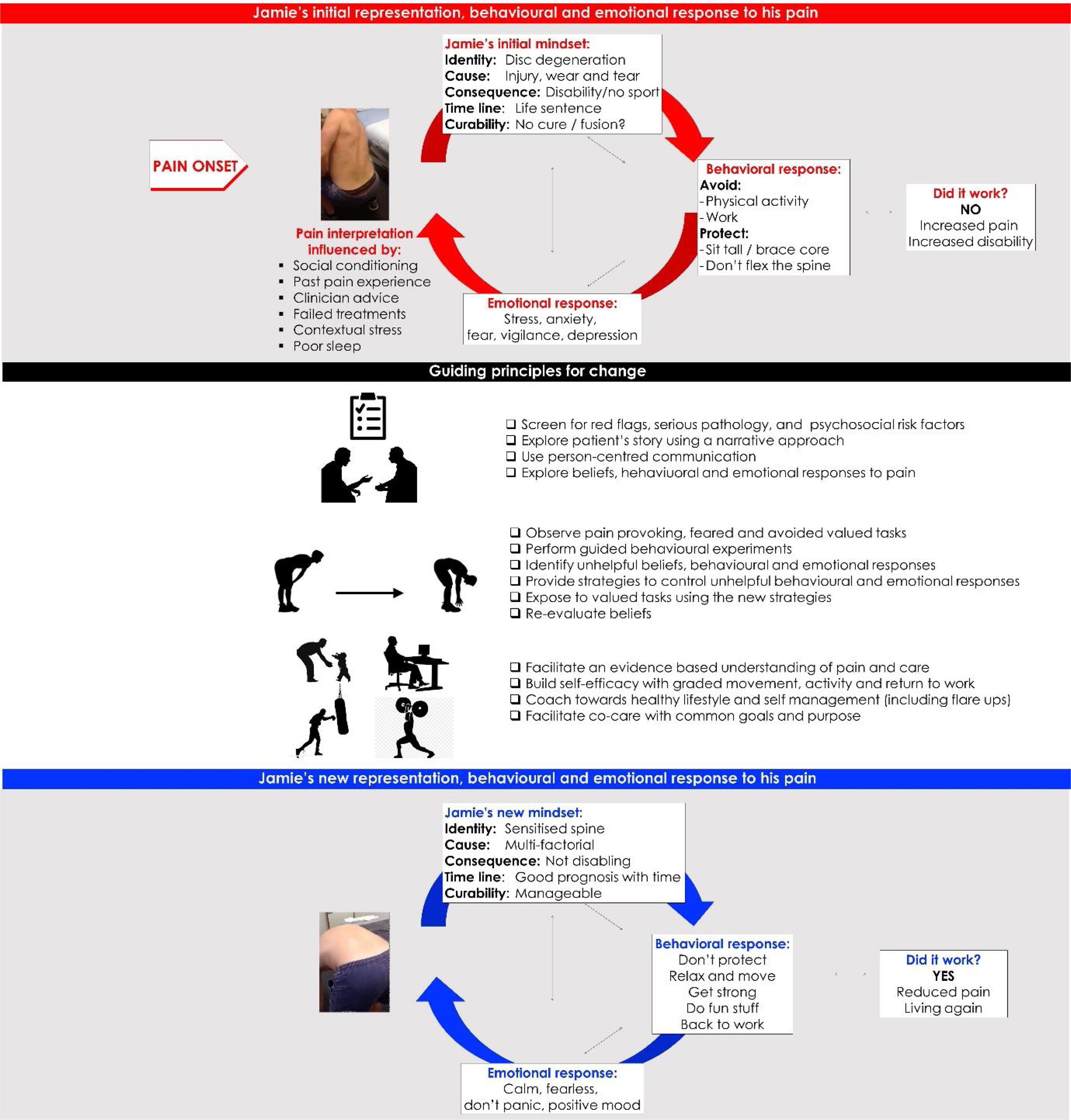
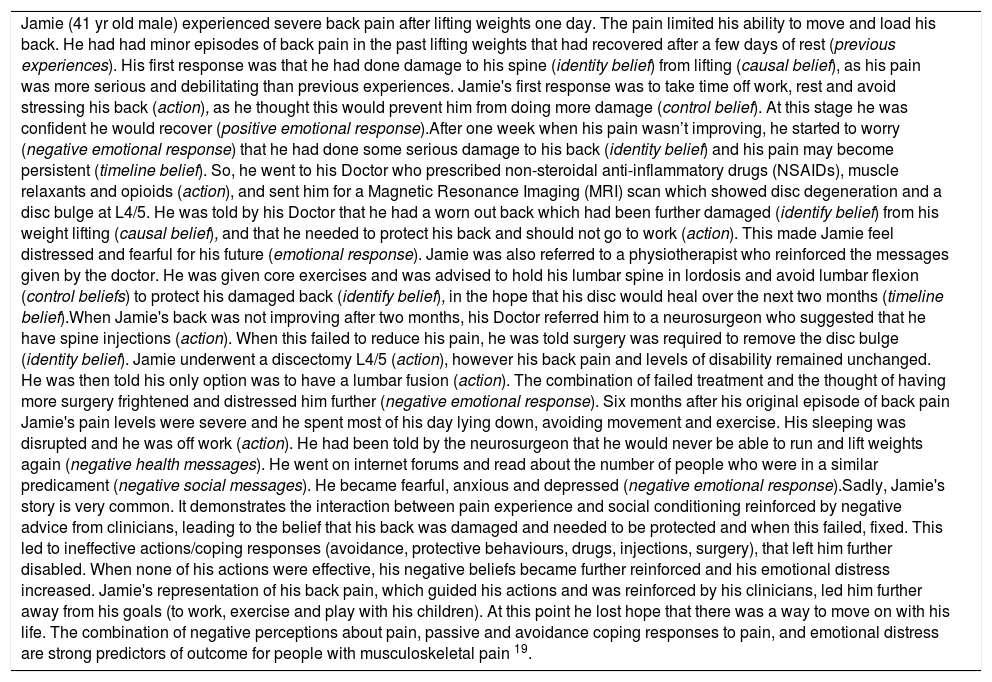
Clinical scenario: Jamie's story – a vicious cycle of pain and disability.
| Jamie (41 yr old male) experienced severe back pain after lifting weights one day. The pain limited his ability to move and load his back. He had had minor episodes of back pain in the past lifting weights that had recovered after a few days of rest (previous experiences). His first response was that he had done damage to his spine (identity belief) from lifting (causal belief), as his pain was more serious and debilitating than previous experiences. Jamie's first response was to take time off work, rest and avoid stressing his back (action), as he thought this would prevent him from doing more damage (control belief). At this stage he was confident he would recover (positive emotional response).After one week when his pain wasn’t improving, he started to worry (negative emotional response) that he had done some serious damage to his back (identity belief) and his pain may become persistent (timeline belief). So, he went to his Doctor who prescribed non-steroidal anti-inflammatory drugs (NSAIDs), muscle relaxants and opioids (action), and sent him for a Magnetic Resonance Imaging (MRI) scan which showed disc degeneration and a disc bulge at L4/5. He was told by his Doctor that he had a worn out back which had been further damaged (identify belief) from his weight lifting (causal belief), and that he needed to protect his back and should not go to work (action). This made Jamie feel distressed and fearful for his future (emotional response). Jamie was also referred to a physiotherapist who reinforced the messages given by the doctor. He was given core exercises and was advised to hold his lumbar spine in lordosis and avoid lumbar flexion (control beliefs) to protect his damaged back (identify belief), in the hope that his disc would heal over the next two months (timeline belief).When Jamie's back was not improving after two months, his Doctor referred him to a neurosurgeon who suggested that he have spine injections (action). When this failed to reduce his pain, he was told surgery was required to remove the disc bulge (identity belief). Jamie underwent a discectomy L4/5 (action), however his back pain and levels of disability remained unchanged. He was then told his only option was to have a lumbar fusion (action). The combination of failed treatment and the thought of having more surgery frightened and distressed him further (negative emotional response). Six months after his original episode of back pain Jamie's pain levels were severe and he spent most of his day lying down, avoiding movement and exercise. His sleeping was disrupted and he was off work (action). He had been told by the neurosurgeon that he would never be able to run and lift weights again (negative health messages). He went on internet forums and read about the number of people who were in a similar predicament (negative social messages). He became fearful, anxious and depressed (negative emotional response).Sadly, Jamie's story is very common. It demonstrates the interaction between pain experience and social conditioning reinforced by negative advice from clinicians, leading to the belief that his back was damaged and needed to be protected and when this failed, fixed. This led to ineffective actions/coping responses (avoidance, protective behaviours, drugs, injections, surgery), that left him further disabled. When none of his actions were effective, his negative beliefs became further reinforced and his emotional distress increased. Jamie's representation of his back pain, which guided his actions and was reinforced by his clinicians, led him further away from his goals (to work, exercise and play with his children). At this point he lost hope that there was a way to move on with his life. The combination of negative perceptions about pain, passive and avoidance coping responses to pain, and emotional distress are strong predictors of outcome for people with musculoskeletal pain 19. |
Most people will have experienced a musculoskeletal pain symptom in the past six months or know someone who has21,22 and will therefore have developed their own beliefs about the symptom. Evidence suggests that pain beliefs emerge early in life and are influenced by parent/carer beliefs and behaviours.23 People of all ages, both with pain and without pain in geographically diverse settings, consistently view the body as a machine; believing pain is a sign that their body is damaged and that the ‘damaged’ body part needs to be rested to heal or be fixed.24–30 Such beliefs are well-captured by quotes from our qualitative research; “If something hurts, it's for a reason, it is your body saying don’t doit”31) “I believe in nuts and bolts; if something's worn out, you pull it out and put a new partin”.32 The notion of the ‘body as a machine’ is deep-seated in society, with roots tracing back to Decartes’ (1644) dualistic ‘biomedical’ model which attributed symptoms of pain to either somatic or psychogenic mechanisms, has dominated medical practice for over 350 years.33 We grow up understanding that pain is essential for our survival. It is the alarm system that protects us from actual or potential physical threat; the warning signal that tells us to withdraw our hand from boiling water or that something requires attention such as a sprained ligament or an unseen tumour. However, pain can also occur in the absence of nociception or injury such as with some acute pain states (i.e. headache and backache in the absence of injury), or pain that persists beyond normal tissue healing time.34,35 In these cases, pain is not usually a signal that damage is occurring to our body and can become unhelpful when it prevents us from engaging in normal activities.36
Despite scientific advancement in our understanding of pain mechanisms, many clinicians continue to believe that pain signals the presence of a damaged body part that needs to be investigated, healed or fixed.37–40 While clinical guidelines recommend against the use of MRI and Computerised Tomography scans (CT) in the diagnosis and management of musculoskeletal pain, the desire among clinicians to diagnose a tissue problem and fear of missing pathology contribute to the inappropriate use of imaging.41 The inappropriate imaging can cause harm by (i) misinterpretation of results leading to unnecessary downstream investigations and invasive interventions including surgery, and (ii) misinterpretation of results by patients leading to catastrophisation about the meaning of pain, fear and avoidance of activity and low expectations of recovery.42 Systematic review evidence suggests that clinicians who endorse ‘biomedical’ pain beliefs are more likely to engage in care that is inconsistent with guideline recommendations.14,15,41 This includes advice to rest, protect the body, and take time off work,43,44 as well as referral to expensive surgical interventions which are of limited benefit to patients and, in some cases, may be harmful.45
Qualitative studies suggest that encounters with clinicians play an important role in the formation and perpetuation of unhelpful pain beliefs in patients.26,46,47 Patients seeking care for musculoskeletal pain report being explicitly told by clinicians to avoid activity to prevent (further) damage to their body.32,43 Other implicit messages from clinicians such as the prescription of exercises to ‘protect’ the damaged body part appear to play a role in reinforcing negative beliefs about the vulnerability of the painful body part.43 Our recent studies have demonstrated that physiotherapists managing patients with musculoskeletal pain have an implicit bias that certain postures and movements are dangerous for the body (e.g. bending and lifting with a round back is dangerous to the back).48–50 Correspondingly, patients with back pain who are more fearful of bending and lifting are more guarded and stiffer when they perform these activities.51,52 Thus, clinician's implicit bias may influence their advice to patients.50,53,54
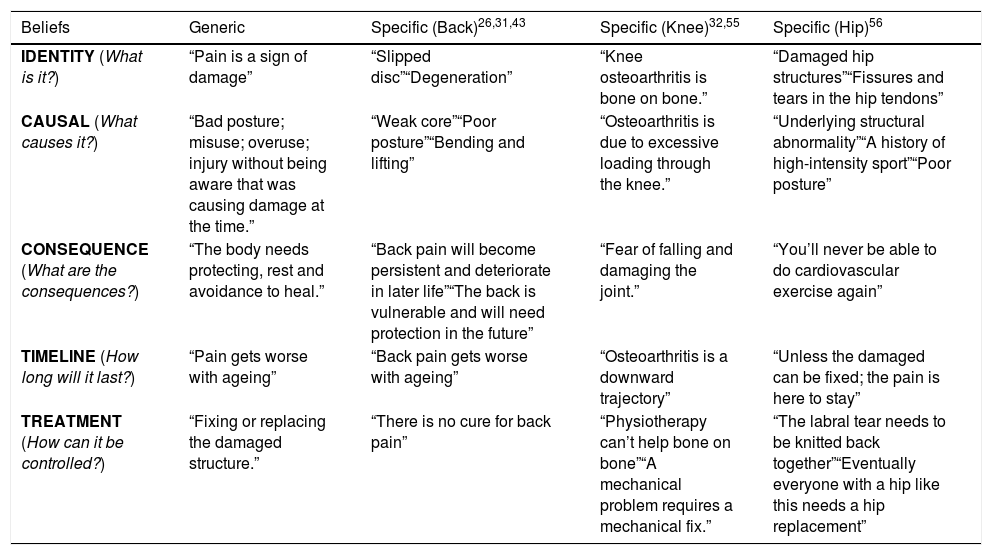
Qualitative studies investigating beliefs of people with common musculoskeletal pain conditions such as back pain,26,31,43 knee osteoarthritis32,55 and hip pain56 have highlighted some of the key beliefs held by society about the body and pain (Table 2).
Common beliefs about the body and pain.
| Beliefs | Generic | Specific (Back)26,31,43 | Specific (Knee)32,55 | Specific (Hip)56 |
|---|---|---|---|---|
| IDENTITY (What is it?) | “Pain is a sign of damage” | “Slipped disc”“Degeneration” | “Knee osteoarthritis is bone on bone.” | “Damaged hip structures”“Fissures and tears in the hip tendons” |
| CAUSAL (What causes it?) | “Bad posture; misuse; overuse; injury without being aware that was causing damage at the time.” | “Weak core”“Poor posture”“Bending and lifting” | “Osteoarthritis is due to excessive loading through the knee.” | “Underlying structural abnormality”“A history of high-intensity sport”“Poor posture” |
| CONSEQUENCE (What are the consequences?) | “The body needs protecting, rest and avoidance to heal.” | “Back pain will become persistent and deteriorate in later life”“The back is vulnerable and will need protection in the future” | “Fear of falling and damaging the joint.” | “You’ll never be able to do cardiovascular exercise again” |
| TIMELINE (How long will it last?) | “Pain gets worse with ageing” | “Back pain gets worse with ageing” | “Osteoarthritis is a downward trajectory” | “Unless the damaged can be fixed; the pain is here to stay” |
| TREATMENT (How can it be controlled?) | “Fixing or replacing the damaged structure.” | “There is no cure for back pain” | “Physiotherapy can’t help bone on bone”“A mechanical problem requires a mechanical fix.” | “The labral tear needs to be knitted back together”“Eventually everyone with a hip like this needs a hip replacement” |
Unhelpful pain beliefs play a key role in the transition from acute to chronic musculoskeletal pain. Prospective studies involving individuals without musculoskeletal pain at baseline have found that unhelpful beliefs predict the incidence of future disabling pain11,57 while among people with acute musculoskeletal pain, unhelpful beliefs predict the severity of disability overtime.58–60
Unhelpful behavioural responseThe relationship between pain beliefs and pain-related disability can be explained by the Fear Avoidance Model.36 According to this model, when someone believes a symptom of musculoskeletal pain presents a threat to their health and wellbeing, a fear response may be elicited, resulting in a fear avoidance ‘behavior’. This may manifest as a ‘protective’ response, such as movement restriction or protective muscle guarding, demonstrated in studies where people with back pain move slower, stiffer and with more muscle activity.61 On the other hand it may present as avoidance of activities, movements or postures associated with pain or the threat of pain in some situations, impacting on activities of daily living. In the home setting, fear avoidance of activities believed to be pain provoking or potentially damaging can lead to dependency on family members. For others it may be associated with avoidance of occupational activities, common among people with musculoskeletal pain.25,62,63 In the workplace, fear of pain or injury; concerns about coping with flare-ups in the workplace, and worry about their ability to fulfil work roles in the future can lead to absenteeism.64
Fear avoidance behaviour can be considered a common sense problem-solving response to a health threat, meaning that it is logical to avoid and protect a body part in pain when pain is believed to be a sign that damage is occurring to the body.65 However, there is evidence that these behavioural responses to pain perpetuate pain and disability. For example, bracing and guarding a joint or body region may themselves be pro-nociceptive by increasing tissue loading66 serving to heighten the pain experience and fuel the vicious fear avoidance cycle. Similarly avoidance of physical, occupational and work activity has a negative impact on a person's musculoskeletal and general health.67
Unhelpful emotional responseThere is strong evidence for the role that negative emotional factors play in perpetuating pain and disability. Negative emotional responses for many people represent a response to ineffective coping strategies to manage their pain, leading to a loss of engagement in valued activities, threatening their work and social life, as well as their physical health.68 For example avoidance of occupational activities affects job security and future financial security, causing emotional distress which further serves to heighten the pain experience.25 Other negative emotions such as frustration, anger and guilt at the inability to engage in valued life activities can lead to an altered “sense of self” compounding pain-related distress25 and the ability to cope with co-morbid conditions such as depression and anxiety as well as insomnia.56,62
An inability to make sense of the pain experience can also catalyse a negative emotional response. Believing that an underlying pathology is “both a necessary and sufficient cause of the symptoms experienced”33 becomes problematic when no identifiable pathology is observed. The default belief is that the absence of pathology means the symptom must instead be caused by psychogenic mechanics. Patients diagnosed with ‘non-specific’ musculoskeletal pain commonly perceive that the legitimacy of their pain experience is being called into question by others.25 This is reinforced by evidence that clinicians stigmatise patients without an identifiable pathology that can explain their symptoms, perceiving the patients’ pain is “all in their head”.12 In search of a biomedical explanation to legitimise their symptoms and enter the diagnosis-treatment-cure pathway, these patients may seek more care, more frequently,69 increasing the likelihood of receiving conflicting information which in turn, exacerbates diagnostic uncertainty and can be considered a form of iatrogenic distress.25 According to the Common Sense Model, the inability to make sense of a threatening pain experience will elicit a fear response. In the absence of a useful cognitive representation to inform problem solving behaviour, behaviour will be driven by this fear response.20
Clinicians’ beliefs about musculoskeletal painThere is strong evidence that clinicians commonly hold erroneous and unhelpful beliefs about musculoskeletal pain.43,44 As noted above, clinician beliefs can strongly influence their advice to patients, potentially fueling unhelpful coping responses.43,70
In the clinical setting, managing patient's beliefs, expectations and distress, while providing treatment under the time constraints of an appointment pose a significant challenge. In this context, reliance on automatic associations (biases) of clinical profiles (e.g. back and knee pain is associated with tissue damage) and treatment advice (e.g. protect the back/knee and avoid physical activity and loading) may unintendedly influence the clinician's advice.50,53,54 Therefore, clinicians may find it helpful to reflect on their own beliefs and experiences with pain. Here are examples of questions clinicians can use for self-reflection:
- •
What beliefs do I hold about the body and musculoskeletal pain?
- •
Where did these beliefs come from?
- •
What are my own experiences with pain?
- •
What was my coping response to the pain?
- •
What was my emotional response to the pain?
- •
Has this experience influenced the way I communicate with and manage my patients?
- •
Do I feel equipped to explore my patients’ beliefs, behavioural and emotional responses to pain?
- •
Am I aware of my own clinical biases?
- •
What stresses or frustrates me in clinical encounters?
How do I respond to my patient's emotional distress or conflicting beliefs?
“To understand the sufferer, one must understand the narrative, for it is through the story that the patient's suffering is accessed. This means both hearing the illness story and listening for the suffering narrative therein.”71
In this section, we will use the Common Sense Model (Fig. 1) as a framework to understand patient's beliefs, behavioural and emotional responses to their condition and the process by which change can be facilitated.
Person-centred communication underpins this process. This collaborative communication style involves incorporating the patient's perspective as part of the therapeutic process with the goal to engage the patient in a dialogue that elicits insights that may not be individually attained.71–73 Nonverbal communication such as body positioning, eye contact, use of expressive touch, good integration of documentation in the assessment can also be used to enhance patient engagement and provide opportunities for patients to fully express their concerns.72,74 Person-centred communication and nonverbal behaviour that is respectful, validating, non-judgemental, and empathetic builds trust and facilitates disclosure.72,75 This establishes a strong therapeutic alliance that can facilitate behavioural change.74
Person-centred interviewCompletion of a body chart and a multidimensional screening questionnaire (e.g. short form Orebro) prior to the interview can provide helpful insight into the patient's perception of their pain.76 Relevant items from the questionnaire can be used to explore patient's beliefs in the interview and examination. For instance, clinicians can use scores in individual items to guide the interview, and to facilitate disclosure about specific factors (e.g. “You scored 8/10 on ‘avoiding painful activities and work’; can you tell me about this?”).
How does this patient represent their symptoms?The interview provides the clinician with the cues needed for a targeted examination to explore behavioural and emotional responses linked to the patient's narrative. The following are key elements of this process:
- •
Use of open-ended questions such as “Tell me yourstory” facilitates a narrative approach to explore the patient's pain journey from their perspective.71
- •
The clinician provides a flexible framework during the interview that allows for sensitive, non-judgmental questioning and careful prompting to explore and interpret the patient's experience. This includes exploration of:
- •
How they represent their problem along the five belief dimensions that comprise the representation, and how previous experiences have led to adopting this representation (Table 3).
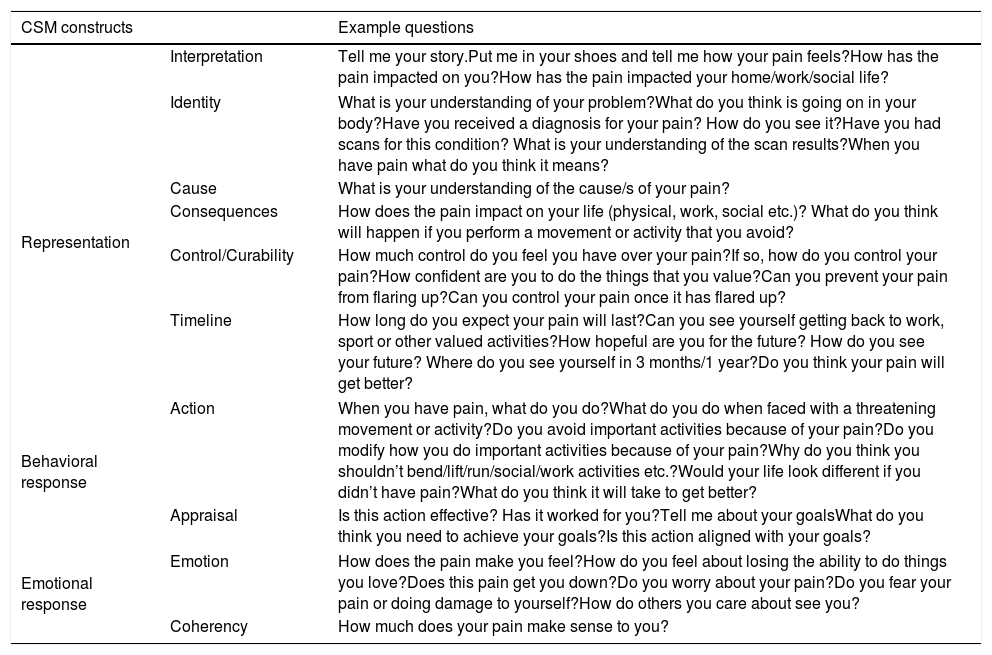
Table 3.How to explore patients’ understanding of pain using the CSM framework.
CSM constructs Example questions Interpretation Tell me your story.Put me in your shoes and tell me how your pain feels?How has the pain impacted on you?How has the pain impacted your home/work/social life? Representation Identity What is your understanding of your problem?What do you think is going on in your body?Have you received a diagnosis for your pain? How do you see it?Have you had scans for this condition? What is your understanding of the scan results?When you have pain what do you think it means? Cause What is your understanding of the cause/s of your pain? Consequences How does the pain impact on your life (physical, work, social etc.)? What do you think will happen if you perform a movement or activity that you avoid? Control/Curability How much control do you feel you have over your pain?If so, how do you control your pain?How confident are you to do the things that you value?Can you prevent your pain from flaring up?Can you control your pain once it has flared up? Timeline How long do you expect your pain will last?Can you see yourself getting back to work, sport or other valued activities?How hopeful are you for the future? How do you see your future? Where do you see yourself in 3 months/1 year?Do you think your pain will get better? Behavioral response Action When you have pain, what do you do?What do you do when faced with a threatening movement or activity?Do you avoid important activities because of your pain?Do you modify how you do important activities because of your pain?Why do you think you shouldn’t bend/lift/run/social/work activities etc.?Would your life look different if you didn’t have pain?What do you think it will take to get better? Appraisal Is this action effective? Has it worked for you?Tell me about your goalsWhat do you think you need to achieve your goals?Is this action aligned with your goals? Emotional response Emotion How does the pain make you feel?How do you feel about losing the ability to do things you love?Does this pain get you down?Do you worry about your pain?Do you fear your pain or doing damage to yourself?How do others you care about see you? Coherency How much does your pain make sense to you? - •
Contextual factors associated with their pain (e.g. home/social/work situation)
- •
Understanding a patient's behavioural response to their pain provides an insight into their beliefs (pain representation) as well as direction for the physical examination. This includes exploration of the patient's:
- •
Coping responses to pain
- •
Engagement or avoidance of physical, social, work or valued activities.
- •
Identification of postures, movements and activities that are feared, protected, avoided or that provoke the patient's pain
- •
Lifestyle behaviours such as sleep patterns and activity levels, and barriers to engage in a healthier lifestyle.
- •
Goals and expectations
Exploration of a person's emotional responses can be threatening to both the clinician and patient and needs to be sensitively done. Key aspects to explore include the patient's:
- •
Emotional response to pain, past treatments, and loss of valued activities.
- •
Fear of movement and activity (e.g. belief that movement may cause damage, or pain and functional loss)
- •
Overall levels of psychological well-being (e.g. anxiety, mood, stress)
- •
Social context and support
Clinicians must also screen for red flags, specific pathology, and comorbid health conditions.
At the end of the interview, the clinician summarises the patient's story, identifies gaps, discrepancies, and misconceptions in the representation, to reflect on how these impact the pain experience and how the patient makes sense of their pain experience.
Behavioural assessmentA person's representation, behavioural and emotional responses about their pain problem may not be entirely revealed by the interview. People can hold explicit views about the body and pain, but implicitly hold beliefs, fears and worries that drive their behaviour. Implicit beliefs that drive certain behaviours may be only revealed through exposure to the threat (posture, movement or activity) during a targeted behavioural assessment.48
Guided behavioural experiments can be used to assess the patient's pain, behavioural and emotional response during the performance of these tasks. Exposure to the target activities may elicit protective responses within the body that the patient may not be aware of, as it often unravels people's implicit beliefs and fears linked to specific daily tasks. Key actions that guide this process include:
- •
Target: The clinician identifies specific postures, movements or daily life activities identified in the interview as provocative, feared or avoided and that are linked to their goals.
- •
Question: Before exposure, the clinician asks the patient about their beliefs, fears and anticipated outcome (e.g. pain escalation) in relation to the task they are about to perform.
- •
Expose: The clinician performs non-judgemental observation of the behaviours adopted by the patient such as autonomic responses (e.g. respiratory pattern, body tension), pain behaviours (e.g. grimacing) and safety-seeking behaviours (e.g. bracing, avoidance of limb loading) during the performance of the nominated tasks.
- •
Reflect: The clinician asks the patient if they are aware of their behaviour during the performance of the task and guides the patient to reflect on the reason why they adopted such behaviour. For instance, a patient with knee pain may shift their weight to the opposite leg while getting up from a chair. Their reason for such behaviour may be that they believe that putting weight through the joint may cause more wear and tear. A patient with back pain may not be aware that they brace their abdominal muscles and breath-hold while picking an object off the floor. When asked about it, they may say that it is ‘common knowledge’ that people protect their back and brace their core when they bend.
- •
Expose with control: First the clinician coaches the patient to relax their body posture and breathing pattern to ensure the patient feels safe and calm. During exposure, the clinician provides strategies to control unhelpful behavioural (e.g. avoidance of leg loading on sit to stand) and emotional (e.g. worry about pain) responses, providing an opportunity for the person to perform the task in a different way (new mindset and behaviour) that often yields a different outcome. For a person with knee pain the strategy may be engaging leg muscles and loading both legs equally on sit to stand. For a person with back pain, the strategy may be breathing, relaxing the back and core while bending or lifting.
- •
Appraise: After exposure, the clinician asks the patient to reflect on their experience and if the predicted outcome occurred or not.
- •
Repeat exposure in new way: The clinician repeats exposure of the task to build confidence, and gradually progresses the task towards the patient's needs and goals. Clinicians must consider and be sensitive to the patient's levels of distress, tissue sensitivity and levels of conditioning, as an aversive experience may negatively reinforce their beliefs and emotional responses (i.e. “bending is scary, it makes my pain worse and should beavoided”). This guides how quickly exposure is progressed to more threatening and demanding tasks.
This process tests the validity of patients’ belief systems; where discrepancies between anticipated and actual pain experience may challenge and disconfirm the person's beliefs that movement is threatening and should be avoided.77 In addition, it can reinforce that valued activities can be safely confronted when performed with effective strategies and a more positive mindset. This process provides the clinician with clear directions for targeted management.66,78
Development of a new representation that makes senseThis is an interactive learning process where the clinician uses the patient's own narrative and experience during the examination to help them make sense of their pain condition through a biopsychosocial lens, with the aim to facilitate mindset and behavioural change, and reduce emotional distress. In this process, the clinician:
- •
Uses a person-centred communication style that empowers the patient's narrative and that enables effective shared decision-making in the rehabilitation process.
- •
Explains in the patient's own words how unhelpful beliefs, behaviours and emotional responses to pain can set up a vicious cycle of pain and disability.
- •
Delivers education in simple language combined with their experiences during the guided behavioural experiments to dispel myths about pain.
- •
Identifies new ways of thinking as well as positive behavioural and emotional ways to respond to pain.
- •
Promotes learning not only via explanation, but also via demonstration, behavioural experimentation (doing, and reflecting), visual feedback (mirror, recording), and self-experimentation (out of the clinic).
- •
Uses educational resources78,79 (e.g.www.lowbackpaincommunication.com), educational websites, and patient stories to augment this learning process (e.g. www.painhealth.csse.uwa.edu.au;www.myjointpain.org.au;www.pain-ed.com).
- •
Identifies goals and sets realistic time frames.
Behavioural change may only occur if the patient feels confident to independently test the new strategies in their daily life. In order to reinforce behaviour change clinicians need to:
- •
Encourage patients to integrate the new learned functional strategies immediately into daily activities to build self-efficacy and to strengthen the new representation.
- •
Engage family and friends to support the process.
- •
Encourage healthy lifestyle changes such as physical activity, weight loss and good sleep habits. Changes that are in line with patient's context, preferences, and goals are likely to be sustainable.
- •
Coach patients to progress gradually according to their goals, level of conditioning and perceived control over their pain.
- •
Encourage patients to respond differently to pain (in a more positive way) and perform valued activities with confidence, and without pain vigilance.
This enables a process of self-learning and self-discovery during the rehabilitation that helps patients build confidence, reinforce the new mindset and feel in charge of their rehabilitation to achieve their goals.
Integrated co-careMusculoskeletal pain conditions share risk factors with other chronic health conditions such as cardiovascular disease, type 2 diabetes, and mental health disorders.80 The pattern of health and disease in our population is changing. As such, the proportion of patients who experience pain (in one or more body regions) and that have comorbid health conditions continues to increase.81
Clinicians should refer patients for co-care in the presence of comorbid mental (e.g. emotional distress, depression, eating disorders) and physical health conditions (e.g. type 2 diabetes, heart disease, morbid obesity). We contend that multi-disciplinary care including psychologist, pain physician, medical doctor and physiotherapist needs to be integrated, so the team shares a common framework and delivers consistent messages that prevents care fragmentation and patient distress.82,83
Barriers for implementing changeThere are a number of barriers to implement behavioural change. These include:
- •
Patients’ own beliefs about pain (e.g. caused by structural damage) and expectations towards management (e.g. treatments targeting a faulty structure will ‘fix’ their pain).
- •
Patients may be confronted by mixed or erroneous messages across many levels of society including family, work, and media. For instance, a patient may receive evidence-based information from their physiotherapist that it is safe to exercise with knee osteoarthritis; however, when sharing this message with their partner the information is confronted by ‘popular belief’ that exercise is harmful as it causes joint wear and tear. For patients with low self-efficacy, this situation may reduce the patient's confidence in engaging with an exercise programme.
- •
Patients can also receive mixed messages when engaging with the healthcare system. For example, one clinician tells the patient that it is safe to return to work, while another says that returning to work may hinder recovery. These mixed messages often leave the patient confused and distressed.
- •
Clinician's tendency to lecture patients, rather than adopting a patient-centred reflective approach to care.
- •
Clinicians’ beliefs about pain, implicit biases, perceived competence to address psychosocial factors and other comorbid heath conditions, time constraints of appointments, financial pressures are some of the barriers for clinicians to implement person-centred approaches.
- •
Lack of adequate funding for evidence-based care.
- •
Social circumstances may also be a barrier for implementation of sound advice. Consider a patient with knee osteoarthritis who has been advised to exercise regularly. Although the advice is sound, this patient is a single mother of two, who works part-time and cares for her own ill mother. This context may not be conducive of implementing the suggested management plan.
Both patients and clinicians need to understand pain from a biopsychosocial perspective in which multiple factors can influence the onset and persistence of pain, and that ultimately the development of self-management skills is paramount. Patients’ beliefs and treatment expectations may benefit from mass media campaigns that aim to promote evidence-based information and subsequently improve health behaviours in musculoskeletal pain, as it has in other fields such as heart disease.84 Here are strategies that may benefit clinicians in the delivery of a person-centred approach to managing musculoskeletal pain:
- •
Be interested, curious and non-judgemental.
- •
Observe experienced clinicians in action.
- •
Seek peer review feedback and mentoring.
- •
Self-reflect upon clinical sessions that yielded both positive and negative outcomes.
- •
Watch videos of yourself interacting with a patient to identify potential areas for change in terms of clinical skills, verbal and non-verbal communication style, habits and biases.
- •
Develop communication skills that allow for sensitive exploration of the person's experience across multiple domains to identify targets for behavioural change.
- •
Take time to listen, reflect and act accordingly.
- •
Develop good diagnostic, observational, analytical and interpretive skills to confidently address unhelpful behaviours and provide adequate clinical advice to patients.
- •
Develop skills to better manage coexisting physical and mental health problems.
The process of change is unique for each person.77 For some this process can be fast (4–12 weeks), while for others it may take longer (3–6 months). Booster sessions may be necessary for when pain again becomes uncontrollable, distressing and/or disabling. During pain flares, the old representation can resurge strongly, often re-activating unhelpful behavioural and emotional responses. Clinicians must use pain flares as an opportunity for reinforcing the new representation and new ways to respond to pain without emotional distress, protective behaviours and avoidance of movement, physical, work or social engagement.66,85
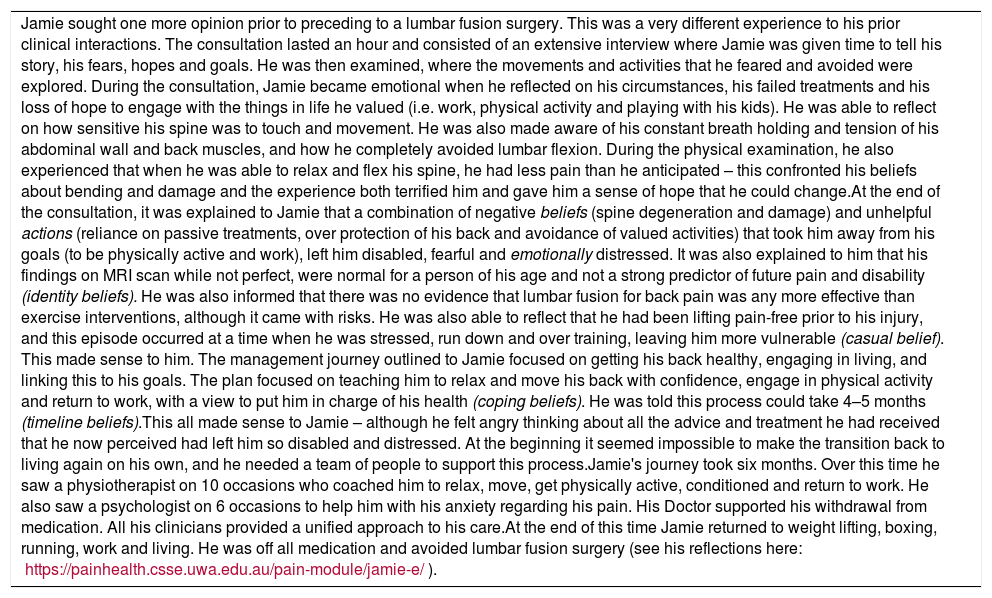
The critical role that beliefs can have on the outcome of musculoskeletal pain is illustrated in Table 4 (Jamie's story - a journey to recovery; and an interview with Jamie). These beliefs include those of the clinician and the patient. It highlights how person-centred care can be used to facilitate helpful beliefs, as well as positive behavioural and emotional responses to musculoskeletal pain (Fig. 2). This approach in the acute phase can prevent ongoing pain and disability in the long term,86 and in the chronic phase reduce the disability burden of musculoskeletal pain.87,88 There are huge obstacles to deliver this model of care that need to be overcome.
Clinical scenario: Jamie's story – a journey to recovery.
| Jamie sought one more opinion prior to preceding to a lumbar fusion surgery. This was a very different experience to his prior clinical interactions. The consultation lasted an hour and consisted of an extensive interview where Jamie was given time to tell his story, his fears, hopes and goals. He was then examined, where the movements and activities that he feared and avoided were explored. During the consultation, Jamie became emotional when he reflected on his circumstances, his failed treatments and his loss of hope to engage with the things in life he valued (i.e. work, physical activity and playing with his kids). He was able to reflect on how sensitive his spine was to touch and movement. He was also made aware of his constant breath holding and tension of his abdominal wall and back muscles, and how he completely avoided lumbar flexion. During the physical examination, he also experienced that when he was able to relax and flex his spine, he had less pain than he anticipated – this confronted his beliefs about bending and damage and the experience both terrified him and gave him a sense of hope that he could change.At the end of the consultation, it was explained to Jamie that a combination of negative beliefs (spine degeneration and damage) and unhelpful actions (reliance on passive treatments, over protection of his back and avoidance of valued activities) that took him away from his goals (to be physically active and work), left him disabled, fearful and emotionally distressed. It was also explained to him that his findings on MRI scan while not perfect, were normal for a person of his age and not a strong predictor of future pain and disability (identity beliefs). He was also informed that there was no evidence that lumbar fusion for back pain was any more effective than exercise interventions, although it came with risks. He was also able to reflect that he had been lifting pain-free prior to his injury, and this episode occurred at a time when he was stressed, run down and over training, leaving him more vulnerable (casual belief). This made sense to him. The management journey outlined to Jamie focused on getting his back healthy, engaging in living, and linking this to his goals. The plan focused on teaching him to relax and move his back with confidence, engage in physical activity and return to work, with a view to put him in charge of his health (coping beliefs). He was told this process could take 4–5 months (timeline beliefs).This all made sense to Jamie – although he felt angry thinking about all the advice and treatment he had received that he now perceived had left him so disabled and distressed. At the beginning it seemed impossible to make the transition back to living again on his own, and he needed a team of people to support this process.Jamie's journey took six months. Over this time he saw a physiotherapist on 10 occasions who coached him to relax, move, get physically active, conditioned and return to work. He also saw a psychologist on 6 occasions to help him with his anxiety regarding his pain. His Doctor supported his withdrawal from medication. All his clinicians provided a unified approach to his care.At the end of this time Jamie returned to weight lifting, boxing, running, work and living. He was off all medication and avoided lumbar fusion surgery (see his reflections here: https://painhealth.csse.uwa.edu.au/pain-module/jamie-e/). |
Beliefs about the body and musculoskeletal pain influence a person's behavioural and emotional response to pain. Beliefs are modifiable and should be considered an important target for the management of musculoskeletal pain. Clinicians have an important role to disseminate positive, evidence-based beliefs about musculoskeletal pain to both patients and society in general. However, many clinicians hold erroneous beliefs themselves, while others feel unskilled to explore and target patients’ beliefs, perceiving this to be outside of their scope of practice. As such, we encourage clinicians to exercise self-reflection to explore their own beliefs and better understand their biases, which may influence their management of patients with musculoskeletal pain. Training may be required to facilitate this process.
We propose that clinical encounters should be used to create a learning opportunity in which a person's representation, behavioural and emotional responses to their pain can be safely explored. Disconfirming unhelpful beliefs through behavioural learning, self-reflection and evidence-based education, can promote a new understanding that empowers self-management.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interestJP Caneiro and Peter O'Sullivan deliver educational workshops on patient-centred care for the management of pain. Samantha Bunzli declares no conflict of interest.
The authors acknowledge the patient (Jamie E) for sharing his story.